Sprayable Peptide Amphiphile Nanofibers: A Revolutionary Biomaterial for Advanced Wound Healing
This article comprehensively reviews the development, application, and therapeutic potential of sprayable peptide amphiphile (PA) nanofibers for wound management.
Sprayable Peptide Amphiphile Nanofibers: A Revolutionary Biomaterial for Advanced Wound Healing
Abstract
This article comprehensively reviews the development, application, and therapeutic potential of sprayable peptide amphiphile (PA) nanofibers for wound management. Targeting researchers, scientists, and drug development professionals, we explore the foundational chemistry of PA self-assembly into bioactive nanofibers that mimic the native extracellular matrix. The scope covers molecular design principles, innovative sprayable delivery methodologies that enable in-situ gelation, and optimization strategies to overcome translational challenges. We further present rigorous preclinical validation data and comparative analyses with conventional wound therapies, highlighting the significant enhancement in healing outcomes for burns and chronic wounds. This synthesis aims to inform future research and accelerate the clinical adoption of this transformative nanotechnology.
The Molecular Blueprint: Understanding Peptide Amphiphile Self-Assembly and Bioactivity
Core Molecular Structure of Peptide Amphiphiles
Peptide amphiphiles (PAs) are a class of peptide-based molecules that combine the structural features of amphiphilic surfactants with the functions of bioactive peptides [1]. These molecules are designed to self-assemble into a variety of supramolecular nanostructures, including high-aspect-ratio nanofibers, which are of significant interest for wound healing applications [1] [2]. The canonical structure of a peptide amphiphile, as developed in foundational research, comprises four distinct key segments [1] [2]:
- 1. Hydrophobic Domain: This region typically consists of a long alkyl tail (e.g., palmitic acid with 10-16 carbons) and serves as the primary driver for the self-assembly process via the hydrophobic effect [1] [2].
- 2. β-Sheet Forming Sequence: Adjacent to the hydrophobic segment, this region consists of a short sequence of hydrophobic amino acids with a strong propensity to form intermolecular hydrogen bonds, stabilizing the resulting one-dimensional nanostructure [1].
- 3. Charged Amino Acids: This hydrophilic segment contains ionizable residues (e.g., aspartic acid, glutamic acid, lysine) that enhance the PA's solubility in aqueous solutions and allow for the design of systems responsive to pH and ionic strength [1] [2].
- 4. Bioactive Epitope: The terminal region of the peptide sequence is functionalized with a bioactive signal (e.g., RGD, IKVAV) designed to interact with cells or proteins, imparting specific biological functions to the self-assembled material [1] [2].
Table 1: Core Segments of a Canonical Peptide Amphiphile Molecule
| Segment Number | Segment Name | Core Function | Common Molecular Components |
|---|---|---|---|
| 1 | Hydrophobic Domain | Drives self-assembly via hydrophobic collapse | Alkyl tail (e.g., palmitic acid, C16) |
| 2 | β-Sheet Forming Sequence | Enforces nanofiber geometry via H-bonding | Repetitive sequences like VVVAAA or (SL)6 |
| 3 | Charged Amino Acids | Confers water solubility & triggers assembly | Aspartic acid, Glutamic acid, Lysine |
| 4 | Bioactive Epitope | Elicits specific biological responses | RGD (cell adhesion), IKVAV (neurite outgrowth) |
Molecular Self-Assembly into Nanofibers
The self-assembly of PAs into nanofibers is a hierarchical process. In an aqueous environment, the hydrophobic tails aggregate to minimize their contact with water, forming the core of the structure. Simultaneously, the β-sheet-forming sequences align and create a network of hydrogen bonds, forming the cylindrical wall of the nanofiber. This arrangement positions the charged residues and, crucially, the bioactive epitopes on the exterior surface of the fiber, making them available for biological interactions [1]. This assembly can be triggered by a physiological stimulus, such as the presence of salts in bodily fluids, making PAs excellent candidates for injectable or sprayable therapies that gel in situ [1] [2].
Protocol: Fabrication of Sprayable PA Nanofiber Hydrogels for Wound Healing
This protocol details the synthesis, self-assembly, and in vitro characterization of a bioactive PA hydrogel designed for sprayable wound healing applications. The model PA incorporates the IKVAV epitope, known for promoting neurite outgrowth and wound repair [1].
Materials and Reagents
Table 2: Essential Research Reagents and Materials
| Item Name | Function/Application | Exemplary Supplier/Part Number |
|---|---|---|
| Palmitic Acid | Hydrophobic tail component for PA synthesis | Sigma-Aldrich, P0500 |
| Rink Amide MBHA Resin | Solid support for peptide synthesis | AAPPTec, SP-1000 |
| Fmoc-Protected Amino Acids | Building blocks for peptide sequence | AAPPTec or ChemPep |
| IKVAV Peptide Epitope | Bioactive signal for promoting wound healing | Custom synthesis required |
| Dulbecco's Phosphate Buffered Saline (DPBS) | Physiological trigger for self-assembly | Thermo Fisher, 14190144 |
| Dichloromethane (DCM) | Solvent for resin washing | Sigma-Aldrich, 270997 |
| N,N-Dimethylformamide (DMF) | Solvent for peptide synthesis | Sigma-Aldrich, 227056 |
| Trifluoroacetic Acid (TFA) | Cleavage cocktail component for resin cleavage | Sigma-Aldrich, T6508 |
| Diethyl Ether | Solvent for PA precipitation | Sigma-Aldrich, 309966 |
Step-by-Step Experimental Procedure
Part A: Solid-Phase Peptide Synthesis of the PA Molecule
- Resin Swelling: Place 0.5 g of Rink Amide MBHA resin (loading: 0.5 mmol/g) into a solid-phase peptide synthesis (SPPS) reactor. Swell the resin with 10 mL of DCM for 30 minutes with gentle agitation.
- Fmoc Deprotection: Drain the DCM and treat the resin twice with 10 mL of 20% (v/v) piperidine in DMF (5 min per treatment) to remove the Fmoc protecting group.
- Coupling Cycle: After thorough washing with DMF (5 x 10 mL), add 4 equivalents of the first Fmoc-protected amino acid, 4 equivalents of HBTU, and 8 equivalents of N,N-Diisopropylethylamine (DIPEA) in DMF. React for 45-60 minutes with agitation.
- Sequence Elongation: Repeat steps 2 and 3 for each amino acid in the sequence: C16-VVVAAAEEEE-IKVAV (from C- to N-terminus).
- Palmitoylation: After the final Fmoc deprotection, couple palmitic acid (4 eq) using HBTU/DIPEA activation overnight.
- Cleavage and Deprotection: Cleave the PA from the resin and remove side-chain protecting groups using a cocktail of TFA:Triisopropylsilane:Water (95:2.5:2.5) for 3 hours.
- Precipitation and Purification: Precipitate the crude PA in cold diethyl ether, collect by centrifugation, and purify via reversed-phase HPLC. Lyophilize the pure fractions to obtain a white fluffy solid.
Part B: Preparation and Characterization of the Sprayable Hydrogel
- Stock Solution Preparation: Dissolve the purified PA in sterile, deionized water to a final concentration of 1.0% (w/v). Adjust the pH to 7.4 using a dilute NaOH solution. Sterilize the solution by passing it through a 0.22 µm filter. Note: The solution should remain clear and have low viscosity at this stage.
- Gelation Triggering (Spray Simulation): Load the PA solution into a spray device (e.g., an airbrush system). Spray the solution onto a sterile surface from a distance of 10-15 cm. Simultaneously, mist the stream with a simulated physiological buffer (e.g., 150 mM NaCl or DPBS) to trigger instantaneous gelation upon contact.
- Rheological Characterization: To quantify mechanical properties, induce gelation in situ on the plate of a rheometer by adding 20 µL of 10x DPBS to 180 µL of the PA solution. Perform a time sweep experiment at 1 Hz frequency and 1% strain to monitor the storage (G') and loss (G'') moduli over time.
Quality Control and Functional Assay
- Critical Aggregation Concentration (CAC): Determine the CAC using a pyrene fluorescence assay. The CAC is typically in the low micromolar range (e.g., 5-20 µM) for effective PAs [1].
- Cytocompatibility (ISO 10993-5): Culture human dermal fibroblasts (HDFs) in the presence of PA hydrogel extracts. Assess cell viability after 24 hours using a standard MTT assay. A viability >90% relative to the control is considered non-cytotoxic.
- In Vitro Wound Healing Assay: Create a scratch wound in a confluent monolayer of HDFs. Monitor wound closure over 48 hours in the presence of the PA hydrogel or its eluent compared to a control. Calculate the percentage of wound closure at 12, 24, and 48-hour time points.
Table 3: Key Quantitative Parameters for a Functional PA Hydrogel
| Parameter | Target Value/Range | Analytical Method |
|---|---|---|
| PA Purity | >95% | Analytical HPLC |
| Critical Aggregation Concentration (CAC) | 5 - 20 µM | Pyrene Assay |
| Gelation Time | < 60 seconds | Visual test / Rheometry |
| Storage Modulus (G') | 100 - 5000 Pa | Oscillatory Rheometry |
| Fibroblast Viability | >90% | MTT Assay |
| IKVAV Density on Fiber | ~ 10^15 epitopes/cm² | Calculated from structure [1] |
Application Notes and Troubleshooting
- Bioactivity Failure: If the final PA gel lacks the expected bioactivity, verify the integrity of the bioactive epitope after synthesis via mass spectrometry. The epitope may be susceptible to degradation or improper folding during synthesis.
- Insufficient Gel Strength: If the hydrogel is too weak, consider increasing the length of the β-sheet forming segment or the alkyl tail to enhance intermolecular interactions. Alternatively, increase the overall PA concentration.
- Slow Gelation Kinetics: For a sprayable system, rapid gelation is critical. If gelation is too slow, pre-mix the PA solution with a minimal volume of a concentrated salt solution immediately before the spray nozzle, or use a dual-spray system that mixes the streams upon ejection.
- PA Precipitation: If the PA precipitates instead of forming a gel upon salt addition, the charged segment might be too short. Redesign the PA to include additional charged residues to improve solubility before assembly.
Supramolecular chemistry, famously termed "chemistry beyond the molecule," provides the foundation for designing highly organized systems across multiple length scales without covalent bonds [3]. This approach is particularly powerful in creating biomaterials for regenerative medicine, where peptide amphiphiles (PAs) have emerged as a versatile platform for constructing nanofibrous structures that emulate the native extracellular matrix (ECM) [3] [4]. These self-assembled nanostructures are exceptionally suitable for wound healing applications, as they can be designed to display bioactive signals, deliver therapeutic payloads, and assemble into injectable or sprayable hydrogels that conform to complex wound beds [5] [4]. The dynamic and reversible nature of supramolecular interactions enables the creation of smart materials that can respond to physiological cues, making them ideal for advanced therapeutic strategies in skin regeneration and repair [3] [6].
Molecular Design of Peptide Amphiphiles
The structural blueprint of peptide amphiphiles follows a modular domain approach, with each segment playing a distinct role in the self-assembly process and biological function [3] [7]. A typical PA molecule incorporates four key regions that work in concert to drive nanofiber formation and bioactivity.
- Hydrophobic Domain: This segment typically consists of a long alkyl tail (often derived from palmitic acid) that drives the hydrophobic collapse and forms the core of the nanofiber. This domain is crucial for the amphiphilic character of the molecule [3].
- β-Sheet Forming Sequence: Adjacent to the alkyl tail, a short peptide sequence with a strong propensity to form intermolecular hydrogen bonds promotes the formation of β-sheets. The principal axes of these β-sheets run parallel to the long axis of the nanofiber, governing the one-dimensional growth into high-aspect-ratio nanostructures [3].
- Charged Segment: This region contains acidic or basic amino acids that provide electrostatic repulsion in solutions of low ionic strength, ensuring adequate solubility and preventing premature assembly. This design enables triggered self-assembly upon exposure to physiological electrolytes, facilitating injectable or sprayable formulations that gel at the wound site [3] [5].
- Bioactive Epitope: The terminus opposite the hydrophobic tail is functionalized with a bioactive peptide signal (e.g., RGDS or IKVAV) that interacts with cellular receptors. This epitope is displayed on the nanofiber surface at high density, enabling the material to directly signal cells and influence their behavior [3] [7].
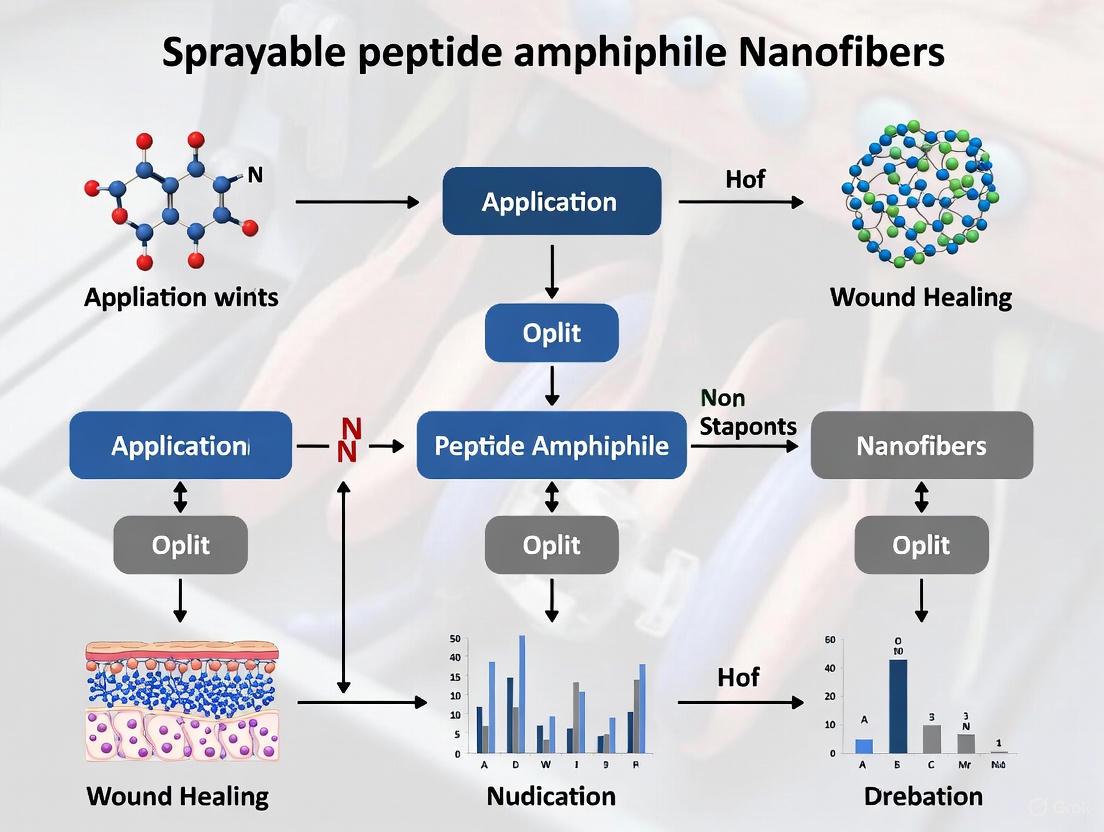
The following diagram illustrates the logical relationship between the molecular structure of a peptide amphiphile and its hierarchical assembly into a bioactive nanofiber network suitable for wound healing.
Key Characterization Data for PA Nanofibers
Rigorous characterization is essential to confirm the successful synthesis of PA monomers and their subsequent assembly into the desired supramolecular structures. The following data, derived from established protocols, provides benchmarks for key physical and biological properties.
Table 1: Quantitative Characterization Data for Peptide Amphiphile Nanofibers
| Characterization Method | Key Parameters Measured | Typical Results/Output |
|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Molecular weight, purity of PA monomers | Confirmation of exact mass; purity >95% often required for biological applications [5]. |
| Circular Dichroism (CD) | Secondary structure, internal ordering during assembly | Characteristic minimum at ~218 nm indicating β-sheet formation [5]. |
| Transmission Electron Microscopy (TEM) | Nanofiber morphology, diameter, length | High-aspect-ratio cylindrical nanofibers; diameters ~6-10 nm [3] [5]. |
| Rheology | Storage modulus (G'), loss modulus (G"), gelation time | Shear-thinning behavior; G' > G" indicating solid-like gel behavior; gelation via ionic crosslinking [5]. |
| Cell Viability Assay (e.g., LDH) | Biocompatibility, cytotoxicity | >90% cell viability confirmed in human embryonic kidney cells [5]. |
| Endothelial Cell Tube Formation Assay | Angiogenic potential | Significant increase in tubule length and branch points compared to controls [5]. |
Table 2: Biological Performance of PA Nanofibers in Wound Healing Models
| Bioactive Signal | Experimental Model | Key Healing Outcomes |
|---|---|---|
| RGDS | In vitro thermally damaged human fibroblasts (hFBs) and human umbilical vein endothelial cells (HUVECs) | Significant stimulation of cell proliferation and migration [7]. |
| RGDS | In vivo rat burn model | Accelerated burn wound closure; stimulation of fibroblast and epithelial cell proliferation [7]. |
| Pro-angiogenic PA | In vitro endothelial cell tube formation assay | Enhanced blood vessel formation, indicating promise for treating deep dermal burns [5]. |
Experimental Protocols
The following protocols detail the essential procedures for the preparation, characterization, and functional testing of peptide amphiphile nanofibers for wound healing applications.
Protocol: Solid-Phase Synthesis of Peptide Amphiphiles
This protocol describes the synthesis of peptide amphiphiles using solid-phase peptide synthesis (SPPS), which allows for the sequential addition of protected amino acids while the growing chain is anchored to an insoluble resin [5] [8].
- Resin Loading: Begin with a rink amide resin (loading capacity: ~0.5 mmol/g). Place the resin in a solid-phase reaction vessel. Deprotect the Fmoc group by treating the resin with 20% piperidine in DMF (2 x 10 mL, 5 min each).
- Amino Acid Coupling: For each amino acid in the sequence (starting from the C-terminus), perform the following:
- Wash the resin with DMF (3 x 10 mL).
- Prepare a coupling mixture of Fmoc-protected amino acid (4 equiv.), HBTU (3.9 equiv.), and HOBt (3.9 equiv.) in DMF. Add DIPEA (8 equiv.) to activate the amino acid.
- Add the coupling mixture to the resin and agitate for 1-2 hours at room temperature.
- Wash the resin with DMF (3 x 10 mL) after coupling is complete.
- Remove the Fmoc protecting group with 20% piperidine in DMF (2 x 10 mL, 5 min each) before the next coupling cycle. Confirm deprotection by a Kaiser test.
- Alkylation: Following the completion of the peptide sequence, couple palmitic acid (4 equiv.) using the same coupling reagents and protocol (HBTU/HOBt/DIPEA) to form the hydrophobic tail [3].
- Cleavage and Deprotection: After the final Fmoc deprotection, wash the resin with DCM (3 x 10 mL). Cleave the peptide amphiphile from the resin and remove side-chain protecting groups using a cleavage cocktail (e.g., TFA:TIS:Water, 95:2.5:2.5, 3 mL per 100 mg resin) for 3 hours with gentle agitation.
- Precipitation and Purification: Filter the cleavage mixture and precipitate the crude PA in cold diethyl ether. Centrifuge to collect the pellet. Purify the PA via reverse-phase high-performance liquid chromatography (RP-HPLC). Analyze the final product using LC-MS to confirm molecular weight and purity [5].
Protocol: Self-Assembly and Gelation of PA Nanofibers
This protocol triggers the self-assembly of PA monomers into nanofibers and the subsequent formation of a hydrogel network, suitable for creating a sprayable wound dressing [3] [5].
- Preparation of Aqueous PA Solution: Dissolve the purified PA in ultrapure water (e.g., 1% w/v) by gently vortexing and/or brief sonication in an ice bath. The solution should be clear and have a low viscosity at this stage.
- Induction of Self-Assembly:
- Salt-Triggered Assembly: Add a calculated volume of a sterile, concentrated phosphate-buffered saline (PBS) or Dulbecco's PBS (DPBS) solution to the aqueous PA solution to achieve physiological ionic strength (e.g., 1x PBS). Mix gently. An immediate increase in viscosity and gelation will be observed.
- pH-Triggered Assembly: Alternatively, for PAs containing acidic residues, self-assembly can be initiated by adding a minimal volume of a basic solution (e.g., NaOH) to neutralize the charges and reduce electrostatic repulsion.
- Ionic Crosslinking: To enhance the mechanical stability of the hydrogel, the PA nanofiber network can be ionically crosslinked. This is achieved by the addition of divalent cations such as Ca²⁺ or Mg²⁺ (e.g., from CaCl₂ solution), which chelate with terminal carboxylic acid groups on the PA fibers [5].
Protocol: In Vitro Angiogenesis Assay
This protocol assesses the pro-angiogenic potential of the bioactive PA nanofibers by measuring their ability to promote endothelial tube formation, a critical process in wound healing [5].
- Preparation of Gelled PA Substrate:
- Place a 24-well culture plate on ice. Add 300 µL of the sterile aqueous PA solution (prepared in Protocol 4.2, Step 1) to each well.
- Carefully add 300 µL of sterile, warm (37°C) cell culture medium (e.g., EGM-2 for HUVECs) containing 2x concentration of serum and ions to trigger gelation. Gently swirl to mix without introducing bubbles.
- Incubate the plate at 37°C for 30 minutes to allow a firm gel to form.
- Cell Seeding and Tubule Formation:
- Trypsinize and harvest human umbilical vein endothelial cells (HUVECs). Resuspend the cells in complete endothelial cell growth medium.
- Seed HUVECs onto the surface of the pre-formed PA gel at a density of 1.0 x 10⁵ cells per well.
- Incubate the cells at 37°C, 5% CO₂ for 6-18 hours.
- Imaging and Quantification:
- After incubation, image the tubular structures using an inverted phase-contrast microscope at 4x or 10x magnification. Acquire multiple non-overlapping images per well.
- Analyze the images using image analysis software (e.g., ImageJ with the Angiogenesis Analyzer plugin). Quantify key parameters including the total tube length, number of branches, and number of master segments per field of view. Compare results to control groups (e.g., cells on non-bioactive PA gels or tissue culture plastic).
The Scientist's Toolkit: Essential Research Reagents
Successful research and development in supramolecular biomaterials require a specific set of reagents and instruments. The following table lists the essential components for working with peptide amphiphile nanofibers.
Table 3: Essential Research Reagents and Materials for PA Nanofiber Development
| Item Category | Specific Examples | Function/Purpose |
|---|---|---|
| Synthesis & Purification | Rink Amide Resin, Fmoc-Protected Amino Acids, Palmitic Acid, HBTU/HOBt, DIPEA, Trifluoroacetic Acid (TFA), HPLC-grade solvents (Acetonitrile, Water) | Solid-phase synthesis of the PA molecule; cleavage from resin; purification and analysis of the final product [5] [8]. |
| Assembly & Formulation | Ultrapure Water, Phosphate-Buffered Saline (PBS), Calcium Chloride (CaCl₂) Solution | To solubilize PA monomers; trigger self-assembly into nanofibers via physiological electrolytes; and ionically crosslink the nanofiber network to form a hydrogel [3] [5]. |
| Characterization | Liquid Chromatography-Mass Spectrometry (LC-MS), Circular Dichroism (CD) Spectropolarimeter, Transmission Electron Microscope (TEM), Rheometer | Confirm PA identity and purity; analyze secondary structure (β-sheet content); visualize nanofiber morphology; and measure mechanical properties of the hydrogel [5]. |
| Biological Assessment | Human Dermal Fibroblasts (hFBs), Human Umbilical Vein Endothelial Cells (HUVECs), Cell Culture Media and Supplements, Lactate Dehydrogenase (LDH) Assay Kit, Matrigel (for assay control) | Evaluate biocompatibility (cytotoxicity); assess functional bioactivity, such as the ability to promote angiogenesis in vitro [7] [5]. |
Application Workflow for a Sprayable Wound Dressing
The pathway from molecular design to functional application integrates synthesis, characterization, and formulation steps. The following diagram outlines the comprehensive workflow for developing a sprayable PA nanofiber dressing, highlighting the key decision points and quality control checks.
The native extracellular matrix (ECM) is a dynamic, three-dimensional network of proteins and polysaccharides that provides not only structural support but also critical biochemical and mechanical signals that direct cellular behavior. Mimicking this complex environment represents a frontier in developing advanced therapies for wound healing, particularly for chronic wounds that fail to progress through normal healing phases. The ECM's composition is tissue-specific and undergoes constant remodeling through covalent and non-covalent interactions, creating impressive functions ranging from cellular signaling to structural integrity maintenance [9]. In chronic wounds, several pathophysiological mechanisms impede healing, including excessive ECM degradation by proteases, poor vascularization, decreased growth factor activity, and bacterial infection [4]. By creating biomaterials that replicate key aspects of the native ECM—architectural, mechanical, and bioactive properties—researchers can develop more effective wound treatments that actively promote regeneration rather than merely providing a passive covering.
The emergence of supramolecular biomaterials, particularly peptide-based systems that self-assemble into nanostructured environments, has created unprecedented opportunities for ECM mimicry. These materials can be designed "from scratch" with tunable properties, allowing precise control over their interaction with cellular components [9] [4]. When formulated as sprayable hydrogels incorporating peptide amphiphiles, these ECM-mimetic materials offer additional advantages for wound care, including conformal application to irregular wound beds, minimally invasive delivery, and the potential for in situ polymerization that enables on-demand gelation at target sites [10]. This application note details the principles, quantitative parameters, and experimental protocols for leveraging these advanced biomaterial platforms in wound healing research.
Quantitative Landscape of ECM-Mimetic Biomaterials
The design of biomaterials that mimic the native ECM requires careful consideration of architectural, mechanical, and biological parameters. The following tables summarize key quantitative data for major biomaterial classes used in ECM mimicry for wound healing applications.
Table 1: Architectural and Mechanical Properties of ECM-Mimetic Biomaterials
| Biomaterial Class | Fiber Diameter/Structure | Elastic Modulus/Stiffness | Porosity | Degradation Profile |
|---|---|---|---|---|
| Electrospun Nanofibers (Polysaccharide-based) [11] | 50-500 nm (mimicking natural ECM fibers) | Varies with polymer blend (e.g., Sol/SPI/Mp: 3.61 ± 0.29 MPa tensile strength) | High porosity (>80% reported for Sol/SPI systems) | Sol/SPI/Mp: 33.73 ± 3.55% degradation in 5 days in vitro |
| Peptide Amphiphile (PA) Nanofibers [12] [4] | 5-10 nm diameter, μm length (β-sheet nanofibers) | Tunable via peptide sequence; RGDS-PA gels showed significant healing enhancement | Nanofibrous hydrogel with high water content | Proteolytically degradable; sequence-dependent rates |
| Self-Assembled Peptides (SAPs) [4] | β-sheet nanofibers (e.g., RADA16-I: ~10 nm) | Tunable mechanics via concentration (e.g., FF hydrogels) | Nanoscale mesh with hydrogel properties | Susceptible to protease degradation; can be crosslinked |
| Supramolecular Hydrogels [9] | Hierarchical structures from self-assembly | Viscoelastic; can mimic tissue-specific mechanics (1.9 kPa lungs to 20 GPa bone) | Hydrated network permeable to nutrients/cells | Dynamic/reversible bonds enable remodeling |
Table 2: Functional Performance Metrics of ECM-Mimetic Wound Dressings
| Biomaterial System | Antimicrobial Efficacy | Wound Closure Rate | Cellular Response | Key Bioactive Components |
|---|---|---|---|---|
| AMP-Loaded Dressings [13] | Broad-spectrum activity; anti-biofilm properties | Enhanced re-epithelialization in chronic wounds | Stimulates cell proliferation, angiogenesis, immunomodulation | Antimicrobial peptides (e.g., LL-37, defensins) |
| Sol/SPI/Mp Nanofibers [14] | 93.06% S. aureus, 90.40% E. coli kill rate | Fastest re-epithelialization in rat model | Notable HaCat keratinocyte biocompatibility | Mupirocin, soy protein isolate, Soluplus |
| RGDS-PA Nanofiber Gels [12] | Not specifically reported | Significantly enhanced re-epithelialization days 7-28 in burns | Increased proliferation of thermally damaged fibroblasts and HUVECs | RGDS (Arg-Gly-Asp-Ser) peptide sequence |
| Chitosan-based Nanofibers [11] | Broad antibacterial (S. aureus, E. coli) via NH3+ interaction | Accelerated wound healing in various models | Promotes cell adhesion and proliferation | Chitosan (cationic polysaccharide) |
Experimental Protocols for ECM-Mimetic Biomaterial Evaluation
Protocol: Fabrication of Electrospun Nanofibrous Dressings
Principle: Electrospinning uses high-voltage electric fields to produce continuous polymer nanofibers that architecturally mimic the native ECM, creating high surface area-to-volume ratio scaffolds ideal for cell adhesion and bioactive factor delivery [11] [14].
Materials:
- Polymer solution (e.g., Soluplus, soy protein isolate, peptide amphiphiles)
- High-voltage power supply (0-30 kV capability)
- Syringe pump with flow rate control
- Collector plate (stationary or rotating)
- Solvent system appropriate for polymers
Procedure:
- Prepare polymer solution at optimal concentration (e.g., 33% w/v Soluplus in distilled water, 10% w/v SPI) with stirring for homogeneous dissolution [14].
- For drug-loaded systems, incorporate bioactive agents (e.g., 2% w/w mupirocin) into polymer solution with continuous stirring.
- Load solution into syringe with metallic needle (0.6 mm diameter typical).
- Set syringe pump to controlled flow rate (e.g., 1 mL/h).
- Apply high voltage (e.g., 15 kV) between needle and collector.
- Maintain fixed distance (e.g., 12 cm) between needle and collector.
- Collect nanofibers on aluminum foil or other substrate.
- Characterize fiber morphology by SEM, diameter distribution by ImageJ analysis.
Technical Notes:
- Solution parameters (viscosity, conductivity, surface tension) critically influence fiber morphology [11].
- Environmental parameters (temperature, humidity) must be controlled for reproducibility.
- Coaxial electrospinning can be employed for core-shell structures protecting bioactive components [11].
Protocol: Functional Characterization of Wound Dressings
Principle: Comprehensive evaluation of physical, mechanical, and biological properties predicts in vivo performance and ensures biomaterials meet requirements for wound healing applications [14].
Mechanical Testing:
- Cut nanofiber mats into standardized specimens (e.g., 10×50 mm strips).
- Perform tensile testing using universal testing machine.
- Calculate ultimate tensile strength, elastic modulus, and elongation at break from stress-strain curves.
Water Absorption and Permeability:
- Weigh dry nanofiber samples (20×20 mm).
- Immerse in distilled water for 24 hours.
- Remove, blot excess surface water, and reweigh.
- Calculate water absorption percentage: [(Wwet - Wdry)/Wdry] × 100.
- For water vapor permeability, use gravimetric method: measure weight loss of water-filled cup covered with nanofiber membrane over 24 hours.
In Vitro Degradation:
- Weigh initial dry samples (Winitial).
- Immerse in phosphate-buffered saline (PBS) or simulated wound fluid at 37°C.
- At predetermined time points, remove samples, dry completely, and reweigh (Wfinal).
- Calculate degradation percentage: [(Winitial - Wfinal)/Winitial] × 100.
Antibacterial Assessment:
- Prepare bacterial suspensions (S. aureus, E. coli) at ~10⁶ CFU/mL in nutrient broth.
- Incubate with nanofiber samples for 24 hours at 37°C.
- Plate serial dilutions on agar plates.
- Count colonies after 24 hours incubation.
- Calculate bacterial reduction percentage compared to control.
Protocol: In Vivo Evaluation of Wound Healing Efficacy
Principle: Animal models provide critical assessment of biomaterial performance in complex biological environments, measuring re-epithelialization, tissue regeneration, and immune response [12] [14].
Materials:
- Animal model (e.g., rat, mouse)
- Burn/wound creation apparatus
- Test biomaterials (nanofiber dressings, hydrogels)
- Histological supplies (fixatives, stains, embedding materials)
Procedure:
- Anesthetize animals according to approved protocol.
- Create standardized wounds (e.g., deep partial-thickness burns, excisional wounds).
- Apply test biomaterials to wound beds.
- Use appropriate controls (no treatment, commercial dressings).
- Monitor wound closure through regular imaging and planimetric analysis.
- Harvest tissue samples at predetermined endpoints (e.g., days 7, 14, 21, 28).
- Process samples for histology (H&E staining, Masson's trichrome for collagen).
- Evaluate re-epithelialization, granulation tissue formation, collagen deposition, and immune cell infiltration.
Technical Notes:
- RGDS-PA nanofiber gels showed significant enhancement of re-epithelialization between days 7-28 in burn wounds [12].
- Sol/SPI/Mp nanofibers demonstrated the fastest re-epithelialization and wound healing in rat models [14].
- Chronic wound models (diabetic, ischemic) provide more clinically relevant assessment for pathological healing impairment.
Signaling Pathways in ECM-Biomaterial Interactions
The interaction between cells and ECM-mimetic biomaterials occurs through specific receptor-mediated signaling pathways that direct cellular responses critical for wound healing. The integrin receptor family serves as a primary mediator of cell-biomaterial interactions, initiating signaling cascades that influence cell adhesion, migration, proliferation, and differentiation [9].
Diagram Title: ECM-Biomaterial Signaling in Wound Healing
The diagram illustrates how ECM-mimetic biomaterials, particularly those containing bioactive motifs like RGDS, activate integrin receptors that trigger intracellular signaling cascades through focal adhesion kinase (FAK). This initiation leads to two primary pathways: the Ras-MAPK pathway driving cell proliferation, and the PI3K-Akt pathway promoting cell survival and angiogenesis. Concurrently, integrin activation facilitates cytoskeleton reorganization, enabling cell migration critical for re-epithelialization. These coordinated cellular responses collectively contribute to enhanced wound healing outcomes observed with peptide amphiphile nanofibers and other ECM-mimetic biomaterials [12] [9].
Self-Assembly Mechanisms of Peptide-Based Biomaterials
Peptide amphiphiles and self-assembling peptides form nanostructured biomaterials through well-defined molecular mechanisms that create ECM-mimetic architectures. Understanding these assembly pathways is essential for rational design of sprayable wound healing formulations.
Diagram Title: Peptide Amphiphile Self-Assembly Pathway
The self-assembly process begins with peptide amphiphile monomers containing four distinct domains: a bioactive domain for receptor binding, a polar domain for aqueous solubility, a stabilization domain (typically β-sheet forming), and a hydrophobic tail. Upon environmental triggers such as pH change, salt concentration, or temperature adjustment, these monomers undergo molecular self-assembly through non-covalent interactions including hydrogen bonding, van der Waals forces, hydrophobic interactions, and π-π stacking. This process yields cylindrical β-sheet nanofibers with diameters of 5-10 nm, which subsequently entangle to form nanofibrous hydrogels with viscoelastic properties, topography, and bioactive signaling reminiscent of native ECM [4]. The resulting three-dimensional structure is easily tunable by modifying the amino acid sequence, allowing precise control over mechanical and biological properties for specific wound healing applications.
Research Reagent Solutions for ECM-Mimetic Wound Healing Studies
Table 3: Essential Research Reagents for ECM-Mimetic Biomaterial Development
| Reagent/Category | Function/Application | Representative Examples | Key Characteristics |
|---|---|---|---|
| Peptide Amphiphiles (PAs) | Self-assembling nanofiber formation | RGDS-PA, RADA16-I, RADA16-II, EAK16-II | Four-domain structure: bioactive, polar, stabilization, hydrophobic; β-sheet formation [12] [4] |
| Structural Polymers | Electrospinning matrix materials | Chitosan, Soluplus, Soy Protein Isolate (SPI), Polyvinyl alcohol (PVA) | Biocompatibility, tunable mechanics, processing versatility [11] [14] |
| Antimicrobial Agents | Infection control in wound dressings | Mupirocin, antimicrobial peptides (LL-37, defensins) | Broad-spectrum activity, low resistance propensity, biofilm disruption [13] [14] |
| Bioactive Motifs | Cellular recognition and signaling | RGDS (Arg-Gly-Asp-Ser), IKVAV, YIGSR | Integrin-binding domains, promotion of cell adhesion and migration [12] [9] |
| Crosslinking Agents | Modifying mechanical stability and degradation | Physical (temperature, pH), chemical (genipin, glutaraldehyde) | Control of structural integrity, tunable degradation rates [10] |
| Characterization Tools | Material property assessment | SEM, FTIR, tensile testing, BET surface area analysis | Verification of nanostructure, chemistry, mechanics, porosity [14] |
The research reagents outlined in Table 3 represent core components for developing and evaluating ECM-mimetic biomaterials for wound healing. Peptide amphiphiles serve as fundamental building blocks for self-assembling systems, with RGDS-modified PAs demonstrating significant enhancement of re-epithelialization in burn wound models [12]. Structural polymers like chitosan and Soluplus/SPI blends provide the macromolecular framework for electrospun nanofibers, offering both processability and bioactivity. Antimicrobial agents address the critical concern of infection in chronic wounds, with AMP-loaded dressings providing broad-spectrum activity and anti-biofilm properties while mitigating resistance development [13]. Incorporating bioactive motifs such as RGDS enables specific integrin-mediated cellular interactions that direct healing processes, while crosslinking agents allow fine-tuning of mechanical properties and degradation kinetics to match specific wound requirements. Comprehensive characterization using the outlined tools ensures reproducible fabrication and predictable in vivo performance.
The design of advanced biomaterials for wound healing is increasingly focused on mimicking the native extracellular matrix (ECM) to direct specific cellular responses. Within this framework, short bioactive peptide sequences derived from full-length ECM proteins have emerged as powerful tools for functionalizing synthetic materials. The RGDS (Arg-Gly-Asp-Ser) and IKVAV (Ile-Lys-Val-Ala-Val) epitopes are two of the most prominent and well-studied sequences, each playing a unique and critical role in cellular signaling, adhesion, and differentiation [15] [16]. Their integration into sprayable peptide amphiphile nanofiber systems presents a promising strategy for creating proactive wound dressings that not only provide a scaffold but also actively instruct the local cellular environment to promote healing. This application note details the molecular mechanisms, quantitative bioactivity, and experimental protocols for utilizing these epitopes in wound healing research.
Molecular Mechanisms and Signaling Pathways
RGDS: The Master Integrin Binder
The RGDS sequence is a canonical recognition motif found in numerous ECM proteins, including fibronectin, vitronectin, and fibrinogen [17] [18]. Its primary function is to serve as a ligand for the integrin family of cell surface receptors.
- Integin Binding: RGDS binds to a subset of integrins, including α5β1, αvβ3, and αIIbβ3 [17] [19]. This interaction is a cornerstone of cell-ECM adhesion.
- Outside-In Signaling: Ligand binding induces integrin clustering and the formation of focal adhesion complexes, initiating crucial downstream signaling pathways such as FAK (Focal Adhesion Kinase) and Src kinase activation [17]. This signaling cascades to influence cell survival, proliferation, and migration—all vital processes in wound healing.
- Role in Healing: In the context of wounds, RGDS promotes the attachment and spreading of fibroblasts and keratinocytes, facilitates angiogenesis by supporting endothelial cell function, and enhances the deposition of new ECM [15] [19].
The following diagram illustrates the key signaling pathway triggered by RGDS-integrin interaction:
IKVAV: A Multifunctional Laminin Epitope
The IKVAV sequence is derived from the α1-chain of laminin-1, a major component of the basement membrane [16]. Its bioactivity extends beyond simple adhesion to encompass potent modulation of cell behavior.
- Integrin Interaction: IKVAV is known to interact with integrin receptors, with recent research pointing to a role for α2β1 integrin in mediating its effects on certain cell types, including macrophages [16].
- Cellular Differentiation: A key function of IKVAV is the promotion of neurite outgrowth and the differentiation of neural stem/progenitor cells [20]. This makes it highly relevant for nerve regeneration within wound beds.
- Immunomodulation: Emerging evidence indicates that IKVAV can modulate macrophage phenotype, reducing pro-inflammatory (M1) markers and promoting anti-inflammatory (M2) markers, thereby potentially resolving chronic inflammation [16].
- Angiogenic Potential: IKVAV also exhibits pro-angiogenic abilities, supporting the formation of new blood vessels [16] [20].
The multifaceted cellular responses to the IKVAV peptide are summarized below:
Quantitative Bioactivity and Performance Data
The efficacy of RGDS and IKVAV is concentration-dependent and influenced by their presentation format. The data below summarizes key quantitative findings from recent literature.
Table 1: Quantitative Bioactivity Profile of RGDS and IKVAV Peptides
| Peptide Epitope | Cellular Assay / Model | Key Quantitative Outcome | Optimal Concentration / Density | Reference |
|---|---|---|---|---|
| RGDS | Mesenchymal stem cell adhesion on hydroxyapatite | Enhanced initial cell attachment; higher densities can inhibit bone formation in vivo when competing with adsorbed serum proteins. | Controlled density is critical; low densities enhance attachment. | [21] |
| RGDS | Fibroblast and keratinocyte adhesion in wound matrices | Promotes attachment, spreading, and proliferation of skin cells crucial for re-epithelialization. | Varies by material system; often used in 0.1-2.0 mM range for functionalization. | [15] [19] |
| IKVAV | Murine macrophage (M1) culture in 2D | Reduced iNOS expression from 82.13 ± 23.97 a.u. to 50.95 ± 7.3 a.u.; increased Arg-1 expression in M0 macrophages. | 3 mM (soluble treatment). | [16] |
| IKVAV | Neurogenic PC-12 cell culture | Concentration-dependent effects on proliferation and morphological differentiation. | Existence of an optimal-density range for peptide incorporation. | [20] |
| Cyclic RGD | Glioma-targeted drug delivery | Demonstrated ~1000x greater binding affinity for αvβ3 integrin compared to linear RGD. | N/A (affinity comparison). | [19] |
Experimental Protocols
Protocol 1: Functionalization of Biomaterials with RGDS and IKVAV
This protocol describes a method for covalently incorporating peptide epitopes into a gelatin-based cryogel or hydrogel, adaptable for sprayable nanofiber systems.
- Principle: Peptides are modified with terminal functional groups (e.g., lysine residues) to enable in-situ cross-linking during polymer network formation [20].
- Materials:
- Synthetic Peptides: K-RGDS-K and K-IKVAV-K (with N- and C-terminal lysines).
- Polymer Matrix: Gelatin methacryloyl (GelMA) or other cross-linkable biopolymer.
- Cross-linker: Glutaraldehyde or a photo-initiator (e.g., Irgacure 2959 for UV cross-linking).
- Procedure:
- Peptide Synthesis: Synthesize and purify K-RGDS-K and K-IKVAV-K peptides using standard Fmoc solid-phase peptide synthesis. Confirm structure via HPLC and mass spectrometry [20].
- Precursor Solution Preparation: Dissolve the GelMA polymer (e.g., 5-10% w/v) in PBS. Separately, dissolve the modified peptides in PBS.
- Mixing and Cross-linking: Combine the GelMA solution with the peptide solution at the desired molar ratio. Add cross-linker (e.g., 0.25% v/v glutaraldehyde for chemical cross-linking) or photo-initiator (0.5% w/v for UV cross-linking). Mix thoroughly.
- Cryogel Formation (Optional): For cryogels, pour the mixture into a mold and freeze at -16°C for 16 hours, then thaw at room temperature [20].
- Hydrogel Formation: For hydrogels, expose the mixture to UV light (e.g., 365 nm, 5-10 mW/cm² for 2-5 minutes) to initiate cross-linking.
- Washing: Wash the resulting functionalized gel extensively in sterile PBS or deionized water to remove unreacted species.
Protocol 2: In Vitro Assessment of Macrophage Immunomodulation
This protocol is used to evaluate the effect of IKVAV on macrophage polarization, a key process in regulating wound inflammation.
- Principle: Soluble IKVAV peptide is applied to macrophages stimulated towards a pro-inflammatory (M1) phenotype, and changes in phenotypic markers are quantified [16].
- Materials:
- Cells: Murine macrophage cell line (e.g., RAW 264.7) or primary bone marrow-derived macrophages.
- IKVAV Peptide: Soluble IKVAV peptide stock solution (e.g., 30 mM in PBS).
- Inducers: Lipopolysaccharide (LPS, 100 ng/mL) and Interferon-gamma (IFN-γ, 20 ng/mL) for M1 polarization.
- Procedure:
- Cell Seeding: Seed macrophages in 24-well plates at a density of 2 x 10^5 cells per well and allow to adhere overnight.
- Treatment: Pre-treat cells with 3 mM IKVAV peptide for 1 hour.
- Polarization: Stimulate macrophages with LPS/IFN-γ in the continued presence of IKVAV for 18-24 hours to induce M1 polarization.
- Analysis:
- Immunocytochemistry: Fix cells and stain for M1 marker (iNOS) and M2 marker (Arg-1). Quantify mean fluorescence intensity.
- Gene Expression: Extract RNA, perform reverse transcription, and analyze expression of pro-inflammatory (e.g., TNF-α, IL-6) and anti-inflammatory (e.g., IL-10, Arg-1) genes via qPCR [16].
The workflow for this immunomodulation assay is outlined below:
Integration into Sprayable Peptide Amphiphile Nanofibers
For wound healing applications, the RGDS and IKVAV epitopes can be engineered into the design of peptide amphiphile (PA) molecules. These PAs self-assemble in physiological conditions to form nanofibers that display a high density of bioactive signals at the surface.
- Molecular Design: The PA molecule typically includes a hydrophobic tail, a β-sheet forming sequence, and the bioactive epitope (RGDS or IKVAV) at the N-terminus.
- Sprayable Formulation: The PAs can be formulated as a solution in a sterile, biocompatible buffer (e.g., PBS or sucrose solution). Upon spray application to the wound bed, which often involves a change in ionic strength or pH, the PAs spontaneously self-assemble into a nanofiber network that forms a hydrogel in situ, creating a protective, bioactive barrier [15] [22].
- Functional Synergy: A co-assembling system containing both RGDS-PA and IKVAV-PA can be created. This allows for a single sprayable dressing that simultaneously promotes cell adhesion and migration (via RGDS) while modulating inflammation and encouraging neurite ingrowth (via IKVAV), addressing multiple aspects of the healing process concurrently.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Working with RGDS and IKVAV Epitopes
| Reagent / Material | Function and Application | Example Use Case |
|---|---|---|
| Linear RGDS Peptide | Promotes general cell adhesion and spreading via integrin binding. Functionalization of 2D surfaces for cell culture or simple hydrogel systems. | Studying fibroblast migration in a 2D wound healing assay. |
| Cyclic RGDfK Peptide | Offers superior stability and binding affinity to αvβ3 integrin; used for targeted delivery and potent angiogenesis inhibition. | Targeting therapeutic nanoparticles to angiogenic endothelial cells in wounds. |
| K-IKVAV-K Peptide | Modified peptide with terminal lysines for efficient covalent cross-linking into polymer matrices during fabrication. | Creating stable, IKVAV-functionalized cryogels for neural tissue engineering [20]. |
| Gelatin Methacryloyl (GelMA) | A photocrosslinkable, tunable hydrogel backbone that mimics the natural ECM. | Forming sprayable, UV-curable hydrogels for wound dressing. |
| Poly-ε-Caprolactone (PCL) | A biodegradable synthetic polymer providing mechanical strength; often used as a conduit or shell. | Fabricating a supportive outer tube for a nerve guidance conduit [20]. |
| Irgacure 2959 | A cytocompatible photo-initiator for UV-induced cross-linking of hydrogels. | Cross-linking GelMA-based sprayable formulations upon application to a wound. |
The clinical management of chronic wounds, such as diabetic foot ulcers and venous leg ulcers, presents a substantial global healthcare challenge, with an estimated prevalence of between 1.47 and 2.2 per 1,000 population [10]. For researchers developing advanced therapeutic solutions like sprayable peptide amphiphile (PA) nanofibers, two fundamental properties dictate translational success: biocompatibility and biodegradability. These inherent characteristics ensure that a biomaterial can perform its function without eliciting adverse host responses while harmoniously supporting the body's natural healing processes.
Peptide amphiphiles are a class of molecules specifically engineered to address these requirements. Their typical molecular architecture includes: (1) a hydrophobic alkyl tail, (2) a β-sheet forming peptide sequence that promotes self-assembly, (3) charged amino acids for solubility, and (4) a bioactive peptide epitope at the terminus for cell signaling [3]. This precise molecular design enables PAs to spontaneously assemble in physiological conditions into supramolecular nanofibers that closely mimic the native extracellular matrix (ECM) [23] [24], creating a bioactive scaffold ideal for wound healing applications.
This document provides detailed application notes and standardized protocols to assist researchers in quantifying, validating, and applying these critical properties in the development of PA-based wound healing technologies.
Molecular Design Rationale for Biocompatibility and Biodegradability
The inherent biocompatibility of PAs stems from their peptide-based composition. As these molecules are constructed from natural amino acids, they present a familiar biochemical interface to cells, promoting favorable cellular interactions while minimizing cytotoxicity and inflammatory responses [23]. The presentation of bioactive signals, such as the RGDS (Arg-Gly-Asp-Ser) epitope derived from fibronectin, further enhances biocompatibility by promoting specific integrin-mediated cell adhesion—a crucial process during wound healing [3].
Biodegradability is engineered into PA molecules through the incorporation of peptide bonds susceptible to hydrolysis or enzymatic cleavage by proteases present in the wound environment [23]. This ensures that the nanofibrous scaffold undergoes controlled resorption, gradually making way for newly formed natural tissue without requiring surgical removal. The degradation rate can be tuned by modifying the peptide sequence, with more labile amino acid sequences resulting in faster breakdown [24].
Table 1: Key Molecular Components of Peptide Amphiphiles and Their Functional Roles
| Molecular Component | Chemical Features | Primary Function | Impact on Biocompatibility/Biodegradability |
|---|---|---|---|
| Hydrophobic Tail | Alkyl chain (e.g., palmitic acid) | Drives self-assembly via hydrophobic collapse; forms core of nanofiber [3] | Affects interaction with cell membranes; longer chains can slow degradation [25] |
| β-Sheet Forming Sequence | Short peptide (e.g., VVVAAA) | Enables hydrogen bonding; dictates one-dimensional nanofiber growth [3] [23] | Stable yet dynamic structure; bonds are susceptible to enzymatic cleavage [23] |
| Charged Amino Acids | Ionizable residues (e.g., glutamic acid, lysine) | Provides aqueous solubility; enables salt-responsive gelation [3] | Electrostatic interactions can influence protein adsorption and cell behavior [23] |
| Bioactive Epitope | Short signaling sequence (e.g., RGDS, IKVAV) | Confers specific bioactivity (e.g., cell adhesion, differentiation) [3] | Directly mediates cell-scaffold communication, crucial for biocompatibility [3] [23] |
Diagram 1: PA Design Principles for Wound Healing
Quantitative Assessment of Material Properties
Rigorous in vitro characterization is essential to validate the performance of PA nanofibers before proceeding to complex animal models or clinical studies. The following tables summarize key parameters and methods for evaluating the core properties of PA-based hydrogels and nanofibers.
Table 2: Key Parameters for Assessing Biocompatibility of PA Nanofibers
| Assessment Method | Measured Parameters | Typical Target/Outcome for PAs | Relevant Standard |
|---|---|---|---|
| MTT/XTT Assay | Cell viability (%) , Metabolic activity | >90% viability relative to control [26] [14] | ISO 10993-5 |
| Live/Dead Staining | Ratio of live to dead cells, Cell morphology | High density of live cells, normal morphology | ISO 10993-5 |
| Hemolysis Assay | Hemoglobin release (%) | <5% hemolysis [14] | ASTM F756 |
| Cytokine ELISA | Inflammatory cytokine levels (e.g., TNF-α, IL-6) | Significant reduction vs. negative control | N/A |
| Direct Contact Assay | Cell morphology, Lysis, Growth inhibition | Grade 0 (no reactivity) or Grade 1 (slight reactivity) | ISO 10993-5 |
Table 3: Key Parameters for Assessing Biodegradability of PA Nanofibers
| Assessment Method | Measured Parameters | Degradation Influencing Factors | Data Interpretation |
|---|---|---|---|
| Mass Loss Measurement | Remaining mass (%) over time | Peptide sequence, Crosslinking density, Protease concentration | Degradation profile should match tissue ingrowth rate [23] |
| Gel Permeation Chromatography (GPC) | Molecular weight change, Dispersity | Cleavage of peptide bonds, Fragment solubility | Shift to lower molecular weights indicates breakdown |
| Rheology | Storage (G') and Loss (G'') moduli | Network integrity, Fiber disassembly | Drop in G' indicates loss of mechanical structure |
| HPLC/MS Analysis | Degradation product identification | Enzyme specificity, Environmental pH | Identifies non-toxic degradation products (amino acids) [23] |
| Scanning Electron Microscopy (SEM) | Nanofiber morphology, Pore size, Surface erosion | Self-assembly stability, Solubility of segments | Visual confirmation of structural disintegration |
Experimental Protocols
Protocol: Synthesis and Purification of Peptide Amphiphiles
This protocol describes the solid-phase peptide synthesis (SPPS) of a model PA, C16-VVVAAAGGRGDS, incorporating a hydrophobic tail, a β-sheet domain, and a bioactive RGDS sequence [3] [26].
Research Reagent Solutions:
- Resin: Rink Amide resin (loading: 0.5 mmol/g)
- Amino Acids: Fmoc-protected amino acids: Fmoc-Ser(tBu)-OH, Fmoc-Asp(OtBu)-OH, Fmoc-Gly-OH, Fmoc-Arg(Pbf)-OH, Fmoc-Ala-OH, Fmoc-Val-OH
- Solvents: Dimethylformamide (DMF), Dichloromethane (DCM), Diethyl ether
- Reagents for Coupling: 2-(1H-Benzotriazol-1-yl)-1,1,3,3-tetramethyluronium hexafluorophosphate (HBTU), N,N-Diisopropylethylamine (DIEA)
- Deprotection Reagent: 20% (v/v) Piperidine in DMF
- Cleavage Cocktail: 95:2.5:2.5 Trifluoroacetic Acid (TFA) : Triisopropylsilane : Water
- Lipid Conjugation: Palmitic acid
Methodology:
Resin Preparation: Place 1.0 g of Rink Amide resin (0.5 mmol) into a solid-phase reaction vessel. Swell the resin in 10 mL DCM for 30 minutes, then drain. Perform Fmoc deprotection by treating the resin with 10 mL of 20% piperidine/DMF solution for 2 x 10 minutes with gentle agitation. Drain and wash the resin thoroughly with DMF (5 x 10 mL).
Peptide Chain Elongation:
- For each amino acid in the sequence (from C-terminal to N-terminal, starting with Ser), perform the following coupling cycle:
- Coupling: Prepare a solution of 4 equivalents of the Fmoc-amino acid, 3.95 equivalents of HBTU, and 6 equivalents of DIEA in 10 mL DMF. Add this solution to the resin and agitate for 45-60 minutes. Drain and wash with DMF (3 x 5 mL).
- Deprotection: Add 10 mL of 20% piperidine/DMF to remove the Fmoc group, agitate for 2 x 10 minutes. Drain and wash with DMF (3 x 5 mL).
- Monitor coupling completion using the Kaiser test.
- After coupling the final N-terminal amino acid (Val), conjugate palmitic acid using the same coupling protocol.
Cleavage and Deprotection: Drain the resin and wash sequentially with DMF, DCM, and methanol. Transfer the resin to a clean vessel and add 10 mL of the TFA-based cleavage cocktail. Agitate the mixture for 3 hours at room temperature. Filter the solution to separate the cleaved peptide from the resin, collecting the filtrate.
Precipitation and Purification: Precipitate the crude PA by slowly adding the TFA filtrate into 50 mL of cold diethyl ether in a centrifuge tube. Centrifuge at 4000 rpm for 10 minutes at 4°C to pellet the product. Decant the supernatant and wash the pellet with fresh cold ether. Repeat the centrifugation and washing steps twice.
- Dissolve the crude pellet in water and lyophilize to obtain a white powder.
- Purify the PA using reversed-phase High-Performance Liquid Chromatography (HPLC). Confirm the molecular weight and purity using Mass Spectrometry (MS) and analytical HPLC [26].
Diagram 2: PA Synthesis Workflow
Protocol: In Vitro Biocompatibility and Cytotoxicity Assessment (MTT Assay)
This protocol assesses the cytotoxicity of PA nanofiber degradation products on human dermal fibroblasts (HDFs) according to ISO 10993-5 standards [26] [14].
Research Reagent Solutions:
- Cells: Human Dermal Fibroblasts (HDFs)
- Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS) and 1% Penicillin-Streptomycin.
- Test Material: PA nanofibers (sterilized under UV light for 30 minutes).
- Extraction Medium: Serum-free DMEM.
- MTT Reagent: 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide, prepared as 5 mg/mL stock in PBS.
- Solubilization Solution: Dimethyl Sulfoxide (DMSO).
Methodology:
Preparation of Extracts:
- Sterilize 100 mg of PA nanofibers and place them in 5 mL of extraction medium (resulting in a 20 mg/mL concentration).
- Incubate the mixture at 37°C for 24 hours under gentle agitation.
- After incubation, centrifuge the solution at 10,000 rpm for 10 minutes and collect the supernatant (the extract). Prepare serial dilutions of this extract in complete culture medium (e.g., 10 mg/mL, 5 mg/mL, 1 mg/mL).
Cell Seeding and Treatment:
- Harvest HDFs and seed them in a 96-well plate at a density of 1 x 10⁴ cells per well in 100 μL of complete medium.
- Incubate the plate for 24 hours at 37°C in a 5% CO₂ atmosphere to allow cell attachment.
- Carefully aspirate the medium from the wells and replace it with 100 μL of the various extract dilutions. Include control wells containing only complete medium (negative control) and wells with 1% Triton X-100 (positive control). Use at least 5 replicates per condition.
MTT Incubation and Measurement:
- After a 24-hour exposure period, carefully remove the treatment media.
- Add 100 μL of fresh serum-free medium containing 10% (v/v) of the MTT stock solution (final MTT concentration: 0.5 mg/mL) to each well.
- Incubate the plate for 4 hours at 37°C.
- Carefully remove the MTT solution and add 100 μL of DMSO to each well to dissolve the formed formazan crystals.
- Agitate the plate on an orbital shaker for 10 minutes to ensure complete dissolution.
- Measure the absorbance of each well at a wavelength of 570 nm, using a microplate reader.
Data Analysis:
- Calculate the percentage of cell viability for each test group using the formula:
Cell Viability (%) = (Mean Absorbance of Test Group / Mean Absorbance of Negative Control) x 100 - A material is generally considered non-cytotoxic if cell viability exceeds 90% relative to the negative control [26] [14].
- Calculate the percentage of cell viability for each test group using the formula:
Protocol: Enzymatic Biodegradation Profiling
This protocol monitors the mass loss of PA nanofiber hydrogels over time in the presence of collagenase, a protease relevant to the wound environment [23].
Research Reagent Solutions:
- Hydrogel Preparation: 1.0% (w/v) PA solution in PBS, gelled by adjusting pH or adding physiological salts.
- Enzyme Solution: Collagenase Type I, dissolved in PBS containing 1 mM CaCl₂, to a final activity of 50 U/mL.
- Control Buffer: PBS with 1 mM CaCl₂ (enzyme-free).
- Other: Phosphate Buffered Saline (PBS), Calcium Chloride (CaCl₂).
Methodology:
Hydrogel Preparation and Weighing:
- Prepare PA hydrogels in pre-weighed 1.5 mL microcentrifuge tubes (Wₜᵤᵦₑ). Allow the gels to set completely.
- Record the initial mass of the gel (Wᵢₙᵢₜᵢₐₗ) after removing any surface moisture.
Degradation Incubation:
- Carefully add 1.0 mL of the collagenase solution (50 U/mL) to the test gels. For control gels, add 1.0 mL of the control buffer.
- Incubate the tubes at 37°C under gentle agitation (50 rpm).
- Replace the enzyme solution and control buffer every 48 hours to maintain consistent enzyme activity.
Mass Loss Measurement:
- At predetermined time points (e.g., days 1, 3, 5, 7), carefully remove the incubation solution.
- Rinse the gels gently with distilled water to stop degradation and remove soluble degradation products.
- Blot the gels lightly with filter paper to remove excess surface water and record the wet mass (Wₜ).
- Lyophilize the gels until a constant dry mass is achieved (W𝒹).
Data Analysis:
- Calculate the percentage of remaining mass at each time point using both wet and dry mass measurements:
Remaining Mass (%) = (Wₜ / Wᵢₙᵢₜᵢₐₗ) x 100(for wet mass)Remaining Mass (%) = (W𝒹 / Wᵢₙᵢₜᵢₐₗ) x 100(for dry mass) - Plot the remaining mass (%) versus time to generate a degradation profile for the PA hydrogel. Compare the degradation rates between the enzyme-treated and control groups.
- Calculate the percentage of remaining mass at each time point using both wet and dry mass measurements:
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for PA Wound Healing Studies
| Reagent / Material | Supplier Examples | Critical Function | Application Notes |
|---|---|---|---|
| Fmoc-Protected Amino Acids | NovaBiochem, Sigma-Aldrich | Building blocks for SPPS; R groups define PA bioactivity [27] [26] | Store desiccated at -20°C; quality critical for synthesis yield |
| Rink Amide Resin | NovaBiochem | Solid support for SPPS; yields C-terminal amide upon cleavage | Swell thoroughly in DCM before use for optimal coupling |
| HBTU / HATU | Sigma-Aldrich | Peptide coupling reagents; activate carboxyl group of amino acids | Freshly prepare in DMF immediately before use |
| Collagenase Type I | Worthington, Sigma-Aldrich | Models enzymatic degradation in the wound environment [23] | Activity varies by batch; prepare stock solutions fresh |
| Human Dermal Fibroblasts (HDFs) | ATCC | In vitro model for dermal layer; primary cells are preferred for relevance | Use low passage numbers (<8) for consistent, reliable data |
| MTT Reagent | Thermo Fisher, Sigma-Aldrich | Tetrazolium salt; measures mitochondrial activity in viability assays [14] | Filter sterilize stock solution; protect from light during storage |
Concluding Remarks
The strategic molecular design of peptide amphiphiles inherently provides the biocompatibility and biodegradability essential for effective wound healing scaffolds. The protocols outlined herein for synthesis, biocompatibility testing, and degradation profiling provide a foundational framework for researchers. Future developments in this field will likely focus on creating increasingly sophisticated "smart" PA systems that dynamically respond to specific wound microenvironment cues, such as pH or enzyme profiles, to further optimize the healing process for chronic wounds.
From Synthesis to Bedside: Fabricating and Delivering Sprayable Nanofiber Therapies
Peptide amphiphiles (PAs) represent a class of biomolecules gaining significant traction in advanced wound healing therapies. These molecules are synthetically designed to combine a hydrophobic segment, typically an alkyl tail, with a hydrophilic peptide sequence, enabling them to self-assemble in aqueous environments into supramolecular nanofibers [3]. These nanofibers are exceptionally valuable for regenerative medicine as they can closely mimic the structure and function of the native extracellular matrix (ECM)—a crucial factor in guiding cellular behavior during tissue repair [3] [28].
The relevance of PA nanofibers to wound healing is multifaceted. They can be functionalized with bioactive epitopes, such as the laminin-derived IKVAV sequence for neural outgrowth or the ubiquitous RGDS cell-adhesion motif, to directly influence cellular processes like migration, proliferation, and angiogenesis [3] [29]. Furthermore, the viscoelastic properties of PA assemblies can be engineered to be shear-thinning, meaning they can be easily sprayed onto complex wound geometries as a low-viscosity liquid, after which they rapidly reassemble into a stable, gel-like scaffold that covers the injury [5]. This sprayable delivery method is minimally invasive and conforms perfectly to irregular wound beds, making it an ideal platform for treating conditions like deep dermal burns and diabetic ulcers [5] [22]. The synthesis of these sophisticated molecules, therefore, forms the foundational step in creating next-generation wound dressings.
Solid-Phase Peptide Synthesis (SPPS) of Peptide Amphiphiles
Solid-Phase Peptide Synthesis is the most established and widely used method for the laboratory-scale production of peptide amphiphiles. Its principle advantage lies in its simplicity and high efficiency, allowing for the rapid, sequential addition of protected amino acids to a growing peptide chain that is covalently anchored to an insoluble solid support [5]. This facilitates the easy removal of excess reagents and by-products through simple filtration and washing steps, enabling high reaction yields.
Molecular Design of a Model Wound-Healing PA
A typical PA designed for a pro-angiogenic wound-healing application, as characterized in the search results, can be broken down into four key regions [3]:
- Hydrophobic Tail: A long alkyl chain (e.g., derived from palmitic acid) that drives self-assembly via hydrophobic collapse.
- β-Sheet Forming Region: A short peptide sequence (e.g., VVVAAA) with a high propensity for intermolecular hydrogen bonding, promoting one-dimensional nanofiber growth.
- Charged Segment: Amino acids with ionizable side chains (e.g., glutamic acid, E) that provide water solubility and allow for gelation triggered by physiological electrolytes.
- Bioactive Epitope: A terminal peptide signal (e.g., RGDS) that interacts with cell surface receptors to promote specific therapeutic outcomes such as cell adhesion and angiogenesis [5] [29].
Table 1: Key Research Reagent Solutions for PA Synthesis and Characterization
| Reagent/Material | Function in Protocol |
|---|---|
| Fmoc-Protected Amino Acids | Building blocks for the peptide sequence; Fmoc group protects the α-amine during chain elongation. |
| Rink Amide Resin | A common solid support that yields a C-terminal amide upon cleavage, a common feature in PAs. |
| Palmitic Acid | Source of the hydrophobic alkyl tail; coupled to the N-terminus of the assembled peptide. |
| Nile Red | A fluorescent dye used in an assay to monitor the critical aggregation concentration and self-assembly of PAs [5]. |
| Tris(2-carboxyethyl)phosphine (TCEP) | A reducing agent used to characterize the cleavage of disulfide-based, glutathione-responsive linkers in drug-delivery PAs [30]. |
Detailed SPPS Protocol for a Pro-Angiogenic PA
The following protocol outlines the step-by-step synthesis of a model PA, C16-VVVAAAGGRGDS, using standard Fmoc-SPPS procedures [5].
Experiment Title: Fmoc-Solid Phase Synthesis of a Bioactive Peptide Amphiphile. Objective: To synthesize and cleave a peptide amphiphile from solid support, yielding a crude product for subsequent purification and self-assembly testing. Materials: Rink Amide MBHA resin, Fmoc-protected amino acids (Fmoc-Ser(tBu)-OH, Fmoc-Gly-OH, Fmoc-Asp(OtBu)-OH, Fmoc-Arg(Pbf)-OH, Fmoc-Ala-OH, Fmoc-Val-OH), Palmitic acid, Deprotection reagent (20% Piperidine in DMF), Coupling reagents (HBTU and HOAt in DMF), Activator base (N,N-Diisopropylethylamine, DIPEA), Cleavage cocktail (Trifluoroacetic acid, TFA, with triisopropylsilane and water as scavengers), DMF, DCM, Diethyl ether.
Workflow:
- Resin Swelling: Place the Rink Amide resin (0.1 mmol) in a solid-phase reaction vessel. Add 5 mL of DCM and gently agitate for 30 minutes to swell the resin matrix. Drain the DCM.
- Fmoc Deprotection (Cycle): Add 5 mL of 20% piperidine in DMF. Agitate the mixture for 5 minutes, then drain. Repeat this step for a second 5-minute treatment. Drain completely and wash the resin thoroughly with DMF (5 x 1 minute washes).
- Amino Acid Coupling (Cycle): For each amino acid in the sequence (from C-terminal to N-terminal): a. Prepare a coupling solution: 4 equivalents of Fmoc-amino acid, HBTU, and HOAt in DMF, activated with 8 equivalents of DIPEA. b. Add the solution to the reaction vessel and agitate for 45-60 minutes. c. Drain the coupling solution and wash the resin with DMF (3 x 1 minute washes). d. Perform a Kaiser test to confirm complete coupling. If the test is positive (indicating free amines), repeat the coupling step. e. Perform steps 2 and 3 to deprotect the newly coupled amino acid and begin the next cycle.
- Palmitic Acid Coupling: After the final Fmoc deprotection (of the N-terminal Valine), couple palmitic acid using the same coupling procedure described in step 3, using 4 equivalents of palmitic acid.
- Final Cleavage and Deprotection: a. Wash the resin with DCM (3 x 1 minute) and dry it in vacuo. b. Prepare a cold cleavage cocktail (TFA/Triisopropylsilane/Water, 95:2.5:2.5). c. Add the cleavage cocktail to the dried resin (∼10 mL per gram of resin) and agitate for 3 hours at room temperature. d. Filter the mixture to separate the resin from the cleaved PA solution. Wash the resin with a small amount of fresh TFA.
- Precipitation and Isolation: a. Combine the TFA filtrates and concentrate the volume under a stream of nitrogen or by rotary evaporation. b. Precipitate the crude PA by slowly dripping the concentrated TFA solution into 40 mL of cold diethyl ether in a 50 mL centrifuge tube. c. Cool the tube at -20°C for 30 minutes to complete precipitation. d. Centrifuge the tube at 4000 rpm for 10 minutes to pellet the PA. Decant the ether supernatant. e. Wash the pellet with fresh cold ether and re-centrifuge. Decant the ether and dry the pellet under a vacuum to yield the crude PA as a white solid.
Flow Chemistry for Peptide Synthesis
While SPPS is highly effective, flow chemistry presents a modern alternative with potential for improved control and scalability. In continuous flow synthesis, reagent solutions are pumped through a temperature-controlled reactor, as opposed to the batch-wise process of SPPS. This can lead to more efficient mixing, superior heat and mass transfer, and the ability to integrate multiple synthetic and purification steps in a single, automated system. Although not explicitly detailed in the wound-healing context of the search results, the principles of flow chemistry are highly applicable to peptide synthesis and can be leveraged for producing PAs with higher reproducibility and at a larger scale.
Analytical Characterization of Synthesized PAs
Rigorous characterization is essential to confirm the identity, purity, and self-assembling properties of the synthesized PA.
Table 2: Key Analytical Methods for Peptide Amphiphile Characterization
| Analytical Method | Measurable Parameters | Application in PA Development |
|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Molecular weight, Purity [5]. | Confirms the successful synthesis of the target PA and assesses crude product purity before purification. |
| Circular Dichroism (CD) | Secondary structure (e.g., β-sheet formation) [5]. | Monitors the internal ordering of PA molecules during assembly; a shift towards a β-sheet signature indicates successful nanofiber formation. |
| Transmission Electron Microscopy (TEM) | Nanofiber morphology, diameter, and length [5]. | Directly visualizes the supramolecular structure of the assembled PA nanofibers. |
| Rheology | Storage (G') and Loss (G'') moduli, viscoelasticity [5]. | Quantifies the mechanical strength and shear-thinning behavior of the PA hydrogel, critical for sprayability and scaffold stability. |
Detailed Protocol: Confirming Self-Assembly via Circular Dichroism (CD) Spectroscopy Objective: To characterize the secondary structure of the PA in solution and confirm β-sheet formation. Materials: Purified PA powder, Ultrapure water, Phosphate Buffered Saline (PBS), 0.1 M NaOH, 0.1 M HCl, CD spectrometer quartz cuvette (path length 0.1 cm or 1 mm). Workflow:
- Sample Preparation: Dissolve the PA in ultrapure water at a concentration of 0.1% (w/v) by gently vortexing. The solution may be sonicated in a cold water bath for 10 minutes to aid dissolution.
- Triggering Assembly: Add a calculated volume of 10X PBS to the PA solution to achieve a final 1X PBS concentration, thereby triggering self-assembly via charge screening. Gently mix and allow the solution to incubate at room temperature for 1 hour.
- CD Measurement: Load the assembled PA solution into a quartz cuvette. Acquire the CD spectrum at room temperature over a wavelength range of 190-260 nm.
- Data Analysis: A characteristic signature for β-sheet structure is a positive peak near 195 nm and a negative peak near 218 nm. Compare the spectrum of the assembled PA to that of the unassembled PA in pure water to confirm the structural transition.
Application Protocol: Forming and Testing Sprayable PA Gels
The ultimate test for a wound-healing PA is its functionality as a sprayable scaffold that supports cellular processes.
Detailed Protocol: Spray Delivery and Angiogenesis Assay Objective: To form a PA hydrogel via ionic crosslinking, assess its sprayability, and evaluate its pro-angiogenic potential. Materials: Sterile PA solution (1% w/v in water), Sterile CaCl₂ solution (100 mM in water), Spray device (e.g., dual-barrel syringe or airbrush), Human Umbilical Vein Endothelial Cells (HUVECs), Matrigel, Cell culture incubator. Workflow:
- Gelation and Spraying: a. Load the sterile PA solution into one syringe and the sterile CaCl₂ solution into a second syringe. b. Connect the syringes via a luer-lock connector or a spray head designed for mixing. c. Depress the plungers simultaneously to mix the PA and crosslinker upon ejection, resulting in the instantaneous formation of a gel that can be sprayed directly onto a surface (e.g., an in vitro wound model or a material for rheological testing) [5] [22].
- Endothelial Cell Tube Formation Assay: a. Thaw Matrigel on ice and pipet it into a pre-chilled 96-well plate. Allow it to polymerize for 30 minutes at 37°C. b. Prepare two test conditions: 1) PA nanofiber gel formed in cell culture medium, and 2) Control (medium only). c. Seed HUVECs onto the surface of the Matrigel and the test PA gel. d. Incubate the cells for 6-18 hours at 37°C and 5% CO₂. e. Image the cells using an inverted microscope. Quantify the total tube length, number of branch points, and number of meshes per field of view. A significant increase in these parameters in the PA gel condition indicates enhanced in vitro angiogenesis, a critical process for wound healing [5].
Pathway and Workflow Diagrams
The following diagrams summarize the key signaling pathways involved in wound healing and the experimental workflow for PA development.
Diagram 1: PAs in wound healing pathways. Peptide amphiphile nanofibers (red and green) positively influence the natural wound healing process by scavenging harmful ROS and presenting signals that enhance fibroblast activity.
Diagram 2: PA development workflow. The linear workflow for developing a sprayable PA wound therapy, from molecular design to functional testing.
Electrospinning and Alternative Methods for Nanofiber Production
Nanofibers have emerged as a pivotal component in advanced biomedical research due to their high surface area-to-volume ratio, porosity, and ability to mimic the native extracellular matrix (ECM) [31] [32]. These properties are particularly valuable in wound healing applications, where nanofibrous scaffolds can promote cell adhesion, proliferation, and migration [33]. For researchers focused on developing sprayable peptide amphiphile (PA) nanofibers for wound healing, understanding the fabrication landscape is essential for selecting appropriate manufacturing strategies. This document provides a comprehensive technical comparison of prominent nanofiber production methods, with emphasis on their applicability to wound healing research, particularly for creating advanced, functionalized wound dressings.
The two primary approaches for nanofiber fabrication are electrospinning (a fiber production method) and molecular self-assembly (a bottom-up synthetic approach). Electrospinning utilizes electrical forces to draw charged threads from polymer solutions, producing fibrous mats with diameters ranging from nanometers to several micrometers [34] [32]. In contrast, molecular self-assembly relies on supramolecular chemistry to create nanofibers through the spontaneous organization of molecules under specific thermodynamic conditions [3] [30]. For research involving sprayable PA nanofibers, both approaches offer distinct advantages: electrospinning provides robust structural scaffolds, while self-assembling PAs enable precise biochemical signaling and minimally invasive application.
Comparative Analysis of Nanofiber Fabrication Methods
Table 1: Technical Comparison of Primary Nanofiber Fabrication Methods
| Parameter | Electrospinning | Molecular Self-Assembly | Phase Separation | Template Synthesis |
|---|---|---|---|---|
| Fiber Diameter | 50 nm - 5 μm [33] [32] | 5 - 20 nm [3] [30] | 50 - 500 nm [31] | >50 nm [31] |
| Principal Driving Force | High-voltage electric field [34] [32] | Non-covalent interactions (hydrogen bonding, hydrophobic collapse, electrostatic) [3] | Thermodynamic parameters and solvent-non-solvent interactions [31] | Filtration through porous membrane [31] |
| Typical Materials | Synthetic/natural polymers (PVA, chitosan, PU) [34] [32] | Peptide amphiphiles, lipids, block copolymers [3] [30] | Biodegradable polymers (PLGA, PLLA) [31] | Various polymers, carbon nanotubes [31] |
| Porosity | High (inter-fiber), tunable [33] [32] | Molecularly defined, lower inter-fiber porosity [3] | High intra-fiber porosity [31] | Dependent on template [31] |
| Throughput & Scalability | High to industrial scale [34] | Moderate, limited by peptide synthesis [3] | Laboratory scale [31] | Laboratory scale [31] |
| Key Advantages for Wound Healing | ECM-mimetic structure, tunable mechanics, facile functionalization [33] [32] | Bioactive signaling, injectable/sprayable formats, responsive to physiological triggers [3] [30] | 3D scaffold formation, biocompatibility [31] | Control over diameter and length [31] |
| Primary Limitations | Solvent toxicity concerns, limited clinical translation of portable devices [34] [33] | Limited mechanical strength, complex characterization [3] [30] | Limited material choices, solvent residues [31] | Limited fiber length, complex setup [31] |
Detailed Experimental Protocols
Protocol: Electrospinning of Functionalized Nanofibers for Wound Dressings
This protocol details the production of bioactive nanofiber dressings via electrospinning, suitable for delivering therapeutic agents in wound healing models [34] [32] [35].
Materials:
- Polymer Solution: Medical-grade polyurethane (e.g., for Spincare) or blend of synthetic (PCL, PLGA) and natural (chitosan, gelatin) polymers [33] [32].
- Solvents: Hexafluoro-2-isopropanol (HFIP), Trifluoroethanol (TFE), or Acetic Acid (for chitosan) [32].
- Bioactive Compounds: Antimicrobial peptides (LL-37, defensins), growth factors (VEGF, FGF), or metal nanoparticles (silver, zinc oxide) [13] [32].
- Equipment: Electrospinning apparatus with high-voltage power supply (5-30 kV), syringe pump, grounded collector (static or rotating), and environmental control chamber [34] [33].
Procedure:
- Solution Preparation: Dissolve polymers at 8-15% (w/v) in appropriate solvent with stirring for 12 hours until homogeneous. For functionalization, incorporate bioactive compounds (typically 1-5% w/w relative to polymer) and mix gently to avoid denaturation [32].
- Parameter Optimization: Load solution into syringe. Systematically vary key parameters to achieve uniform fiber morphology without beads:
- Fiber Collection: Collect fibers on aluminum foil, mandrel, or directly on wound models. For portable clinical devices like Spincare, the collector is the wound bed itself [33].
- Post-Processing: Crosslink fibers if needed (e.g., glutaraldehyde vapor for gelatin-based fibers) to enhance stability in moist wound environments. Sterilize via UV irradiation or ethylene oxide gas [32] [35].
Applications in Wound Healing: Electrospun dressings create a physical barrier against infection while maintaining moisture balance. Functionalized fibers enable controlled release of antimicrobials to combat biofilms or growth factors to stimulate angiogenesis and re-epithelialization [13] [32].
Protocol: Self-Assembly of Bioactive Peptide Amphiphile Nanofibers
This protocol describes the synthesis and self-assembly of peptide amphiphiles (PAs) designed to form supramolecular nanofibers for targeted therapeutic delivery in wound healing [3] [30].
Materials:
- Peptide Amphiphiles: Synthesized via standard Fmoc solid-phase peptide synthesis, incorporating:
- Alkyl tail (e.g., palmitic acid) for hydrophobic collapse
- β-sheet forming sequence (e.g., VVVAAA)
- Charged amino acids (e.g., EEE) for solubility
- Bioactive epitope (e.g., RGDS, IKVAV) [3]
- Triggering Agents: Phosphate-buffered saline (PBS) or cell culture media to initiate self-assembly in physiological conditions [3] [30].
- Purification Equipment: HPLC system for PA purification, LC-MS for characterization [30].
Procedure:
- PA Synthesis and Characterization:
- Self-Assembly Induction:
- Dissolve purified PA in deionized water (typically 0.1-1.0% w/v) and sonicate briefly.
- Trigger self-assembly by adding 10X PBS or DMEM to achieve physiological pH and ionicity (final 1X concentration). Alternatively, adjust pH to neutral range [3].
- Nanofiber Characterization:
- Functional Validation:
Therapeutic Applications: Self-assembled PA nanofibers can be designed as injectable or sprayable therapies that gel in situ upon contact with wound fluid. They provide biochemical cues to direct cell behavior, promote angiogenesis, modulate inflammation, and combat infection with lower risk of resistance compared to conventional antibiotics [3] [13] [30].
Visualization of Methodologies and Applications
Diagram 1: Nanofiber Fabrication Workflows and Therapeutic Applications. This diagram illustrates the parallel processes for electrospinning and molecular self-assembly, highlighting their convergence on common biomedical applications in wound healing.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Nanofiber Wound Healing Applications
| Reagent/Material | Function/Application | Examples & Specifications |
|---|---|---|
| Medical-Grade Polymers | Base material for electrospun nanofibers providing structural integrity and biocompatibility [33] [32] | Polyurethane (Spincare), Polycaprolactone (PCL), Polylactic-co-glycolic acid (PLGA), Chitosan, Gelatin |
| Peptide Amphiphiles | Molecular building blocks for self-assembling nanofibers with bioactive signaling [3] [30] | C16-VVVAAAEEE-GRGDS, C16-VVVAAAEEE-IKVAV (custom synthesis >95% purity) |
| Bioactive Compounds | Functionalization agents providing therapeutic effects (antimicrobial, pro-angiogenic) [13] [32] | Antimicrobial peptides (LL-37, nisin), Growth factors (VEGF, FGF), Silver nanoparticles (5-50 nm) |
| Responsive Linkers | Enable controlled drug release in response to wound microenvironment cues [30] | ROS-cleavable (e.g., proline-rich), Glutathione-cleavable (e.g., disulfide bonds like SPDP, NDEC) |
| Crosslinking Agents | Enhance stability of nanofibers in aqueous wound environments [32] [35] | Genipin (natural), Glutaraldehyde vapor, UV irradiation, EDC/NHS chemistry |
| Characterization Standards | Validate nanofiber properties and ensure batch-to-batch consistency [3] [30] [33] | NMR solvents, HPLC standards, TEM grids, SAXS calibration standards |
Electrospinning and molecular self-assembly represent complementary approaches for producing nanofibers with distinct advantages for wound healing applications. Electrospinning enables fabrication of high-strength, ECM-mimetic scaffolds with tunable mechanical properties, while self-assembling peptide amphiphiles offer precise biochemical signaling and minimally invasive application formats. The protocols and analyses provided herein offer researchers a foundation for selecting and optimizing nanofiber production methods based on specific therapeutic requirements. As the field advances, hybrid approaches combining both methodologies may yield next-generation wound healing solutions with enhanced regenerative capabilities.
The management of chronic wounds, particularly in the context of diabetic complications, presents a significant clinical challenge due to their irregular geometry and disrupted neurovascular microenvironment [36]. Sprayable biomaterial systems that undergo in-situ gelation on the wound bed offer a promising therapeutic strategy, enabling conformal coverage and the delivery of bioactive cues directly to the wound site. Framed within broader thesis research on sprayable peptide amphiphile (PA) nanofibers, this application note details the formulation principles, characterization methodologies, and functional validation protocols for developing such systems. These sprayable systems are designed to emulate the fibrous architecture of the native extracellular matrix (ECM) while providing practical application advantages for complex wound geometries [3] [37]. The following sections provide a structured guide for researchers and drug development professionals, summarizing critical quantitative data, experimental workflows, and essential reagent solutions for developing and evaluating these advanced wound healing platforms.
Molecular Design and Formulation Principles
Peptide Amphiphile (PA) Design
The core molecular building blocks for these systems are peptide amphiphiles, which are specifically engineered to self-assemble into supramolecular nanofibers under physiological conditions. The canonical PA structure incorporates four distinct regions [3]:
- Hydrophobic Domain: A long alkyl tail (e.g., from palmitic acid) that drives hydrophobic collapse and forms the core of the nanofiber.
- β-Sheet Forming Sequence: A short peptide segment (e.g., VVVAAA) that promotes hydrogen bonding and directs one-dimensional nanofiber growth.
- Charged Region: Amino acids with ionizable side chains (e.g., glutamic acid) that provide aqueous solubility and enable gelation triggered by physiological electrolytes.
- Bioactive Epitope: A terminal peptide signal (e.g., RGDS or IKVAV) for specific biological interactions, such as promoting cell adhesion or neurite outgrowth [3].
Table 1: Key Structural Regions of a Model Peptide Amphiphile
| Structural Region | Chemical Component | Primary Function | Example |
|---|---|---|---|
| Hydrophobic Domain | Alkyl tail | Drives assembly via hydrophobic collapse | C16 (Palmitic acid) |
| β-Sheet Region | Short peptide sequence | Enforces nanofiber growth via H-bonding | VVVAAA |
| Charged Region | Ionizable amino acids | Confers water solubility; enables salt-triggered gelation | Glutamic acid |
| Bioactive Epitope | Signaling peptide | Directs biological function (e.g., cell adhesion) | RGDS, IKVAV |
This molecular design allows a low-viscosity aqueous solution of PAs to be sprayed onto a wound bed, where contact with physiological salt concentrations screens electrostatic repulsions, triggering self-assembly into a nanofibrous gel that structurally mimics the native ECM [3].
Composite Hydrogel Systems
To enhance mechanical integrity and functionality, PAs can be integrated with polymer-based hydrogels. A widely used system involves methacrylated gelatin (GelMA) and hyaluronic acid (HAMA), which form covalently crosslinked networks via photopolymerization [37] [36]. The combination of these components creates a synergistic system:
- GelMA provides cell-adhesive motifs and enzymatically degradable sites, supporting cell infiltration and proliferation [37].
- HAMA contributes to structural strength and elasticity, and helps maintain a hydrated wound microenvironment [37].
- Peptide Amphiphiles co-assemble within this polymer network to present a high density of nanoscale bioactive signals.
This composite approach allows for the creation of a sprayable precursor solution that can be photocrosslinked in situ to form a stable, biomimetic matrix. The viscosity of the precursor solution is critical for sprayability, with GelMA concentrations typically ranging from 5% to 15% (w/v) and HAMA at 1% (w/v) to ensure a balance between flowability and post-crosslinking mechanical properties [37].
Diagram 1: In-Situ Gelation Workflow.
Quantitative Formulation Parameters
Successful formulation requires careful optimization of component concentrations to ensure sprayability, gelation kinetics, and final material properties. The following tables summarize key quantitative data for both PA-based and polymer-based sprayable systems.
Table 2: Key Parameters for Sprayable Hydrogel Precursors [37]
| Component | Concentration Range | Function | Impact on Properties |
|---|---|---|---|
| GelMA | 5 - 15% (w/v) | Polymer backbone for cell adhesion and migration | ↑ Concentration → ↑ Viscosity, ↑ Mechanical Strength |
| HAMA | 1% (w/v) | Enhances elastic modulus and structural integrity | Provides hydration; improves handling |
| Photoinitiator (Irgacure 2959) | 0.5 - 1% (w/v) | Enables UV light-triggered crosslinking | Critical for gelation speed and network formation |
| Calcium Peroxide (CaO₂) | 0 - 12 mg/mL | Oxygen release; antibacterial activity | Sustained O₂ release for up to 2 weeks [37] |
Table 3: Functional Additives for Advanced Wound Healing
| Bioactive Additive | Representative Concentration | Primary Function | Experimental Outcome |
|---|---|---|---|
| VEGF-mimetic peptide (KLT) | Co-functionalized with RGI [36] | Promotes angiogenesis and endothelial cell maturation | Enhanced neovascularization in diabetic rat model [36] |
| BDNF-mimetic peptide (RGI) | Co-functionalized with KLT [36] | Enhances Schwann cell activity and axonal regeneration | Improved neurovascular niche formation [36] |
| Antimicrobial Peptide (HHC-36) | Encapsulated in GelMA-DOPA hydrogel [22] | Broad-spectrum antibacterial activity | ~100% bactericidal capacity against S. aureus and P. aeruginosa [22] |
| Cerium Oxide Nanoparticles (CeONs) | Encapsulated in GelMA-DOPA hydrogel [22] | Reactive Oxygen Species (ROS) scavenging | Reduced oxidative stress and scar formation [22] |
Experimental Protocols
Protocol: Formulation and Spray Application of a PA-Polymer Composite Hydrogel
This protocol describes the preparation and application of a multifunctional, sprayable hydrogel combining peptide amphiphiles and a GelMA-HAMA polymer network.
I. Materials Preparation
- Research Reagent Solutions:
- Synthesized Peptide Amphiphiles (PAs): Dissolved in sterile, deionized water at 1% (w/v) and sonicated to create a monodisperse solution.
- GelMA/HAMA Stock Solution: 10% (w/v) GelMA and 1% (w/v) HAMA in PBS (sterile).
- Photoinitiator Solution: 2% (w/v) Irgacure 2959 in PBS. Protect from light.
- Functional Additives: Prepare stock solutions of CaO₂ (e.g., 100 mg/mL in water), therapeutic peptides, or nanoparticles as required.
II. Precursor Solution Formulation
- Mix the GelMA/HAMA stock solution with the PA solution to the desired final concentration (e.g., 8% GelMA, 1% HAMA, 0.5% PA).
- Add the photoinitiator solution to the mixture for a final concentration of 0.5% (w/v).
- Incorporate any functional additives (e.g., CaO₂ at 6 mg/mL final concentration).
- Gently agitate the mixture on a rotary mixer at 37°C for 30 minutes to ensure complete homogenization without bubble formation. The solution should remain a low-viscosity liquid.
III. Spray Application and In-Situ Gelation
- Equipment Setup: Load the precursor solution into a spray device (e.g., a pneumatic spray gun or a simple bottle with a spray nozzle). Ensure the system is sterile.
- Wound Bed Preparation: Clean and debride the wound bed according to standard surgical procedures.
- Spray Application: Holding the spray nozzle 10-15 cm from the wound surface, apply the precursor solution in a sweeping motion to achieve a uniform, continuous layer.
- Gelation Trigger:
- PA Self-Assembly: Occurs immediately upon contact with the wound bed's ionic fluid.
- Polymer Crosslinking: Immediately after spraying, expose the coated wound to low-intensity UV light (e.g., 365 nm, 5-10 mW/cm²) for 60-120 seconds to initiate photocrosslinking and form a stable hydrogel.
Protocol: In-Vitro Characterization of Sprayability and Gelation
This protocol outlines the quantitative assessment of the precursor solution's sprayability and the properties of the resulting gel.
I. Sprayability and Coverage Assessment
- Setup: Preheat the precursor solution to 37°C to simulate physiological conditions. Use a spray system with a calibrated nozzle.
- Spray Volume Measurement: Spray the solution five times into a pre-weighed container. Weigh the container to determine the total mass dispensed and calculate the average volume per spray.
- Droplet Size and Pattern Analysis: Spray the solution onto a flat surface covered with absorbent paper. Capture images and use image analysis software to determine the covered area and assess droplet size distribution and uniformity [37].
II. Rheological Characterization
- Pre-gelation Viscosity: Using a rheometer with a cone-and-plate geometry, measure the viscosity of the precursor solution at 37°C over a range of shear rates (0.1 to 100 s⁻¹). A shear-thinning behavior is desirable for sprayability.
- Gelation Kinetics: After depositing the solution onto the rheometer plate, initiate crosslinking (e.g., via UV light) while monitoring the storage (G') and loss (G'') moduli over time. The gel point is identified when G' surpasses G''.
III. Oxygen Release Profiling
- Setup: Place a crosslinked hydrogel disc containing CaO₂ into a sealed container filled with PBS.
- Measurement: Use a dissolved oxygen meter or sensor to measure the oxygen concentration in the PBS at predetermined time points over 14 days [37].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Sprayable Hydrogel Formulation
| Reagent / Material | Function / Role | Key Characteristic | Considerations for Use |
|---|---|---|---|
| GelMA (Gelatin Methacryloyl) | Biodegradable polymer backbone providing cell-adhesive motifs. | Degree of methacrylation controls crosslinking density. | Higher concentrations (e.g., 15% w/v) improve mechanical strength but increase viscosity [37]. |
| HAMA (Hyaluronic Acid Methacrylate) | ECM-derived component enhancing hydration and elasticity. | Contributes to a moist wound microenvironment. | Often used at lower concentrations (e.g., 1% w/v) in composite with GelMA [37]. |
| Irgacure 2959 | Photoinitiator for UV-induced radical polymerization. | Cytocompatible at concentrations ≤ 0.5% (w/v). | UV exposure time and intensity must be optimized to balance gelation and cell viability. |
| Peptide Amphiphiles (PAs) | Supramolecular nanofiber formation; presentation of bioactive signals. | Sequence defines bioactivity and assembly kinetics. | Bioactive epitopes (e.g., IKVAV, RGDS) must be accessible on the fiber surface [3]. |
| Calcium Peroxide (CaO₂) | Oxygen-generating agent; antibacterial. | Decomposes in water to release O₂ and H₂O₂. | Concentration must be controlled to avoid cytotoxic levels of H₂O₂ [37]. |
| Therapeutic Peptides (e.g., KLT, RGI) | Mimic growth factors to promote angiogenesis and innervation. | Overcomes limitations of recombinant proteins (cost, stability). | Can be conjugated to PA molecules or physically entrapped in the hydrogel network [36]. |
Functional Validation and Pathway Analysis
The efficacy of these sprayable systems is validated through their ability to modulate key biological pathways critical for wound healing. Two primary mechanisms of action are the reconstruction of the neurovascular niche and the scavenging of reactive oxygen species.
Neurovascular Regeneration: Co-delivery of VEGF-mimetic (KLT) and BDNF-mimetic (RGI) peptides promotes the formation of a structured neurovascular unit. KLT stimulates endothelial cells to form new blood vessels (angiogenesis), while RGI enhances Schwann cell activity, facilitating axonal regeneration [36]. This intercellular communication leads to the close alignment of CD31+ capillaries with PGP9.5+ nerve fibers, which is essential for functional recovery in diabetic wounds [36]. Furthermore, transcriptomic analyses indicate that these systems can suppress the IL-17 signaling pathway, reducing chronic inflammation [36].
Antibacterial and ROS-Scavenging Functions: The incorporation of Calcium Peroxide (CaO₂) provides sustained oxygen release, which alleviates hypoxia and exhibits antibacterial properties through the generation of hydrogen peroxide [37]. For more severe oxidative stress, Cerium Oxide Nanoparticles (CeONs) can be encapsulated; they act as potent catalytic antioxidants, scavenging excess ROS and protecting tissues from oxidative damage, thereby reducing scar formation [22].
Diagram 2: Key Biofunctional Pathways.
Sprayable peptide amphiphile (PA) nanofibers represent a groundbreaking platform in advanced wound healing research, offering an exceptional combination of minimally invasive application and sophisticated biofunctionality. These supramolecular structures are engineered to self-assemble into ECM-mimicking nanofibrous networks that provide a protective, hydrated wound environment while serving as a versatile delivery vehicle for therapeutic agents [38] [39]. The modular design of PA molecules enables precise incorporation of multiple bioactive peptide sequences within a single supramolecular framework, allowing researchers to concurrently address distinct biological processes critical to wound repair [39]. This application note details standardized protocols for functionalizing sprayable PA nanofibers with therapeutic cargos and provides characterization methodologies to validate their performance in wound healing applications.
The fundamental structure of a peptide amphiphile typically consists of a hydrophobic alkyl tail conjugated to a functional peptide sequence, which may include bioactive motifs for specific therapeutic actions [38] [39]. When self-assembled under physiological conditions, these molecules form stable nanofibers with displayed bioactive epitopes that can interact with cellular receptors and structural components of the wound environment [38]. The sprayable nature of these systems allows for high-throughput deposition over uneven wound surfaces, facilitating complete coverage of complex wound geometries while maintaining strong tissue adhesion in wet, physiological environments [38].
Bioactive Cargos and Functionalization Strategies
Cargo Loading Methods and Characterization
Table 1: Functionalization Approaches for Sprayable PA Nanofibers
| Functionalization Method | Bioactive Cargo Compatibility | Loading Efficiency Range | Release Profile | Key Advantages |
|---|---|---|---|---|
| Co-assembly Integration | Antimicrobial peptides, Collagen-binding peptides, Mineralization sequences | 85-95% [39] | Sustained release over 7-21 days [39] | Homogeneous distribution, Minimal processing steps |
| Physical Encapsulation | Cerium oxide nanoparticles, Small molecule drugs, Growth factors | 70-90% [22] | Burst release initially, sustained for 14-28 days [22] [38] | Protection of cargo bioactivity, No chemical modification required |
| Surface Conjugation | Adhesive motifs (DOPA), Cell-binding ligands (RGD) | >90% [22] [39] | Stable presentation, minimal release [39] | Direct exposure to cellular receptors, Enhanced binding interactions |
| Supramolecular Binding | Nucleic acids, Charged peptides, Therapeutic proteins | 60-80% [38] | Stimuli-responsive to pH, enzymes, or ROS [38] | Triggered release mechanisms, Protection of sensitive biologics |
Experimental Protocol: Co-assembly of Multifunctional PA Nanofibers
Principle: This protocol describes the integration of multiple bioactive PA sequences through co-assembly into multifunctional nanofibers, creating a complex wound healing matrix that addresses infection control, tissue integration, and regenerative signaling simultaneously [39].
Materials:
- Synthesized peptide amphiphiles (DGEA-PA, EEE-PA, DOPA-PA, GL13K-PA) [39]
- Deionized water (18.2 MΩ·cm resistivity)
- Phosphate buffered saline (10× concentrate, sterile)
- Ultrasonic water bath
- pH meter and adjustment solutions (0.1M HCl, 0.1M NaOH)
Procedure:
- Prepare individual PA solutions: Dissolve each PA (DGEA-PA, EEE-PA, DOPA-PA, GL13K-PA) in deionized water at a concentration of 1% (w/v) individually. Sonicate for 15 minutes at 25°C to ensure complete dissolution [39].
- Determine mixing ratios: Based on desired functionality, combine PA solutions at appropriate molar ratios. A standard ratio for wound healing applications is 2:2:1:1 (DGEA-PA:EEE-PA:DOPA-PA:GL13K-PA) to balance osteoinduction, mineralization, adhesion, and antimicrobial properties [39].
- Co-assemble nanofibers: Mix the PA solutions thoroughly by vortexing for 30 seconds followed by gentle shaking for 2 hours at room temperature.
- Induce gelation: Add 10× PBS to the PA mixture to achieve a final 1× PBS concentration. Gelation typically occurs within 15 seconds as evidenced by crossover of storage modulus (G′) above loss modulus (G″) in rheological measurements [38].
- Characterize assembly: Verify nanofiber formation using transmission electron microscopy (TEM). Specimens should show flexible filaments several micrometers in length with diameters of approximately 11 nm [38].
- Assess bioactivity: Conduct antibacterial assays against S. aureus and P. aeruginosa for antimicrobial functionality, and cell adhesion studies with fibroblasts or stem cells to validate integrin-binding capability [39].
Troubleshooting Tips:
- If gelation occurs too rapidly, reduce PBS concentration to 0.5× and gradually increase.
- If nanofibers appear fragmented or short, extend the self-assembly time before PBS addition.
- For sprayability optimization, adjust total PA concentration between 1-4 mM to balance viscosity and bioactivity [38].
Characterization Methodologies
Structural and Mechanical Analysis
Nanofiber Morphology and Structural Integrity:
- TEM Sample Preparation: Apply 5 μL of PA solution (pre- and post-gelation) to Formvar-coated copper grids. Negative stain with 1% uranyl acetate for 30 seconds. Image using an accelerating voltage of 80 kV [38]. Expect to observe long, flexible filaments with occasional twisting and entanglement points.
- Circular Dichroism Spectroscopy: Prepare PA solutions at 0.01% (w/v) in deionized water. Record spectra from 190-260 nm using a 1 mm path length quartz cuvette. Characteristic β-sheet formation shows a positive band at ~195 nm and negative band at ~218 nm [38] [39].
- Rheological Analysis: Conduct oscillatory rheometry using a 25 mm parallel plate geometry with a 0.5 mm gap. Set frequency to 1 Hz and strain to 1% (within linear viscoelastic region). Monitor G′ and G″ for 10 minutes post-PBS addition to document gelation kinetics. Sprayed gels typically show slightly reduced stiffness (G′ of ~250 Pa) compared to non-sprayed controls (G′ of ~300 Pa) due to minor filament alignment [38].
Biofunctional Assessment
Table 2: Quantitative Functional Assessment of Bioactive PA Nanofibers
| Functional Assessment | Test Method | Performance Metrics | Acceptance Criteria |
|---|---|---|---|
| Antimicrobial Efficacy | Time-kill assay against S. aureus and P. aeruginosa [22] [39] | >99% reduction in bacterial viability within 4 hours [22] | No bacterial recovery after 24 hours incubation |
| ROS Scavenging Capacity | H₂O₂ degradation assay using peroxide test strips [22] | >80% H₂O₂ degradation within 30 minutes [22] | Linear degradation kinetics for first 15 minutes |
| Cell Adhesion and Viability Live/dead staining with Calcein-AM/propidium iodide [38] [39] | >95% cell viability after 7 days culture [38] | Confluent cell layers with spreading morphology by day 7 | |
| Osteogenic Differentiation | ALP activity assay and osteogenic gene expression (qRT-PCR) [39] | 3-5 fold increase in RUNX2, OPN, COL1A1 expression [39] | Significant mineralization by Alizarin Red staining at day 21 |
| Tissue Adhesion Strength | Lap shear test on excised porcine skin [38] | Strong adhesion to multiple organ surfaces with minimal detachment [38] | Cohesive failure rather than adhesive failure |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for PA Nanofiber Functionalization
| Reagent/Category | Specific Examples | Function in Experimental Workflow | Supplier Notes |
|---|---|---|---|
| Peptide Amphiphile Building Blocks | DGEA-PA, EEE-PA, DOPA-PA, GL13K-PA [39] | Core structural components providing bioactivity | Synthesize via Fmoc-SPPS; purity >95% by HPLC |
| Antimicrobial Peptides | HHC-36 (KRWWKWWRR) [22], GL13K [39] | Broad-spectrum antibacterial activity against wound pathogens | Source from commercial peptide synthesis services |
| ROS-Scavenging Nanoparticles | Cerium oxide nanoparticles (CeONs) [22] | Protect against oxidative stress in chronic wounds | 10-100 nm diameter range for optimal encapsulation |
| Adhesive Motifs | DOPA-conjugated polymers [22] [39], Collagen-binding peptides (LRELHLNNN) [38] | Enhanced tissue adhesion in wet wound environments | KD = 1.7×10⁻⁷ M for collagen-binding peptides [38] |
| Crosslinking Agents | Irgacure 2959 [22], HRP enzyme [40] | Photocrosslinking or enzymatic hydrogel stabilization | Use at 0.1% (w/v) for UV initiation (365 nm) |
| Characterization Tools | TEM grids, rheometer fixtures, CD spectropolarimeter cells | Structural and mechanical analysis of nanofibers | Standard laboratory equipment from scientific suppliers |
Application Protocol: In Vivo Wound Healing Assessment
Principle: This protocol describes the methodology for evaluating the efficacy of functionalized sprayable PA nanofibers in promoting wound healing using established animal models, with specific focus on infection control, re-epithelialization, and tissue remodeling [22] [39].
Materials:
- Sprayable PA nanofiber formulation (4 mM in sterile water)
- Mucosal atomizer or airbrush sprayer (0.3-0.5 mm nozzle)
- Animal model (e.g., diabetic mouse, rabbit ear)
- Bacterial suspension for infection models (e.g., MRSA, P. aeruginosa)
- Histological processing supplies (formalin, paraffin, staining solutions)
Procedure:
- Wound Creation and Infection: Create full-thickness excisional wounds (6-8 mm diameter) on the dorsum of anesthetized animals. For infection models, inoculate with 10⁷ CFU of bacteria in 10 μL PBS and allow establishment for 24 hours [22].
- Nanofiber Application: Load PA solution into spray applicator. Hold nozzle 10-15 cm from wound surface and apply with gentle, sweeping motions until complete coverage is achieved. Gelation occurs within seconds of contact with wound fluid [38].
- Treatment Schedule: Apply every 3-4 days based on degradation profiling. For CBPA-based systems, linear degradation of approximately 0.23%/day was observed in sprayed gels [38].
- Monitoring and Assessment:
- Daily Documentation: Capture digital images with scale reference for wound area measurement.
- Bacterial Load: At sacrifice, harvest wound tissue, homogenize, and plate serial dilutions on agar for CFU counting [22].
- Histological Analysis: Process healed tissue at day 14 for H&E staining (re-epithelialization), Masson's trichrome (collagen deposition), and immunohistochemistry (CD31 for angiogenesis) [39].
- Statistical Analysis: Compare treatment groups using one-way ANOVA with post-hoc Tukey test (n≥5). Significance threshold at p<0.05.
Expected Results: Multifunctional PA nanofibers should demonstrate significantly accelerated wound closure rates (>50% by day 7), reduced bacterial loads (2-3 log reduction), enhanced granulation tissue formation, and improved collagen organization compared to controls [22] [39].
Sprayable peptide amphiphile nanofibers functionalized with bioactive cargos represent a versatile and effective platform for advanced wound healing research. The protocols outlined in this application note provide researchers with standardized methodologies for developing, characterizing, and evaluating these sophisticated biomaterial systems. The integration of multiple bioactive signals—including antimicrobial protection, ROS scavenging, tissue integration, and regenerative promotion—enables comprehensive management of the complex wound healing cascade.
Critical technical considerations for successful implementation include maintaining sterility throughout PA synthesis and processing, optimizing spraying parameters for different wound geometries, and validating batch-to-batch consistency through rigorous structural characterization. The modular nature of the PA platform allows researchers to tailor biofunctional compositions to specific wound healing challenges, from diabetic ulcers to burn wounds and surgical site infections. As research progresses, these sprayable nanofiber systems hold significant promise for clinical translation, potentially offering improved outcomes for patients with challenging wound healing scenarios.
Practical Application Protocols for Burn and Chronic Wound Management
The management of burns and chronic wounds represents a significant clinical challenge, exacerbated by the rising threat of antimicrobial resistance and the complexity of the wound healing cascade. Sprayable peptide amphiphile (PA) nanofibers have emerged as a transformative therapeutic platform, offering a unique combination of targeted bioactivity and practical application. These supramolecular nanomaterials are engineered to emulate the fibrous architecture of the native extracellular matrix (ECM) while delivering concentrated therapeutic signals directly to the wound bed [3]. Their sprayable format enables rapid, conformable coverage of irregularly shaped wound surfaces, facilitating minimally invasive application and improved patient compliance [41] [42]. This document provides detailed application notes and experimental protocols for researchers developing PA nanofiber-based therapies for advanced wound management.
Molecular Design and Self-Assembly Fundamentals
Peptide Amphiphile Structure-Function Relationship
Peptide amphiphiles are synthetically designed molecules that integrate a hydrophobic alkyl tail with a hydrophilic peptide sequence. A canonical PA structure comprises four distinct regions, each serving a specific function in self-assembly and bioactivity [3]:
- Hydrophobic Domain: A long alkyl tail (e.g., palmitic acid) that drives hydrophobic collapse in aqueous environments, forming the core of the nanofiber.
- β-Sheet Forming Sequence: A short peptide segment (e.g., VVVAAA) that promotes intermolecular hydrogen bonding, enforcing one-dimensional growth into nanofibers.
- Charged Segment: Ionizable amino acids (e.g., glutamic acid) that provide aqueous solubility and enable triggered gelation via physiological electrolytes.
- Bioactive Epitope: A terminal peptide signal (e.g., RGDS, IKVAV) that interacts with cellular receptors to direct specific biological responses.
Table 1: Key Bioactive Epitopes for Wound Healing Applications
| Bioactive Epitope | Sequence | Biological Function | Target Wound Phase |
|---|---|---|---|
| RGDS | Arg-Gly-Asp-Ser | Promotes integrin-mediated cell adhesion and spreading [3] | Proliferation |
| IKVAV | Ile-Lys-Val-Ala-Val | Enhances neurite outgrowth and neuronal cell migration [3] | Proliferation/Remodeling |
| LL-37 | Derived from human cathelicidin | Broad-spectrum antimicrobial; immunomodulatory; promotes angiogenesis and re-epithelialization [13] | Inflammation/Proliferation |
Mechanism of Self-Assembly and Gelation
The therapeutic application of PAs relies on their in situ transition from a liquid solution to a nanofibrous network. The self-assembly process is governed by three primary energy contributions: hydrophobic collapse of the alkyl tails, hydrogen bonding within the β-sheet regions, and electrostatic modulation via the charged segments [3].
The resulting supramolecular polymers form high-aspect-ratio nanofibers that display a high density of bioactive signals on their surface. These nanofibers can entangle to form a stable hydrogel network upon contact with physiological saline or divalent cations present in wound exudate, creating a protective and bioactive barrier over the wound [3]. This mechanism enables the formulation of a low-viscosity, easy-to-spray solution that transforms into a structured matrix upon application.
Diagram 1: PA Self-Assembly Pathway
Practical Application Protocols
Protocol 1: Formulation of a Sprayable PA Solution for Infected Burn Wounds
This protocol outlines the preparation of an antimicrobial PA solution designed for spray application on burn wounds, which are highly susceptible to infection.
Research Reagent Solutions:
- PA Monomer: Synthesized PA with a C16 alkyl tail, VVVAAA β-sheet sequence, four glutamic acid residues, and a terminal KR-12 antimicrobial peptide (derived from LL-37).
- Sterile Deionized Water: Aqueous solvent for molecular dissolution.
- Buffer Solution: Low-ionic-strength buffer (e.g., 1 mM Tris-HCl, pH 7.4) to maintain PA solubility pre-application.
Procedure:
- Dissolution: Dissolve the PA monomer in sterile, ice-cold deionized water or low-ionic-strength buffer to a final concentration of 1.0% (w/v).
- Sterilization: Filter the solution through a 0.22 µm sterile syringe filter into an airtight, sterile vial. This step is critical for burn wound applications.
- Storage: Store the sterile solution at 4°C for up to 2 weeks. Do not freeze.
- Application Setup: Load the PA solution into a sterile spray bottle or an air-assisted nebulizer. For preclinical models, a 10 mL sterile plastic spray bottle with a fine-mist nozzle is effective.
- Spray Application: Hold the nozzle 10-15 cm from the wound surface. Apply 2-3 sprays per cm² of wound area, ensuring complete and even coverage. The solution will appear as a thin, clear film.
- Gelation: Gelation occurs within 30-60 seconds upon contact with wound exudate. The formation of a stable, translucent gel indicates successful fiber assembly.
Protocol 2: Application of a Pro-Healing PA Formulation for Diabetic Ulcers
This protocol describes the use of a PA system functionalized with the RGDS epitope to promote cellular proliferation and re-epithelialization in chronic, non-healing diabetic ulcers.
Research Reagent Solutions:
- PA Monomer: Synthesized PA with a C16 alkyl tail, VVVAAA β-sheet sequence, four glutamic acid residues, and a terminal RGDS cell-adhesion peptide.
- Sterile Water for Injection (WFI): Apyrogenic solvent.
- Photoinitiator: Irgacure 2959 (2-Hydroxy-4'-(2-hydroxyethoxy)-2-methylpropiophenone), prepared as a 0.5% (w/v) stock solution in WFI.
Procedure:
- Solution Preparation: Dissolve the PA monomer in WFI to a final concentration of 1.5% (w/v). Gently vortex until clear.
- Photoinitiator Addition: Add the Irgacure 2959 stock solution to the PA solution to a final concentration of 0.05% (w/v). Protect from light by wrapping the vial in aluminum foil.
- Sterile Filtration: Filter the mixture through a 0.22 µm sterile syringe filter.
- Wound Bed Preparation: Debride the diabetic ulcer to remove necrotic tissue and create a bleeding edge, which is essential for healing.
- Spray Application: Apply the PA solution evenly across the debrided wound bed using a sterile spray device.
- Photocrosslinking: Immediately after spraying, expose the wound to low-intensity UV light (365 nm, 5-10 mW/cm²) for 2-3 minutes to induce additional covalent crosslinking within the nanofiber network, enhancing mechanical stability in high-exudate environments [42].
Quantitative Performance Benchmarks
Data from in vitro and preclinical studies provide key benchmarks for evaluating the efficacy of PA-based wound therapies. The following table summarizes expected performance outcomes based on advanced wound dressing technologies.
Table 2: Performance Benchmarks for Advanced Wound Therapies
| Performance Parameter | Target Benchmark | Relevant Methodology | Reference Platform |
|---|---|---|---|
| Antibacterial Efficacy | >90% reduction in bacterial load (S. aureus, E. coli) vs. control in 24h [14] | ISO 22196 / JIS Z 2801 | Mupirocin-loaded nanofibers [14] |
| Oxygen Release | Sustained release over 14 days [42] | Optical dissolved oxygen probe | CaO₂-loaded hydrogel [42] |
| Drug Release Profile | Sustained release over 5-7 days; >85% cumulative release [14] | In vitro elution (PBS, 37°C) | Sol/SPI/Mp Nanofibers [14] |
| Water Vapor Permeability | ~820 g/m²/day [14] | Gravimetric cup method (ASTM E96) | Sol/SPI/Mp Nanofibers [14] |
| In Vivo Wound Closure | ~100% closure in 18 days in diabetic mouse model [32] | Digital planimetry of full-thickness wounds | Berberine-loaded PHBV nanofibers [32] |
Analytical and Characterization Methods
Protocol 3: In Vitro Assessment of Antibacterial and Biofilm Disruption Activity
Objective: To quantify the antibacterial efficacy and biofilm disruption potential of antimicrobial PA nanofibers.
Reagents: Tryptic Soy Broth (TSB), Crystal Violet (0.1%), Phosphate Buffered Saline (PBS). Equipment: Microplate reader, Scanning Electron Microscope (SEM). Bacterial Strains: Staphylococcus aureus (ATCC 25923), Pseudomonas aeruginosa (ATCC 27853).
Procedure:
- Direct Contact Assay: Prepare PA-coated surfaces by spraying 1 mL of PA solution into 24-well plates and inducing gelation. Inoculate with 10µL of bacterial suspension (1x10⁶ CFU/mL in TSB). Incubate at 37°C for 24h.
- Viability Quantification: Recover bacteria by sonication in 1 mL PBS. Serially dilute and plate on TSB agar. Count Colony Forming Units (CFUs) after 24h. Calculate log reduction compared to control wells [14].
- Biofilm Assay: Grow biofilms on PA-coated surfaces for 48h. Gently wash to remove non-adherent cells. Fix biofilm with methanol and stain with 0.1% Crystal Violet for 15 minutes. Elute dye with 33% acetic acid and measure absorbance at 595 nm to quantify biofilm biomass [13].
Protocol 4: In Vivo Evaluation in a Diabetic Murine Wound Model
Objective: To evaluate the efficacy of pro-healing PA nanofibers in a pathologically relevant chronic wound model.
Animal Model: Genetically diabetic (db/db) mice, 8-10 weeks old. Wound Creation: Create two full-thickness excisional wounds (6 mm diameter) on the dorsal skin under anesthesia.
Procedure:
- Group Allocation: Randomize animals into three groups (n=6-8): (i) PA-RGDS treatment, (ii) Unloaded PA (control), (iii) Commercial hydrogel dressing (positive control).
- Treatment: Apply the assigned treatment according to Protocol 2 on day 0 and every 3 days thereafter.
- Wound Closure Monitoring: Capture high-resolution digital images of wounds on days 0, 3, 7, 10, 14, and 18. Calculate wound area using image analysis software (e.g., ImageJ). Express closure as percentage of original area.
- Histological Analysis: Euthanize animals at defined endpoints (e.g., day 7 and 18). Excise wound tissue, fix in formalin, and embed in paraffin. Section and stain with Hematoxylin & Eosin (H&E) to assess general morphology and Masson's Trichrome to evaluate collagen deposition. Score for re-epithelialization, granulation tissue formation, and neutrophil infiltration [14] [32].
Diagram 2: In Vivo Evaluation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for PA Wound Healing Research
| Reagent / Material | Function & Rationale | Example Source / Specification |
|---|---|---|
| Methacrylate-modified Gelatin (GelMA) | Provides a biocompatible, photocrosslinkable matrix to blend with PAs; enhances cell adhesion and structural integrity [42]. | Sigma-Aldrich, Catalog # ESI-BIO-GM-50 |
| Calcium Peroxide (CaO₂) | Solid peroxide providing controlled oxygen release and antibacterial H₂O₂; relieves wound hypoxia [42]. | Sigma-Aldrich, 99% purity, Catalog # 289044 |
| Irgacure 2959 | A biocompatible photoinitiator for UV-induced crosslinking of methacrylated polymers and PAs [42]. | Sigma-Aldrich, Catalog # 410896 |
| Soluplus | An amphiphilic graft copolymer used to enhance drug solubility and fabricate composite nanofibers [14]. | BASF |
| Mupirocin | A broad-spectrum antibiotic effective against Gram-positive and Gram-negative bacteria; used for benchmarking antimicrobial efficacy [14]. | Sigma-Aldrich, Catalog # M7694 |
Navigating Translational Hurdles: Charge, Stability, and Scalability
Optimizing Nanofiber Charge and Cohesion for Enhanced Bioavailability
The development of advanced wound dressings represents a critical frontier in regenerative medicine, particularly for complex injuries such as chronic wounds and severe burns. Among the most promising platforms are sprayable peptide amphiphile (PA) nanofibers, which form hydrogels in situ that closely mimic the native extracellular matrix (ECM). The therapeutic efficacy of these nanofibrous systems is fundamentally governed by their bioavailability—the extent and rate at which the active therapeutic moiety reaches the intended site of action. This bioavailability is directly influenced by two core physicochemical properties: nanofiber surface charge and inter-fiber cohesion. Optimal surface charge modulates cellular interactions, including adhesion, proliferation, and signaling, while tailored cohesion ensures the formation of a mechanically stable, yet biologically active, 3D network that can withstand the wound environment and facilitate controlled release of therapeutic agents [28] [43].
This Application Note provides a structured framework for researchers and drug development professionals to quantitatively optimize these parameters. It details standardized protocols for the synthesis, characterization, and functional validation of sprayable PA nanofiber hydrogels, with a specific focus on enhancing their performance in wound healing applications.
Key Physicochemical Properties and Their Biological Impact
The design of effective PA nanofiber systems requires a deep understanding of the interrelationship between their physical structure, chemical properties, and subsequent biological responses. The table below summarizes the core properties that require optimization and their direct impact on bioavailability and wound healing outcomes.
Table 1: Key Physicochemical Properties of Peptide Amphiphile Nanofibers and Their Biological Impact
| Property | Influence on Bioavailability | Impact on Wound Healing |
|---|---|---|
| Surface Charge (Zeta Potential) | Determines interaction with negatively charged cell membranes; positive charge can enhance cellular adhesion and internalization [44]. | Promotes fibroblast and endothelial cell adhesion and proliferation, crucial for re-epithelialization and granulation tissue formation [43]. |
| Nanofiber Cohesion / Gel Stiffness | Influences the diffusion rate of encapsulated bioactive molecules and the infiltration of cells into the gel matrix [37]. | A stable, yet pliable, 3D matrix supports cell migration and provides a scaffold for new tissue formation, preventing wound contraction [28] [44]. |
| Bioactive Epitope Density | Controls the number of available binding sites for cell surface integrins, directly regulating signaling activation [43]. | The presence of motifs like RGDS (Arg-Gly-Asp-Ser) significantly accelerates re-epithelialization and wound closure by promoting integrin-mediated cell spreading [43]. |
| Oxygen Release Capacity | Alleviates local hypoxia, a major barrier to healing, thereby improving cell survival and metabolic activity [37]. | Self-oxygenating hydrogels have been shown to reduce cell death under hypoxia and promote angiogenic responses, which are vital for nourishing new tissue [37]. |
Quantitative Optimization Data
To guide the formulation process, the following tables consolidate critical quantitative data from relevant studies. This information is essential for establishing baseline parameters and predicting in vivo performance based on in vitro characterization.
Table 2: Impact of Bioactive Epitopes on Cellular Proliferation and Wound Closure
| PA Nanofiber Type | Bioactive Signal | Fibroblast Proliferation (vs. Control) | In Vivo Wound Closure Rate | Key Findings |
|---|---|---|---|---|
| RGDS-Modified PA | RGDS | Significantly Higher [43] | Accelerated (Days 7-28) [43] | Promoted fibroblast stimulation and created a conducive environment for epithelialization [43]. |
| Non-Bioactive PA | None / Scrambled | Lower [43] | Standard [43] | Served as a physical scaffold without active biological signaling [43]. |
| Collagen Gel | Native Collagen Motifs | Moderate [43] | Standard [43] | Used as a standard biomaterial control in comparative studies [43]. |
Table 3: Characterization of Sprayable Hydrogel Formulations for Functional Delivery
| Formulation Component | Concentration Range | Key Functional Outcome | Measurement Technique |
|---|---|---|---|
| GelMA | 5 - 15% (w/v) [37] | Determines sprayability and viscosity; 10% offers optimal balance for spraying and stable gel formation [37]. | Rheometry, Spray Volume Analysis [37] |
| HAMA | 1% (w/v) [37] | Provides structural strength and elasticity to the composite hydrogel [37]. | Mechanical Compression Testing [37] |
| Calcium Peroxide (CaO2) | 0 - 12 mg/mL [37] | Provides sustained oxygen release for up to two weeks and confers antibacterial properties [37]. | Oxygen Probe, Antibacterial Assay [37] |
Experimental Protocols
Protocol 1: Synthesis of RGDS-Functionalized Peptide Amphiphiles
This protocol describes the solid-phase peptide synthesis (SPPS) of a canonical PA functionalized with the RGDS cell-adhesion motif.
Materials:
- Rink Amide MBHA Resin: Solid support for synthesis.
- Fmoc-Protected Amino Acids: Fmoc-Ser(tBu)-OH, Fmoc-Asp(OtBu)-OH, Fmoc-Gly-OH, Fmoc-Arg(Pbf)-OH.
- Palmitic Acid: Hydrophobic tail for the amphiphile.
- Coupling Reagents: HBTU (Hexafluorophosphate Benzotriazole Tetramethyl Uronium) and HOBt (Hydroxybenzotriazole).
- Deprotection Reagent: 20% Piperidine in DMF.
- Cleavage Cocktail: Trifluoroacetic Acid (TFA) with scavengers.
Procedure:
- Resin Swelling: Place 1.0 g of Rink Amide MBHA resin (loading: 0.68 mmol/g) in a peptide synthesis vessel and swell in DCM for 30 minutes.
- Fmoc Deprotection: Drain DCM and treat the resin with 20% piperidine in DMF (2 x 10 mL, 5 + 15 minutes) to remove the Fmoc group. Wash thoroughly with DMF.
- Amino Acid Coupling: For each amino acid (in sequence: Fmoc-Ser(tBu)-OH, Fmoc-Asp(OtBu)-OH, Fmoc-Gly-OH, Fmoc-Arg(Pbf)-OH):
- Pre-activate 4 equivalents of the Fmoc-amino acid and 4 equivalents of HOBt with 4 equivalents of HBTU and 8 equivalents of N,N-Diisopropylethylamine (DIPEA) in DMF for 3 minutes.
- Add the activated solution to the resin and agitate for 2 hours at room temperature.
- Drain and wash the resin with DMF (3 x 10 mL) after each coupling.
- Perform a Kaiser test to confirm coupling completion before proceeding to the next deprotection.
- Palmitoylation: After the final Fmoc deprotection (Arg), couple palmitic acid (4 eq) using the same coupling protocol as above.
- Cleavage and Deprotection: Wash the resin with DCM and dry. Treat the resin with a cleavage cocktail of TFA/Triisopropylsilane/Water (95:2.5:2.5) for 3 hours to simultaneously cleave the peptide from the resin and remove all acid-labile protecting groups.
- Precipitation and Purification: Filter the TFA solution into cold diethyl ether to precipitate the crude PA. Centrifuge, collect the pellet, and dissolve in a 1:1 water-acetonitrile mixture. Purify via reverse-phase HPLC and confirm the identity and purity using Mass Spectrometry (MS) and analytical HPLC.
Protocol 2: Electrospinning and In-Situ Gelation of PA Nanofiber Hydrogel
This protocol outlines the preparation of a sprayable PA solution and its subsequent self-assembly into a nanofibrous hydrogel upon contact with the wound bed.
Materials:
- Synthesized PA: Purified RGDS-PA from Protocol 1.
- Solvent: Deionized water or Phosphate Buffered Saline (PBS).
- Electrospinning Apparatus: Syringe pump, high-voltage power supply, and a grounded collector.
- Spray Device: Commercial air-assisted or airless spray system with a fine mist nozzle.
Procedure:
- Solution Preparation: Dissolve the synthesized PA in a sterile, physiological buffer (e.g., PBS) at a concentration of 0.5-1.0% (w/v). Gently agitate or vortex until a clear solution is obtained. Ensure the solution is kept sterile.
- Nanofiber Formation (In Vitro Characterization): To confirm nanofiber formation, load the PA solution into a syringe for electrospinning. Use a flow rate of 0.5-2 mL/h, an applied voltage of 10-20 kV, and a working distance of 10-20 cm. Collect the nanofibers on aluminum foil for analysis by Scanning Electron Microscopy (SEM).
- Sprayability and In-Situ Gelation:
- Load the sterile PA solution into the reservoir of the spray device.
- For application, direct the spray nozzle 10-15 cm from the target surface (e.g., an in vitro wound model or an in vivo wound).
- Apply a thin, uniform layer. Gelation is triggered by the presence of physiological divalent cations (e.g., Ca²⁺, Mg²⁺) in the wound exudate or a pre-applied saline solution.
- Validation: Assess the quality of the formed hydrogel by its viscoelastic properties using rheometry and its nanofibrous morphology using SEM after critical point drying.
Protocol 3: Characterization of Nanofiber Zeta Potential and Cohesion
This protocol describes key analytical methods to quantify the surface charge of nanofibers and the mechanical cohesion of the resulting hydrogel.
Materials:
- PA Nanofiber Dispersion: Prepared by diluting the PA solution from Protocol 2.
- Zeta Potential Analyzer: Equipped with a laser Doppler velocimeter.
- Rheometer: Cone-plate or parallel-plate configuration.
Procedure: Part A: Zeta Potential Measurement
- Sample Preparation: Dilute the PA solution to an appropriate concentration (e.g., 0.1 mg/mL) in a low-conductivity buffer (e.g., 1 mM NaCl) to minimize interference. Filter through a 0.45 μm membrane if necessary.
- Measurement: Load the sample into a clear disposable zeta cell. Insert the cell into the instrument and set the temperature to 25°C. Allow the system to equilibrate.
- Data Acquisition: Run at least 3 measurements per sample, with a minimum of 12 runs per measurement. The instrument will calculate the zeta potential based on the electrophoretic mobility.
- Analysis: Report the average zeta potential and standard deviation. A positive value (e.g., > +15 mV) suggests good cellular interaction potential, while a highly negative value (e.g., < -30 mV) indicates strong electrostatic colloidal stability.
Part B: Rheological Analysis of Gel Cohesion
- Sample Loading: Form a hydrogel disc (e.g., 8 mm diameter) directly on the rheometer's bottom plate. Lower the upper geometry (e.g., 8 mm parallel plate) to a defined gap (e.g., 0.5 mm).
- Amplitude Sweep: Perform an amplitude sweep at a constant frequency (e.g., 1 Hz) to determine the linear viscoelastic region (LVR) by applying oscillatory strain from 0.1% to 100%.
- Frequency Sweep: At a strain within the LVR, perform a frequency sweep (e.g., 0.1 to 100 rad/s) to characterize the mechanical spectrum (Storage Modulus, G', and Loss Modulus, G''). A G' that is significantly higher than G'' across the frequency range indicates a solid, cohesive gel.
- Analysis: Report the plateau value of G' as a key indicator of gel cohesion and mechanical stability.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Developing Sprayable PA Nanofiber Hydrogels
| Reagent / Material | Function / Rationale | Example Vendor / Catalog Note |
|---|---|---|
| Fmoc-Protected Amino Acids | Building blocks for solid-phase synthesis of the peptide sequence. | Sigma-Aldrich, ChemPep |
| Rink Amide MBHA Resin | Solid support for peptide synthesis, yielding a C-terminal amide upon cleavage. | EMD Millipore, GL Biochem |
| Palmitic Acid | Provides the hydrophobic moiety of the PA, driving self-assembly into nanofibers in aqueous media. | Sigma-Aldrich, TCI Chemicals |
| HATU/HBTU Coupling Reagents | High-efficiency activating agents for amide bond formation during peptide synthesis. | Sigma-Aldrich, AAPPTec |
| Dimethylformamide (DMF) | High-quality solvent for peptide synthesis. | Sigma-Aldrich (Peptide Grade) |
| Trifluoroacetic Acid (TFA) | Used in the final cleavage/deprotection step to liberate the final PA from the resin. | Sigma-Aldrich, Thermo Scientific |
| Dulbecco's Phosphate Buffered Saline (DPBS) | A physiologically compatible solvent for preparing the final PA solution for spraying. | Thermo Fisher Scientific, Gibco |
| Electrospinning Apparatus | For in-vitro characterization of nanofiber morphology and diameter. | Holmarc, Linari Nanotech |
| Malvern Zetasizer Nano ZSP | Instrument for measuring zeta potential and particle size. | Malvern Panalytical |
| TA Instruments Discovery HR Rheometer | For characterizing the mechanical properties and cohesion (G', G'') of the hydrogel. | TA Instruments |
Signaling Pathways and Experimental Workflows
Diagram 1: RGDS-mediated cell signaling pathway.
Diagram 2: Integrated experimental workflow for optimization.
Controlling Drug Release Kinetics and Preventing Payload Trapping
In the context of advanced wound healing applications, sprayable peptide amphiphile (PA) nanofibers represent a promising platform for localized therapeutic delivery. Achieving precise control over drug release kinetics and preventing the irreversible trapping of active payloads are critical for therapeutic efficacy. This document provides detailed application notes and protocols for researchers aiming to design and characterize PA-based delivery systems that address these challenges, focusing on molecular design, co-assembly strategies, and analytical characterization.
Quantitative Data on Release Kinetics and Payload Encapsulation
The design of PA systems significantly influences their drug loading capacity and release profile. The data below summarize key quantitative relationships essential for experimental planning.
Table 1: Influence of PA Molecular Design on Drug Release Kinetics
| Molecular Design Feature | Impact on Release Kinetics | Key Quantitative Findings | Reference |
|---|---|---|---|
| Payload Position in PA Sequence | Directly controls release rate via packing density. | Systematic variation of a hydrazide-derivatized Prodan dye position resulted in near zero-order release with tunable half-lives. | [45] |
| β-sheet Character | Inverse correlation with payload mobility. | Increased β-sheet character in the peptide core correlates with slower payload release. | [45] |
| Co-assembly of Opposing PAs | Enables high encapsulation efficiency for hydrophobic drugs. | Co-assembly of E-PA and K-PA increased solubility of camptothecin (CPT) by 60-fold with high encapsulation efficiency. | [46] |
Table 2: Strategies to Prevent Payload Trapping and Improve Functionality
| Strategy | Mechanism | Experimental Outcome | Reference |
|---|---|---|---|
| Synergistic Co-assembly | Hydrophobic attraction, electrostatic interaction, and hydrogen bonding create a soluble, encapsulated nanofiber. | CPT encapsulated in hybrid nanofibers retained its antitumor activity in vitro against HepG2 cells. | [46] |
| Stapled Peptides | Hydrocarbon stapling enhances proteolytic resistance and stabilizes secondary structure. | Superior stability and performance compared to parent peptides; increases half-life. | [47] |
| D-Amino Acid Substitution | Swapping L- for D-amino acids creates resistance to enzymatic degradation. | Increases peptide stability and half-life in biological environments. | [47] |
Experimental Protocols
Protocol: Co-assembly of Oppositely Charged PAs for Hydrophobic Drug Encapsulation
This protocol describes a method to encapsulate hydrophobic drugs like camptothecin (CPT) using two oppositely charged PAs (e.g., anionic E-PA: C16-AAAAAEEEEGGK and cationic K-PA: C16-VVVAAAKKKGGK) via synergistic assembly and solvent evaporation [46].
- Key Driving Forces: Hydrophobic attraction, electrostatic interaction, and hydrogen bonding.
- Key Advantage: Negates the need for external assembly triggers like pH or temperature changes.
Materials & Reagents
- Peptide Amphiphiles: E-PA and K-PA (e.g., from Biopeptek Pharmaceuticals, LLC).
- Drug: Camptothecin (CPT) or other hydrophobic active.
- Solvents: Dimethyl sulfoxide (DMSO), Ethanol, Deionized Water.
- Equipment: Sonicator, Lyophilizer, Analytical HPLC system, Electrospray Ionization Mass Spectrometer (ESI-MS).
Procedure
- Preparation of Stock Solutions:
- Dissolve E-PA and K-PA separately in DMSO to a final concentration of 10 mg/mL.
- Dissolve CPT in DMSO to a concentration of 5 mg/mL.
- Co-assembly and Encapsulation:
- Mix the E-PA and K-PA solutions at a desired molar ratio (e.g., 1:1) in a vial.
- Add the CPT solution to the PA mixture and vortex thoroughly.
- Add deionized water dropwise to the mixture under gentle stirring to a final peptide concentration of 1% (w/v).
- Sonicate the mixture in a bath sonicator for 10 minutes to ensure homogeneity.
- Solvent Evaporation and Harvesting:
- Place the vial in a fume hood overnight to allow the organic solvent to evaporate slowly.
- The resulting suspension can be lyophilized for storage or used directly for characterization and in vitro testing.
Protocol: Characterizing Drug Release from PA Nanofiber Gels
This protocol outlines methods to create a nanofiber gel and quantify the release kinetics of an encapsulated payload, based on studies that achieved near zero-order release [45].
Materials & Reagents
- PA Solution: PA functionalized with a drug or a model fluorophore (e.g., Prodan).
- Gelling Agent: Calcium Chloride (CaCl₂) solution or other divalent cation solution.
- Release Medium: Phosphate Buffered Saline (PBS), pH 7.4.
- Equipment: Fluorescence Spectrophotometer, Cryogenic Transmission Electron Microscope (Cryo-TEM), Circular Dichroism (CD) Spectrometer, Dialysis membrane or centrifugal filters.
Procedure
- Nanofiber Gel Formation:
- Prepare an aqueous solution of the drug-loaded PA.
- Add a calculated volume of CaCl₂ solution to screen the charges on the PA molecules, initiating self-assembly and gelation. Gently mix to form a homogeneous gel.
- In Vitro Release Study:
- Place the PA gel in a tube containing a known volume of pre-warmed PBS (release medium).
- Agitate the tube in a shaking incubator at 37°C.
- At predetermined time intervals, withdraw a sample of the release medium and replace it with an equal volume of fresh PBS to maintain sink conditions.
- Quantification and Analysis:
- Analyze the concentration of the released drug in the samples using a fluorescence spectrophotometer (for fluorophores) or HPLC (for drugs).
- Plot the cumulative drug release (%) versus time to generate release kinetics profiles.
- Use techniques like Cryo-TEM and CD spectroscopy to correlate release rates with nanofiber morphology and secondary structure (β-sheet content) of the PA.
Pathway and Workflow Visualizations
Molecular Design to Release Control
Experimental Workflow for PA-Drug Formulation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PA-Based Drug Delivery Research
| Item | Function/Application in Research | Key Considerations |
|---|---|---|
| Palmitic Acid (C16) | Standard hydrophobic tail conjugated to N-terminus of peptide to create the PA [3]. | Chain length can be varied to tune hydrophobic interaction strength and nanostructure stability [48]. |
| β-Sheet Forming Sequences (e.g., VVVAAA, AAAAA) | Forms hydrogen-bonded backbone driving 1D nanofiber growth [3] [46]. | Sequence impacts core packing density, affecting drug release rate [45]. |
| Charged Amino Acids (e.g., E, K) | Provide aqueous solubility and a trigger for gelation via charge screening [3]. | Oppositely charged PAs can be co-assembled for synergistic encapsulation [46]. |
| Cell-Penetrating Peptides (e.g., TAT) | Enhances cellular uptake of conjugates; can be incorporated into PAs [47] [49]. | The basic domain (e.g., RKKRRQRRR) is crucial for translocation activity [47]. |
| Solvatochromic Dye (Prodan) | Model hydrophobic payload for studying release kinetics from PA gels [45]. | Its fluorescence properties can report on the local microenvironment. |
| Camptothecin (CPT) | Model hydrophobic chemotherapeutic drug for encapsulation studies [46]. | Used to validate encapsulation efficiency and anti-tumor efficacy in vitro. |
| Divalent Cations (Ca²⁺) | Screens negative charges on PA molecules, triggering self-assembly into nanofiber gels [45]. | Concentration controls the kinetics and final mechanical properties of the gel. |
Addressing Scalability and Manufacturing Challenges for Clinical Translation
The translation of sprayable peptide amphiphile (PA) nanofibers from promising laboratory constructs to clinically viable wound healing therapies necessitates overcoming significant scalability and manufacturing challenges. These supramolecular biomaterials, which emulate the fibrous architecture of the native extracellular matrix (ECM), offer exceptional potential for advanced wound care due to their bioactive epitope presentation, injectable shear-thinning properties, and ability to create favorable microenvironments for tissue regeneration [3] [5]. However, their clinical adoption depends on developing robust, reproducible, and scalable production methodologies that maintain critical quality attributes (CQAs) throughout the manufacturing process. This application note details standardized protocols and analytical strategies to address these translational barriers, providing researchers with a framework to advance PA nanofiber technologies toward commercial and clinical reality.
Quantitative Characterization of PA Nanofibers
A comprehensive characterization strategy is foundational to process development and quality control. The following table summarizes the essential quantitative analyses required to define CQAs for PA nanofibers.
Table 1: Essential Quantitative Analyses for PA Nanofiber Characterization
| Analysis Parameter | Technique(s) | Key Outcome Measures | Significance for Scalability |
|---|---|---|---|
| Molecular Weight & Purity | Liquid Chromatography-Mass Spectrometry (LC-MS) | Molecular ion peak confirmation, purity percentage [5] | Ensures batch-to-batch consistency of the PA monomer building blocks. |
| Critical Assembly Concentration (CAC) | Nile Red Assay, Pyrene Assay | Concentration at which supramolecular polymerization initiates [5] | Determines optimal and cost-effective working concentrations for large-scale production. |
| Secondary Structure & Internal Ordering | Circular Dichroism (CD) | Spectral minima/maxima indicating β-sheet content (e.g., ~218 nm) [3] [5] | Correlates internal fiber structure with mechanical and bioactive properties. |
| Nanofiber Morphology | Transmission Electron Microscopy (TEM), Cryo-TEM | Fiber diameter, length, and aspect ratio; network structure [3] [5] [30] | Defines the primary nanostructure and confirms self-assembly post-processing (e.g., spraying). |
| Viscoelastic Properties | Rheology | Storage (G') and Loss (G'') moduli, shear-thinning behavior, recovery kinetics [5] | Critical for sprayability and in-situ scaffold formation; must be maintained after scale-up. |
| Biocompatibility | Lactate Dehydrogenase (LDH) Assay, Cell Viability Assays (e.g., MTT) | Percentage cytotoxicity, cell viability relative to controls [5] | Mandatory safety profile; must be consistent across scaled batches. |
| Biofunctional Efficacy | Cell-based Assays (e.g., Endothelial Tube Formation) | Quantifiable metrics (e.g., tube length, branch points) [5] | Confirms biological activity of the final product is retained. |
Detailed Experimental Protocols
Protocol: Solid-Phase Peptide Synthesis (SPPS) and Purification of PA Monomers
This protocol outlines the synthesis of peptide amphiphiles, which is the first critical step in manufacturing.
Principle: PA monomers are synthesized from the C- to N-terminus on a solid support (resin), followed by cleavage and purification. The hydrophobic tail (e.g., palmitic acid) is typically conjugated to the N-terminus of the peptide sequence [3] [8].
Materials:
- Rink Amide MBHA resin (or other suitable solid support)
- Fmoc-protected amino acids
- Palmitic acid
- Coupling reagents: HBTU/HATU and DIPEA
- Deprotection reagent: 20% Piperidine in DMF
- Cleavage cocktail: Trifluoroacetic acid (TFA), Triisopropylsilane (TIS), Water
- Solvents: Dimethylformamide (DMF), Diethyl ether, Acetonitrile (HPLC grade)
- Purification System: Preparative High-Performance Liquid Chromatography (HPLC)
Procedure:
- Resin Swelling: Place the resin in a peptide synthesis vessel and swell with DMF for 30 minutes.
- Fmoc Deprotection: Drain the DMF and treat the resin with 20% piperidine in DMF (2 x 10 minutes) to remove the Fmoc protecting group. Wash thoroughly with DMF.
- Amino Acid Coupling: For each amino acid in the sequence (from C- to N-terminus):
- Pre-activate 4 equivalents of the Fmoc-protected amino acid with 4 equivalents of HBTU and 8 equivalents of DIPEA in DMF.
- Add the activated amino acid solution to the resin and agitate for 1-2 hours.
- Drain and wash the resin with DMF. Perform a Kaiser test to confirm coupling completion. Repeat coupling if necessary.
- Palmitic Acid Coupling: After the final Fmoc deprotection, couple palmitic acid using the same method as step 3.
- Final Cleavage and Deprotection: Wash the resin with DMF and dichloromethane (DCM) and dry. Treat the resin with a cleavage cocktail (e.g., TFA/TIS/Water, 95:2.5:2.5) for 2-4 hours to cleave the PA from the resin and remove all side-chain protecting groups.
- Precipitation and Isolation: Filter the cleavage mixture into cold diethyl ether to precipitate the crude PA. Centrifuge to pellet the product and wash with cold ether.
- Purification: Dissolve the crude pellet in HPLC-grade acetonitrile/water and purify using preparative reverse-phase HPLC.
- Analysis and Storage: Verify the molecular weight and purity of the collected fractions using analytical LC-MS [5]. Lyophilize the pure PA and store at -20°C.
Protocol: Supramolecular Polymerization and Nanofiber Gel Formation
This protocol describes the assembly of PA monomers into nanofibers and the formation of a gel suitable for spray delivery.
Principle: PA molecules self-assemble in aqueous environments driven by hydrophobic collapse of the alkyl tails and hydrogen bonding within the β-sheet-forming peptide region [3]. Gelation can be triggered by ionic crosslinking with divalent cations present in physiological fluids [5].
Materials:
- Purified PA monomer
- Sterile, deionized water
- Phosphate Buffered Saline (PBS) or Dulbecco's Phosphate Buffered Saline (DPBS)
- pH meter and adjusters (e.g., NaOH, HCl)
- Bath sonicator
- Vortex mixer
Procedure:
- Primary Nanofiber Assembly:
- Dissolve the lyophilized PA in sterile water at a concentration above its predetermined CAC (e.g., 1% w/v). This may require brief sonication and vortexing to fully dissolve the PA.
- Adjust the pH to 7.4 using dilute NaOH to ensure the charged residues are deprotonated, promoting nanofiber growth through charge screening [3].
- Aging/Annealing: To achieve a thermodynamically stable nanofiber population, either:
- Gelation via Ionic Crosslinking:
- Combine the pre-assembled PA solution with an equal volume of a DPBS solution containing Ca²⁺ and Mg²⁺ ions. Alternatively, a solution of specific divalent cations (e.g., CaCl₂) can be used.
- Gently mix to initiate ionic crosslinking via chelation with terminal carboxylic acid groups on the PA nanofibers, leading to the formation of a self-supporting hydrogel [5].
- Post-Assembly Characterization: Confirm nanofiber formation and morphology using TEM and CD spectroscopy as outlined in Table 1.
Protocol: Functional Assessment of Pro-Angiogenic PA Nanofibers
This protocol provides a method to validate the bioactivity of PA nanofibers functionalized with angiogenic epitopes (e.g., VEGF-mimetic peptides).
Principle: The success of wound healing therapies depends on revascularization. An in vitro endothelial cell tube formation assay assesses the material's ability to promote angiogenesis [5].
Materials:
- Endothelial Cells (e.g., Human Umbilical Vein Endothelial Cells - HUVECs)
- Reduced Growth Factor (RGF) Basement Membrane Extract (BME)
- Cell culture media and supplements
- PA nanofiber gel (test material) and control (e.g., non-bioactive PA gel)
- Confocal microscopy equipment
Procedure:
- Matrix Preparation: Thaw BME on ice and pipet a pre-determined volume (e.g., 50 µL) into each well of a pre-chilled multi-well plate. Incubate the plate at 37°C for 30 minutes to allow the BME to polymerize.
- Sample Application: Gently overlay the polymerized BME with the PA nanofiber gel or control.
- Cell Seeding: Trypsinize, count, and resuspend HUVECs in serum-free media. Seed the cells directly onto the surface of the test and control gels at a standardized density (e.g., 1.0 x 10⁴ cells per well).
- Incubation and Imaging: Incubate the plate at 37°C, 5% CO₂ for 4-16 hours.
- Analysis: After incubation, image the wells using a microscope. Quantify the pro-angiogenic response by measuring the total tube length, number of branch points, and number of meshes per field of view using image analysis software. Compare results between the bioactive PA and the control [5].
Pathway and Workflow Visualizations
PA Nanofiber Self-Assembly Mechanism
Scalable Manufacturing and Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for PA Nanofiber Research and Development
| Category | Item | Function/Application | Key Considerations |
|---|---|---|---|
| Synthesis | Fmoc-Amino Acids | Building blocks for PA sequence | Purity >99%; sequence defines bioactivity and assembly [3] [8] |
| Palmitic Acid | Standard hydrophobic tail | Conjugated to N-terminus to drive hydrophobic collapse [3] | |
| Solid Support (Resin) | Platform for SPPS | Rink Amide MBHA resin common for C-terminal amidation [8] | |
| Assembly & Formulation | DPBS / CaCl₂ Solution | Ionic crosslinker | Triggers gelation upon contact with PA nanofibers [5] |
| pH Adjusters (NaOH/HCl) | Charge screening | Controls self-assembly kinetics and fiber dimensions [3] | |
| Characterization | Nile Red Dye | Fluorescent probe for CAC determination | Emission spectrum shifts in hydrophobic environments [5] |
| LDH Assay Kit | Cytotoxicity measurement | Quantifies cell membrane damage for biocompatibility [5] | |
| Bioactivity Testing | Endothelial Cells (HUVECs) | Angiogenesis model | For tube formation assays to test pro-angiogenic PAs [5] |
| Basement Membrane Extract (BME) | Synthetic ECM for cell assays | Provides a substrate for endothelial network formation [5] |
Ensuring Sterility and Stability of Supramolecular Formulations
Supramolecular systems, particularly sprayable peptide amphiphile (PA) nanofibers, represent a transformative approach in advanced wound healing research [3]. These materials are designed to emulate the fibrous architecture of the native extracellular matrix (ECM), providing a bioactive scaffold that supports cell adhesion, proliferation, and tissue regeneration [3]. A typical PA molecule incorporates a alkyl tail for hydrophobic collapse, a β-sheet forming peptide sequence to drive one-dimensional assembly, charged amino acids for water solubility and salt-responsive gelation, and a bioactive epitope (e.g., RGDS or IKVAV) at the terminus to interact with cells [3]. The functionality of these systems hinges on their precise supramolecular structure, which is assembled and maintained through dynamic non-covalent interactions. This application note details critical protocols and analytical methods to ensure the sterility and stability of these sophisticated formulations, guaranteeing their performance and safety from benchtop to bedside.
Key Stability Challenges in Supramolecular Systems
The translation of supramolecular biomaterials from laboratory research to clinical applications is contingent upon overcoming significant stability and sterility challenges. The dynamic and reversible nature of the non-covalent interactions that underpin these systems, while central to their functionality, also renders them susceptible to disruption under physiological conditions.
The table below summarizes the primary stability challenges and the associated mechanisms that can compromise the integrity and performance of supramolecular formulations.
Table 1: Key Stability Challenges for Supramolecular Formulations
| Challenge Category | Specific Challenge | Impact on Formulation |
|---|---|---|
| Structural Integrity | Thermodynamic instability of non-covalent bonds [50] | Compromised nanofiber morphology and premature disassembly. |
| Susceptibility to enzymatic degradation [50] | Loss of structural integrity and bioactive signal presentation. | |
| Performance in Biological Environments | Protein corona formation [50] | Obscured targeting ligands, reduced cellular specificity. |
| Inadequate specificity of environmental responsiveness [50] | Off-target activation and uncontrolled drug release. | |
| Manufacturing & Sterilization | Scalability and batch-to-batch consistency [50] | Difficulty in reproducing therapeutic efficacy. |
| Structural damage from sterilization processes | Alteration of nanofiber morphology and bioactivity. |
Experimental Protocols for Sterility and Stability Assessment
Protocol for the Aseptic Preparation and Sterilization of PA Solutions
This protocol describes the preparation of sterile PA solutions suitable for electrospinning or direct sprayable gel formation, utilizing filter sterilization to preserve supramolecular integrity.
Principle: To achieve sterility without exposing the pre-assembled nanofibers to harsh conditions that may cause aggregation or disassembly, the PA monomer solution is sterilized prior to the self-assembly process.
Materials:
- Peptide amphiphile (PA) stock solution (1-5% w/v in sterile water or compatible buffer)
- Sterile syringes (e.g., 5 mL, 10 mL)
- Syringe filter, 0.22 µm pore size (e.g., PVDF or PES membrane)
- Sterile collection vial
- Laminar flow hood
- pH meter
Procedure:
- Preparation: Dissolve the PA in a suitable aqueous solvent (e.g., ultrapure water, 10 mM PBS) under aseptic conditions within a laminar flow hood to a final concentration of 1-5% w/v.
- pH Adjustment: Adjust the pH of the solution as required to maintain PA solubility and prevent premature self-assembly. Monitor pH carefully as it is a critical process parameter (CPP).
- Filtration: Draw the PA solution into a sterile syringe. Attach a 0.22 µm syringe filter. Gently and steadily push the plunger to filter the solution into a sterile collection vial. Note: Avoid using filters with cellulose acetate membranes if the solvent contains DMSO.
- Sterility Check: Follow the guidelines in section 3.3 to confirm the sterility of the filtered solution.
- Triggered Assembly: The sterile PA solution can now be used to initiate nanofiber formation. For sprayable gels, this is typically achieved by mixing with a sterile solution containing ions (e.g., cell culture media, simulated body fluid) to trigger salt-mediated self-assembly immediately upon application [3].
Protocol for Assessing Supramolecular Stability via Spectroscopy and Microscopy
This protocol outlines methods to characterize the structural stability of PA nanofibers under simulated physiological conditions.
Principle: To monitor the stability of the supramolecular architecture over time by analyzing changes in secondary structure (via Circular Dichroism) and nanoscale morphology (via Scanning Electron Microscopy).
Materials:
- PA nanofiber hydrogel or solution
- Simulated physiological buffer (e.g., PBS at pH 7.4)
- Circular Dichroism (CD) spectropolarometer
- Quartz cuvette with short path length (e.g., 0.1 cm)
- Scanning Electron Microscope (SEM)
- Sample stubs and sputter coater
Procedure: Part A: Secondary Structure Analysis by Circular Dichroism (CD)
- Sample Preparation: Dilute the PA nanofiber suspension in the appropriate buffer to a concentration that provides an adequate signal (typically 0.1-0.5 mg/mL).
- Baseline Measurement: Place the buffer solution in the quartz cuvette and acquire a baseline spectrum.
- Sample Measurement: Replace the buffer with the PA sample and acquire the CD spectrum across a wavelength range of 190-260 nm.
- Data Analysis: Monitor the characteristic spectral features. A dominant negative peak at approximately 218 nm is indicative of a β-sheet-rich secondary structure, which is the hallmark of properly assembled PA nanofibers [3]. A decrease in the intensity of this peak over time indicates a loss of β-sheet structure and nanofiber instability.
Part B: Morphological Analysis by Scanning Electron Microscopy (SEM)
- Sample Preparation: Apply a small volume of the PA nanofiber solution to a clean SEM sample stub.
- Fixation: To preserve structure, gently rinse the sample with deionized water and then fix with a 2.5% glutaraldehyde solution for 1-2 hours.
- Dehydration: Dehydrate the sample through a graded series of ethanol solutions (e.g., 30%, 50%, 70%, 90%, 100%).
- Drying and Coating: Critical point dry the sample or allow it to air dry. Sputter-coat the sample with a thin layer of gold/palladium.
- Imaging: Observe the sample under SEM. Stable PA formulations will display a homogeneous population of high-aspect-ratio nanofibers with diameters typically in the range of 5-20 nm [3]. The presence of spherical aggregates or fragmented fibers is a sign of instability.
Protocol for Sterility Testing According to Compendial Methods
This protocol describes the standard test for sterility to ensure the absence of viable microorganisms in the final supramolecular formulation.
Principle: To demonstrate that the PA formulation does not support microbial growth by incubating it in nutrient-rich media.
Materials:
- Fluid Thioglycollate Medium (FTM)
- Soybean-Casein Digest Medium (SCDM)
- Sterile syringes and transfer needles
- Incubators set at 20-25°C and 30-35°C
- Positive control organisms (e.g., Staphylococcus aureus, Pseudomonas aeruginosa)
Procedure:
- Sample Transfer: Aseptically transfer the specified volume of the sterile PA formulation (as per USP guidelines) into containers of FTM and SCDM.
- Incubation:
- Incubate the FTM containers at 30-35°C for not less than 14 days.
- Incubate the SCDM containers at 20-25°C for not less than 14 days.
- Controls:
- Negative Control: Incubate un-inoculated media to confirm its sterility.
- Positive Control: Inoculate separate containers of media with a small number of viable microorganisms to demonstrate the media's ability to support growth.
- Observation and Interpretation: Examine the media for signs of microbial growth (turbidity) daily. The formulation meets the requirements for sterility if no growth is observed in the test containers, while growth occurs in the positive control containers.
Quantitative Stability and Performance Data
Rigorous quantitative assessment is essential for establishing the shelf-life and in-vivo performance of supramolecular wound dressings. The following table compiles key stability and functionality metrics for different formulation types, based on data from recent literature.
Table 2: Stability and Performance Metrics of Supramolecular Formulations
| Formulation Type | Key Stability / Performance Metric | Test Method | Reported Value |
|---|---|---|---|
| Soluplus/Soy Protein Isolate Nanofibers [14] | In vitro degradability (5 days) | Mass loss in buffer | 33.73 ± 3.55% |
| Ultimate Tensile Strength | Mechanical testing | 3.61 ± 0.29 MPa | |
| Drug Release Profile (5 days) | In vitro release assay | 85.90 ± 6.02% | |
| Antibacterial Efficacy (% kill) | Against S. aureus and E. coli | 93.06 ± 5.40% and 90.40 ± 5.66% | |
| Sprayable GelMA-DOPA Hydrogel [22] | Adhesive Strength | Lap-shear test | ~2.5-fold increase vs control |
| ROS-Scavenging Capacity | DPPH assay | >80% scavenging | |
| Antibacterial Efficacy (in vivo) | Reduction in bacterial load in wound model | ~90% reduction vs control | |
| Host-Guest Supramolecular Material (FcP15@β-CD) [51] | Deposition & Retention on Leaf | SEM, adhesion tests | Improved lamellar structure for surface retention |
| Antibacterial Efficacy (EC50) | Turbidimetric assay | 4.45 µg/mL |
The Scientist's Toolkit: Essential Research Reagents
The table below lists key materials and their functions for developing and testing sterile supramolecular formulations for wound healing.
Table 3: Research Reagent Solutions for Supramolecular Formulations
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Peptide Amphiphiles (PAs) [3] | Core building block for self-assembling nanofibers. | Sequence must include alkyl tail, β-sheet segment, charged residues, and bioactive epitope. |
| Syringe Filter (0.22 µm) | Sterile filtration of monomeric PA solutions. | Use PVDF or PES membranes for broad solvent compatibility; avoid cellulose acetate for organic solvents. |
| Simulated Body Fluid (SBF) | Triggering salt-mediated self-assembly of PAs into nanofibers [3]. | Ionic strength is a Critical Process Parameter (CPP) for gelation kinetics and fiber morphology. |
| GelMA-DOPA [22] | Photocrosslinkable, adhesive hydrogel backbone for sprayable dressings. | Functionalized with catechol motifs for enhanced binding to wound surfaces. |
| Antimicrobial Peptides (AMPs) [22] | Broad-spectrum antibacterial agents for incorporation into dressings. | Targets bacterial membranes, reducing risk of resistance compared to traditional antibiotics. |
| Cerium Oxide Nanoparticles (CeONs) [22] | Reactive Oxygen Species (ROS)-scavenging additive. | Mitigates oxidative stress in the wound bed, promoting healing and reducing scarring. |
Stability Challenge and Testing Pathway
The following diagram visualizes the stability challenges faced by supramolecular formulations and the corresponding testing pathway to address them, integrating the protocols described in this document.
Diagram 1: A workflow mapping stability challenges to corresponding testing protocols and key success metrics for supramolecular formulations.
The clinical translation of sprayable supramolecular nanofiber formulations is critically dependent on a rigorous and systematic approach to ensuring sterility and stability. The protocols and data outlined in this application note provide a foundational framework for researchers. By implementing aseptic preparation techniques, employing a suite of physico-chemical and biological stability assays, and adhering to compendial sterility tests, developers can generate the robust data required to advance these promising peptide amphiphile-based therapies through the development pipeline and into clinical application for wound healing.
Adapting Material Properties for Specific Wound Microenvironments
The wound healing process is a dynamic cascade that creates distinct biochemical and cellular microenvironments through its coordinated stages: hemostasis, inflammation, proliferation, and remodeling [13] [52]. Chronic wounds, which affect over 150 million people globally, represent a significant healthcare challenge characterized by pathological microenvironments featuring microbial colonization, dysregulated inflammation, and impaired regenerative processes [53]. These pathological states create specific challenges that can be addressed through advanced material design.
Sprayable peptide amphiphile (PA) nanofibers represent an emerging platform technology that can be engineered to respond to these dynamic wound conditions [30]. PAs are composed of palmitic acid conjugated to peptides with β-sheet hydrogen bonding domains, enabling self-assembly into high-aspect-ratio nanofibers in aqueous solutions [30]. Their modular design allows for the incorporation of bioactive sequences that participate in surface receptor binding and intracellular signaling, making them ideal for creating responsive wound therapies. By functionalizing these nanofibers with microenvironment-sensitive components, researchers can create intelligent dressings that adapt their properties to the specific pathological features of different wound types.
Key Wound Microenvironment Parameters and Material Adaptation Strategies
The table below summarizes the primary pathological features of compromised wound microenvironments and corresponding material adaptation strategies using PA nanofiber technology.
Table 1: Wound Microenvironment Parameters and Material Adaptation Strategies
| Microenvironment Parameter | Pathological Significance | Material Adaptation Strategy | PA Nanofiber Functionalization |
|---|---|---|---|
| Elevated Protease Levels | Matrix metalloproteinases (MMPs) and bacterial proteases degrade ECM and endogenous growth factors, impeding healing [13] | Incorporate protease-resistant D-amino acids or cyclic peptide structures; use MMP-cleavable linkers for controlled drug release [13] | Engineered with non-canonical amino acids or stabilized β-sheet structures to resist degradation |
| Microbial Colonization & Biofilms | Bacterial biofilms prevent antibiotic penetration and perpetuate inflammation; >90% of chronic wounds contain biofilms [14] | Integrate broad-spectrum antimicrobial peptides (AMPs) with anti-biofilm activity; design materials with charge-based microbial membrane disruption [13] | Functionalization with AMPs like LL-37 or synthetic mimics; cationic surface charge for membrane disruption |
| pH Variation | Chronic wounds often exhibit alkaline pH (7.2-8.9) versus normal skin (pH 4-6); infected wounds show localized acidosis [53] | Implement pH-responsive structural changes or drug release via acid-labile bonds (e.g., hydrazone, acetal) [54] | Incorporation of pH-sensitive ionizable groups that alter nanofiber assembly/disassembly |
| Redox Imbalance | Elevated reactive oxygen species (ROS) and altered glutathione levels in chronic wounds create oxidative stress [30] | Integrate ROS-scavenging moieties (e.g., phenylboronic acid); utilize ROS/glutathione-cleavable linkages for controlled therapeutic release [30] | ROS-sensitive proline linkages or glutathione-responsive disulfide bonds (SPDP/NDEC chemistry) for targeted drug release |
| Moisture & Exudate Levels | Varying exudate composition and volume affect healing; excessive moisture causes maceration while dryness impedes cell migration [52] | Design tunable fluid absorption capacity through controlled hydrophilicity/hydrophobicity balance and porosity [11] | Modulation of PA side chain chemistry to control hydration and swelling properties |
Quantitative Performance Data of Advanced Wound Dressings
Recent studies have demonstrated the efficacy of various advanced dressing formats in addressing specific wound microenvironment challenges. The following table compares the performance metrics of different material platforms relevant to PA nanofiber development.
Table 2: Performance Metrics of Advanced Wound Dressing Materials
| Material Platform | Antimicrobial Efficacy | Drug Release Profile | Mechanical Properties | Biocompatibility & Healing Outcomes |
|---|---|---|---|---|
| Soluplus-SPI-Mupirocin Nanofibers [14] | 93.06% reduction of S. aureus; 90.40% reduction of E. coli within 24 hours | 85.90% mupirocin release over 5 days; sustained release kinetics | Tensile strength: 3.61 ± 0.29 MPa; Elongation: 59.11 ± 1.94% | Significant acceleration of re-epithelialization in rat model; high HaCat keratinocyte viability |
| AMP-Loaded Hydrogels [13] | Broad-spectrum activity against drug-resistant pathogens; 3-4 log reduction in bacterial load | Controlled release over 3-7 days depending on hydrogel cross-linking density | Storage modulus (G'): 0.5-5 kPa, tunable to match skin mechanical properties | Enhanced angiogenesis; reduced inflammation; stimulated epithelial migration |
| Chitosan-Based Nanofibers [11] | >90% inhibition of common wound pathogens due to cationic antimicrobial action | Variable release profiles from rapid (24h) to sustained (5-7 days) based on fiber composition | Fiber diameter: 100-500 nm; Porosity: 80-90% for exudate management | Excellent hemostatic properties; promoted fibroblast proliferation and migration |
| Electrospun Polysaccharide Fibers [11] | Antimicrobial when functionalized with AgNPs or AMPs; inhibition zones of 8-12mm in disc diffusion | Diffusion-controlled release through nanofiber matrix over 72-120 hours | High specific surface area (20-40 m²/g) for enhanced cell-naterial interactions | ECM-mimetic structure supports cell adhesion and proliferation |
Experimental Protocols for PA Nanofiber Characterization and Testing
Protocol: Synthesis of Responsive PA Nanofibers for Wound Applications
Objective: To synthesize and characterize stimulus-responsive PA nanofibers capable of releasing therapeutic agents in specific wound microenvironments.
Materials:
- Fmoc-protected amino acids
- Rink amide MBHA resin
- Palmitic acid
- Succinimidyl 3-(2-pyridyldithio)propionate (SPDP) or 4-nitrophenyl 2-(2-pyridyldithio)ethyl carbonate (NDEC)
- Cleavage cocktail (TFA/TIS/water, 95:2.5:2.5)
- Diethyl ether
- Therapeutic agent (LXR agonist, AMP, etc.)
Procedure:
- Solid-Phase Peptide Synthesis:
- Perform standard Fmoc-SPPS on rink amide MBHA resin (0.1 mmol scale)
- Incorporate β-sheet forming sequence (e.g., VVVAAA) at C-terminal
- Add functional peptide sequence (e.g., ApoA1-mimetic for targeting)
- Couple palmitic acid at N-terminal using HBTU/DIPEA activation
Responsive Linker Incorporation:
- For ROS-sensitive PAs: Incorporate proline-rich sequence (e.g., PPPP) as ROS-cleavable linker
- For glutathione-sensitive PAs: React with SPDP or NDEC to introduce disulfide linkages
- Conjugate therapeutic agent through responsive linkage
Cleavage and Purification:
- Cleave from resin using TFA-based cocktail (2 hours, RT)
- Precipitate in cold diethyl ether
- Purify by reverse-phase HPLC, characterize by LC-MS
Nanofiber Self-Assembly:
- Dissolve purified PA in ultrapure water (1% w/v)
- For co-assemblies: Mix with 40 mol% targeting PA (ApoA1-PA) and 50 mol% diluent PA (E2-PA)
- Age at 4°C for 24 hours or anneal (80°C for 30 min, cool gradually to RT)
- Confirm nanofiber formation by cryoTEM [30]
Protocol: In Vitro Assessment of Responsive Drug Release
Objective: To quantify therapeutic agent release from responsive PA nanofibers under simulated wound microenvironment conditions.
Materials:
- Prepared PA nanofibers
- Hydrogen peroxide (250 μM for ROS simulation)
- Tris(2-carboxyethyl)phosphine (TCEP, 10 mM for reducing environment)
- Protease solution (e.g., MMP-9 at 100 ng/mL)
- PBS buffer (pH 5.5, 7.4 for pH response testing)
- Dialysis membranes (MWCO 3.5-7 kDa)
- HPLC system with appropriate detection
Procedure:
- Sample Preparation:
- Place 2 mL of PA nanofiber solution (1% w/v) in dialysis membranes
- Immerse in 50 mL release medium under different conditions:
- Condition A: PBS pH 7.4 + 250 μM H₂O₂ (ROS simulation)
- Condition B: PBS pH 7.4 + 10 mM TCEP (reducing environment)
- Condition C: PBS pH 5.5 (acidic wound environment)
- Condition D: PBS pH 7.4 + MMP-9 (protease-rich environment)
- Condition E: PBS pH 7.4 (control)
Release Kinetics:
- Incubate at 37°C with gentle shaking (50 rpm)
- Withdraw 1 mL aliquots at predetermined time points (1, 3, 6, 12, 24, 48, 72h)
- Replace with fresh medium to maintain sink conditions
- Analyze samples by HPLC to quantify drug release
- Calculate cumulative release percentage [30]
Data Analysis:
- Plot cumulative release versus time for each condition
- Determine release kinetics using mathematical models (zero-order, first-order, Higuchi)
- Compare release profiles to identify microenvironment-specific responsiveness
Protocol: Antimicrobial and Anti-Biofilm Efficacy Testing
Objective: To evaluate the antimicrobial and anti-biofilm activity of functionalized PA nanofibers against common wound pathogens.
Materials:
- Test organisms: Staphylococcus aureus (ATCC 25923), Pseudomonas aeruginosa (ATCC 27853)
- Mueller-Hinton broth
- Crystal violet solution (0.1%)
- 96-well polystyrene plates
- MTT solution (5 mg/mL in PBS)
Procedure:
- Antimicrobial Susceptibility Testing:
- Prepare bacterial suspensions at ~1×10⁸ CFU/mL in Mueller-Hinton broth
- Add 100 μL to wells containing 100 μL of PA nanofiber solutions at various concentrations
- Incubate 24h at 37°C
- Measure OD600 to determine growth inhibition
- Calculate percentage reduction compared to untreated controls [14]
Anti-Biofilm Activity:
- Add 200 μL bacterial suspension (1×10⁶ CFU/mL) to wells and incubate 48h at 37°C to form biofilms
- Treat established biofilms with PA nanofiber solutions for 24h
- Remove planktonic cells and stain adherent biofilm with 0.1% crystal violet (15 min)
- Destain with 30% acetic acid, measure OD590 to quantify biofilm biomass [13]
Time-Kill Kinetics:
- Exponentially growing bacteria to PA nanofibers at 1× and 4× MIC
- Take samples at 0, 2, 4, 6, 8, and 24h, serially dilute and plate on agar
- Count colonies after 24h incubation to determine bactericidal kinetics
Signaling Pathways and Experimental Workflows
Diagram 1: PA Nanofiber Responsive Mechanisms in Wound Microenvironments
Diagram 2: PA Nanofiber Development and Testing Workflow
Research Reagent Solutions for Wound Microenvironment Studies
Table 3: Essential Research Reagents for PA Nanofiber Wound Healing Applications
| Reagent Category | Specific Examples | Function & Application | Key Considerations |
|---|---|---|---|
| Peptide Synthesis | Fmoc-amino acids, Rink amide MBHA resin, HBTU/HATU, Palmitic acid | Solid-phase peptide synthesis of PA backbone; hydrophobic domain incorporation | Purity >95%; sequence verification by MS; scale: 0.1-0.25 mmol for initial studies |
| Responsive Linkers | SPDP, NDEC, N-succinimidyl S-acetylthioacetate (SATA) | Introduce disulfide bonds for glutathione-responsive release; enable therapeutic conjugation | Cleavage efficiency validation under physiological reductant concentrations (10 mM GSH) |
| Therapeutic Agents | LL-37, IDR-1018, LXR agonists (GW3965), Growth factors (VEGF, FGF) | Antimicrobial, immunomodulatory, or pro-regenerative activities; primary therapeutic effects | Stability in formulation; release kinetics matching clinical need (3-7 days sustained) |
| Characterization Tools | LC-MS, cryoTEM, SAXS, FTIR, BET surface area analyzer | Structural verification; nanofiber morphology; secondary structure; porosity assessment | Multi-technique approach recommended for comprehensive characterization |
| Biological Assays | Bacterial strains (S. aureus, P. aeruginosa), HaCat keratinocytes, MTT assay kits | Antimicrobial efficacy testing; cytocompatibility assessment; cellular response evaluation | Follow CLSI guidelines for antimicrobial testing; use relevant cell lines for wound healing |
| Animal Models | Diabetic db/db mice, splinted excision wound models | In vivo efficacy studies; wound closure kinetics; histopathological analysis | Appropriate model selection critical for clinical translation prediction |
The adaptation of material properties to specific wound microenvironments represents a paradigm shift in wound care, moving from passive coverage to active, dynamic intervention. Sprayable PA nanofibers offer a particularly promising platform due to their modular design, bioresponsive capabilities, and biomimetic properties. As research advances, the integration of sensing and feedback mechanisms within these materials will enable truly intelligent wound dressings that can autonomously adjust their therapeutic actions based on real-time assessment of wound status.
Future developments in this field will likely focus on enhancing the sophistication of microenvironment responsiveness, potentially incorporating multiple stimulus-sensitive mechanisms within a single material system. Additionally, the combination of PA nanofibers with complementary technologies such as biosensors, electrical stimulation modalities, and advanced drug delivery systems will further expand their therapeutic potential. As standardization in testing protocols improves and manufacturing scalability advances, these innovative material strategies promise to significantly impact clinical outcomes for patients with complex and chronic wounds.
Proof of Efficacy: Preclinical Models and Comparative Clinical Advantages
Sprayable peptide amphiphile (PA) nanofibers represent a groundbreaking therapeutic strategy in regenerative medicine, particularly for burn wound healing. These supramolecular nanomaterials are engineered to mimic the native extracellular matrix (ECM), providing a bioactive scaffold that supports cellular processes critical for tissue repair [3]. The core innovation lies in the molecular design of PAs, which self-assemble under physiological conditions into nanofibrous gels that can be delivered via minimally invasive sprayable formats [3] [30]. This application note details standardized in vitro protocols for validating the efficacy of bioactive PA nanofiber gels in enhancing the proliferation of thermally damaged cells, providing researchers with a framework for evaluating novel PA formulations before advancing to in vivo models.
The molecular architecture of peptide amphiphiles typically incorporates four key regions: a hydrophobic alkyl tail for driving self-assembly through hydrophobic collapse, a β-sheet forming peptide segment to enforce one-dimensional nanofiber growth, charged amino acids for solubility and salt-responsive gelation, and a terminal bioactive epitope for specific cellular interactions [3]. This versatile design enables the creation of nanofibers that display high densities of bioactive signals, such as the RGDS (Arg-Gly-Asp-Ser) epitope found in fibronectin, which promotes cell adhesion through integrin binding [12] [3].
Experimental Design
Research Objectives and Rationale
This protocol aims to quantitatively evaluate the capacity of PA nanofiber gels to enhance the proliferation of thermally damaged cells in vitro. The experimental design utilizes standardized burn injury models on relevant cell types to simulate the cellular environment of burn wounds, enabling high-throughput screening of PA formulations before advancing to animal studies. The central hypothesis is that PA nanofibers displaying specific bioactive signals create a microenvironment conducive to cell proliferation and migration, thereby accelerating the early stages of wound healing [12].
The rationale is grounded in the understanding that deep partial and full-thickness burns heal slowly with standard wound care alone, primarily due to the extensive damage to both epidermal and dermal structures and the compromised regenerative capacity of resident cells [12]. By providing an ECM-mimetic scaffold with integrated bioactive cues, PA nanofibers directly address this clinical challenge at the cellular level.
Key Signaling Pathways in Wound Healing
The following diagram illustrates the primary cellular signaling pathways involved in wound healing that are targeted by PA nanofiber interventions:
Diagram 1: Key cellular signaling pathways targeted by PA nanofibers in wound healing. PA nanofibers functionalized with RGDS epitopes promote integrin binding and focal adhesion formation, activating downstream signaling pathways including PDGF, TGF-β, and VEGF that collectively enhance cell proliferation, migration, and tissue remodeling [12] [55].
Materials and Reagents
Research Reagent Solutions
Table 1: Essential research reagents for in vitro validation of PA nanofibers on thermally damaged cells
| Reagent/Material | Function/Application | Specifications |
|---|---|---|
| RGDS-Modified PA | Bioactive nanofiber component displaying cell adhesion epitope | Custom synthesis; 1-10 mg/mL in aqueous solution [12] |
| Non-bioactive PA | Control nanofiber without signaling epitopes | Custom synthesis; matched concentration to bioactive PA [12] |
| Human Dermal Fibroblasts | Primary cell model for thermal damage studies | Commercially sourced; passages 3-8 recommended [12] |
| HUVECs | Endothelial cell model for vascularization studies | Commercially sourced; passages 3-6 recommended [12] |
| MTT Assay Kit | Quantitative measurement of cell proliferation | Standard commercial kit; 0.5-1 mg/mL final concentration [12] |
| Cell Culture Medium | Maintenance and experimentation base | DMEM/F12 with 10% FBS and 1% penicillin-streptomycin [12] |
| Thermal Injury Apparatus | Induction of standardized thermal damage | Precision water bath or metal block at 50-60°C [12] |
Peptide Amphiphile Formulations
Table 2: Characterization of peptide amphiphile nanofiber formulations used in proliferation assays
| PA Formulation | Bioactive Sequence | Key Structural Features | Reported Effect on Cell Proliferation |
|---|---|---|---|
| RGDS-PA | Arg-Gly-Asp-Ser | Integrin-binding epitope promotes cell adhesion | Significantly enhanced proliferation of thermally damaged fibroblasts and HUVECs vs. controls [12] |
| IKVAV-PA | Ile-Lys-Val-Ala-Val | Laminin-derived neural adhesion epitope | Promotes neuron attachment and neurite outgrowth; applicable for neural applications [3] |
| ApoA1-PA | Acetyl-AAAAAKEKEKEKEK | Apolipoprotein A1-mimetic peptide | Enables plaque targeting in cardiovascular applications [30] |
| E2 Diluent PA | None | Unmodified diluent for co-assembly | Improves nanofiber formation without direct bioactivity [30] |
Methodology
Experimental Workflow
The following diagram outlines the complete experimental workflow from PA preparation to data analysis:
Diagram 2: Experimental workflow for in vitro validation of PA nanofibers. The complete protocol spans approximately two weeks, beginning with PA preparation and cell culture expansion, followed by thermal damage induction and PA application with subsequent proliferation assessment at multiple time points [12].
PA Nanofiber Preparation and Characterization
PA Solution Preparation: Dissolve lyophilized PA in sterile, ultrapure water at a concentration of 1-10 mg/mL. Sterilize the solution by passing through a 0.22 μm filter. Induce self-assembly into nanofibers by adding 10X phosphate-buffered saline (PBS) to achieve final 1X PBS concentration, or by adjusting pH to neutral using dilute NaOH [3]. For co-assembled systems (e.g., ApoA1-LXR PAs), combine constituent PAs at predetermined molar ratios (typically 40-50% targeting PA, ≤10% therapeutic PA, balance diluent PA) [30].
Nanofiber Characterization: Confirm successful nanofiber formation using cryogenic transmission electron microscopy (cryo-TEM) to visualize nanofiber morphology. Employ circular dichroism (CD) spectroscopy to verify β-sheet secondary structure. Utilize small-angle X-ray scattering (SAXS) to characterize nanofiber geometry and packing parameters [30]. Ensure nanofibers remain stable under physiological conditions (37°C, pH 7.4) for at least 7 days.
Thermal Damage Induction on Cell Cultures
Cell Culture Maintenance: Maintain human dermal fibroblasts and human umbilical vein endothelial cells (HUVECs) in complete medium (DMEM/F12 supplemented with 10% fetal bovine serum and 1% penicillin-streptomycin) at 37°C in a 5% CO₂ atmosphere. Passage cells at 80-90% confluence using standard trypsinization protocols [12].
Thermal Injury Model: Seed cells in 96-well plates at optimized densities (5,000-10,000 cells/well for fibroblasts; 8,000-12,000 cells/well for HUVECs) and culture until 70-80% confluence. Induce thermal damage by partially immersing culture plates in a precision water bath set to 50°C for 30 seconds. Maintain control cells at 37°C. Confirm thermal damage by observing ~50% reduction in viability 24 hours post-injury using MTT assay [12].
Proliferation Assay Protocol
PA Application: Following thermal injury, carefully remove culture medium and immediately apply PA nanofiber gels diluted in fresh culture medium. Test multiple concentrations (0.1-1.0 mg/mL) to establish dose-response relationships. Include appropriate controls: non-treated thermally damaged cells, non-damaged cells, and cells treated with non-bioactive PA nanofibers [12].
Proliferation Kinetics: Assess cell proliferation at 24, 72, 120, and 168 hours post-treatment using MTT colorimetric assay. Briefly, add MTT reagent (0.5 mg/mL final concentration) to each well and incubate for 3-4 hours at 37°C. Carefully remove medium and solubilize formed formazan crystals in dimethyl sulfoxide (DMSO). Measure absorbance at 570 nm with a reference wavelength of 630 nm using a microplate reader [12].
Data Normalization and Analysis: Normalize absorbance values to non-treated thermally damaged controls (set to 100%). Calculate fold-increase in proliferation relative to controls. Perform experiments with a minimum of n=6 replicates per condition and repeat independently three times. Statistical analysis should employ two-way ANOVA with post-hoc Tukey testing to account for multiple comparisons across time points and treatment groups [12].
Results and Data Analysis
Quantitative Proliferation Data
Table 3: Temporal progression of cell proliferation following PA nanofiber treatment
| Cell Type | Treatment Condition | Proliferation Rate (% of Control) at Time Points | |||
|---|---|---|---|---|---|
| 24 hours | 72 hours | 120 hours | 168 hours | ||
| Thermally Damaged Fibroblasts | Non-treated control | 100 ± 8 | 100 ± 7 | 100 ± 9 | 100 ± 6 |
| Non-bioactive PA | 118 ± 9 | 125 ± 10 | 132 ± 8 | 128 ± 11 | |
| RGDS-PA | 145 ± 11 | 187 ± 14 | 210 ± 16 | 225 ± 15 | |
| Thermally Damaged HUVECs | Non-treated control | 100 ± 6 | 100 ± 8 | 100 ± 7 | 100 ± 9 |
| Non-bioactive PA | 115 ± 10 | 122 ± 9 | 119 ± 11 | 121 ± 8 | |
| RGDS-PA | 152 ± 12 | 195 ± 13 | 218 ± 17 | 231 ± 14 |
Data presented as mean ± standard deviation (n=6). RGDS-PA treated groups showed statistically significant enhancement (p<0.01) in proliferation compared to both non-treated controls and non-bioactive PA at all time points beyond 24 hours [12].
Data Interpretation Guidelines
The quantitative data generated through these protocols provides crucial validation of PA nanofiber bioactivity. Key interpretation principles include:
Dose-Response Relationship: Optimal PA concentrations typically fall between 0.5-1.0 mg/mL, with higher concentrations potentially inhibiting proliferation due to altered physical properties or receptor saturation [12].
Temporal Kinetics: The most significant proliferation enhancement is typically observed between 72-120 hours post-treatment, suggesting PA nanofibers influence cell cycle re-entry rather than providing immediate protection from thermal damage [12].
Bioactivity Specificity: The superior performance of RGDS-functionalized PAs compared to non-bioactive controls confirms that proliferation enhancement is specifically mediated through integrin-binding interactions rather than general scaffold effects [12] [3].
Troubleshooting and Technical Notes
Inconsistent Nanofiber Formation: If PA solutions fail to form nanofibers upon salt addition, verify PA purity (>95% recommended) and ensure proper storage conditions (lyophilized at -20°C). For problematic formulations, implement annealing protocols (heating to 80°C for 30 minutes followed by gradual cooling to room temperature) to promote thermodynamically favored nanofiber assembly [30].
Variable Thermal Damage: To ensure consistent thermal injury across experiments, calibrate heating apparatus regularly and maintain consistent cell confluence at time of injury. Include viability assessment 24 hours post-injury to confirm approximately 50% reduction compared to non-damaged controls [12].
High Background in MTT Assay: To minimize background signal, ensure complete removal of culture medium before MTT addition and use fresh DMSO for formazan solubilization. Include blank wells containing culture medium and MTT reagent without cells for background subtraction [12].
This application note provides comprehensive protocols for the in vitro validation of sprayable peptide amphiphile nanofibers designed to enhance proliferation of thermally damaged cells. The standardized methodologies enable robust quantification of PA bioactivity, with specific emphasis on RGDS-functionalized systems that demonstrate significant proliferation enhancement in both fibroblasts and endothelial cells—the key cellular players in wound healing. The integration of quantitative proliferation assays with appropriate control conditions ensures reliable assessment of PA formulations before advancing to complex in vivo models, ultimately accelerating the development of effective nanofiber therapies for burn wound treatment.
This document details the application and protocol for using sprayable peptide amphiphile (PA) nanofiber gels to accelerate burn wound healing in rat models. The data demonstrates that PA gels, particularly those functionalized with the bioactive arginine-glycine-aspartic acid-serine (RGDS) peptide sequence, create a supportive nanostructured environment that significantly enhances the rate of wound closure and re-epithelialization in deep partial-thickness burn wounds [12] [56].
The mechanism of action is twofold: the supramolecular nanofibers mimic the native extracellular matrix (ECM), providing a scaffold for cell migration and proliferation, while the displayed bioactive signals directly stimulate cellular processes critical for repair [3]. The following sections provide the quantitative evidence and detailed methodologies for reproducing these findings.
Key Quantitative Findings
Table 1: In-Vivo Efficacy Outcomes of RGDS-PA Gel in a Rat Burn Model
| Metric | Findings | Assessment Method |
|---|---|---|
| Re-epithelialization | Significantly enhanced between post-operative days 7 and 28 [12]. | Histologic evaluation [12]. |
| Wound Closure | Accelerated recovery of deep partial-thickness burn wounds [12] [56]. | Macroscopic observation and measurement [12] [56]. |
| Cellular Proliferation | Significant increase in proliferation of thermally damaged fibroblasts and HUVECs in vitro compared to controls [12]. | WST-1 cell proliferation assay [12] [56]. |
Table 2: In-Vitro Cell Proliferation on Various PA Gels
| PA Gel Type | Bioactive Signal | Cell Proliferation Outcome |
|---|---|---|
| RGDS-PA | RGDS (Fibronectin-derived) | Significantly higher than backbone-PA and collagen gels [12] [56]. |
| Backbone-PA | None (Non-bioactive) | Lower proliferation, serving as a control [12]. |
| Collagen Gel | N/A (Standard substrate) | Lower proliferation, serving as a standard control [12]. |
Experimental Protocols
Protocol 1: Synthesis and Characterization of Bioactive PA Nanofiber Gels
This protocol describes the creation and basic validation of the functional PA system.
- Principle: PA molecules are designed to self-assemble in physiological conditions into supramolecular nanofibers that display a high density of bioactive epitopes on their surface [3].
- Molecular Design: The PA is synthesized to include four key regions:
- A hydrophobic alkyl tail to drive self-assembly.
- A β-sheet forming peptide sequence (e.g., VVVAAA).
- Charged amino acids (e.g., glutamic acid) for water solubility and salt-responsive gelation.
- A terminal bioactive peptide signal (e.g., RGDS) [3].
- Preparation of PA Solution:
- Induction of Gelation:
- The self-assembly into a nanofiber gel is triggered upon exposure to physiological pH or electrolyte concentrations.
- For in-vivo application, the sterile PA solution is loaded into a spray syringe or applicator. Gelation occurs instantly upon contact with the tissue fluids at the wound site [3].
Diagram 1: PA molecule synthesis and self-assembly pathway.
Protocol 2: Establishing a Deep Partial-Thickness Burn Wound Model in Rats
This protocol outlines the creation of a standardized and reproducible burn wound for efficacy testing.
- Animal Model: Adult Sprague-Dawley or Wistar rats.
- Anesthesia: Anesthetize rats using an injectable cocktail of Ketamine (e.g., 75 mg/kg) and Xylazine (e.g., 10 mg/kg) [14].
- Pre-operative Preparation:
- Shave the dorsal area of the rat.
- Clean the shaved skin thoroughly with a disinfectant like 70% ethanol or betadine.
- Burn Infliction:
- Utilize a standardized brass metal rod heated in boiling water.
- Apply the pre-heated rod to the shaved skin for a defined duration (e.g., 10-15 seconds) without additional pressure to create a deep partial-thickness burn.
- Confirm burn depth by histology (H&E staining) post-infliction, showing coagulation necrosis of the epidermis and upper dermis with damaged hair follicles [12].
Protocol 3: In-Vivo Treatment and Efficacy Assessment
This protocol covers the treatment application and the multi-faceted analysis of wound healing.
- Experimental Groups:
- Group 1 (Test): Burn wound treated with RGDS-PA gel.
- Group 2 (Control): Burn wound treated with a non-bioactive backbone-PA gel.
- Group 3 (Control): Burn wound left untreated or treated with a standard dressing like saline gauze.
- Treatment Application:
- Wound Closure Monitoring:
- Photograph wounds regularly (e.g., every other day) until complete closure or study endpoint.
- Calculate wound area from photographs using image analysis software (e.g., ImageJ).
- Express wound closure as a percentage of the original wound area [12].
- Histological and Immunohistochemical Analysis:
- At predetermined time points (e.g., days 7, 14, 21, 28), euthanize animals and harvest wound tissue with a margin of surrounding healthy skin.
- Process samples for histology: fix in formalin, embed in paraffin, and section.
- Stain sections with Hematoxylin and Eosin (H&E) to assess general tissue architecture, granulation tissue formation, and re-epithelialization.
- Use Masson's Trichrome stain to evaluate collagen deposition and maturation.
- Perform immunohistochemistry for specific markers (e.g., Ki-67 for cell proliferation, CD31 for angiogenesis) to investigate the mechanism of healing [12].
Diagram 2: In-vivo treatment and analysis workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PA-Based Burn Wound Healing Research
| Item/Category | Function/Description | Examples & Notes |
|---|---|---|
| Peptide Amphiphile (PA) | Core self-assembling molecule forming the nanofibrous scaffold. | Custom synthesis with RGDS or other bioactive epitopes (e.g., IKVAV) [12] [3]. |
| Sprayable Applicator | For facile in-vivo delivery of liquid PA solution to the wound bed. | Sterile syringe or commercial spray device; gelation occurs upon contact with tissue [3]. |
| Cell Lines for In-Vitro Validation | Preliminary assessment of biocompatibility and bioactivity. | Thermally damaged fibroblasts, Human Umbilical Vein Endothelial Cells (HUVECs) [12]. |
| WST-1 Assay Kit | Colorimetric method to quantitatively measure cell proliferation in vitro [56]. | More modern alternative to MTT; measures metabolic activity [12] [56]. |
| Animal Burn Model System | Standardized creation of burn wounds for in-vivo testing. | Heated metal rod of defined diameter and material (e.g., brass) [12]. |
| Image Analysis Software | Quantification of wound closure from serial photographs. | ImageJ (Fiji) with appropriate plugins for area measurement [12] [14]. |
| Histology Stains | For microscopic evaluation of tissue repair quality. | H&E (general morphology), Masson's Trichrome (collagen) [12]. |
Comparative Analysis Against Traditional Dressings and Hydrogels
The management of wounds has evolved significantly from passive dry coverings to advanced interactive therapies. Traditional dressings, such as gauzes and bandages, often adhere to the wound bed, cause pain upon removal, and provide suboptimal conditions for healing by creating a dry environment [57]. In contrast, modern hydrogel dressings are three-dimensional, hydrophilic polymer networks that maintain a moist wound environment, facilitating autolytic debridement, promoting cell migration, and enhancing patient comfort [58] [52]. Within the realm of advanced hydrogels, sprayable peptide amphiphile (PA) nanofibers represent a cutting-edge therapeutic modality. These supramolecular systems are engineered to self-assemble under physiological conditions, creating a bioactive, biodegradable matrix that closely mimics the native extracellular matrix (ECM) [3] [38]. This application note provides a comparative analysis of these dressing types and details experimental protocols for evaluating sprayable PA hydrogels within a research setting.
Comparative Performance: Hydrogels vs. Traditional Dressings
Extensive clinical studies and meta-analyses have quantitatively demonstrated the superior efficacy of hydrogel dressings across multiple wound types and healing parameters compared to traditional non-hydrogel dressings [59]. The table below summarizes key performance metrics from a systematic review and meta-analysis of 43 clinical studies.
Table 1: Clinical Performance Metrics of Hydrogel vs. Non-Hydrogel Dressings [59]
| Wound Type | Healing Time | Cure Rate | Pain Relief | Notes |
|---|---|---|---|---|
| Degree II Burns | Significantly shortened | Not Specified | Significant relief | Includes both superficial and deep wounds. |
| Diabetic Foot Ulcers | Significantly shortened | Significantly increased | Not Specified | A key application for advanced hydrogels. |
| Traumatic Injuries | Significantly shortened | Not Specified | Significant relief | Includes laser treatment-induced wounds. |
| Surgical Wounds | No significant difference | Significantly increased | Not Specified | Improved cure rate despite similar healing time. |
| Pressure Ulcers (Inpatients) | Not Specified | No significant difference | Not Specified | Highlights need for targeted formulations. |
The fundamental advantage of hydrogels lies in their ability to create and maintain a moist wound environment. This moisture supports key healing processes, including the preservation of endogenous growth factors, facilitation of cell migration, and induction of collagen synthesis, which are often impeded by the dry conditions under traditional dressings [52]. Furthermore, the inherent flexibility of hydrogels allows for their functionalization with a wide range of bioactive agents, such as antimicrobial peptides (AMPs) and reactive oxygen species (ROS)-scavenging nanoparticles, to address specific pathological features of chronic wounds [22].
The Paradigm of Sprayable Peptide Amphiphile Nanofibers
Sprayable PA nanofibers constitute a significant advancement within the hydrogel domain, offering unique benefits for minimal-access application and dynamic wound management.
Molecular Design and Self-Assembly
PA molecules are synthetically tailored to comprise several key structural regions: a hydrophobic alkyl tail, a β-sheet forming peptide sequence, charged amino acids for solubility, and a bioactive peptide epitope (e.g., RGDS or IKVAV) at the C-terminus [3]. Upon dissolution in an aqueous solution and exposure to the physiological ionic strength of a wound bed (e.g., via spraying), these molecules undergo rapid self-assembly into supramolecular nanofibers. This process is driven by hydrophobic collapse of the alkyl tails and stabilization through hydrogen bonding within the β-sheet region, resulting in the formation of a three-dimensional nanofibrous hydrogel in situ [3] [38].
Functional Advantages for Wound Healing
The nanofibrous structure of PA hydrogels closely emulates the architecture of native ECM proteins like collagen and fibronectin, providing a biomimetic scaffold that supports cell adhesion, proliferation, and infiltration [3]. The sprayable delivery format offers unparalleled convenience, enabling high-throughput, non-invasive application over large and anatomically complex wound surfaces without causing shear-induced tissue damage [38]. A critical feature of these systems is their shear-thinning behavior; the hydrogel exhibits viscous flow under the shear stress of spraying but rapidly recovers its gel state upon deposition, ensuring stable coverage [38]. Bioadhesion can be further engineered into the system by incorporating specific peptide sequences, such as collagen-binding peptides (e.g., LRELHLNNN), which provide strong adhesion to wet tissue surfaces and prolong residence time at the wound site [38].
Experimental Protocols for Evaluating Sprayable PA Hydrogels
Protocol: Fabrication and Rheological Characterization of PA Hydrogel
Objective: To synthesize a bioactive PA and characterize its mechanical properties and gelation kinetics.
Materials:
- CBPA (Collagen-Binding Peptide Amphiphile) or similar PA molecule [38]
- Sterile, deionized water
- Phosphate-Buffered Saline (PBS), 10x concentration
- Rheometer with parallel plate geometry
Method:
- PA Solution Preparation: Dissolve the synthesized CBPA in sterile water to a final concentration of 1-4 mM. Ensure complete dissolution by gentle agitation or mild sonication.
- Gelation Induction: Mix the PA solution with 10x PBS in a 9:1 ratio (v/v) to achieve a final 1x PBS concentration. Gently pipette to mix and observe the rapid sol-gel transition.
- Rheological Analysis:
- Load the pre-gelled PA solution onto the rheometer plate.
- Initiate time-sweep measurements at a constant frequency (e.g., 1 Hz) and strain (e.g., 1%).
- At the 2-minute mark, carefully add a small, defined volume of 10x PBS to the edge of the plate without disrupting the measurement.
- Continue monitoring the storage modulus (G′) and loss modulus (G″) until they stabilize.
- Shear-Thinning Test: For sprayability assessment, subject the formed hydrogel to a high shear rate (e.g., 100 s⁻¹) for 1 minute, then immediately return to a low shear rate (e.g., 1 s⁻¹) to monitor the recovery of G′ and G″.
Expected Outcome: The crossover point where G′ surpasses G″ indicates gelation. A rapid recovery of G′ after high-shear exposure confirms the desired shear-thinning and self-healing properties essential for sprayable application [38].
Protocol: In Vitro Antibacterial and Biofilm Disruption Assay
Objective: To evaluate the efficacy of an AMP-loaded PA hydrogel against planktonic bacteria and established biofilms.
Materials:
- AMP (e.g., HHC-36 [22])
- PA hydrogel (e.g., GelMA-DOPA [22])
- Bacterial cultures (e.g., S. aureus, P. aeruginosa)
- Tryptic Soy Broth (TSB)
- 96-well microtiter plates
- Calcein-AM staining solution
Method:
- Hydrogel Preparation: Encapsulate the AMP within the PA hydrogel matrix during the polymer cross-linking process.
- Planktonic Bactericidal Assay:
- Incubate bacteria (~10⁶ CFU/mL) in TSB with the AMP-hydrogel or control dressings.
- After 4-6 hours, serially dilute the suspensions and plate on agar.
- Count colonies after 24 hours to determine the bactericidal rate.
- Biofilm Disruption Assay:
- Grow biofilms in 96-well plates for 48 hours.
- Apply the AMP-hydrogel directly to the pre-formed biofilms.
- After 24 hours of treatment, stain with Calcein-AM and quantify the viable biofilm biomass using a fluorescence plate reader.
Expected Outcome: A potent AMP-loaded hydrogel should achieve near 100% bactericidal capacity against common pathogens and significantly reduce the fluorescence signal from established biofilms, indicating effective penetration and disruption [22].
Protocol: In Vivo Evaluation in a Diabetic Wound Model
Objective: To assess the therapeutic effect of a sprayable PA hydrogel on wound closure and tissue regeneration.
Materials:
- Genetically diabetic (db/db) mice
- Sprayable CBPA or functionalized PA hydrogel [38]
- Control treatments (e.g., saline, traditional gauze)
- Digital camera and planimetry software
- Tissue processing supplies for histology
Method:
- Wound Creation: Anesthetize mice and create full-thickness excisional wounds on the dorsum.
- Treatment Protocol: Randomize animals into groups. Spray the PA hydrogel directly onto the wound bed to form a uniform layer. Re-apply every 3-4 days, or as needed based on degradation observations.
- Monitoring:
- Photograph wounds every other day.
- Use planimetry software to calculate wound area over time. Express data as percentage closure relative to original area.
- Endpoint Analysis: At day 10-14, euthanize animals and harvest wound tissue.
- Process for H&E staining to assess re-epithelialization and granulation tissue thickness.
- Perform Masson's Trichrome staining to evaluate collagen deposition and maturity.
Expected Outcome: Wounds treated with the bioactive sprayable PA hydrogel are expected to show significantly accelerated wound closure, more complete re-epithelialization, and better-organized collagen structure compared to control groups [22] [38].
Visualization of Key Concepts
Peptide Amphiphile Self-Assembly and Therapeutic Action
Diagram 1: PA self-assembly and therapeutic action pathway.
Experimental Workflow for Hydrogel Evaluation
Diagram 2: Experimental workflow for hydrogel evaluation.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Sprayable PA Hydrogel Research
| Reagent / Material | Function / Role | Research Context |
|---|---|---|
| Peptide Amphiphile (PA) | Core building block; self-assembles into nanofibers. | Synthesized with specific sequences (e.g., C12-LRELHLNNN for collagen binding) [38]. |
| Antimicrobial Peptides (AMPs) | Provides broad-spectrum, rapid bactericidal activity. | Encapsulated in hydrogel (e.g., HHC-36) to combat infection [22] [13]. |
| Cerium Oxide Nanoparticles (CeONs) | Scavenges reactive oxygen species (ROS). | Co-encapsulated with AMPs to modulate oxidative stress and reduce scarring [22]. |
| Gelatin Methacryloyl (GelMA) | Forms the backbone of photocrosslinkable hydrogels. | Functionalized with dopamine (GelMA-DOPA) for enhanced tissue adhesion [22]. |
| Photo-initiator (Irgacure 2959) | Initiates radical polymerization upon UV exposure. | Used for cross-linking and stabilizing spray-applied hydrogels [22]. |
| Collagen-Binding Peptide (LRELHLNNN) | Confers strong adhesion to wet tissue surfaces. | Incorporated into PA design to improve retention on wound beds [38]. |
Application Notes
Peptide amphiphile (PA) nanofibers represent a transformative platform in regenerative medicine, engineered to mimic the native extracellular matrix (ECM) and deliver multiple therapeutic signals in a spatiotemporally controlled manner [39] [28]. Their inherent biocompatibility, biodegradability, and capacity for molecular self-assembly make them ideal scaffolds for combination therapies targeting complex biological processes such as wound healing and bone regeneration [60] [5]. The synergistic potential of PAs is unlocked through the co-assembly of distinct PA monomers, each designed with a specific bioactive epitope—such as sequences promoting cell adhesion, vascularization, anti-inflammatory action, or antimicrobial activity [61] [39]. This modularity allows researchers to construct a multifaceted therapeutic environment from a single material system.
A key advancement is the development of sprayable PA formulations, which enable minimally invasive application conformally to irregular wound beds [41] [5]. These systems facilitate in-situ gelation, often through ionic crosslinking, creating a stable, bioactive scaffold directly at the site of injury [5]. Furthermore, the design of "smart" PA nanofibers that respond to pathological microenvironmental cues—such as elevated reactive oxygen species (ROS) or glutathione levels—enables precise, condition-dependent drug release, maximizing therapeutic efficacy while minimizing off-target effects [30]. This document details the quantitative evidence, standardized protocols, and essential reagents for implementing these advanced PA nanofiber platforms in a research setting.
Table 1: Quantitative Performance of PA Nanofiber Combination Therapies
| Therapeutic Application | PA Composition / Bioactive Signals | Key Quantitative Findings | Experimental Model |
|---|---|---|---|
| Bone Regeneration [39] | DGEA-PA (osteoinductive), EEE-PA (mineralization), DOPA-PA (adhesive), GL13K-PA (antimicrobial) | • >2x increase in early cell adhesion & proliferation• Marked upregulation of RUNX2, OPN, COL1A1• Significantly greater bone volume & trabecular maturation in vivo | In vitro: Human DPSCs; In vivo: Rabbit calvarial CSD |
| Infected Wound Healing [61] | MXene NIR-responsive nanofibers, DFOM (vascularization control), Acetylsalicylic Acid (anti-inflammatory) | • NIR photothermal effect for controlled DFOM release• Effective limitation of excessive angiogenesis• Regulated immune micro-environment at wound site | Not specified |
| Atherosclerosis Therapy [30] | ApoA1-PA (plaque targeting), LXR-PA (cholesterol efflux), E2-PA (diluent) | • ~40% LXR release in 24h with H~2~O~2~ (250 µM)• ~87-97% LXR release in 24h with TCEP (10 mM)• Activated ABCA1 expression with reduced liver toxicity | In vitro: Macrophages; In vivo: LDLR KO mouse model |
| Pro-Angiogenic Spray [5] | Pro-angiogenic PA, Ionic crosslinker (Ca^2+^) | • Confirmed self-assembly into nanofibers post-spray• Demonstrated favorable viscoelasticity after gelation• Supported cell viability, migration, and angiogenesis | In vitro: HEK cells; Endothelial cell tube formation assay |
Experimental Protocols
Protocol 1: Synthesis and Functionalization of Multifunctional PA Nanofibers
This protocol describes the solid-phase synthesis of a four-component PA system for enhanced bone regeneration, adapted from a study demonstrating significant in vitro and in vivo performance [39].
Materials:
- Resin: Rink Amide Resin (0.65 mmol/g loading)
- Reagents: Fmoc-protected amino acids, HBTU, HOBt, DIPEA, Lauric Acid, Trifluoroacetic Acid (TFA), Triisopropylsilane (TIS)
- Solvents: N,N-Dimethylformamide (DMF), Dichloromethane (DCM), Diethyl Ether
- Equipment: Automated peptide synthesizer, Preparative HPLC, ESI Mass Spectrometer
Procedure:
- Peptide Synthesis: Using Fmoc-chemistry on a rink amide resin, sequentially couple amino acids for each PA sequence via HBTU/HOBt activation.
- DGEA-PA: Lauryl–V–V–A–G–K–K–G–D–G–E–A–amide
- EEE-PA: Lauryl–V–V–A–G–K–K–G–E–E–E–A–amide
- DOPA-PA: Lauryl–V–V–A–G–K–K–G–DOPA–G–E–A–amide
- GL13K-PA: Lauryl–V–V–A–G–K–K–G–G–L–K–K–amide
- Lipidation: Conjugate lauric acid to the N-terminus of each peptide chain to confer amphiphilic properties.
- Cleavage and Deprotection: Cleave peptides from the resin and remove side-chain protecting groups using a cocktail of TFA:TIS:water (95:2.5:2.5, v/v) for 2 hours at room temperature.
- Precipitation and Lyophilization: Precipitate crude PA products in cold diethyl ether, collect via centrifugation, and lyophilize.
- Purification and Characterization: Purify PAs via reverse-phase HPLC. Confirm molecular identity and purity (>95%) using ESI-MS.
- Co-assembly: Combine the four PAs in a specific molar ratio in deionized water (e.g., 1 wt% total concentration). Sonicate and incubate for 24 hours in phosphate buffer (10 mM, pH 7.4, 150 mM NaCl) to promote nanofiber self-assembly.
- Graft Functionalization: Immerse the graft material (e.g., xenograft, allograft, or synthetic hydroxyapatite particles) in the co-assembled PA solution. Incubate to allow the adhesive DOPA-PA to facilitate stable coating.
Protocol 2: In Vitro Evaluation of Osteogenic Differentiation on PA-Coated Grafts
This protocol assesses the bioactivity of PA-coated grafts using human dental pulp stem cells (DPSCs) [39].
Materials:
- Cells: Human Dental Pulp Stem Cells (DPSCs)
- Culture Reagents: DMEM (high glucose), Fetal Bovine Serum (FBS), Penicillin-Streptomycin, Osteogenic induction supplements
- Assay Kits: MTT, Alkaline Phosphatase (ALP) activity (pNPP), Alizarin Red S, TRIzol, cDNA Synthesis Kit, SYBR Green qPCR reagents
Procedure:
- Cell Seeding: Seed DPSCs onto PA-coated and uncoated (control) grafts at a standardized density.
- Cell Viability (MTT Assay): At designated time points (e.g., 1, 3, 7 days), incubate cells with MTT reagent for 4 hours. Solubilize the formed formazan crystals and measure absorbance at 570 nm.
- Osteogenic Gene Expression (qRT-PCR): After 7-14 days of osteogenic induction, extract total RNA using TRIzol. Synthesize cDNA and perform qPCR to quantify expression of osteogenic markers (e.g., RUNX2, OPN, COL1A1). Normalize data to a housekeeping gene like GAPDH.
- ALP Activity Assay: Lyse cells at an early osteogenic time point (e.g., 7-10 days). Incubate lysates with pNPP substrate and measure the conversion to p-nitrophenol by reading absorbance at 405 nm. Normalize to total protein content.
- Mineralization (Alizarin Red S Staining): After 21-28 days, fix cells and stain with 2% Alizarin Red S (pH 4.2) to detect calcium deposits. Quantify by eluting the stain with cetylpyridinium chloride and measuring absorbance at 562 nm.
Visualization of Signaling Pathways and Workflows
Diagram 1: PA Nanofiber Self-Assembly and Therapeutic Action Workflow
Diagram 2: Key Signaling Pathways in PA-Mediated Wound Healing and Bone Regeneration
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for PA Nanofiber Research
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Fmoc-Protected Amino Acids [39] | Building blocks for solid-phase peptide synthesis of PA monomers. | Include standard and modified residues (e.g., DOPA for adhesion [39]). |
| Rink Amide MBHA Resin [39] | Solid support for SPPS, yielding C-terminal amide peptides. | Loading capacity of 0.65 mmol/g is commonly used [39]. |
| Coupling Reagents (HBTU/HOBt) [39] | Activate amino acids for efficient amide bond formation during SPPS. | Used with base DIPEA in DMF solvent [39]. |
| Lipid Tail (e.g., Lauric Acid) [39] | Conjugated to peptide N-terminus to create the amphiphile structure. | The hydrophobic driver for self-assembly into nanofibers [39]. |
| Cleavage Cocktail (TFA/TIS/Water) [39] | Cleaves peptide from resin and removes acid-labile side-chain protecting groups. | Typical ratio: 95:2.5:2.5 (v/v) [39]. |
| Ionic Crosslinker (CaCl₂) [5] | Induces rapid gelation of anionic PA solutions for sprayable formulations. | Enables in-situ formation of a stable scaffold [5]. |
| Human Dental Pulp Stem Cells (DPSCs) [39] | A relevant mesenchymal stem cell model for in vitro osteogenesis assays. | Used to test bone regeneration therapies [39]. |
| qRT-PCR Reagents [39] | Quantify mRNA expression levels of osteogenic genes (RUNX2, OPN, COL1A1). | SYBR Green is a common choice [39]. |
Assessing Angiogenesis, Collagen Deposition, and Scar Formation
The development of advanced wound healing therapies requires precise assessment of key regenerative processes: angiogenesis, collagen deposition, and scar formation. Sprayable peptide amphiphile (PA) nanofibers represent an innovative platform for wound management, offering minimally invasive application and structural mimicry of the native extracellular matrix (ECM) [3] [10]. This document provides detailed application notes and standardized protocols for evaluating these critical healing parameters within the context of PA nanofiber research, enabling robust quantification and comparison across experimental conditions.
Research Reagent Solutions
The table below catalogues essential materials and reagents for conducting the assessments described in this protocol.
Table 1: Key Research Reagent Solutions for Wound Healing Assessment
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Peptide Amphiphiles (PAs) | Self-assembling nanofiber scaffold backbone [1] [3]. | C16-V3A3K3G-NH2 [62]; Collagen-Binding PA (CBPA) [38]. Customize bioactive epitopes (e.g., IKVAV, RGDS). |
| Soluplus & Soy Protein Isolate (SPI) | Polymer & natural protein component for electrospun nanofiber dressings; enhances drug loading and cell compatibility [14]. | Used to fabricate composite nanofibers loaded with antibiotics (e.g., Mupirocin) or other active compounds [14]. |
| Antimicrobial Peptides (AMPs) | Provide broad-spectrum antimicrobial activity and immunomodulatory functions [13]. | LL-37, defensins, or custom-designed AMPs. Can be co-assembled with or loaded into PA nanofibers. |
| Silk Nanofiber Hydrogels | Biomaterial for hydrophobic drug delivery (e.g., Asiaticoside) to regulate inflammation and angiogenesis [63]. | Beta-sheet rich silk hydrogels prepared via concentration-dilution-thermal incubation [63]. |
| Mupirocin | Antibiotic agent for evaluating antibacterial efficacy of nanofiber dressings against Gram-positive and Gram-negative bacteria [14]. | Example loading: 2% w/w in Soluplus/SPI nanofibers [14]. |
| Asiaticoside (AC) | Hydrophobic drug with anti-inflammatory, antioxidant, and pro-angiogenic properties; used to functionalize hydrogels [63]. | Loaded into silk nanofiber hydrogels to achieve scarless wound repair in vivo [63]. |
Experimental Workflow for Comprehensive Assessment
The overall process for developing and evaluating sprayable PA nanofiber systems for wound healing involves sequential stages from material preparation to final histological analysis.
Quantitative Assessment Metrics and Standards
Establishing standardized quantitative metrics is essential for objective evaluation of wound healing progression. The following table summarizes key parameters and their measurement methods.
Table 2: Key Quantitative Metrics for Wound Healing Assessment
| Process | Key Metric | Measurement Method | Exemplary Data from Literature |
|---|---|---|---|
| Angiogenesis | - Number of new blood vessels- Vessel density & maturity- Hemoglobin content | - Immunohistochemistry (CD31)- Tube formation assay- Hemoglobin assay | - Asiaticoside-laden silk hydrogels showed regulated vascularization, leading to scarless repair [63].- HUVEC tube formation confirmed bioactivity of released compounds [63]. |
| Collagen Deposition & Maturation | - Collagen fiber density- Collagen I/III ratio- Fiber organization | - Masson's Trichrome- Picrosirius Red- Second Harmonic Generation (SHG) imaging | - Electrospun Sol/SPI/Mp nanofibers accelerated re-epithelialization and wound healing in a rat model [14].- AM-FM nanomechanical mapping can determine Young's moduli of β-sheet nanofibers [64]. |
| Scar Formation & Tissue Remodeling | - Epidermal thickness- Scar elevation index- Tensile strength of healed tissue | - H&E staining- Histomorphometry- Tensiometry | - AC-laden hydrogels achieved scarless wound repair with regeneration similar to normal skin [63].- PA:PSSNa co-assemblies could sustain water pressure up to 3 bars, indicating mechanical stability [62]. |
| Anti-Biofilm & Antimicrobial Activity | - Bacterial reduction percentage- Biofilm biomass reduction | - Colony Forming Unit (CFU) counts- Crystal Violet assay | - Sol/SPI/Mp nanofibers killed 93.06% of S. aureus and 90.40% of E. coli [14].- AMPs exhibit broad-spectrum activity and diverse mechanisms of action [13]. |
Detailed Experimental Protocols
Protocol: In Vitro Tube Formation Assay for Angiogenesis
Principle: This assay evaluates the pro-angiogenic potential of PA nanofiber leachates or conditioned media by quantifying the ability of human umbilical vein endothelial cells (HUVECs) to form capillary-like tube structures on a basement membrane matrix (Matrigel) [63].
Materials:
- HUVECs (Human Umbilical Vein Endothelial Cells)
- Growth factor-reduced Matrigel
- 24-well tissue culture plate
- Conditioned media from PA nanofiber cultures
- Inverted microscope with camera
Procedure:
- Matrigel Coating: Thaw Matrigel on ice overnight. Pipette 200 µL of Matrigel into each well of a pre-chilled 24-well plate. Incubate the plate at 37°C for 30 minutes to allow polymerization.
- Cell Preparation: Trypsinize, count, and resuspend HUVECs in the test conditioned media or standard media containing the desired concentration of PA nanofiber leachates. Centrifuge examples include media containing Asiaticoside-laden silk nanofiber hydrogels (SNF-AC) [63].
- Seeding: Seed 8.0 × 10^4 cells per well in 500 µL of the respective media onto the polymerized Matrigel. Perform triplicate wells for each condition.
- Incubation: Incubate the plate at 37°C in a 5% CO2 atmosphere for 6-12 hours.
- Imaging & Quantification: After incubation, capture multiple non-overlapping images per well using an inverted microscope (e.g., 4x or 10x objective). Analyze images with software such as ImageJ Angiogenesis Analyzer to quantify:
- Total tube length per field of view
- Number of branching points
- Number of complete meshes
Notes: Include appropriate controls (e.g., positive control with VEGF, negative control with basal media). Ensure Matrigel is handled on ice to prevent premature gelling.
Protocol: Analysis of Collagen Deposition and Maturation via Picrosirius Red Staining
Principle: Picrosirius Red stain, when combined with polarized light microscopy, selectively highlights collagen fibers and differentiates thin, immature (green/yellow) collagen III from thick, mature (orange/red) collagen I based on birefringence [14].
Materials:
- Deparaffinized tissue sections (5-7 µm thickness)
- Picrosirius Red Stain Kit (or separate Sirius Red and Picric Acid solutions)
- Xylene, Ethanol series
- Mounting medium
- Light microscope with polarized light filters
Procedure:
- Deparaffinization and Hydration: Process formalin-fixed, paraffin-embedded (FFPE) wound tissue sections following standard protocol: xylene (2 x 5 min) -> 100% ethanol (2 x 3 min) -> 95% ethanol (2 min) -> 70% ethanol (2 min) -> rinse in distilled water.
- Staining: Immerse the slides in Picrosirius Red solution for 60 minutes at room temperature with gentle agitation.
- Washing: Rinse the slides briefly in two changes of acidified water (0.5% acetic acid in water) to remove non-specific stain.
- Dehydration: Rapidly dehydrate the sections through graded ethanols: 70% ethanol (quick dip) -> 95% ethanol (2 min) -> 100% ethanol (2 x 2 min).
- Clearing and Mounting: Clear in xylene (2 x 3 min) and mount with a resinous mounting medium.
- Imaging and Analysis:
- Brightfield Imaging: View under standard light to assess total collagen area (appears red).
- Polarized Light Imaging: Capture images under polarized light. Mature collagen I fibers will appear bright orange or red, while immature collagen III fibers will appear green.
- Use image analysis software (e.g., ImageJ) with color thresholding to calculate:
- Percentage of collagen area per total tissue area.
- Collagen I/III ratio based on the area of red vs. green birefringence.
Protocol: In Vivo Scar Formation Assessment via Histomorphometry
Principle: This protocol quantifies scar tissue formation in an in vivo wound model by measuring the Scar Elevation Index (SEI) from standard Hematoxylin and Eosin (H&E) stained sections, providing a metric for hypertrophic scarring.
Materials:
- H&E-stained full-wound cross-sections
- Light microscope with digital camera
- Image analysis software (e.g., ImageJ)
Procedure:
- Sectioning: Ensure tissue is sectioned perpendicular to the wound surface and the skin's longitudinal axis to obtain a true full-thickness cross-section of the wound.
- Identification of Regions: On the H&E-stained image, identify the following zones for a wound healed primarily by re-epithelialization:
- Epidermal Region: The newly formed epithelium above the granulation tissue.
- Dermal Region: The area between the mature underlying dermis and the new epidermis.
- Unwounded Dermis: The adjacent, normal dermal tissue on either side of the wound.
- Measurement:
- Measure the total wound area (T), defined as the area of the new dermal tissue plus the area of the new epidermal tissue.
- Measure the area of unwounded dermis (D) that would have occupied the same span if the wound had not occurred. This is done by projecting lines from the edges of the unwounded dermis across the wound bed.
- Calculation:
- Scar Elevation Index (SEI) = T / D.
- An SEI > 1 indicates the presence of elevated hypertrophic scar tissue. A value closer to 1 indicates a more normal, flat repair.
- Additional Metric - Epidermal Thickness: Measure the thickness of the neo-epidermis at the wound center and compare it to the thickness of the normal epidermis adjacent to the wound. Increased thickness indicates abnormal differentiation.
Molecular Design and Functional Pathways of Peptide Amphiphiles
The bioactivity of sprayable PA nanofibers is intrinsically linked to their molecular structure. A rational design incorporates specific domains that direct self-assembly and interact with biological systems.
Molecular Design Logic: The canonical PA structure is modular [1] [3]. The hydrophobic tail (Region 1, e.g., palmitic acid) drives self-assembly in aqueous environments via hydrophobic collapse. The adjacent β-sheet forming sequence (Region 2, e.g., V(3)A(3)) stabilizes the nanofiber core through extensive hydrogen bonding, dictating the cylindrical geometry. Charged residues (Region 3, e.g., K(_3) for positive charge) provide water solubility and enable triggered gelation upon exposure to physiological salt concentrations, which is crucial for sprayable formulations [62] [38]. The bioactive epitope (Region 4, e.g., IKVAV for neurite outgrowth, RGDS for cell adhesion, or a collagen-binding sequence) is displayed on the nanofiber surface at high density, directly influencing cellular responses such as endothelial cell migration for angiogenesis or fibroblast activity for collagen production [3] [38].
The integrated application notes and protocols provided herein establish a standardized framework for evaluating the efficacy of sprayable peptide amphiphile nanofibers in promoting wound healing. By employing these quantitative assessments for angiogenesis, collagen deposition, and scar formation, researchers can robustly validate the functional benefits of their material designs, thereby accelerating the development of advanced, regenerative wound therapies.
Conclusion
Sprayable peptide amphiphile nanofibers represent a paradigm shift in wound care, successfully merging supramolecular chemistry with regenerative medicine. The foundational research establishes their unique ability to create biomimetic microenvironments that actively promote healing. Methodological advances have enabled their practical delivery as sprayable systems, while ongoing optimization addresses key translational challenges of stability and bioavailability. Crucially, robust preclinical validation demonstrates superior efficacy in accelerating wound closure, enhancing re-epithelialization, and improving overall healing quality compared to standard care. Future directions must focus on advancing human clinical trials, developing targeted PA designs for specific wound etiologies like diabetic ulcers, and exploring combination therapies with antimicrobials and biologics. The continued refinement of this platform holds immense promise for delivering next-generation, precision wound therapies that significantly improve patient outcomes.
References
- 1. Self-Assembly of Peptide Amphiphiles - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2921868/]
- 2. Peptide amphiphile [https://en.wikipedia.org/wiki/Peptide_amphiphile]
- 3. Supramolecular Nanofibers of Peptide Amphiphiles for Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3922220/]
- 4. Self-Assembled Nanomaterials for Chronic Skin Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8024239/]
- 5. Development and Characterization of a Pro-Angiogenic Peptide Amphiphile for Deep Dermal Burn Healing via Spray Delivery [https://aquila.usm.edu/honors_theses/1018/]
- 6. Lego-like Visible Assembly of Responsive Components via ... [https://www.sciencedirect.com/science/article/pii/S266724052500008X]
- 7. Bioactive peptide amphiphile nanofiber gels enhance burn ... [https://www.sciencedirect.com/science/article/pii/S030541791830514X]
- 8. New updates on peptides and peptide-based biopolymeric ... [https://www.sciencedirect.com/science/article/abs/pii/S0167732225013546]
- 9. Mimicking the extracellular world: from natural to fully synthetic ... [https://pubs.rsc.org/en/content/articlehtml/2024/nr/d4nr02088j]
- 10. Innovative hydrogels in cutaneous wound healing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1454903/full]
- 11. Polysaccharide Electrospun Nanofibers for Wound Healing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9464040/]
- 12. Bioactive peptide amphiphile nanofiber gels enhance burn ... [https://pubmed.ncbi.nlm.nih.gov/31043333/]
- 13. Application of Antimicrobial Peptides in Wound Dressings [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457083/]
- 14. Antibacterial and wound healing stimulant nanofibrous ... [https://www.nature.com/articles/s41598-024-78161-4]
- 15. Design and applications of self-assembled polypeptide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375629/]
- 16. Laminin-derived peptide, IKVAV, modulates macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10884775/]
- 17. The emerging role of human transmembrane RGD-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492590/]
- 18. The RGD Peptide, origins and applications [https://www.cellgs.com/blog/the-rgd-peptide-origins-and-applications.html]
- 19. RGD-decorated nanoparticles: Therapeutic potential ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224724005938]
- 20. Newly Designed PCL-Wrapped Cryogel-Based Conduit ... [https://www.mdpi.com/1999-4923/16/12/1569]
- 21. Advantages of RGD peptides for directing cell association with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3091033/]
- 22. Sprayable hydrogel dressing accelerates wound healing ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706121000878]
- 23. Designed peptide amphiphiles as scaffolds for tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S0001868623000337]
- 24. Advanced Peptide Nanofibers in Delivery of Therapeutic ... [https://www.mdpi.com/2079-6439/13/10/130]
- 25. Self-assembling short peptide as versatile delivery... amphiphiles [https://pubs.rsc.org/en/content/articlehtml/2024/cc/d4cc01762e]
- 26. of a new Synthesis and evaluation of its cytotoxicity and... peptide [https://jabonline.in/abstract.php?article_id=1302&sts=2]
- 27. Sulfated GAG mimetic peptide enhance chondrogenic... nanofibers [https://pmc.ncbi.nlm.nih.gov/articles/PMC9847523/]
- 28. Peptide Nanofibers and Skin Regeneration [https://pubmed.ncbi.nlm.nih.gov/39841381/]
- 29. Peptide-driven approaches in advanced wound healing ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625001539]
- 30. Self-Assembled Peptide Amphiphile Nanofibers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8680456/]
- 31. A review on fabrication methods of nanofibers and ... [https://www.sciencedirect.com/science/article/pii/S2666893922000779]
- 32. Electrospun nanofibers synthesized from polymers ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02491-8]
- 33. Electrospun Nanofibers in Wound Healing: Real-World ... [https://www.mdpi.com/2306-5354/12/5/500]
- 34. Electrospinning in promoting chronic wound healing [https://pubmed.ncbi.nlm.nih.gov/40114848/]
- 35. Review: functionalization of biopolymer-based electrospun ... [https://link.springer.com/article/10.1007/s10853-025-10931-5]
- 36. Sprayable hydrogel sponge for neurovascular ... [https://www.sciencedirect.com/science/article/pii/S2452199X25003615]
- 37. Development of a Sprayable Hydrogel-Based Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10970460/]
- 38. Collagen-Binding Peptide-Enabled Supramolecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9844543/]
- 39. Multifunctional peptide nanofiber coatings enhance bone ... [https://www.nature.com/articles/s41598-025-15743-w]
- 40. Biomimetic Hydrogels to Promote Wound Healing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.718377/full]
- 41. Innovative nanofibre spraying for bioactive delivery [https://www.sciencedirect.com/science/article/pii/S2468519425003283]
- 42. Development of a Sprayable Hydrogel-Based Wound ... [https://www.mdpi.com/2310-2861/10/3/176]
- 43. Bioactive peptide amphiphile nanofiber gels enhance burn ... [https://www.bohrium.com/paper-details/bioactive-peptide-amphiphile-nanofiber-gels-enhance-burn-wound-healing/812777800170733568-9755]
- 44. Current Insight of Peptide-Based Hydrogels for Chronic ... [https://pubmed.ncbi.nlm.nih.gov/39861121/]
- 45. Nanostructure-templated control of drug release from peptide ... [https://pubmed.ncbi.nlm.nih.gov/23130084/]
- 46. Synergistic assembly of peptide amphiphiles with varying ... [https://www.sciencedirect.com/science/article/abs/pii/S2589152919303126]
- 47. Strategies for Improving Peptide Stability and Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9610364/]
- 48. Peptide-Mediated Nanocarriers for Targeted Drug Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC10893007/]
- 49. Current progress and remaining challenges of peptide–drug ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03277-2]
- 50. Recent Advances in Supramolecular Systems for Precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473587/]
- 51. A supramolecular bactericidal material for preventing and ... [https://www.nature.com/articles/s41467-025-57839-x]
- 52. A review of the current state of natural biomaterials in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1309541/full]
- 53. Research Progress on the Application of Novel Wound ... [https://www.mdpi.com/1999-4923/17/8/976]
- 54. Biomaterials-mediated sequential drug delivery: emerging ... [https://www.sciencedirect.com/science/article/pii/S1818087625000728]
- 55. Electrospinning in promoting chronic wound healing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1550553/full]
- 56. Bioactive Peptide Amphiphilic Gels Enhance Burn Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5147223/]
- 57. Modern Wound Dressings: Hydrogel Dressings - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8472341/]
- 58. Advancements in hydrogels: A comprehensive review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025078274]
- 59. A Systematic Review and Meta-Analysis of Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6881259/]
- 60. Nanofiber Scaffolds as Drug Delivery Systems Promoting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10384736/]
- 61. Nanofibers and hydrogel hybrid system with synergistic ... [https://www.sciencedirect.com/science/article/pii/S2590049822000200]
- 62. Nano-Fibrous Networks from Co-Assembly of Amphiphilic ... [https://www.mdpi.com/2073-4360/13/22/3983]
- 63. Asiaticoside-laden Silk Nanofiber Hydrogels to Regulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8319114/]
- 64. Quantitative nanomechanical properties evaluation of a ... [https://www.sciencedirect.com/science/article/pii/S1751616121004197]