Preventing Endosomal Damage from Lipid Nanoparticles: Strategies for Safer RNA Therapeutics
Lipid nanoparticles (LNPs) are the leading platform for RNA therapeutic delivery, but their hallmark feature—endosomal escape—is a double-edged sword that can trigger inflammatory responses by causing endosomal membrane damage.
Preventing Endosomal Damage from Lipid Nanoparticles: Strategies for Safer RNA Therapeutics
Abstract
Lipid nanoparticles (LNPs) are the leading platform for RNA therapeutic delivery, but their hallmark feature—endosomal escape—is a double-edged sword that can trigger inflammatory responses by causing endosomal membrane damage. This article provides a comprehensive analysis for researchers and drug development professionals, exploring the fundamental mechanisms of LNP-induced endosomal damage, the cellular sensors that detect this damage, and the resulting inflammatory pathways. It details cutting-edge methodological advances in LNP design, including novel ionizable lipids that minimize membrane disruption and strategies to engage cellular repair machinery. The content further covers troubleshooting and optimization techniques to balance efficient cargo delivery with minimal cellular perturbation, and concludes with validation approaches comparing the efficacy and safety profiles of next-generation LNPs. The synthesis of these perspectives aims to guide the development of safer, non-inflammatory LNP formulations for a broader range of therapeutic applications, including treatment of inflammatory diseases.
The Double-Edged Sword: How LNP Endosomal Escape Triggers Inflammation
The Essential yet Damaging Process of Endosomal Escape
Frequently Asked Questions (FAQs)
1. Why does endosomal escape, a desired process, cause damage and inflammation? Endosomal escape is necessary for functional RNA delivery because it allows the genetic cargo to reach the cytosol where it can be translated by ribosomes. However, the mechanism by which LNPs facilitate this escape often involves physically disrupting the endosomal membrane [1] [2]. This disruption is sensed by the cell as damage. Specifically, large, irreparable holes in the endosomal membrane expose glycans to the cytosol, which are detected by proteins called galectins [2]. This galectin binding initiates potent inflammatory signaling pathways, leading to the release of cytokines like IL-6 and TNF-α [2].
2. What is the difference between "productive" and "non-productive" endosomal damage? Recent research distinguishes between two types of LNP-induced endosomal damage:
- Productive Damage (Galectin-positive): Membrane damage marked by the recruitment of galectins (particularly galectin-9) is statistically correlated with successful cytosolic release of RNA cargo [1]. This damage is conducive to escape.
- Non-productive Damage (ESCRT-recruited): Membrane perturbations that recruit the Endosomal Sorting Complexes Required for Transport (ESCRT) machinery are typically repaired by the cell and do not permit significant endosomal escape [1]. LNPs that create smaller, reparable holes may thus cause damage without enabling efficient functional delivery [2].
3. What fraction of internalized LNPs successfully triggers RNA release? The process is highly inefficient. Live-cell microscopy studies reveal that only a fraction of internalized LNPs trigger galectin-9 recruitment, which is associated with payload release [1]. Furthermore, even within a damaged endosome, only a small fraction of the total RNA cargo is released into the cytosol [1]. Surprisingly, many endosomes showing galectin-9 recruitment contain no detectable RNA payload at all, a phenomenon more pronounced for mRNA-LNPs than for siRNA-LNPs [1].
4. How can LNP design reduce immunogenicity without compromising delivery efficiency? Strategies focus on engineering the lipids to create a less disruptive escape mechanism:
- ESCRT-Recruiting Ionizable Lipids: A novel class of ionizable lipids can create intermediate-sized holes in the endosome that are recognized and repaired by the ESCRT machinery. This design can produce high expression from mRNA cargo while minimizing galectin-triggered inflammation [2].
- PEG Replacement: Replacing conventional PEG-lipids with alternatives like poly(carboxybetaine) (PCB) lipids can reduce immunogenicity and the "Accelerated Blood Clearance" phenomenon, while also enhancing endosomal escape through better membrane interaction [3].
Troubleshooting Guides
Problem: High Cytotoxicity and Inflammation from LNPs
Potential Causes and Solutions:
| Cause | Supporting Evidence | Proposed Solution |
|---|---|---|
| Overly disruptive ionizable lipids | Ionizable lipid chemistry and the rate/magnitude of endosomal disruption directly correlate with cytotoxicity [4] [2]. | Screen or design ionizable lipids that recruit the ESCRT repair machinery to create smaller, reparable membrane holes [2]. |
| Formulation-induced excessive galectin signaling | Cytosolic galectin sensors (e.g., galectin-9) detect endosomal damage and drive inflammation; inhibition of galectins abrogates LNP-associated inflammation [2]. | Implement galectin-9 recruitment assays early in screening to identify inflammatory formulations [1] [4]. |
| High anti-PEG antibody response | Anti-PEG antibodies can cause accelerated blood clearance, reduce efficacy, and pose safety risks, especially upon repeated dosing [3]. | Replace linear PEG-lipids with low-immunogenicity alternatives like hydroxyl-PEG (HO-PEG), branched PEGs, or non-PEG alternatives like PCB lipids [3]. |
Experimental Protocol: Quantifying Endosomal Damage with a Galectin-9 Reporter
- Objective: To visualize and quantify LNP-induced endosomal membrane damage in live cells.
- Materials:
- Method:
- Cell Preparation: Seed cells in a glass-bottom imaging dish and transfert with a plasmid expressing a fluorescent galectin-9 protein (e.g., GFP-Gal9).
- LNP Exposure: After 24-48 hours, treat cells with a therapeutically relevant dose of LNPs (e.g., 400 ng/mL for RAW cells [2]).
- Live-Cell Imaging: Use fast live-cell microscopy (e.g., confocal or TIRF) to image cells immediately after LNP addition. Capture images every 5-10 seconds for 1-2 hours [1].
- Data Analysis:
- Quantify the number of galectin-9-positive foci per cell over time.
- Track individual endosomes to identify de novo recruitment events [1].
- Correlate the timing and intensity of galectin-9 recruitment with the presence of fluorescently labeled LNP cargo.
Problem: Low Functional Delivery Efficiency Despite High Cellular Uptake
Potential Causes and Solutions:
| Cause | Supporting Evidence | Proposed Solution |
|---|---|---|
| Inefficient endosomal escape | Only a small fraction of RNA is released from galectin-marked endosomes; many damaged endosomes contain no detectable RNA [1]. | Optimize the pKa of the ionizable lipid (typically ~6.4-6.5) to improve endosomal membrane disruption and payload release [1]. |
| Payload/lipid segregation | During endosomal sorting, the ionizable lipid and RNA payload can segregate within and across endosomal compartments, preventing coordinated escape [1]. | Develop co-localization assays (using dual-fluorescent LNPs with labeled lipid and RNA) to monitor payload retention during trafficking [1]. |
| Dense PEG coating | The PEG "stealth" layer can act as a physical barrier, reducing LNP-membrane interactions needed for endosomal escape (the "PEG dilemma") [3]. | Use cleavable PEG-lipids (acid- or enzyme-responsive) that shed the PEG layer in the endosome, or replace PEG with PCB lipids that enhance membrane interaction [3]. |
Experimental Protocol: Evaluating Payload and Lipid Co-localization
- Objective: To determine if the RNA payload dissociates from the LNP core during intracellular trafficking.
- Materials:
- Dual-labeled LNPs: LNPs formulated with a fluorescently labeled ionizable lipid (e.g., BODIPY-MC3, green) and fluorescently labeled RNA (e.g., Cy5 or AlexaFluor 647, red) [1].
- Cells: Relevant cell line for your application.
- Method:
- Treatment and Uptake: Incubate cells with dual-labeled LNPs for a set time (e.g., 1-4 hours).
- Fixation and Imaging: Fix cells and image using super-resolution microscopy (e.g., STORM or STED) to achieve high spatial resolution [1].
- Image Analysis:
- Identify individual endosomes and quantify the fluorescence intensity of both the lipid (green) and RNA (red) channels.
- Calculate a correlation coefficient (e.g., Pearson's) for the two signals within single endosomes.
- Identify and count endosomes that are positive for the ionizable lipid but negative for the RNA payload, and vice-versa.
Table 1: Efficiency of Cytosolic RNA Delivery from Galectin-9-Positive Endosomes
This table summarizes key quantitative findings from live-cell imaging studies, highlighting the inefficiencies in the endosomal escape process [1].
| Parameter | siRNA-LNPs | mRNA-LNPs | Experimental Context |
|---|---|---|---|
| Fraction of damaged endosomes with detectable RNA ("Hit Rate") | 67% - 74% | ~20% | Live-cell imaging in cultured cells |
| Dose for saturated galectin-9 response | 50 nM (0.72 µg/mL) | 0.75 µg/mL | Dose-response in cultured cells |
| Relative fluorescence intensity per intact LNP | ~2x higher than mRNA-LNP | Baseline | In vitro measurement of fluorescently labeled LNPs |
| Signal increase upon LNP disintegration | ~2.6-fold increase | <20% increase | Treatment with Triton X-100 detergent |
Table 2: Inflammatory Profile Induced by LNP Treatment In Vivo
This table quantifies the pro-inflammatory effects observed in mice after administration of mRNA-LNPs, demonstrating the systemic nature of the response [2].
| Inflammatory Marker | Change after Intratracheal LNP (7.5 µg mRNA) | Change after Intravenous LNP (7.5 µg mRNA) | Cell Culture Model (RAW 264.7 macrophages) |
|---|---|---|---|
| IL-6 | Significant Increase | Significant Increase | Upregulated by mRNA, empty, and PSS LNPs |
| TNF-α | Significant Increase | Significant Increase | Upregulated by mRNA, empty, and PSS LNPs |
| IFN-β | Significant Increase | Significant Increase | Upregulated by mRNA, empty, and PSS LNPs |
| MCP-1 | Significant Increase | Significant Increase | Upregulated by mRNA, empty, and PSS LNPs |
| BAL Protein | Large, dose-dependent increase (2.5-10 µg dose) | Not Reported | Not Applicable |
| BAL Leukocytes | Large, dose-dependent increase (2.5-10 µg dose) | Not Reported | Not Applicable |
Signaling Pathways and Experimental Workflows
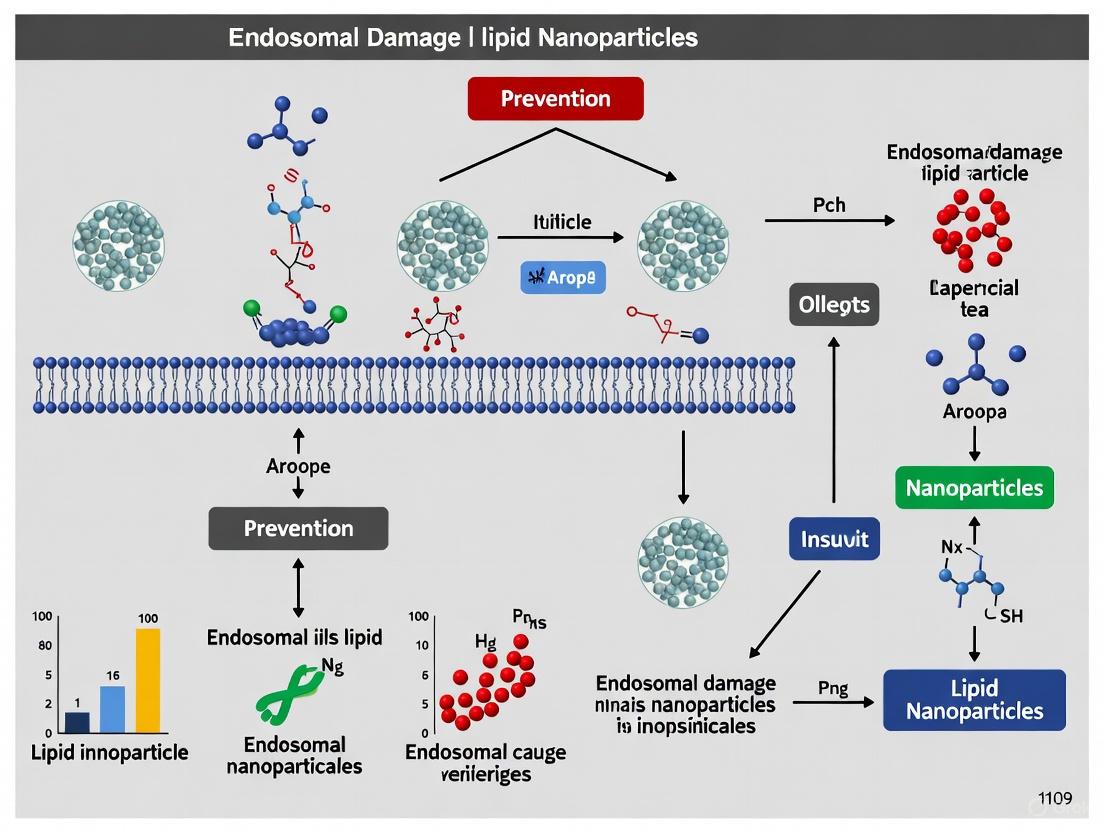
Diagram 1: LNP-induced endosomal damage pathways. This flowchart illustrates the critical juncture after lipid nanoparticle (LNP)-induced endosomal membrane damage. The size of the membrane hole determines the cellular response: large holes trigger galectin-mediated inflammation, while smaller holes are repaired by the ESCRT machinery, minimizing immune activation. RNA release is an inefficient process that can occur from damaged endosomes [1] [2].
Diagram 2: Galectin-9 recruitment assay workflow. This protocol provides a step-by-step guide for using a galectin-9 fluorescent reporter to visualize and quantify LNP-induced endosomal membrane damage in live cells [1] [4] [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying and Improving Endosomal Escape
| Reagent / Tool | Function / Application | Key Feature / Rationale |
|---|---|---|
| GFP-Galectin-9 Reporter | A fluorescent biosensor to detect endosomal membrane damage in live cells [1] [4] [2]. | Galectin-9 is a highly sensitive sensor for LNP-induced damage; allows real-time kinetic studies [1]. |
| ESCRT Pathway Inhibitors | Chemical or genetic tools to inhibit the ESCRT machinery (e.g., VPS4 inhibitors) to study its role in mitigating LNP toxicity [2]. | Validates whether a novel LNP formulation creates small, ESCRT-repairable holes versus large, inflammatory ones [2]. |
| Ionizable Lipids (ESCRT-recruiting) | Next-generation lipids designed to create intermediate-sized endosomal holes [2]. | Aims to balance high RNA delivery efficiency with minimal induction of inflammation [2]. |
| PEG Alternatives (e.g., PCB Lipids) | Zwitterionic polymers that replace PEG-lipids in LNP formulations [3]. | Reduce anti-PEG immunogenicity and enhance endosomal escape via membrane interaction, enabling repeated dosing [3]. |
| Dual-Labeled LNPs | LNPs with separately fluorescently tagged ionizable lipids and RNA payload [1]. | Enables study of payload/lipid segregation during endosomal trafficking, a key inefficiency barrier [1]. |
| Branched / Cleavable PEG Lipids | Engineered PEG-lipids designed to reduce immunogenicity [3]. | Branched or Y-shaped PEGs reduce anti-PEG antibody production; cleavable PEGs shed in the endosome to improve membrane contact [3]. |
Core Concept FAQs
What are galectins and what is their primary function in the context of endosomal damage? Galectins are a class of β-galactoside-binding proteins characterized by a conserved carbohydrate recognition domain (CRD). They are among the most widely expressed lectins and function as key sensors of endosomal membrane damage. When lipid nanoparticles (LNPs) create holes in the endosomal membrane during escape, intracellular glycans become exposed to the cytosol. Cytosolic galectins recognize and bind to these exposed glycans, triggering downstream inflammatory signaling pathways [5] [2] [6].
Why is LNP-induced endosomal damage a significant concern for therapeutic development? While endosomal escape is necessary for RNA delivery, the accompanying membrane damage activates inflammation through galectin sensing. This inflammation can be severe and massively aggravate pre-existing inflammatory conditions—by more than 10-fold in some models. This presents a major roadblock for using LNPs in patients with inflammatory diseases (including most elderly and hospitalized patients) and prevents their safe use for treating common inflammatory conditions like heart attack and stroke [5] [2].
What is the difference between galectin-recruited and ESCRT-recruited endosomal damage? The cellular response to LNP-induced endosomal damage depends on the size of the membrane holes:
- Large, irreparable holes are recognized by galectins, which detect exposed glycans and activate inflammatory pathways [5] [2].
- Smaller, reparable holes recruit the Endosomal Sorting Complex Required for Transport (ESCRT) machinery, which promotes membrane repair without triggering significant inflammation [5] [2].
The key distinction is that galectin recruitment leads to inflammation, while ESCRT recruitment generally allows for endosomal repair and avoids inflammatory responses.
Troubleshooting Guides
Problem: High Inflammation with Efficient RNA Delivery
Observation: Your LNPs provide excellent RNA expression but trigger severe inflammatory responses in vitro and in vivo.
Potential Causes and Solutions:
- Cause: The ionizable lipid creates large, irreparable endosomal holes that trigger galectin-dependent inflammation.
- Solution 1: Reformulate with rapidly biodegradable ionizable lipids. These create smaller, ESCRT-repairable holes that minimize galectin recruitment while maintaining delivery efficiency [5].
- Solution 2: Implement galectin inhibition strategies in your therapeutic approach. Research shows galectin inhibition abrogates LNP-associated inflammation both in vitro and in vivo [5] [2].
- Validation: Monitor galectin-9 recruitment as a marker for inflammatory endosomal damage using live-cell imaging [1].
Problem: Inconsistent Endosomal Escape Efficiency
Observation: Variable transfection efficiency between cell types or experiments, with poor correlation between LNP uptake and functional delivery.
Investigation and Resolution:
- Quantify Actual Escape: Use galectin recruitment as a direct marker for endosomal damage conducive to escape. Only a small fraction of RNA is released from galectin-marked endosomes, and many damaged endosomes contain no detectable RNA cargo due to payload-lipid segregation during endosomal sorting [1].
- Optimize Ionizable Lipid pKa: Ensure ionizable lipids have optimal pKa (typically 6-7) for endosomal membrane interaction. The chemical structure of the ionizable lipid, particularly alkyl chain saturation and branching, critically influences phase transition behavior and escape efficiency [7].
- Balance PEG Content: Address the "PEG dilemma" by optimizing PEGylated lipid percentage. While PEG provides stability and stealth properties, excessive PEG reduces cellular uptake and endosomal escape. Consider biodegradable PEG alternatives [7].
Table 1: Efficiency Metrics of LNP-Mediated RNA Delivery and Associated Damage
| Parameter | siRNA-LNPs | mRNA-LNPs | Measurement Technique |
|---|---|---|---|
| Endosomal Escape Efficiency | 1-2% of endosomal cargo [7] | Not quantified, but lower than siRNA [1] | Functional cytosolic delivery assessment |
| Galectin-9+ Vesicles with RNA Cargo ("Hit Rate") | 67-74% [1] | ~20% [1] | Live-cell microscopy with fluorescent RNA |
| Dose for Galectin Response Saturation | 50 nM (0.72 µg/mL) [1] | 0.75 µg/mL [1] | Galectin-9 foci quantification |
| Inflammation Exacerbation | >10-fold increase in pre-existing inflammation markers [2] | Similar profile to siRNA-LNPs [2] | Cytokine analysis in disease models |
Table 2: Strategies for Controlling LNP-Induced Inflammation
| Strategy | Mechanism of Action | Effect on Expression | Effect on Inflammation |
|---|---|---|---|
| Galectin Inhibition | Blocks detection of large endosomal ruptures | Maintains high expression [5] [2] | Abrogated in vitro and in vivo [5] [2] |
| ESCRT-Recruiting Lipids | Creates smaller, reparable membrane holes | Maintains high expression [5] [2] | Minimal inflammation [5] [2] |
| Standard Inflammatory LNPs | Creates large, irreparable holes triggering galectins | High expression [5] | Severe exacerbation of inflammation [5] |
Detailed Experimental Protocols
Protocol 1: Assessing Galectin Recruitment via Live-Cell Imaging
Purpose: To visualize and quantify LNP-induced endosomal damage in real-time.
Materials:
- Galectin-9 fluorescent protein construct (e.g., Galectin-9-GFP)
- Confocal or super-resolution live-cell microscopy system
- Cells stably expressing galectin-9-GFP (e.g., RAW 264.7 macrophage cell line)
- Fluorescently labeled LNPs (e.g., with Cy5 or AlexaFluor dyes on RNA)
Procedure:
- Plate galectin-9-GFP expressing cells in glass-bottom imaging dishes 24 hours before experiment.
- Replace medium with imaging-appropriate buffer immediately before assay.
- Add fluorescent LNPs at working concentration (e.g., 0.75 µg/mL for mRNA-LNPs).
- Begin immediate time-lapse imaging using temperature and CO₂ control.
- Acquire images every 30-60 seconds for 1-3 hours to capture damage events.
- Analyze data by tracking de novo recruitment of galectin-9 to vesicular structures containing LNPs.
Key Observations:
- Galectin recruitment typically occurs within 1 hour of LNP addition [1].
- Look for transient or sustained galectin-9 foci that co-localize with LNP signals.
- Note that only a fraction of internalized LNPs trigger galectin recruitment [1].
Protocol 2: Evaluating Inflammatory Response to LNPs
Purpose: To quantify cytokine release and immune activation following LNP administration.
In Vivo Model (Mouse):
- Administer LNPs intratracheally at therapeutically relevant doses (2.5-10 μg mRNA per mouse) [2].
- Euthanize animals 24 hours post-instillation.
- Collect bronchoalveolar lavage (BAL) fluid and plasma.
- Analyze BAL for protein content (capillary leak marker) and leukocyte count (infiltration marker).
- Measure pro-inflammatory cytokines (IL-6, TNF-α, IL-1α, IFN-β) and chemokines (MCP-1) in BAL and plasma using ELISA.
In Vitro Model (Macrophage):
- Expose RAW 264.7 macrophages to LNPs at dose of 400 ng/mL for 6 hours [2].
- Include controls: empty LNPs (no cargo) and LNPs with non-RNA cargo (e.g., PSS).
- Collect supernatant and measure same cytokine panel as in vivo.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Ionizable Lipids (e.g., cKK-E12, MC3) | Enables RNA encapsulation and endosomal escape | pKa (~6-7) and biodegradability critical for inflammation profile [5] [2] |
| Galectin-9 Fluorescent Constructs | Visualizing endosomal membrane damage | Most sensitive sensor for LNP-induced damage [1] |
| ESCRT Pathway Reporters | Detecting repair-competent membrane damage | Distinguishes inflammatory vs. non-inflammatory escape [5] |
| Cytokine ELISA Kits (IL-6, TNF-α) | Quantifying inflammatory response | Essential for safety profiling of new LNP formulations [2] |
| Biodegradable Ionizable Lipids | Creating ESCRT-recruitable small holes | Key to non-inflammatory, high-expression LNPs [5] |
Mechanism and Workflow Diagrams
LNP Endosomal Escape Pathways
Troubleshooting Experimental Workflow
From Membrane Holes to Inflammatory Signaling Cascades
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our therapeutic mRNA LNPs show good protein expression but also induce high levels of IL-6 in animal models. What is the likely mechanism and how can we mitigate this?
A: The inflammation is likely triggered by endosomal membrane damage during escape. When LNPs create large, irreparable holes in the endosomal membrane, cytosolic galectin proteins recognize exposed glycans and initiate inflammatory signaling cascades, leading to cytokine production including IL-6 [2]. To mitigate this, consider reformulating with ionizable lipids that create smaller, reparable membrane holes. These intermediate-sized holes recruit the ESCRT machinery for repair instead of triggering galectin-mediated inflammation, potentially reducing IL-6 secretion while maintaining expression [2].
Q2: Why do we observe strong inflammatory responses even when using "empty" LNPs with no RNA cargo?
A: Empty LNPs still induce inflammation because the lipid components themselves, particularly through endosomal membrane damage, are sufficient to trigger immune recognition. Studies show that empty LNPs, LNPs loaded with non-RNA cargo, and mRNA-LNPs all upregulate similar pro-inflammatory cytokines (IL-1α, IL-6, TNF-α, IFN-β, MCP-1), with empty LNPs sometimes producing the highest cytokine concentrations [2]. This confirms the lipid component and its disruptive interaction with endosomal membranes is a primary driver of inflammation, independent of RNA-mediated immune activation.
Q3: When imaging galectin-positive endosomal damage, we find many damaged endosomes contain no detectable RNA cargo. Does this indicate a problem with our LNP formulation?
A: Not necessarily. Recent research using high-resolution microscopy reveals that RNA payload and ionizable lipid can segregate during endosomal sorting, resulting in galectin-9-positive damaged endosomes that lack detectable RNA [1]. This segregation between the damaging component (ionizable lipid) and cargo (RNA) is a naturally occurring inefficiency in LNP delivery. Focus instead on quantifying the correlation between functional delivery and damage, and consider that hit rates (damaged vesicles with cargo) differ between siRNA (~70%) and mRNA (~20%) LNPs [1].
Q4: What are the key signaling pathways activated by nanoparticle-induced endosomal damage?
A: The primary sensors are galectins that detect membrane damage, but downstream signaling involves multiple pathways. Beyond galectin recognition, LNP-induced membrane damage can activate MAP kinase cascades (ERK, p38, JNK) and redox-sensitive transcription factors like NF-κB and Nrf-2 [8]. Additionally, oxidative stress from nanoparticle interactions can trigger NLRP3 inflammasome activation, leading to caspase-1 activation and inflammation [9]. For metallic nanoparticles, Toll-like Receptor (TLR) signaling is also a significant pathway for pro-inflammatory cytokine production [9].
Troubleshooting Guide: Managing LNP-Induced Inflammation
| Problem | Potential Cause | Solution |
|---|---|---|
| High cytokine secretion | Large, irreparable endosomal holes triggering galectin-mediated inflammation [2] | Reformulate with ESCRT-recruiting ionizable lipids; Consider galectin inhibition strategies |
| Poor expression with low inflammation | Insufficient endosomal escape; Over-optimized for safety [2] | Screen ionizable lipids with pKa ~6.0-6.5; Balance escape efficiency with damage control |
| Variable responses across cell types | Differences in ESCRT machinery or galectin expression [2] | Characterize repair capacity of target cells; Consider cell-specific formulation optimization |
| Cargo-independent inflammation | Lipid composition directly activating immune receptors [10] | Modify ionizable lipid structure; Consider alternative phospholipid components |
| Rapid clearance in vivo | PEG immunogenicity; ABC phenomenon [10] | Optimize PEG lipid anchor and percentage; Consider alternative stealth lipids |
Quantitative Data on LNP-Induced Inflammation
Inflammatory Marker Elevation Following LNP Administration
Table 1: Markers of LNP-induced inflammation in mouse models following intratracheal instillation of cKK-E12 mRNA-LNPs (7.5 μg dose) [2]
| Inflammatory Marker | Fold Increase vs Control | Biological Significance |
|---|---|---|
| BAL Protein Content | Large, dose-dependent increase [2] | Capillary leak, lung barrier dysfunction |
| BAL Leukocyte Count | Large, dose-dependent increase [2] | Immune cell infiltration to alveoli |
| IL-6 | Significantly increased [2] | Pro-inflammatory cytokine, acute phase response |
| TNF-α | Significantly increased [2] | Pro-inflammatory cytokine, systemic inflammation |
| IFN-β | Significantly increased [2] | Type I interferon, antiviral state induction |
| MCP-1 | Significantly increased [2] | Chemokine, monocyte recruitment |
Table 2: Comparison of inflammatory responses across administration routes for cKK-E12 mRNA-LNPs [2]
| Administration Route | Tissue Cytokine Profile | Systemic Effects |
|---|---|---|
| Intratracheal | Upregulation of IL-1α, IL-6, TNF-α, IFN-β, MCP-1 in BAL fluid [2] | Local lung inflammation, hepatization |
| Intravenous | Upregulation of same cytokines in plasma [2] | Leukocytosis, lymphopenia, neutrophilia, liver/spleen inflammation |
| Intradermal | Significant cytokine upregulation in skin tissues [2] | Local skin inflammation |
LNP Formulation Comparison Data
Table 3: Cationic lipid comparison for reactogenicity and immunogenicity in mouse study (5 μg unmodified spike mRNA, intramuscular) [11]
| Lipid Type | Lipid Name | Particle Size (nm) | Zeta Potential (mV) | Encapsulation Efficiency | Post-Prime Weight Loss |
|---|---|---|---|---|---|
| Permanent Cationic | DOTMA | 63-149 [11] | +20.7 [11] | >88% [11] | 3-6% (transient) [11] |
| Ionizable | ALC0315 | 63-149 [11] | Not specified | >88% [11] | 3-6% (transient) [11] |
| Various Ionizable | 4 other structures | 63-149 [11] | Not specified | >88% [11] | 3-6% (transient) [11] |
Experimental Protocols
Protocol 1: Assessing Endosomal Damage via Galectin Recruitment
Purpose: To visualize and quantify LNP-induced endosomal membrane damage using galectin markers [2] [1].
Materials:
- Galectin-9 translocation reporter (e.g., GFP-galectin-9)
- Appropriate cell line (e.g., RAW 264.7 macrophages, primary target cells)
- LNP formulations to test
- Live-cell imaging setup with environmental control
- Fixatives if performing endpoint assays
Procedure:
- Cell Preparation: Plate cells in appropriate imaging chambers 24 hours prior to experiment to achieve 60-70% confluence.
- Transfection: Transfert cells with GFP-galectin-9 construct using standard methods and allow 24-48 hours for expression.
- LNP Exposure: Add LNPs at working concentration (e.g., 50 nM for siRNA-LNPs, 0.75 μg/mL for mRNA-LNPs) directly to imaging medium [1].
- Image Acquisition:
- Begin time-lapse imaging immediately after LNP addition
- Capture images every 2-5 minutes for 1-4 hours
- Maintain temperature at 37°C with 5% CO₂
- Quantification:
- Count galectin-9 positive foci per cell over time
- Calculate percentage of LNP-containing endosomes that recruit galectin-9
- Note intensity and duration of galectin recruitment
Troubleshooting Tips:
- If background galectin signal is high, serum-starve cells for 1-2 hours before imaging
- Optimize LNP dose in pilot experiments to avoid saturation of damage response
- For co-localization studies, use fluorescently labeled LNPs with distinct emission spectrum from GFP
Protocol 2: Evaluating ESCRT Recruitment to Damaged Endosomes
Purpose: To determine if LNP formulations create reparable membrane holes that recruit ESCRT machinery instead of triggering inflammation [2].
Materials:
- ESCRT component reporters (e.g., CHMP4B-GFP, VPS4-mCherry)
- Standard cell culture reagents and equipment
- Confocal or super-resolution microscope
- LNP formulations with varying ionizable lipids
Procedure:
- Cell Preparation: Seed cells expressing ESCRT component fluorescent reporters.
- LNP Exposure: Treat cells with test LNPs at therapeutically relevant concentrations.
- Fixation and Staining: At predetermined timepoints (30-120 minutes post-treatment), fix cells and immunostain for endosomal markers (e.g., Rab5, Rab7, LAMP1).
- Image Analysis:
- Quantify co-localization between ESCRT components and endosomal markers
- Compare ESCRT recruitment between LNP formulations
- Correlate with galectin recruitment in parallel experiments
- Functional Assessment:
- Measure cytokine production (IL-6, TNF-α) from same treatments
- Assess mRNA expression efficiency
Interpretation: Formulations that recruit ESCRT machinery without significant galectin recruitment typically show reduced inflammation while maintaining therapeutic efficacy [2].
Protocol 3: In Vivo Assessment of LNP-Induced Inflammation
Purpose: To evaluate the inflammatory potential of LNP formulations in animal models [2].
Materials:
- Appropriate animal model (e.g., C57BL/6 mice)
- Test LNP formulations
- Control LNPs (empty, known inflammatory, known non-inflammatory)
- Equipment for desired administration route (intravenous, intratracheal, intramuscular)
- BAL collection supplies or blood collection tubes
- Cytokine ELISA kits (IL-6, TNF-α, IFN-β, MCP-1)
Procedure:
- Dosing: Administer LNPs at therapeutically relevant doses to experimental animals.
- Sample Collection:
- For intratracheal administration: Collect bronchoalveolar lavage (BAL) fluid at designated timepoints (e.g., 2, 6, 24 hours)
- For systemic administration: Collect plasma/serum at similar timepoints
- Inflammatory Marker Analysis:
- Quantify total protein in BAL fluid (capillary leak marker)
- Count leukocytes in BAL fluid (immune cell infiltration)
- Measure cytokine levels via ELISA
- Histopathology:
- Harvest relevant tissues (lung, liver, spleen)
- Process for H&E staining
- Score for inflammatory changes
Data Interpretation: Compare inflammatory markers between test formulations and controls. Effective non-inflammatory LNPs should show significantly reduced inflammatory parameters while maintaining target engagement.
Signaling Pathway Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Essential Reagents for Studying LNP-Induced Endosomal Damage
Table 4: Key research reagents for investigating LNP-endosomal interactions and inflammation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Membrane Damage Reporters | GFP-galectin-3, GFP-galectin-9, RFP-galectin-4 [2] [1] | Live-cell imaging of endosomal rupture | Galectin-9 is most sensitive for LNP damage; optimize expression levels |
| ESCRT Machinery Reporters | CHMP4B-GFP, VPS4-mCherry, TSG101 antibodies [2] | Detect reparable vs. irreparable membrane damage | Co-stain with late endosome markers for localization |
| Ionizable Lipids | cKK-E12 (inflammatory reference), ESCRT-recruiting lipids [2] | Structure-function studies of escape vs. inflammation | Screen pKa values ~6.0-6.5 for optimal endosomal activity |
| Cytokine Detection | IL-6, TNF-α, IFN-β, MCP-1 ELISAs [2] | Quantify inflammatory responses | Measure multiple timepoints (2-24h) for complete profile |
| Endosomal Markers | Rab5-GFP (early), Rab7-RFP (late), LAMP1 antibodies [1] | Track LNP trafficking through endocytic pathway | Use super-resolution for precise localization |
| Fluorescent LNP Components | BODIPY-MC3 (lipid), Cy5-mRNA, AF647-siRNA [1] | Visualize cargo/lipid segregation and fate | Account for fluorescence quenching in intact LNPs |
Experimental Workflow Visualization
Frequently Asked Questions
Q1: What are the primary cellular sensors used to detect and quantify LNP-induced endosomal damage? The primary sensors for LNP-induced endosomal damage are cytosolic galectin proteins, particularly galectin-9 and galectin-8. These proteins contain carbohydrate recognition domains that bind to β-galactoside sugars. When endosomal membranes are damaged, these normally hidden glycans on the inner leaflet are exposed to the cytosol. Galectins rapidly recruit to these sites, forming fluorescent puncta that can be imaged and quantified. Galectin-9 is noted as the most sensitive sensor for damages induced by LNPs and small molecule drugs [1] [12].
Q2: Why is the functional delivery of RNA cargo so inefficient despite observed endosomal damage? Research reveals multiple layers of inefficiency. Even when LNPs trigger galectin-9-positive endosomal damage, functional RNA release is not guaranteed. Key factors include:
- Cargo-Payload Segregation: The ionizable lipid and RNA cargo can segregate during endosomal sorting, meaning a damaged endosome may not contain the therapeutic payload [1].
- Low Release Fraction: Only a small fraction of the RNA cargo present in a damaged endosome is actually released into the cytosol [1].
- Variable Damage Response: The cell can activate the ESCRT (Endosomal Sorting Complexes Required for Transport) machinery to repair smaller membrane holes, preventing escape. Only larger, irreparable holes lead to significant galectin recruitment and potential release [2].
Q3: How can I experimentally distinguish between productive and non-productive endosomal damage? Simultaneous live-cell imaging of multiple markers is required. You should track:
- Damage: Using a fluorescent reporter like mCherry-Galectin9.
- Cargo: Using fluorescently labeled RNA (e.g., Cy5-mRNA).
- Repair Machinery: Using fluorescently tagged ESCRT components (e.g., CHMP4b). Productive escape events are typically characterized by strong, sustained galectin-9 recruitment co-localized with the RNA cargo, and an absence of ESCRT machinery. In contrast, ESCRT recruitment indicates repair and likely non-productive damage [2] [1].
Troubleshooting Guides
Problem: Low or Inconsistent Endosomal Escape Efficiency
Potential Causes and Solutions:
Cause 1: Suboptimal Ionizable Lipid Properties The pKa and chemical structure of the ionizable lipid are critical. The lipid should have a pKa between 6.0-6.5 to protonate efficiently in the early endosome. A cone-like structure (with unsaturated or branched tails) promotes the transition to an inverted hexagonal phase in the endosomal membrane, facilitating escape [7].
Cause 2: The "PEG Dilemma" PEGylated lipids are essential for LNP stability and reducing opsonization, but they can also create a steric barrier that inhibits cellular uptake and fusion with the endosomal membrane, thereby reducing escape [7].
- Solution: Optimize the molar percentage of PEG-lipid in your formulation. Consider using exchangeable PEG-lipids that dissociate over time or exploring biodegradable PEG alternatives like polyoxazolines [7].
Cause 3: Inadequate Quantification Method Standard confocal microscopy and flow cytometry lack the resolution to accurately quantify individual endosomal escape events, which are rare, fast, and occur at the nanoscale [13].
- Solution: Implement advanced nanoscopy techniques. Super-resolution microscopy (e.g., STED, SMLM) or electron microscopy (EM) provide the necessary resolution to visualize and quantify endosomal damage and cargo release at the single-vesicle level [13].
Problem: High Cytotoxicity and Inflammation from LNPs
Potential Causes and Solutions:
- Cause: Excessive Endosomal Damage Triggering Potent Immune Responses
Large, irreparable endosomal holes trigger robust galectin recruitment, which initiates inflammatory signaling pathways, leading to the release of cytokines like IL-6 and TNF-α [2].
- Solution 1: Develop "stealth" LNPs that create smaller, reparable holes. Certain ionizable lipid classes generate intermediate-sized membrane perturbations that recruit the ESCRT repair machinery instead of galectins. This allows for sufficient RNA expression while minimizing inflammatory activation [2].
- Solution 2: In experimental models, genetic or pharmacological inhibition of galectins has been shown to abrogate LNP-associated inflammation without completely blocking RNA expression [2].
Quantitative Data on Endosomal Escape Efficiency
The following tables summarize key quantitative findings from recent research, highlighting the profound inefficiencies in the LNP delivery process.
Table 1: Quantifying the Intracellular Barriers to LNP Delivery
| Inefficiency Barrier | Quantitative Measure | Experimental Method | Source |
|---|---|---|---|
| Overall siRNA Release per Endosome | Only 1% - 2% of encapsulated siRNA is released into the cytosol. | Super-resolution microscopy, functional assays | [7] |
| Endosomal Damage without Cargo | For mRNA-LNPs, ~80% of galectin-9 positive damaged endosomes contained no detectable mRNA. | Live-cell microscopy, vesicle tracking | [1] |
| Endosomal Damage with Cargo | For siRNA-LNPs, ~70% of galectin-9 positive damaged endosomes contained siRNA. | Live-cell microscopy, vesicle tracking | [1] |
| LNP Uptake vs. Damage | Only a fraction of internalized LNPs trigger galectin-9 recruitment. | Correlative live-cell imaging | [1] |
Table 2: Comparison of Microscopy Techniques for Quantifying Endosomal Escape
| Technique | Resolution (XY) | Suitable for Live-Cell Imaging? | Quantification Capability | Key Advantage |
|---|---|---|---|---|
| Confocal Microscopy | ~200 nm | Yes | Worst (Low resolution, cannot resolve single NPs) | Simple, accessible, multi-color [13] |
| Electron Microscopy (EM) | ~1 nm | No | Good (Direct visualization and counting) | Highest resolution, definitive localization [13] |
| SMLM (e.g., PALM/STORM) | ~20 nm | No (in most cases) | Good (Single-molecule counting) | Molecular-scale resolution, single-molecule counting [13] |
| STED | ~50 nm | Yes | Good | Super-resolution in live cells [13] |
| CLEM (Correlative Light-EM) | ~1 nm (EM) | No | Best (Combines dynamics with ultrastructure) | Correlates functional data with high-resolution structure [13] |
Experimental Protocols
Protocol 1: High-Throughput Galectin-9 Imaging Assay for Endosomal Damage
This protocol uses a stable cell line expressing a fluorescent galectin-9 reporter to quantify LNP-induced endosomal damage [12].
Workflow:
Detailed Methodology:
- Reporter Cell Generation: Generate stable cell lines (e.g., Huh7, HepG2) expressing mCherry-tagged galectin-9 using a knock-in strategy (e.g., AAVS1 ZFN-targeting) [12].
- Cell Seeding: Plate reporter cells in a 96-well or 384-well optical-bottom imaging plate and culture until ~80% confluent.
- LNP Treatment: Add LNPs containing fluorescently labeled RNA (e.g., Cy5-mRNA) to the cells. Include a positive control (e.g., 10 µM UNC2383 small molecule) and a negative control (vehicle). Add a nuclear stain (e.g., Hoechst) to assess cytotoxicity via nuclear morphology [12].
- Image Acquisition: Use a high-throughput automated microscope for live-cell, time-lapse imaging. Capture images every 30-60 minutes for 6-24 hours using channels for mCherry (damage), Cy5 (cargo), and Hoechst (nuclei) [12].
- Image Analysis: Use image analysis software (e.g., ImageJ, CellProfiler) to:
- Count the number of mCherry-Gal9 puncta per cell over time.
- Measure the co-localization between mCherry-Gal9 puncta and Cy5-RNA signal.
- Analyze nuclear size and intensity in the Hoechst channel to infer compound toxicity [12].
Protocol 2: Correlative Microscopy to Analyze LNP and Cargo Segregation
This protocol combines live-cell dynamics with high-resolution electron microscopy to visualize the disintegration of LNPs and segregation of components inside endosomes [1].
Detailed Methodology:
- Prepare Dual-Labeled LNPs: Formulate LNPs where both the ionizable lipid (e.g., conjugated to BODIPY) and the RNA cargo (e.g., labeled with Cy5) are fluorescently tagged [1].
- Live-Cell Imaging: Treat cells with dual-labeled LNPs and perform live-cell imaging to track the co-localization of the lipid and RNA signals over time in endosomes, particularly those recruiting galectin-9.
- Chemical Fixation: At a time point of interest (e.g., when galectin recruitment is observed), rapidly fix the cells with a suitable fixative (e.g., glutaraldehyde) for EM processing.
- Sample Processing for EM: Process the fixed cells for EM analysis, which includes dehydration, resin embedding, and ultramicrotomy to produce thin sections.
- Correlative Light and Electron Microscopy (CLEM):
- Use the fluorescent signals from the live-cell imaging to map the regions of interest.
- Image the same regions in the EM sections to achieve high-resolution visualization of the endosomal ultrastructure, LNP morphology, and the spatial relationship between LNPs and the endosomal membrane [1].
- Analysis: Quantify the ratio of endosomes where lipid and RNA signals have segregated. Look for visual evidence of LNP disintegration and ionizable lipid enrichment in the endosomal membrane [1].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Endosomal Damage and Escape
| Reagent / Tool | Function / Target | Key Application in Research |
|---|---|---|
| mCherry-Galectin9 Reporter Cell Line | Live-cell sensor for endosomal membrane damage. | High-throughput screening of LNP formulations; quantifying damage kinetics [12]. |
| Fluorescently Labeled RNA (Cy5-mRNA/siRNA) | Visualizing the location and trafficking of LNP cargo. | Determining cargo co-localization with damage markers; quantifying release efficiency [1] [12]. |
| Antibodies to Endosomal Markers (Rab5, Rab7, LAMP1) | Marking different stages of the endolysosomal pathway. | Identifying the subcellular location of LNP accumulation and damage via immunofluorescence [14] [15]. |
| ESCRT Machinery Reporters (e.g., CHMP4b-GFP) | Sensor for endosomal membrane repair pathways. | Distinguishing between reparable (non-leaky) and irreparable (leaky) membrane damage [2]. |
| Ionizable Lipids (e.g., DLin-MC3-DMA, SM-102) | Core functional component of LNPs for endosomal escape. | Formulating LNPs; studying structure-function relationships for efficient, low-inflammatory delivery [2] [7]. |
Visualizing the Endosomal Damage and Escape Pathway
The following diagram illustrates the key cellular decision point that determines whether endosomal damage leads to productive RNA escape or non-productive inflammation/repair.
Troubleshooting Guide: FAQs on Endosomal Damage and Cytotoxicity
FAQ: Why do my Lipid Nanoparticles (LNPs) cause high cytotoxicity in cell cultures, even with modified, non-immunogenic mRNA?
The cytotoxicity is likely driven by the LNP components themselves, not the mRNA cargo. Research shows that changing or even removing the mRNA cargo does not significantly affect cytotoxicity, indicating that the cell response is primarily driven by the lipid components [4] [16]. The key mechanism is endosomal disruption; the rate and magnitude of this disruption directly correlate with observed cell toxicity [4] [2].
FAQ: My LNP formulations show good cellular uptake but poor functional protein expression. What is the bottleneck?
This is a common issue where endosomal escape has failed. While uptake may be efficient, the majority of internalized LNPs are degraded in the lysosome or have their payloads recycled outside the cell [17]. Only a very small fraction of RNA payload is successfully released into the cytosol [1]. The endosomal escape step is a major bottleneck for functional delivery.
FAQ: I observe strong inflammatory responses in my in vivo models after LNP administration. Is this caused by the RNA or the delivery system?
Both can contribute, but the LNP itself is a potent inflammatory trigger. Even empty LNPs (with no RNA cargo) can induce comparable pro-inflammatory cytokine secretion (e.g., IL-6, TNF-α) and act as a strong adjuvant [2]. This inflammation is mechanistically linked to endosomal damage. When the endosomal membrane is disrupted, it is sensed by cytosolic galectin proteins, which subsequently trigger inflammatory pathways [2].
FAQ: How can I design safer LNPs that minimize endosomal trauma but maintain high delivery efficiency?
Focus on the chemical design of the ionizable lipid. Recent studies show that a unique class of ionizable lipids can create smaller, repairable holes in the endosome [2]. These smaller holes are recognized and repaired by the ESCRT (Endosomal Sorting Complex Required for Transport) machinery, allowing for cargo release while minimizing the activation of inflammatory galectin sensors [2]. Furthermore, biodegradable lipids (e.g., those with ester bonds in the acyl tails) are designed to reduce cellular accumulation and can improve safety profiles [16].
The table below summarizes key quantitative relationships between endosomal damage and cellular consequences, as established in recent research.
| Observed Phenomenon | Quantitative Relationship | Experimental Context | Citation |
|---|---|---|---|
| Endosomal Damage vs. Cytotoxicity | Direct correlation between the rate and magnitude of endosomal disruption and measured cytotoxicity. | In vitro models using Galectin-9 reporter systems. | [4] |
| LNP-induced Inflammation | Intratracheal LNP instillation (7.5 µg mRNA dose) caused a >10-fold increase in pro-inflammatory cytokines (IL-6, TNF-α) and severe lung "hepatization". | In vivo mouse model. | [2] |
| Inefficient Endosomal Escape | Only ~1-2% of internalized siRNA is released into the cytoplasm from endosomes/lysosomes. | Study of ionizable lipid nanoparticle delivery. | [18] |
| RNA-less Damaged Endosomes | A high percentage of LNP-damaged endosomes (~80% for mRNA-LNPs; ~26-33% for siRNA-LNPs) contain no detectable RNA cargo. | Live-cell microscopy of vesicles with galectin-9 recruitment. | [1] |
Detailed Experimental Protocols
Protocol 1: Quantifying Endosomal Disruption Kinetics Using a Galectin-9 Reporter
Purpose: To systematically measure LNP-induced endosomal membrane damage and its relationship to cargo expression and cytotoxicity [4].
Key Reagents & Cells:
- Cells: Primary Human Dermal Fibroblasts (NHDFs) or other physiologically relevant cell types [16].
- Reporter: Fluorescently tagged Galectin-9 (e.g., Galectin-9-GFP) [2].
- LNPs: Formulations with fluorescently labeled cargo (e.g., Cy5-mRNA) to track uptake.
Methodology:
- Cell Culture & Transfection: Culture NHDF cells in media supplemented with varying concentrations of FBS (e.g., 2% and 10%) to assess the impact of serum proteins. Transfert cells with the Galectin-9-GFP construct.
- LNP Application: Apply LNPs containing Cy5-labeled mRNA to the cells. Use a range of doses to establish a dose-response profile.
- Live-Cell Imaging & Kinetic Analysis: Use confocal or live-cell microscopy to track, in real-time:
- Cellular Uptake: Quantify the fluorescence intensity of Cy5 signal inside cells.
- Endosomal Disruption: Quantify the recruitment and fluorescence intensity of Galectin-9-GFP to endosomal membranes.
- Cargo Expression: If the mRNA encodes a reporter like eGFP, quantify its expression over time.
- Cytotoxicity Assessment: In parallel, perform a standard cytotoxicity assay (e.g., LDH release, MTT) at relevant time points post-LNP application.
- Data Correlation: Correlate the kinetic data (uptake rate, peak Galectin-9 signal, time to Galectin-9 recruitment) with both final cargo expression levels and cytotoxicity metrics [4] [16].
Protocol 2: Differentiating Endosomal Damage Sensor Pathways
Purpose: To determine whether LNPs create large, irreparable holes (recruiting galectins) or smaller, repairable holes (recruiting the ESCRT machinery) [2].
Key Reagents & Cells:
- Cells: RAW 264.7 macrophages or other immune-responsive cells.
- Reporters: Fluorescently tagged Galectin-3 and an ESCRT component, such as CHMP4B [2].
- LNPs: Formulations with different ionizable lipids (e.g., traditional cKK-E12 vs. novel ESCRT-recruiting lipids).
Methodology:
- Cell Preparation: Seed cells expressing the fluorescent damage sensors (Galectin-3 and CHMP4B).
- LNP Exposure: Treat cells with the different LNP formulations.
- High-Resolution Imaging: At defined time points post-treatment, fix the cells and image using super-resolution microscopy.
- Phenotype Classification: Categorize damaged endosomes based on the primary sensor recruited:
- Galectin-Dominant: Vesicles with strong Galectin-3 signal indicate large, irreparable membrane damage.
- ESCRT-Dominant: Vesicles with strong CHMP4B signal indicate smaller, repairable damage.
- Functional Correlation: Measure the inflammatory cytokine output (e.g., via ELISA for IL-6, TNF-α) from cells treated with each LNP type. LNPs that preferentially recruit the ESCRT machinery should demonstrate high cargo expression with minimal inflammation [2].
The Scientist's Toolkit: Key Research Reagents
This table lists essential reagents and their functions for investigating endosomal trauma.
| Research Reagent | Function & Application |
|---|---|
| Galectin-9 (Fluorescent Reporter) | A highly sensitive sensor for detecting endosomal membrane damage/rupture. Recruitment indicates major endosomal disruption [4] [2]. |
| Ionizable Cationic Lipids (e.g., MC3, cKK-E12) | The primary LNP component responsible for endosomal escape. Its chemical structure (headgroup pKa, tail saturation) dictates the efficiency and toxicity of membrane disruption [16] [2]. |
| ESCRT Pathway Reporters (e.g., CHMP4B) | Markers for the cellular machinery that repairs small holes in endosomal membranes. Recruitment is associated with lower inflammation [2]. |
| Modified mRNA (e.g., N1-methyl-pseudouridine) | mRNA with modified nucleosides reduces innate immune recognition by the cell, helping to isolate lipid-induced toxicity from RNA-induced immunogenicity [16]. |
Signaling Pathways in Endosomal Trauma
The diagram below illustrates the two primary cellular pathways activated by LNP-induced endosomal damage.
Endosomal Damage Sensing Pathways
Experimental Workflow for Cytotoxicity Analysis
This diagram outlines a logical workflow for troubleshooting LNP-induced cytotoxicity in an experimental setting.
Cytotoxicity Analysis Workflow
Engineering Gentler LNPs: Lipid Design for Minimal Membrane Disruption
FAQs: Troubleshooting Ionizable Lipids and LNP Formulation
Q1: Our LNP formulations are triggering significant inflammatory responses in vivo. What is the mechanism, and how can we mitigate this?
A1: Inflammation is often a direct result of endosomal damage caused by the ionizable lipid. During endosomal escape, some lipids create large, irreparable holes in the endosomal membrane. These holes are sensed by cytosolic proteins called galectins (particularly galectin-9), which initiate a potent inflammatory cascade, leading to the secretion of cytokines like IL-6 and TNF-α [2] [1]. Solution: To mitigate this, focus on developing ionizable lipids that create smaller, more transient pores in the endosomal membrane. These smaller holes can be repaired by the cellular ESCRT (Endosomal Sorting Complexes Required for Transport) machinery, thereby preventing galectin sensing and subsequent inflammation. Research shows that LNPs engineered to recruit the ESCRT pathway can achieve high cargo expression with minimal inflammatory side effects [2].
Q2: We are experiencing low RNA delivery efficiency despite high cellular uptake. What are the key intracellular barriers?
A2: Our analysis identifies multiple distinct inefficiencies in the cytosolic delivery pathway [1]:
- Inefficient Endosomal Damage: Only a fraction of internalized LNPs successfully trigger endosomal membrane damage (marked by galectin recruitment) conducive to cargo release.
- Inefficient Cargo Release: Even in galectin-positive damaged endosomes, only a small fraction of the RNA cargo is actually released into the cytosol.
- Component Segregation: During endosomal sorting, the ionizable lipid and RNA payload can segregate from each other, both within single endosomes and across different compartments. This means an endosome can be damaged by the ionizable lipid yet contain little to no RNA, preventing functional delivery [1].
Q3: How can we improve the thermostability of our mRNA-LNP formulations to avoid the need for cryogenic storage?
A3: A major cause of mRNA instability in LNPs is the generation of reactive aldehyde impurities from the degradation of the ionizable lipid. These aldehydes covalently bind to mRNA nucleosides, inactivating them [19]. Solution: Innovate in ionizable lipid chemistry. Research demonstrates that piperidine-based ionizable lipids significantly limit the production of these aldehyde impurities. LNPs formulated with these lipids have been shown to maintain mRNA activity for up to five months when stored as a liquid at 4°C, whereas formulations with other ionizable lipids lost most of their activity within two months under the same conditions [19].
Q4: During scale-up, our LNP particle size and encapsulation efficiency become inconsistent. What manufacturing factors should we control?
A4: Consistency relies on precise control over the mixing process. Manual mixing or methods with low controllability result in polydisperse nanoparticles with poor encapsulation [20]. Solution: Implement controlled mixing technologies. Microfluidics is the gold standard for research and early development, offering superior control over mixing conditions (Total Flow Rate and Flow Rate Ratio) for highly reproducible, monodisperse LNPs (PDI < 0.2) with high encapsulation efficiency (≥90%) [21] [20]. For large-scale GMP production, turbulent jet mixers offer advantages, including smaller particle size, narrow distribution, high encapsulation efficiency, and easier scalability [22].
Q5: What are the critical quality attributes (CQAs) we must monitor for LNP characterization?
A5: Key CQAs for LNP characterization and process control include [22] [20]:
- Particle Size and Polydispersity Index (PDI): Affects biodistribution and cellular uptake. Aim for a small size (e.g., 50-200 nm) and low PDI.
- Encapsulation Efficiency: The percentage of RNA successfully encapsulated within the LNPs. Crucial for therapeutic efficacy.
- Surface Charge (Zeta Potential): Influences colloidal stability and interaction with biological membranes.
- RNA Integrity: Confirms the payload has not been degraded during formulation.
- Stability: The formulation's ability to maintain its physicochemical properties over time.
Key Experimental Protocols
Protocol: Assessing Endosomal Damage and Inflammatory Potential
This protocol uses galectin recruitment as a biomarker for LNP-induced endosomal damage [2] [1].
Methodology:
- Cell Preparation: Seed appropriate cell lines (e.g., RAW 264.7 macrophages or other relevant primary cells) into glass-bottom imaging dishes.
- Transfection: Treat cells with the experimental LNPs. Include controls (e.g., untreated cells, LNPs with known low-inflammatory lipids).
- Staining: Transfect or immuno-stain for a membrane damage sensor, such as galectin-9.
- Live-Cell Imaging: Use fast live-cell or super-resolution microscopy to image cells at defined time points post-transfection (e.g., 1-6 hours).
- Quantification: Quantify the number of galectin-9-positive vesicles per cell and correlate this with the dose of LNPs internalized. A lower ratio of galectin foci to internalized LNPs indicates a less inflammatory formulation [1].
Protocol: Evaluating Lipid Thermostability and mRNA Integrity
This protocol assesses the stability of mRNA-LNP formulations during storage [19].
Methodology:
- Formulation and Storage: Prepare mRNA-LNPs using standard methods (e.g., microfluidics) and divide them into aliquots.
- Stability Challenge: Store aliquots at different temperatures (e.g., -80°C, 4°C, 25°C) for varying durations (e.g., 1 week, 1 month, 3 months).
- Analysis of Aldehyde Impurities:
- Use a fluorescence-based assay with 4-hydrazino-7-nitro-2,1,3-benzoxadiazole hydrazine (NBD-H), which reacts with carbonyl compounds (aldehydes) to form fluorescent hydrazones.
- Incubate lipid samples with NBD-H and measure fluorescence; lower signals indicate fewer reactive aldehydes [19].
- Functional Potency Assay:
- Test the in vivo or in vitro efficacy of stored LNPs. For example, administer LNPs encoding a reporter protein (e.g., human erythropoietin, hEPO) to mice and measure serum protein levels via ELISA.
- Compare the functional output of fresh vs. stored LNPs to determine the rate of activity loss [19].
Data Presentation
Ionizable Lipids: Properties and Performance
Table 1: Commercially Available and Research-Grade Ionizable Lipids. This table provides a comparison of key lipids, including their pKa and noted characteristics, as cited in the literature [23] [19].
| Lipid Name | Reported pKa | Key Characteristics and Applications |
|---|---|---|
| SM-102 | ~6.68 [23] | Used in Moderna's Spikevax COVID-19 vaccine; benchmark for comparing new biodegradable lipids [23]. |
| ALC-0315 | ~6.09 [23] | Used in Pfizer/BioNTech's COVID-19 vaccine; clinically validated for strong immune responses [23]. |
| CP-LC-0729 | ~6.78 [23] | Next-generation lipid; 32-fold increase in pulmonary protein expression vs. MC3; biodegradable [23]. |
| CL15F (Piperidine-based) | 6.24 - 7.15 [19] | Research lipid; demonstrates superior thermostability, maintaining mRNA activity after 5 months at 4°C [19]. |
LNP Formulation: Core Composition and Critical Attributes
Table 2: LNP Component Functions and Target Ratios. This table summarizes the role of each key component in a standard LNP formulation [21] [20].
| LNP Component | Primary Function | Typical Molar Ratio |
|---|---|---|
| Ionizable Lipid | Encapsulates RNA via electrostatic interaction; enables endosomal escape via pH-dependent charge shift. | ~50% |
| Phospholipid (e.g., DSPC) | Provides structural integrity to the LNP bilayer; enhances stability and encapsulation efficiency. | ~10% |
| Cholesterol | Stabilizes the lipid bilayer; enhances membrane fusion and LNP stability. | ~38.5% |
| PEGylated Lipid | Shields LNP surface, improving colloidal stability, reducing aggregation, and modulating biodistribution. | ~1.5% |
Pathway and Workflow Visualizations
LNP Endosomal Escape and Damage Pathways
LNP Formulation and Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for LNP Research. This table lists key tools and their functions for developing and testing ionizable lipids [21] [23] [1].
| Reagent / Material | Function / Application |
|---|---|
| Ionizable Lipids (e.g., SM-102, ALC-0315, CP-LC-0729) | Benchmark compounds for comparing the performance of novel ionizable lipids [23]. |
| Piperidine-Based Lipid Libraries | Research lipids designed to improve thermostability and limit mRNA adduct formation [19]. |
| Fluorescently-Labeled Lipids (e.g., BODIPY-MC3) | Tracing the fate of the ionizable lipid component within cells using live-cell microscopy [1]. |
| Membrane Damage Reporters (e.g., Galectin-9) | Critical biosensors for visualizing and quantifying LNP-induced endosomal damage and inflammatory potential [2] [1]. |
| NBD-H (4-hydrazino-7-nitro-2,1,3-benzoxadiazole hydrazine) | Fluorescent dye used in a microplate assay to quantify reactive aldehyde impurities in lipid formulations [19]. |
| Microfluidic Mixing Systems | Enables reproducible, scalable production of LNPs with controlled size and high encapsulation efficiency [21] [20]. |
ESCRT Pathway FAQ & Troubleshooting Guide
This technical support resource addresses common experimental challenges and questions related to the Endosomal Sorting Complex Required for Transport (ESCRT) pathway, with a specific focus on its role in repairing endosomal damage in lipid nanoparticle (LNP) research.
Table 1: Frequently Asked Questions about the ESCRT Pathway
| Question | Expert Answer | Key References |
|---|---|---|
| What is the primary function of the ESCRT machinery? | The ESCRT machinery performs a unique membrane remodeling and scission reaction away from the cytoplasm. It is best known for driving intralumenal vesicle formation during multivesicular body (MVB) biogenesis but is also essential for cytokinetic abscission and viral budding. | [24] [25] [26] |
| Why is the ESCRT pathway relevant to LNP-induced endosomal damage? | LNPs can cause inflammation by creating holes in the endosomal membrane during "endosomal escape." Recent research shows that if these holes are smaller, the cell can recruit the ESCRT machinery to repair them, thereby reducing inflammatory responses. | [2] |
| Which ESCRT complexes are minimal requirements for membrane scission? | ESCRT-III is considered the minimal machinery required for the final membrane scission event. Processes like HIV budding and cytokinesis can occur with only ESCRT-I, ESCRT-III, and Vps4, bypassing the need for ESCRT-0 and ESCRT-II. | [24] [27] |
| How is the ESCRT pathway linked to neurodegenerative diseases? | ESCRT dysfunction impedes the MVB pathway, disrupting membrane protein turnover. This can lead to the accumulation of toxic proteins like α-synuclein, which is implicated in Parkinson's disease. Some ESCRT-III components, such as CHMP2B, directly interact with these proteins. | [27] [28] |
| What is the role of the Vps4 ATPase? | Vps4 is a key AAA-ATPase that hydrolyzes ATP to disassemble and recycle the ESCRT-III complex from the membrane after scission is complete. This is crucial for maintaining the functionality of the entire pathway. | [24] [29] |
Table 2: Troubleshooting Common ESCRT Experimental Issues
| Problem | Possible Cause | Suggested Solution | |
|---|---|---|---|
| High cytotoxicity when studying ESCRT inhibition | Non-specific or potent inhibition of ESCRT-III can block essential cellular processes like cytokinesis. | Consider using inducible or partial knockdown systems. Studies on the inhibitor retroCHMP3 show that accumulation of mutations that reduce cytotoxicity while preserving virus inhibition is possible. | [30] |
| Impaired endolysosomal degradation in ESCRT mutants | Loss of ESCRT function (e.g., Class E Vps mutants) blocks the MVB pathway, preventing cargo delivery to lysosomes. | Characterize the accumulation of aberrant prevacuolar/endosomal compartments (Class E compartments). Verify using markers for ubiquitinated cargo and late endosomes. | [24] [29] |
| Difficulty detecting transient ESCRT-III interactions | ESCRT-III subunits are transiently assembled on membranes and exist in auto-inhibited states in the cytoplasm. | Use co-immunoprecipitation or fluorescence polarization binding assays with purified recombinant proteins. Capture interactions with known partners like Vps4 or other MIT-domain containing proteins. | [24] [28] |
| Persistent α-synuclein oligomers in cellular models | α-synuclein can directly bind to ESCRT-III (e.g., CHMP2B), impeding endolysosomal function and its own degradation. | Disrupt the α-synuclein-ESCRT interaction using specific peptide inhibitors (e.g., PDpep1.3) to restore endolysosomal function and reduce oligomer levels. | [28] |
Experimental Protocols for Key ESCRT Assays
Protocol 1: Assessing ESCRT-Dependent Endosomal Repair
This protocol is adapted from recent research investigating how the ESCRT machinery repairs LNP-induced endosomal damage [2].
1. Objective: To quantify the recruitment of ESCRT proteins to damaged endosomes and correlate it with membrane repair and inflammation outcomes.
2. Key Materials:
- Galectin-3 or Galectin-8 antibody (Marker for large, irreparable membrane damage)
- Antibody against an ESCRT-III core subunit (e.g., CHMP4 / Snf7)
- Cells with knockdown/knockout of specific ESCRT components (e.g., Vps4)
- LNPs formulated with different ionizable lipids (e.g., standard vs. ESCRT-recruiting lipids)
3. Method:
- Treat cells with the LNPs of interest.
- Fix and stain cells at relevant time points post-treatment for Galectin and ESCRT-III proteins.
- Image and quantify using high-resolution confocal microscopy:
- The co-localization of ESCRT-III with damaged endosomes.
- The ratio of galectin-positive (large hole) to ESCRT-positive (small, reparable hole) endosomes.
- Correlate findings with downstream assays for inflammation (e.g., cytokine ELISA).
4. Expected Outcome: LNPs formulated with ESCRT-recruiting ionizable lipids should show higher ESCRT-III recruitment to endosomes, reduced galectin staining, and lower secretion of pro-inflammatory cytokines (e.g., IL-6, TNF-α) [2].
Protocol 2: Disrupting a Pathological ESCRT Interaction with a Peptide Inhibitor
This protocol is based on a study that identified a peptide to disrupt the α-synuclein-CHMP2B interaction [28].
1. Objective: To mitigate α-synuclein-mediated cytotoxicity by disrupting its inhibitory interaction with ESCRT-III.
2. Key Materials:
- PDpep1.3 peptide (Sequence: DEEIERQLKALG) and a scrambled control peptide.
- Cell models overexpressing wild-type or mutant (A53T) α-synuclein.
- Proteasome inhibitor (e.g., MG132) to induce proteostatic stress.
- Lentiviral system for peptide expression.
3. Method:
- Introduce peptides into cells via lentiviral transduction.
- Induce proteostatic stress by treating cells with MG132.
- Measure cell viability using a standard assay (e.g., MTT or CellTiter-Glo).
- Quantify α-synuclein oligomers using a protein fragment complementation assay (PCA), such as a luciferase-based PCA.
- Validate target engagement via co-immunoprecipitation to confirm disrupted α-synuclein-CHMP2B binding.
4. Expected Outcome: Cells expressing the PDpep1.3 peptide, but not the scrambled control, should show increased cell viability under stress and a significant reduction in α-synuclein oligomer levels [28].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying ESCRT in Membrane Repair
| Reagent / Tool | Function in Research | Example Use Case | |
|---|---|---|---|
| ESCRT-Recruiting LNPs | LNPs with specific ionizable lipids that create smaller, reparable holes in the endosomal membrane. | To study high mRNA delivery with minimal inflammation; as a therapeutic tool for inflammatory diseases. | [2] |
| Peptide Inhibitor (PDpep1.3) | Disrupts the pathological interaction between α-synuclein and ESCRT-III subunit CHMP2B. | To restore endolysosomal function and reduce toxic protein oligomers in Parkinson's disease models. | [28] |
| Vps4 ATPase Mutants | Expressing dominant-negative Vps4 (e.g., ATPase-deficient) blocks ESCRT-III disassembly. | To study the consequences of a "frozen" ESCRT-III state on membrane scission and repair. | [24] [29] |
| Class E Vps Mutants | Yeast or mammalian cells with mutations in ESCRT genes (e.g., Δvps27, Δvps23). | To characterize the classic "Class E compartment" phenotype and study cargo sorting defects in the MVB pathway. | [24] [29] |
| recombinant CHMP2B | Purified ESCRT-III subunit for in vitro binding studies. | Used in fluorescence polarization assays to directly measure binding affinity for peptide inhibitors. | [28] |
ESCRT-Mediated Membrane Repair Signaling Pathway
The following diagram illustrates the cellular decision-making process when an endosome is damaged, highlighting the role of the ESCRT machinery.
ESCRT-III Assembly and Disassembly Workflow
This diagram details the sequential protein interactions that govern the dynamic assembly and disassembly of the ESCRT-III complex, the core machinery for membrane scission.
Frequently Asked Questions: Core Concepts
What is the primary advantage of using BEND lipids in LNPs? The primary advantage of BEND lipids is their demonstrated ability to significantly enhance endosomal escape, which is a major bottleneck in nucleic acid delivery. Their unique terminally branched structure increases the delivery efficiency of mRNA and CRISPR-Cas9 ribonucleoprotein complexes, leading to higher transfection and gene editing efficacy, in some cases by as much as tenfold compared to linear lipids used in commercial COVID-19 vaccines [31] [32].
How does the structure of BEND lipids contribute to reduced cellular damage? While the core BEND lipid study focuses on delivery efficacy, broader LNP research indicates that the nature of endosomal disruption is critical for damage. One strategy involves using ionizable lipids that create smaller, repairable holes in the endosomal membrane. These smaller holes allow for cargo release while enabling the cell to recruit the ESCRT (endosomal sorting complex required for transport) machinery to repair the damage. This repair process prevents large, irreparable ruptures that expose glycans to the cytosol and are detected by galectin proteins, which trigger inflammatory pathways [2]. BEND lipids' branched architecture may allow for finer control over the type of membrane disruption, potentially aligning with this less-damaging mechanism.
For which applications have BEND lipids shown particular promise? BEND lipids have shown high performance in several advanced therapeutic applications, including [33] [34]:
- Hepatic gene editing: Efficient delivery of mRNA and CRISPR-Cas9 ribonucleoprotein complexes to the liver for therapeutic gene editing.
- T cell engineering: Enhanced transfection of hard-to-transfect T cells, which is crucial for CAR-T cell and other immunotherapies.
Troubleshooting Guides: Experimental Design & Optimization
Challenge: Low Endosomal Escape and Transfection Efficiency
| Potential Cause | Proposed Solution | Key Experimental Parameters to Monitor |
|---|---|---|
| Suboptimal branching type or location | Ensure lipid synthesis creates terminal branching (at the end of the lipid tail) rather than branching near the amine headgroup. Test different branched caps (e.g., isopropyl, tert-butyl, sec-butyl) [33]. | • Transfection efficiency (e.g., luminescence from FLuc mRNA) [33]• Gene editing rate (e.g., % of cells with successful edits) [33] |
| Inefficient LNP formulation | Standardize LNP formulation using a herringbone microfluidic device. Use a consistent molar ratio of lipid components (e.g., 35:16:46.5:2.5 for IL/DOPE/Cholesterol/C14-PEG2000) to isolate the effect of the ionizable lipid structure [33]. | • LNP size and PDI (e.g., DLS to target 70-160 nm with PDI ~0.2) [33]• Encapsulation efficiency (should be >80%) [33]• pKa (should be ~6.0 for efficient endosomal escape) [33] |
| Insufficient understanding of structure-activity relationship (SAR) | Systematically vary the lipid tail length and branching pattern while keeping the amine core constant to establish robust SARs. Even minor structural changes can have substantial impacts on delivery efficacy [35]. | • In vivo protein expression (e.g., luciferase expression in target tissues like the liver) [35] |
Challenge: Managing LNP-Induced Inflammation and Cytotoxicity
| Potential Cause | Proposed Solution | Key Experimental Parameters to Monitor |
|---|---|---|
| Excessive endosomal membrane damage | Explore ionizable lipid designs that create smaller, ESCRT-repairable holes in the endosome. Inhibiting galectin-3 can also abrogate inflammation from existing LNP formulations, but engineering less-damaging lipids is a superior long-term strategy [2]. | • Cytokine secretion (e.g., IL-6, TNF-α) in cell culture supernatants or animal models (e.g., BAL fluid) [2]• Cell viability assays (e.g., MTT, LDH release) [16] |
| Fast kinetics of endosomal disruption | Research indicates that the rate of endosomal disruption correlates with cytotoxicity. Slower, more controlled disruption may improve safety profiles. The branched architecture of BEND lipids may offer a handle to tune this kinetic parameter [16]. | • Kinetics of endosomal damage (e.g., using galectin recruitment as a proxy for large, irreparable damage) [2]• High-content imaging to correlate LNP uptake with toxicity markers [16] |
| Lipid accumulation from slow degradation | Consider incorporating biodegradable chemical motifs, such as ester bonds, into the lipid tails. This promotes rapid clearance and reduces the risk of long-term toxicity, which is especially important for therapies requiring repeat dosing [16]. | • Lipid clearance rates in pharmacokinetic studies [16] |
Experimental Data and Protocols
Key Quantitative Findings on BEND Lipid Performance
The following table summarizes critical data from the foundational BEND lipid study, providing benchmarks for your own experiments [33].
| Lipid Structure (Example) | Branching Type | mRNA Delivery Efficiency (Relative to Linear Lipids) | Gene Editing Efficiency | Key Application Notes |
|---|---|---|---|---|
| E8i-494 | Isopropyl | Up to 10-fold increase in vitro | Significantly enhanced | Effective for hepatic delivery and T cell engineering [33]. |
| E12t-494 | tert-Butyl | Up to 10-fold increase in vitro | Significantly enhanced | Improved endosomal disruption due to conical shape [33]. |
| E8s-494 | sec-Butyl | Up to 10-fold increase in vitro | Significantly enhanced | Demonstrates the importance of branching stereochemistry [33]. |
| Linear Control (e.g., MC3) | None | Baseline | Baseline | Benchmark against established ionizable lipids [33]. |
Detailed Protocol: Synthesizing and Testing BEND Lipids
This protocol is adapted from the methods used in the primary research [33].
Synthesis of Branched Epoxides:
- Step 1 (C-C Coupling): Couple a primary bromoalkene with a commercially available branched Grignard cap (e.g., isopropyl, tert-butyl) via a copper-catalyzed Grignard reaction to produce a branched alkene. For longer chains, synthesize the primary bromoalkene first from a terminal dibromoalkane using a mono E2 reaction with tert-butoxide.
- Step 2 (Epoxidation): Convert the branched alkene into the corresponding branched epoxide using m-chloroperbenzoic acid (mCPBA). These two steps can be completed in less than 24 hours.
Synthesis of BEND Ionizable Lipids (ILs):
- React the branched epoxide with a polyamine core (e.g., 494: 2-(2-aminoethoxy)-N-(2-(4-(2-(2-aminoethoxy)ethyl)piperazin-1-yl)ethyl)ethan-1-amine) via an SN2 reaction to form the final BEND IL.
Formulation of LNPs:
- Use a herringbone microfluidic device to formulate LNPs at a standard molar ratio of 35:16:46.5:2.5 (IL:DOPE:Cholesterol:C14-PEG2000).
- Encapsulate mRNA at a 10:1 weight ratio (IL:mRNA).
LNP Characterization:
- Size and PDI: Measure via Dynamic Light Scattering (DLS). Target: 70-160 nm, PDI ~0.2.
- Encapsulation Efficiency: Use a Ribogreen assay. Target: >80%.
- pKa: Determine via TNS fluorescence assay. Target: ~6.0.
Functional Testing:
- In vitro Transfection: Incubate LNPs (e.g., dose of 20 ng FLuc mRNA/20,000 cells) with target cells (e.g., HeLa, T cells) for 24 hours and measure luminescence.
- In vivo Efficacy: Administer LNPs to animal models (e.g., via intravenous injection for liver targeting). Quantify protein expression (luciferase) or gene editing efficiency in target tissues.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in BEND Lipid Research |
|---|---|
| Primary Bromoalkenes | Establishes the length of the lipid tail in the synthetic scheme [33]. |
| Branched Grignard Caps (e.g., isopropyl, tert-butyl) | Introduces the key terminal branching group to the lipid structure [33]. |
| Polyamine Core 494 | Common amine core used to create ionizable lipids with a proven track record in various delivery applications [33]. |
| Helper Lipids (DOPE, Cholesterol, C14-PEG2000) | DOPE: Promotes non-bilayer structures that aid endosomal escape. Cholesterol: Stabilizes the LNP membrane. PEG-lipid: Reduces aggregation and controls particle size [33]. |
| Herringbone Microfluidic Device | Standardizes the LNP formulation process, ensuring reproducible particle size and encapsulation [33]. |
| Galectin Inhibitors | Tool compound used in mechanistic studies to confirm the role of galectin-sensed damage in LNP-induced inflammation [2]. |
Pathways and Mechanisms: Endosomal Damage and Repair
The diagram below illustrates the two primary fates of LNPs in the endosome and their consequences, which is central to the thesis of preventing endosomal damage.
Diagram 1: Fate of LNPs in the Endosomal Pathway and Consequences. The diagram contrasts how BEND lipids promote escape, and how the size of the resulting endosomal damage determines the inflammatory outcome.
Core Concepts: LNPs vs. Extracellular Vesicles
Table: Key Differences in Endosomal Escape Between LNPs and EVs
| Feature | Lipid Nanoparticles (LNPs) | Extracellular Vesicles (EVs) |
|---|---|---|
| Primary Escape Mechanism | Ionizable lipid-mediated membrane disruption [1] [7] | Fusogenic proteins (e.g., VSV-G) mediating membrane fusion [36] |
| Efficiency Estimate | ~1-2% of siRNA payload reaches cytosol [7] [37] | >10-fold higher than some commercial LNPs [7] |
| Membrane Damage | Can cause large, galectin-9-positive holes, triggering inflammation [1] [2] | Minimal membrane damage, efficient and "stealthy" escape [7] |
| Inflammatory Response | Can induce severe inflammation via galectin-sensing of damage [2] | Lower expression of inflammatory cytokines [37] |
| Key Components | Ionizable lipids, PEG-lipids, cholesterol, phospholipids [7] | Fusogenic proteins (e.g., VSV-G), tetraspanins, native lipids [7] [36] |
Troubleshooting Guide: Common LNP Escape Problems & Biomimetic Solutions
FAQ 1: Our LNP formulation shows good cellular uptake but poor functional protein expression. What is the likely bottleneck?
The primary bottleneck is likely inefficient endosomal escape. While uptake is often efficient, it is estimated that only 1-2% of the encapsulated siRNA in commercially available LNPs successfully escapes into the cytosol [7]. The majority of the material remains trapped in the endosomal-lysosomal pathway and is degraded [38].
- Diagnosis Checklist:
- Confirm Endosomal Entrapment: Use live-cell microscopy with fluorescently labeled RNA and endosomal markers (e.g., LysoTracker) to visualize co-localization.
- Test for Membrane Damage: Co-transfect a galectin-9 sensor (e.g., Galectin-9-GFP). The recruitment of galectin-9 to endosomes indicates LNP-induced membrane damage, which is a prerequisite for escape [1].
- Quantify Hit Rate: Analyze the fraction of galectin-9-positive damaged endosomes that actually contain your RNA payload. A low "hit rate" suggests payload and ionizable lipid segregation is a problem [1].
FAQ 2: Our therapeutic LNP causes significant inflammation. How can we mitigate this?
Inflammation is a common side effect of LNP-mediated endosomal escape. When ionizable lipids create large holes in the endosomal membrane, the cell senses this damage via proteins called galectins, which trigger an inflammatory response [2].
- Biomimetic & Engineering Solutions:
- Design "Smarter" Ionizable Lipids: Develop lipids that create smaller, more transient pores in the endosomal membrane. These smaller holes can be repaired by the cell's native ESCRT (Endosomal Sorting Complexes Required for Transport) machinery, minimizing galectin recruitment and subsequent inflammation [2].
- Inhibit the Damage Sensor: Research shows that inhibition of galectins can abrogate LNP-associated inflammation in vitro and in vivo [2].
- Learn from EVs: EVs naturally cause lower inflammatory cytokine expression compared to LNPs [37]. Incorporating EV-derived lipids or surface proteins into LNP design may confer these "stealth" properties.
FAQ 3: How can we directly apply EV escape mechanisms to improve our synthetic LNPs?
The high escape efficiency of EVs stems from their use of fusogenic proteins that promote fusion with the endosomal membrane rather than disruptive pore formation.
- Application Strategies:
- Incorporate Fusogenic Proteins: Engineer producer cells to co-express EV-sorting domains (e.g., CD63) and fusogenic proteins like VSV-G. The VEDIC (VSV-G plus EV-Sorting Domain-Intein-Cargo) system has been shown to achieve high-efficiency cytosolic delivery, with recombination rates over 66% in reporter cells [36].
- Biomimetic Lipid Compositions: Analyze and replicate the lipid composition of natural EVs, which may include high levels of phosphatidylserine or other lipids that promote membrane fusion and negative curvature, facilitating the transition to hexagonal phases conducive to content release [7].
Detailed Experimental Protocols
Protocol 1: Quantifying Endosomal Escape and Membrane Damage using Live-Cell Imaging
This protocol allows you to visualize the key inefficiencies in the LNP delivery process, as identified in recent research [1].
- Objective: To track LNP uptake, endosomal membrane damage, and RNA release in real-time.
- Key Reagents:
- Workflow:
- Cell Preparation: Seed cells in a glass-bottom imaging dish. Transfect with the Galectin-9-GFP plasmid 24 hours before imaging.
- LNP Application: Apply LNPs containing both labeled RNA and labeled lipid to the cells at the desired concentration (e.g., 0.72 µg/mL for siRNA-LNPs) [1].
- Image Acquisition: Use a confocal or super-resolution microscope with an environmental chamber. Acquire images every 5-10 minutes for 1-4 hours.
- Data Analysis:
- Track Co-localization: Follow individual endosomes to determine the timing of galectin-9 recruitment relative to LNP entry.
- Calculate Hit Rate: For each galectin-9-positive endosome, determine if labeled RNA is present. A low hit rate suggests payload/lipid segregation [1].
- Quantify Release: Look for a sudden decrease in RNA fluorescence in a galectin-9-positive endosome, indicating release into the cytosol.
Visualization of the experimental workflow for quantifying endosomal escape and membrane damage.
Protocol 2: Engineering EVs for High-Efficiency Delivery (VEDIC System)
This protocol details the creation of engineered EVs that mimic viral escape mechanisms, achieving high functional delivery [36].
- Objective: To produce EVs loaded with a cargo protein (e.g., Cre recombinase) capable of efficient endosomal escape in recipient cells.
- Key Reagents:
- Plasmids: CD63-Intein-Cre, VSV-G
- HEK293T cells (for EV production)
- Traffic Light (TL) Cre reporter cells (e.g., HeLa-TL, T47D-TL) [36]
- Tangential Flow Filtration (TFF) system for EV isolation
- Workflow:
- EV Production: Co-transfect HEK293T cells with the CD63-Intein-Cre and VSV-G plasmids.
- EV Harvest and Purification: Collect cell culture supernatant 48-72 hours post-transfection. Isolate and concentrate EVs using TFF, with optional further purification by Size Exclusion Chromatography (SEC) [36].
- Characterization: Determine EV concentration and size using Nanoparticle Tracking Analysis (NTA).
- Functional Assay: Apply isolated VEDIC EVs to Traffic Light reporter cells. Analyze by flow cytometry or microscopy after 48 hours for GFP expression, which indicates successful Cre-mediated recombination and cytosolic delivery.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Studying and Improving Endosomal Escape
| Reagent | Function | Example/Best Use |
|---|---|---|
| Ionizable Lipids | Protonate in acidic endosomes, disrupt membrane bilayer to enable escape [7]. | DLin-MC3-DMA: Benchmark for siRNA delivery. SM-102/ALC-0315: Used in COVID-19 mRNA vaccines. New designs focus on cone-shaped structures for better fusogenicity [7]. |
| Fusogenic Proteins | Mediate fusion between vesicle and endosomal membranes for efficient, low-inflammation escape [36]. | VSV-G: Highly effective in engineered EV systems like VEDIC. Can be incorporated into hybrid LNP systems. |
| Membrane Damage Reporters | Detect and quantify endosomal membrane disruptions, a key step in LNP escape and inflammation [1] [2]. | Galectin-3/9-GFP: Recruits to damaged endosomes. ESCRT Machinery Reporters: Indicate repair of smaller, less inflammatory membrane holes [2]. |
| Self-Cleaving Intein System | Enables efficient loading of soluble, active cargo into engineered EVs by releasing it from the EV membrane inside the vesicle lumen [36]. | Mtu RecA mini-intein: Used in the VEDIC system to link cargo (e.g., Cre) to EV-sorting domains (e.g., CD63), enabling cargo release upon vesicle formation [36]. |
| Traffic Light Reporter Cell Line | Sensitively measures functional cytosolic delivery of protein cargo (e.g., Cre recombinase) via a permanent fluorescent switch [36]. | HeLa-TL, T47D-TL: Cre delivery excises a red fluorescent protein (RFP) and leads to permanent GFP expression. Quantify by flow cytometry. |
The ionizable lipid is the cornerstone of a functional Lipid Nanoparticle (LNP), and its acid dissociation constant (pKa) is the critical parameter governing its behavior. This property creates a delicate balancing act: the pKa must be low enough to minimize toxicity and nonspecific binding in the bloodstream (pH 7.4) but high enough to facilitate sufficient protonation and membrane disruption in the endosome (pH ~5.5-6.5) for effective RNA release [39]. This protonation triggers fusogenicity—the ability of the LNP to fuse with or disrupt the endosomal membrane. However, excessive fusogenicity can cause large, irreparable endosomal damage, triggering galectin-dependent inflammatory responses [40]. This guide provides troubleshooting advice for optimizing this critical balance to achieve efficient yet safe endosomal escape.
Frequently Asked Questions (FAQs) and Troubleshooting
What is the ideal pKa range for an ionizable lipid, and why?
Answer: The optimal apparent pKa for an ionizable lipid in mRNA-LNPs is typically between 6.0 and 6.5 [39]. This range ensures the lipid is largely neutral at physiological pH (7.4), reducing cytotoxicity and nonspecific binding with anionic biomolecules during circulation. When the LNP is internalized into the endosome, the dropping pH (to ~5.5-6.5) protonates the lipid, giving it a positive charge. This charge is essential for interacting with the anionic endosomal membrane, inducing the non-lamellar phase transitions that facilitate membrane fusion or disruption and subsequent cargo release.
Troubleshooting: If you observe high cytotoxicity or rapid clearance in vivo, your formulation's pKa may be too high (>7). Conversely, if in vitro or in vivo expression is poor, the pKa may be too low (<5.5) to achieve sufficient protonation and endosomal escape. Measure your LNP's apparent pKa to guide redesign [39].
My LNPs show high transfection efficiency but also high inflammation. What could be happening?
Answer: This is a classic sign of excessive fusogenicity. Highly efficient, fusogenic lipids can create large, irreparable holes in the endosomal membrane [40]. The cell recognizes this severe damage via cytosolic galectin proteins, which then initiate a potent pro-inflammatory signaling cascade. You have successfully optimized for escape but at the cost of safety.
Troubleshooting: Explore ionizable lipids that generate smaller, transient pores in the endosomal membrane. Research indicates that such "mini-holes" can be recognized and repaired by the endosomal sorting complex required for transport (ESCRT) pathway, which actively recruits machinery to mend membrane damage. This allows for mRNA escape while mitigating galectin-triggered inflammation [40]. Look for lipids designed to recruit ESCRT machinery.
How can I accurately measure the apparent pKa of my LNP formulation?
Answer: The apparent pKa of a blank LNP (without RNA) can be measured using two primary methods. It is crucial to remember that the apparent pKa is an experimentally determined value for the entire nanoparticle, which can differ from the intrinsic pKa of the lone lipid molecule due to the local chemical environment [39].
Troubleshooting Guide for pKa Measurement:
- Problem: Inconsistent titration curves.
- Solution: Ensure your blank nanoparticles are thoroughly purified before potentiometric titration to remove any free ions or residual acid/base that could interfere with the measurement [39].
- Problem: Fluorescence signal is weak or noisy in the TNS assay.
- Solution: Confirm the pH of your buffer series is accurate. TNS must be freshly prepared in DMSO, and the ionic strength of the buffers should be kept consistent (e.g., 150 mM NaCl) to avoid artifacts [39].
- Problem: Inconsistent titration curves.
The table below summarizes the core methodologies.
| Method | Principle | Key Procedural Steps |
|---|---|---|
| Potentiometric Titration [39] | Measures pH change while titrating a nanoparticle suspension with base. The pKa is the pH at the midpoint between equivalence points. | 1. Suspend purified blank LNPs in a known concentration of HCl.2. Titrate with standardized NaOH (e.g., 0.1 M) while recording pH.3. Plot the titration curve; pKa is the midpoint pH. |
| TNS Fluorescence Assay [39] | A fluorescent dye (TNS) is non-fluorescent in water but emits strong fluorescence upon binding cationic surfaces. Fluorescence increases as pH drops and lipids protonate. | 1. Prepare a series of buffers covering pH 3-10.2. Mix blank LNPs and TNS dye in each buffer.3. Measure fluorescence (Ex/Em: 325/425 nm).4. Plot fluorescence vs. pH; pKa is the inflection point. |
Can computational tools help me design better ionizable lipids?
- Answer: Yes, absolutely. Computational methods are powerful tools to overcome the slow, resource-intensive trial-and-error of traditional screening.
- Physics-Based Modeling: Molecular Dynamics (MD) simulations, both all-atom and coarse-grained, can model LNP self-assembly, lipid-RNA interactions, and the molecular details of endosomal escape. Newer constant pH MD (CpHMD) methods can accurately simulate the protonation states of lipids in the LNP environment, directly informing on pKa [41].
- Machine Learning (ML): ML models like FormulationLNP can predict key LNP properties like in vivo delivery efficiency and apparent pKa directly from the chemical structure of the ionizable lipid, even with relatively small datasets [42]. This allows for in silico screening of vast virtual lipid libraries before synthesis.
Besides the ionizable lipid, what other formulation factors can influence performance?
- Answer: The entire LNP composition is a system where components interact.
- Helper Phospholipids: The choice between DSPC and DOPE significantly impacts fusogenicity. DOPE, which prefers a reverse hexagonal (HII) phase, can synergize with the ionizable lipid to enhance endosomal disruption and escape, but may also increase inflammation [43].
- PEG-Lipids: The type and molar percentage of PEG-lipid are critical for controlling LNP size, stability, and biodistribution. However, PEG can also create a steric barrier that potentially inhibits cellular uptake and endosomal fusion, a trade-off known as the "PEG dilemma" [44] [20]. Optimization of PEG content and linker chemistry is often necessary.
Experimental Protocols
Protocol 1: Measuring Apparent pKa via the TNS Fluorescence Assay
This is a sensitive and widely used method for determining the apparent pKa of LNPs [39].
- Buffer Preparation: Prepare a series of buffers (e.g., from pH 3 to 10) with constant ionic strength. Use a mixture of 10 mM borate, 10 mM phosphate, and 10 mM citrate, with 150 mM NaCl in all buffers.
- Nanoparticle Sample: Prepare blank LNPs (without RNA) and dilute them in each pH buffer to a consistent lipid concentration.
- Dye Addition: Add a small volume of TNS stock solution (300 µM in DMSO) to each LNP-buffer mixture. A typical final volume is 100 µL with 2 µL of TNS stock.
- Fluorescence Measurement: Incubate the mixtures for a short period and then measure the fluorescence intensity using a plate reader with excitation at 325 nm and emission at 425 nm.
- Data Analysis: Plot the fluorescence intensity as a function of pH. The apparent pKa is identified as the pH at the inflection point of the resulting sigmoidal curve.
Protocol 2: Evaluating Endosomal Damage and Inflammation In Vitro
To assess whether your LNP escape mechanism is causing excessive damage, you can probe for the key danger sensors.
- Cell Treatment: Treat relevant immune cells (e.g., macrophages or dendritic cells) with your LNP formulation.
- Inhibition/Gene Silencing: To confirm the mechanism, use galectin inhibitors (e.g., lactose) or employ siRNA to knock down key galectin proteins (like Galectin-3 or -9) in a test group [40].
- Cytokine Measurement: 12-24 hours post-transfection, collect the cell culture supernatant.
- Analysis: Use an ELISA or a multiplex cytokine array to measure the levels of pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α. A significant reduction in inflammation in the galectin-inhibited group confirms the role of endosomal damage-driven inflammation [40].
Essential Research Reagents and Materials
The following table lists key reagents and their functions for research in this field.
| Reagent/Material | Function in Research |
|---|---|
| Ionizable Lipids (e.g., SM-102, ALC-0315, MC3, novel designs) | The primary functional component; its structure dictates pKa and fusogenicity. Different lipids are used to tune LNP performance [45]. |
| Helper Phospholipids (e.g., DSPC, DOPE) | Provides structural integrity to the LNP bilayer; DOPE specifically enhances fusogenicity and promotes endosomal escape [43]. |
| TNS Fluorescent Dye | A critical research tool for experimentally determining the apparent pKa of blank LNP formulations [39]. |
| Galectin Inhibitors (e.g., lactose) | Pharmacological tools used in vitro to probe the mechanism of inflammation and confirm galectin-mediated sensing of endosomal damage [40]. |
| Microfluidic Mixer (e.g., NanoAssemblr) | The gold-standard equipment for producing uniform, reproducible, and stable LNPs with high encapsulation efficiency, essential for reliable experimental results [45] [20]. |
Pathways and Workflow Diagrams
LNP Endosomal Escape and Inflammation Pathways
This diagram illustrates the two primary cellular pathways determined by the pKa and fusogenicity of the LNP. The optimal balance leads to safe, ESCRT-repaired escape, while excessive fusogenicity triggers galectin-mediated inflammation.
LNP Optimization Workflow
This workflow outlines the iterative process of designing, formulating, and testing LNPs. The key checkpoints of pKa measurement, efficiency, and safety assessment are essential for identifying a successful lead candidate.
Solving the PEG Dilemma and Fine-Tuning LNP Formulations
In the field of nanomedicine, Polyethylene Glycol (PEG) has become the polymer of choice for creating "stealth" nanoparticles that can evade the immune system. By forming a protective, hydrophilic layer on the nanoparticle surface, PEG reduces opsonization—the process where blood plasma proteins bind to foreign particles—and subsequent clearance by the mononuclear phagocyte system (MPS). This results in dramatically prolonged circulation time, allowing nanoparticles to accumulate in target tissues like tumors through the Enhanced Permeability and Retention (EPR) effect. However, this very advantage creates a significant challenge known as the "PEG dilemma": the same stealth properties that prolong circulation time also create a steric barrier that inhibits essential interactions with target cells, reducing cellular uptake and impeding endosomal escape, which is crucial for the intracellular delivery of therapeutic cargo like nucleic acids [46] [47] [48].
This dilemma is particularly acute in gene and nucleic acid therapy, where carriers must not only reach the target tissue but also successfully deliver their cargo to the correct intracellular compartment (the cytosol or nucleus) to be therapeutically effective. The PEG layer can inhibit both the initial binding to the cell membrane and the subsequent destabilization of the endosomal membrane necessary to release the cargo before degradation in the lysosome [48]. The following sections will dissect this dilemma through a technical support format, providing troubleshooting guides, strategic solutions, and detailed experimental protocols to help researchers navigate these challenges.
Troubleshooting Guide: FAQ on the PEG Dilemma
FAQ 1: Why does my PEGylated lipid nanoparticle (LNP) show excellent circulation time but poor therapeutic efficacy in vivo?
This is a classic symptom of the PEG dilemma. The PEG corona successfully confers stealth properties, reducing MPS uptake and increasing circulation half-life. However, this same corona creates a steric barrier that:
- Inhibits Cellular Uptake: It prevents close contact and interaction between the nanoparticle and the cellular membrane, hindering processes like endocytosis [46] [47].
- Impairs Endosomal Escape: PEG stabilizes the lipid bilayer of the nanoparticle, making it less likely to fuse with or disrupt the endosomal membrane. This traps the therapeutic cargo (e.g., mRNA or siRNA) in the endosome, leading to its degradation and loss of function [46] [48].
FAQ 2: My LNP formulation is highly inflammatory. Could PEG be the cause?
While the ionizable lipid is often the primary source of inflammation, the process of endosomal escape—a hallmark of LNP function—is a significant contributor. Recent 2025 research has shown that endosomal escape, necessary for RNA delivery, can trigger inflammation by causing endosomal membrane damage. Large, irreparable holes in the endosomal membrane are recognized by cytosolic galectin proteins (e.g., Galectin-3), which activate downstream inflammatory pathways [40] [49]. Therefore, the very mechanism your LNP uses to deliver its cargo can be inherently inflammatory. Strategies that minimize this damage, such as using ionizable lipids that create smaller, reparable holes, can mitigate this effect [40].
FAQ 3: I've heard about "Anti-PEG Antibodies." How significant is this problem?
Anti-PEG antibodies are a well-documented and growing concern. Their presence can lead to the Accelerated Blood Clearance (ABC) phenomenon, where repeated administration of PEGylated nanoparticles is cleared rapidly from the bloodstream, reducing therapeutic efficacy [46] [50]. During the COVID-19 pandemic, hypersensitivity reactions to PEGylated mRNA vaccines brought this issue to the forefront [51]. The problem is dose-dependent and can be more pronounced with nucleic acid-containing nanoparticles. It is crucial to differentiate between the immunogenicity of PEG (i.e., its ability to generate antibodies) and the general immunostimulatory nature of the LNP platform and its cargo [51].
FAQ 4: What is the optimal PEG density and chain length for balancing stealth and delivery?
The optimal PEG configuration is a balance. The following table summarizes the effects of PEG coverage density, based on in vitro and in vivo studies:
Table 1: Effects of PEG Coverage Density on Nanoparticle Properties
| PEG Density (mol%) | PEG Conformation | Circulation Time | Cellular Uptake & Endosomal Escape | Stability |
|---|---|---|---|---|
| < 5% | Mushroom | Moderate | Higher | Lower, potential aggregation |
| ~5-10% | Mushroom to Brush | Prolonged (Optimal) | Reduced | Good |
| >10-15% | Brush | Prolonged | Strongly Inhibited | May destabilize liposomes |
For chain length, PEG with a molecular weight of 2000 Da (PEG~2000~) is often considered a standard, providing a good balance of stealth and the ability to be displaced or shed [50]. Very short PEG chains cannot effectively prevent protein absorption, while very long chains can create an insurmountable barrier to cell interaction [46] [50].
Strategic Solutions to Overcome the PEG Dilemma
Several innovative strategies have been developed to circumvent the limitations of PEG.
1. Active Targeting: This involves functionalizing the distal end of PEG chains with targeting ligands (e.g., antibodies, peptides, aptamers, folates). These ligands bind specifically to receptors overexpressed on target cells, promoting receptor-mediated endocytosis and overcoming the steric hindrance of the PEG layer [46] [48].
2. Cleavable PEGylation: In this approach, the PEG polymer is conjugated to the nanoparticle via a cleavable linker. The linker is designed to be stable in the bloodstream but break in response to specific stimuli in the tumor microenvironment or inside the cell, such as:
- Low pH
- Reducing conditions (high glutathione levels)
- Specific enzymes (e.g., matrix metalloproteinases) Once cleaved, the PEG shell is shed, restoring the nanoparticle's ability to interact with cells and escape the endosome [46] [48].
3. Biomimetic Coatings: Using membranes derived from natural cells (e.g., red blood cells, leukocytes, platelets) to cloak nanoparticles is a promising alternative. For instance, a red blood cell membrane contains proteins like CD47, which acts as a "marker of self" (a "do not eat me" signal), leading to prolonged circulation without interfering with cellular uptake in the same way as synthetic PEG [46].
4. Advanced Ionizable Lipids for Controlled Endosomal Escape: Recent research highlights a novel class of ionizable lipids designed to minimize inflammatory responses. These lipids are engineered to create smaller, transient pores in the endosomal membrane, which are sufficient for cargo release but can be repaired by the cell's own Endosomal Sorting Complex Required for Transport (ESCRT) machinery. This repair mechanism prevents sustained endosomal damage and the subsequent activation of galectin-driven inflammatory pathways [40] [49].
The logical relationship between LNP composition, its intracellular journey, and the resulting efficacy and safety outcomes can be visualized in the following pathway diagram:
Experimental Protocols for Evaluating PEG Dilemma Solutions
Protocol 1: Assessing Endosomal Escape Efficiency using a Galectin-3 Recruitment Assay
This protocol leverages the latest 2025 research on endosomal damage sensing [40] [49].
- Objective: To quantify the extent of endosomal membrane damage caused by LNPs by measuring the recruitment of Galectin-3, a marker of membrane rupture.
- Materials:
- Cells stably expressing GFP-tagged Galectin-3 (e.g., HeLa or primary macrophages).
- Test LNP formulations (e.g., with standard vs. ESCRT-recruiting ionizable lipids).
- Confocal microscopy setup.
- Cell culture reagents.
- Method:
- Seed cells onto glass-bottom imaging dishes and culture until 60-70% confluent.
- Transfect cells with the GFP-Galectin-3 plasmid if not using a stable line.
- Treat cells with LNPs loaded with a fluorescently-labeled RNA (e.g., Cy5-mRNA) for 4-6 hours.
- Fix cells, stain nuclei with DAPI, and mount for imaging.
- Acquire z-stack images using a confocal microscope.
- Data Analysis:
- Quantify the number of cytoplasmic puncta (dots) of GFP-Galectin-3 that co-localize with Cy5-positive endosomes.
- LNPs causing severe endosomal damage will show significantly higher co-localization, indicating robust galectin recruitment and a higher inflammatory potential.
Protocol 2: Comparing Cellular Uptake and Transfection Efficiency
- Objective: To directly evaluate how PEGylation impacts the internalization and functional delivery of nucleic acid cargo.
- Materials:
- Relevant cell line (e.g., HeLa, HEK293, or a primary cell model).
- PEGylated and non-PEGylated LNPs encapsulating GFP-mRNA or luciferase-siRNA.
- Flow cytometer or plate reader.
- Lysis buffers and qPCR reagents if measuring mRNA levels.
- Method:
- Seed cells in 12-well or 24-well plates.
- Treat cells with a standardized dose (e.g., 50 nM RNA) of both PEGylated and non-PEGylated LNPs.
- For Uptake: After 4-6 hours, trypsinize cells, wash thoroughly, and analyze the geometric mean fluorescence of the cell population via flow cytometry to measure internalized Cy5-labeled LNPs.
- For Transfection/Functional Delivery: After 24-48 hours, analyze GFP expression via flow cytometry or fluorescence microscopy, or measure luciferase activity/gene knockdown using a plate reader or qRT-PCR.
- Data Analysis:
- A successful stealth-but-active formulation should show only a modest reduction in uptake compared to non-PEGylated LNPs but a high level of functional delivery, indicating efficient endosomal escape has been maintained.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating the PEG Dilemma in LNPs
| Reagent Category | Example Compounds | Function & Rationale |
|---|---|---|
| PEG-Lipids | DSPE-PEG~2000~, DMG-PEG~2000~, PEG-DMG | Provides the stealth coating. Varying chain length (1k-5k Da) and anchor lipid (DSPE vs. DMG) influences stability and shedding. [50] [52] |
| Ionizable Lipids | DLin-MC3-DMA, SM-102, ALC-0315 | The "engine" of the LNP, critical for self-assembly, encapsulation efficiency, and endosomal escape. Novel lipids are designed to be less inflammatory. [40] [53] |
| Helper Lipids | DSPC, DOPE, Cholesterol | Provide structural integrity to the LNP bilayer. DOPE is often favored for its tendency to promote non-bilayer structures that facilitate endosomal escape. [53] [48] |
| Targeting Ligands | Folate, Transferrin, Anisamide, Antibody Fab' fragments | Conjugated to the end of PEG chains to mediate active targeting to specific cell surface receptors, overcoming the steric barrier of PEG. [48] |
| Cleavable Linkers | pH-sensitive (e.g., vinyl ether), Reducible (disulfide), Enzyme-cleavable (e.g., MMP substrate) | Used in cleavable PEGylation strategies to shed the PEG layer upon encountering specific intracellular or tumor microenvironment conditions. [46] [48] |
Frequently Asked Questions (FAQs) on SAXS/SANS for LNP Analysis
Q1: What are the key advantages of using SAXS and SANS over other techniques for analyzing LNP structure?
SAXS and SANS are powerful techniques for understanding the mesoscopic architecture of Lipid Nanoparticles (LNPs) in conditions that mimic their natural state. Unlike other methods, they provide population-average structural information under physiological conditions. The table below compares them to other common techniques.
| Technique | Key Advantages for LNP Analysis | Common Limitations |
|---|---|---|
| SAXS/SANS | Probes internal nanostructure (1-200 nm) in solution; provides ensemble-average data; can monitor dynamic processes like pH-induced changes [54] [55]. | Does not visualize individual particles; requires robust modeling for data interpretation [54]. |
| Cryo-EM | Directly visualizes individual particle morphology and internal structure (e.g., "bleb" compartments) [55] [56]. | Limited observable region, leading to potential statistical bias; cannot distinguish molecular identity [54] [57]. |
| DLS | Rapidly measures hydrodynamic diameter and polydispersity [54]. | Only provides overall size; cannot resolve internal structure [54]. |
| Cryo-OrbiSIMS | Provides molecular identity and depth profiling of components (e.g., confirms PEG-lipid orientation) without requiring labels [57]. | Laboratory-based technique; requires cryogenic sample preparation [57]. |
Q2: Our SAXS data for mRNA-loaded LNPs shows a "quasi-periodic" signal. What does this indicate?
This is an expected and crucial finding. The quasi-periodic structure in your SAXS profile originates from the self-assembly of mRNA and ionizable lipids within the LNP core. The negatively charged mRNA backbone and the positively charged, protonated ionizable lipids form an electrostatically driven complex that exhibits a regular, repeating pattern detectable by SAXS. Specialized models, such as a Gaussian distribution model, can be applied to characterize this feature, which is a hallmark of successful nucleic acid encapsulation [54].
Q3: How does LNP structure, as revealed by scattering techniques, relate to the inflammatory response caused by endosomal damage?
Advanced structural characterization is key to understanding and mitigating LNP-induced inflammation. Research shows that the ionizable lipid component dictates the size of the "holes" formed in the endosomal membrane during escape. LNPs that create large, irreparable holes trigger recognition by cytosolic galectin proteins, leading to inflammatory signaling [40] [49]. SAXS can help identify and characterize LNPs formulated with a unique class of ionizable lipids that create smaller holes. These smaller holes can be repaired by the cellular ESCRT pathway, resulting in high mRNA expression with significantly reduced inflammation [40]. Therefore, SAXS/SANS are critical tools for designing safer, non-inflammatory LNPs.
Q4: What is a proven SAXS model for resolving the complex layered structure of LNPs?
A spherical core-triple shell model has been successfully validated for characterizing the hierarchical organization of LNPs. This model resolves the following layers [54]:
- Inner Lipid Layer: The core, which can contain the mRNA-ionizable lipid complex.
- Intermediate Hydrophilic Region.
- Outer PEG Corona: The surface layer dominated by PEG-lipids.
This model has been applied to commercial formulations like Comirnaty, showing that controlled variations in the Nitrogen-to-Phosphorus (N/P) ratio produce distinguishable structural features in the SAXS profile [54].
Q5: How can we improve the resolution of SAXS/SANS for heterogeneous LNP samples?
Coupling SAXS and SANS with a separation technique like Asymmetric Flow Field-Flow Fractionation (AF4) significantly enhances resolution. Online AF4-SAXS/SANS separates particles by size before measurement, reducing heterogeneity and allowing for shape-resolved analysis across the entire elution profile. This integrated approach can resolve primary particles down to ~5 nm and has been used to identify a 2–3 nm polar shell enveloping the hydrophobic lipid core [58].
Troubleshooting Guides
Issue 1: Poor Resolution or Indistinct SAXS/SANS Features
| Possible Cause | Solution | Supporting Protocol/Theory |
|---|---|---|
| High sample polydispersity | Implement an online separation method. Use Asymmetric Flow Field-Flow Fractionation (AF4) coupled directly to your SAXS or SANS instrument. This fractionates the sample by size, allowing you to analyze a more monodisperse population and obtain clearer scattering data [58]. | Protocol Note: Using D₂O as a solvent in AF4-SANS can further sharpen resolution by reducing particle diffusion due to higher solvent viscosity [58]. |
| Inadequate modeling | Employ a core-triple shell model for a more nuanced fit of your SAXS data. This model accounts for the inner lipid layer, intermediate hydrophilic region, and outer PEG corona, providing a more accurate representation of the LNP's complex architecture than simpler models [54]. | Theoretical Basis: The core-triple shell model establishes quantitative correlations between formulation parameters (like N/P ratio) and the resulting mesoscopic structure, directly linking chemistry to function [54]. |
| Weak scattering contrast | For SANS, use selective deuteration. By deuterating specific lipid components (e.g., DSPC) and varying the D₂O concentration in the solvent, you can manipulate the scattering length density (SLD) contrast to highlight different structural regions within the LNP [55] [56]. | Experimental Design: Plan a series of SANS experiments with systematically deuterated components to build a comprehensive structural model [55]. |
Issue 2: Difficulty Correlating Structural Data with Biological Function (Endosomal Escape)
| Challenge | Troubleshooting Strategy | Related Experimental Context |
|---|---|---|
| Linking LNP nanostructure to endosomal damage | Correlate your SAXS/SANS structural data with galectin recruitment assays. The same LNP batches characterized by scattering should be tested in live-cell imaging experiments using a fluorescent galectin-9 reporter. This directly links LNP structure to the induction of endosomal membrane damage [1] [4]. | Key Finding: Membrane damage marked by galectin recruitment is conducive to cytosolic RNA release, while ESCRT recruitment is not. The rate and magnitude of endosomal disruption correlate with cytotoxicity [1] [4]. |
| Low functional delivery efficiency | Use scattering to screen for LNPs with inverse hexagonal phase propensity. While not a direct measurement, SAXS can identify non-lamellar phases that are theorized to facilitate endosomal escape. Focus on ionizable lipids that promote this structural transition at endosomal pH (~pH 6.5) [40]. | Key Finding: A unique class of ionizable lipids can create smaller, ESCRT-repairable holes in the endosome, leading to high cargo expression with minimal inflammation [40]. |
| Uncertainty in component localization | Combine SAXS/SANS with Cryo-OrbiSIMS. While scattering provides an average model, Cryo-OrbiSIMS can directly validate the spatial orientation of specific lipids (e.g., confirming the PEG fragment of DMG-PEG2k is on the LNP surface while the lipid anchor is buried) [57]. | Validating Model: The core-triple shell SAXS model proposes an outer PEG corona, which is directly confirmed by Cryo-OrbiSIMS depth profiling [54] [57]. |
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagents for SAXS/SANS LNP Studies
| Reagent/Material | Function in LNP Formulation & Structural Study |
|---|---|
| Ionizable Lipid (e.g., ALC-0315, DLin-MC3-DMA) | Critical for mRNA encapsulation and endosomal escape; its pKa and structure dictate LNP internal organization and phase behavior [54] [1]. |
| Helper Phospholipid (e.g., DSPC) | Provides structural integrity to the LNP bilayer; can be deuterated for contrast matching in SANS experiments [54] [56]. |
| Cholesterol | Modulates membrane fluidity and stability, enhancing LNP structural integrity [54]. |
| PEG-lipid (e.g., ALC-0159, DMG-PEG2k) | Controls particle size, provides stealth properties, and forms the outer "PEG corona" detectable in SAXS models [54] [57]. |
| Deuterated Lipids (e.g., d-DSPC) | Used in SANS to selectively enhance the scattering contrast of specific components, allowing for precise mapping of their location within the LNP [55] [56]. |
| Citrate Buffer (pH 4.0) | Aqueous phase for LNP formation; acidic pH facilitates mRNA encapsulation by protonating the ionizable lipid [54]. |
Experimental Workflow & Pathway Visualization
The following diagram illustrates the integrated workflow for using SAXS/SANS to guide the development of LNPs with reduced endosomal damage.
Integrated LNP Development Workflow
The pathway below details the cellular mechanism of LNP-induced endosomal damage and the structural features that influence it, providing biological context for your characterization work.
Endosomal Damage and Inflammation Pathway
In the development of Lipid Nanoparticles (LNPs), ionizable lipids often command the spotlight for their pivotal role in endosomal escape. However, the structural and functional helper lipids—phospholipids and cholesterol—are equally critical for creating safe and effective delivery systems. These components are not merely inert fillers; they define the integrity, stability, and intracellular fate of the LNP. This guide addresses key challenges researchers face in optimizing these helper lipids to enhance LNP efficacy while mitigating undesirable endosomal damage and cellular toxicity.
Troubleshooting Guide: Helper Lipids and Endosomal Damage
Problem 1: Inconsistent Endosomal Escape Efficiency
- Question: "My mRNA-LNPs show good cellular uptake, but protein expression is low. How can my helper lipid formulation improve endosomal escape?"
- Answer: Inefficient escape from endosomes is a major bottleneck, often resulting in the degradation of the RNA payload. The composition of helper lipids directly influences the LNP's ability to disrupt the endosomal membrane.
- Phospholipid Selection: The choice of phospholipid, such as DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine), is crucial for forming a stable lipid bilayer. This bilayer fuses with the endosomal membrane, a key step in the release process [59]. Ensure the phospholipid is of high purity and that its phase transition temperature is compatible with your ionizable lipid.
- Cholesterol Optimization: Cholesterol and its analogs are not just structural components. They regulate membrane fluidity and permeability. Replacing standard cholesterol with an analog like β-sitosterol can significantly promote endosomal escape. The structure of β-sitosterol, which includes an alkyl substitution at the C-24 position, disrupts the regular packing of the endosomal membrane, making it more permeable and facilitating the release of the nucleic acids into the cytoplasm [59].
Problem 2: LNP Formulation Instability and High Polydispersity
- Question: "My LNP preparations are unstable, aggregating in storage, and have a high PDI. How do helper lipids contribute to this?"
- Answer: Instability often points to an imbalance in the LNP's core composition, particularly the ratio of structural lipids.
- Cholesterol's Role: Cholesterol acts as a molecular glue, filling the gaps between lipid molecules and enhancing the packing density and stability of the LNP [38]. Suboptimal cholesterol content can lead to a loose structure, cargo leakage, and particle aggregation.
- Phospholipid Function: Helper phospholipids like DSPC form the primary monolayer that encapsulates the LNP core. An incorrect molar ratio can lead to incomplete surface coverage or phase separation, resulting in high polydispersity and inconsistent batch-to-batch performance [59].
Problem 3: Unacceptable Levels of Cellular Toxicity
- Question: "My LNP treatment causes significant cytotoxicity, which is a concern for therapeutic applications. Is this linked to my helper lipids?"
- Answer: While ionizable lipid chemistry is a primary driver of toxicity, helper lipids can modulate these effects. Cytotoxicity is frequently linked to excessive and prolonged endosomal disruption [16] [4].
- Mechanism of Toxicity: When LNPs disrupt endosomes, the cell perceives this as membrane damage. This triggers repair pathways, including the recruitment of galectin proteins and the ESCRT machinery. If the damage is too widespread or persistent, it can lead to inflammatory signaling and cell death [1] [16].
- The Role of Optimization: Fine-tuning the ratio of cholesterol and phospholipids can help achieve a balance where endosomal escape is efficient without causing overwhelming, sustained damage. A well-structured LNP with optimized helper lipids may create a more controlled, transient disruption, thereby improving the therapeutic window [4].
Quantitative Data: Impact of Helper Lipid Composition
Table 1: Characterizing the Impact of Cholesterol Analogs on LNP Physicochemical Properties
| Cholesterol Analog | Key Structural Feature | Impact on Particle Size | Impact on PDI | Postulated Effect on Endosomal Escape |
|---|---|---|---|---|
| Cholesterol | Standard plant-derived sterol with a hydroxyl group. | Baseline | Baseline | Provides standard membrane stability and fusion [60] [59]. |
| β-Sitosterol | Alkyl substitution at the C-24 position. | May reduce size compared to baseline [60]. | May lead to a lower PDI [60]. | Disrupts endosomal lipid packing, enhances membrane permeability, and promotes escape [59]. |
Table 2: Troubleshooting Guide for Common Helper Lipid-Related Issues
| Observed Problem | Potential Root Cause | Experimental Adjustment | Expected Outcome |
|---|---|---|---|
| Low transfection efficiency | Suboptimal membrane fusion due to rigid phospholipid or poor cholesterol content. | Substitute DSPC with a phospholipid with a lower phase transition temperature; Test β-sitosterol. | Enhanced endosomal membrane fusion and disruption, leading to increased protein expression [59]. |
| High cytotoxicity | Excessive, sustained endosomal disruption. | Increase mol% of cholesterol to improve LNP stability; Fine-tune the ionizable lipid-to-helper lipid ratio. | Reduced galectin-9 recruitment and activation of innate immune sensors, lowering toxicity [16] [4]. |
| Poor batch-to-batch reproducibility & high PDI | Improper or inconsistent molar ratios of helper lipids during formulation. | Standardize microfluidic mixing parameters; systematically vary phospholipid (e.g., 5-20 mol%) and cholesterol (20-50 mol%) ratios. | Improved particle stability, consistent size distribution, and more predictable in vivo performance [60] [38]. |
Experimental Protocol: Optimizing Helper Lipids
Objective: To systematically evaluate the effect of cholesterol analogs and phospholipid ratios on LNP efficacy and endosomal damage.
Methodology:
LNP Formulation:
In Vitro Characterization:
- Physicochemical Properties: Use dynamic light scattering (DLS) to measure particle size, polydispersity index (PDI), and zeta potential for each formulation [60].
- Encapsulation Efficiency: Use a dye-based assay like the Quant-it RiboGreen RNA Assay to determine the percentage of encapsulated mRNA [60].
Functional and Safety Assessment in Cells:
- Model System: Use physiologically relevant cells such as primary human dermal fibroblasts (NHDFs) or immune cell lines [16].
- Transfection Efficiency: Transfert cells with LNPs encapsulating eGFP mRNA. Quantify protein expression 24 hours post-transfection using flow cytometry or Western Blot [60] [16].
- Quantifying Endosomal Damage: Use a galectin-9 reporter system.
- Transfert cells with a plasmid expressing a fluorescent protein (e.g., GFP) tagged to galectin-9.
- Treat cells with the experimental LNPs and use live-cell imaging to track the recruitment of Galectin-9-GFP to endosomes.
- Quantify the kinetics (rate and magnitude) and number of galectin-9-positive endosomes as a direct measure of endosomal disruption [16] [4].
- Cytotoxicity Measurement: Perform a cell viability assay (e.g., MTT or LDH) 24-48 hours after LNP treatment. Correlate viability data with galectin-9 recruitment metrics [16].
The workflow for this experimental protocol is outlined below.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Helper Lipids in LNPs
| Reagent / Material | Function in Experimental Workflow | Key Consideration for Helper Lipid Research |
|---|---|---|
| DSPC | A saturated phospholipid that provides structural integrity to the LNP bilayer. | Its high phase transition temperature (~55°C) contributes to LNP stability at physiological temperatures [60] [59]. |
| Cholesterol | A natural sterol that enhances LNP stability and packing, and modulates membrane fluidity. | Sourced from plant (e.g., Avanti Polar Lipids, catalog: 700100P) or animal origins; purity is critical for reproducibility [60] [16]. |
| β-Sitosterol | A cholesterol analog used to investigate enhanced endosomal escape. | Its unique alkyl tail disrupts endosomal membrane packing more effectively than cholesterol, promoting nucleic acid release [59]. |
| DMG-PEG2000 | A PEGylated lipid that confers stability, reduces aggregation, and modulates pharmacokinetics. | The molar percentage and PEG chain length can shield LNP surface and influence cellular uptake [60] [38]. |
| Galectin-9 Reporter Plasmid | A biosensor to visualize and quantify endosomal membrane damage in live cells. | The rate and magnitude of galectin-9 recruitment correlate with LNP-induced cytotoxicity, providing a key safety metric [16] [4]. |
| Microfluidic Mixer | Instrumentation for precise, reproducible, and scalable LNP formulation. | Enables systematic screening of different helper lipid ratios while maintaining consistent particle characteristics [38]. |
Frequently Asked Questions (FAQs)
Q1: Can I simply use the same helper lipid ratios from siRNA-LNPs for mRNA-LNPs? A: Not necessarily. While the components are similar, optimal ratios can differ. mRNA is larger and requires robust encapsulation and efficient cytosolic release for translation. Empirical optimization of phospholipid and cholesterol ratios for your specific mRNA cargo and target cell type is strongly recommended [38] [61].
Q2: How does the ionizable lipid influence the choice of helper lipids? A: The ionizable lipid is the primary driver of endosomal escape, but helper lipids are essential collaborators. The hydrophobic tail of the ionizable lipid interacts with cholesterol and the phospholipid tails within the LNP structure. An ionizable lipid designed for a conical shape (promoting hexagonal phase transition) will require helper lipids that provide initial stability but do not overly constrain this transformative process [59]. The formulation is a synergistic system.
Q3: What is the most direct way to confirm that my helper lipid optimization is reducing endosomal damage? A: The most direct method is to implement the galectin-9 recruitment assay [16] [4]. By quantitatively comparing the number of galectin-9 positive vesicles and the intensity/duration of the signal between your old and new formulations, you can directly assess the level of endosomal disruption. A successful optimization should show maintained or improved protein expression alongside a reduction in sustained galectin-9 signals and lower cytotoxicity.
The success of RNA therapeutics hinges on the development of effective lipid nanoparticle (LNP) delivery vehicles. Traditional formulation approaches have relied heavily on trial-and-error methods, creating significant bottlenecks in therapeutic development. High-throughput screening (HTS) has emerged as a transformative solution, enabling researchers to systematically evaluate thousands of potential LNP formulations and identify optimal candidates with unprecedented speed and precision. This technical support center addresses the specific challenges researchers face when implementing HTS platforms, with particular emphasis on mitigating endosomal damage—a critical barrier to efficient RNA delivery and a significant source of inflammatory responses.
Frequently Asked Questions (FAQs)
FAQ 1: How does high-throughput screening specifically help overcome endosomal trapping and damage?
HTS enables the rapid evaluation of how different lipid compositions affect endosomal escape and membrane damage. By screening vast libraries of ionizable lipids, researchers can identify formulations that balance efficient RNA delivery with minimal endosomal disruption. Advanced HTS platforms can now screen over 400 different LNP formulations simultaneously, identifying lipids that create smaller, reparable endosomal holes via the ESCRT pathway instead of large, irreparable damages that trigger galectin-mediated inflammation [2] [62]. This systematic approach moves beyond the single-formulation testing that previously limited progress in understanding endosomal processing.
FAQ 2: What are the key cellular sensors for LNP-induced endosomal damage, and how can we screen for their activation?
The primary sensors for LNP-induced endosomal damage are galectins (particularly galectin-9) and components of the ESCRT machinery [1] [2]. Galectins recognize membrane damage by binding to glycans exposed to the cytosol upon endosomal rupture, while ESCRT proteins attempt to repair membrane damage. Screening methods include:
- Live-cell microscopy with fluorescently tagged galectins to detect recruitment to damaged endosomes [1]
- Super-resolution microscopy to visualize localized ionizable lipid enrichment in endosomal membranes [1]
- Quantification of galectin-positive foci per cell using automated image analysis
- Assessment of ESCRT component recruitment to endosomal membranes
FAQ 3: Why do many damaged endosomes show no detectable RNA cargo, and what does this mean for delivery efficiency?
Recent research reveals that RNA payload and ionizable lipid components segregate during endosomal sorting, both within single endosomes and across endosomal compartments [1]. This segregation means that membrane damage can occur independently from RNA release, resulting in galectin-positive endosomes with minimal RNA content. For siRNA-LNPs, approximately 30% of damaged vesicles lack detectable siRNA, while for mRNA-LNPs, this increases to approximately 80% [1]. This represents a major efficiency barrier in LNP-mediated delivery, as only a fraction of damaged endosomes actually contribute to functional cytosolic RNA delivery.
FAQ 4: What HTS approaches best predict in vivo performance for tissue-specific targeting?
Traditional in vitro models poorly predict in vivo biodistribution. Advanced HTS methods now enable direct in vivo screening through:
- Peptide barcoding: LNPs encapsulating mRNAs encoding unique peptide barcodes can be pooled and administered together; LC-MS/MS analysis then identifies which formulations successfully deliver to target tissues [62]
- Barcoded lipid screening: Combinatorial synthesis of cationic, degradable lipid-like materials screened using DNA barcodes to quantify delivery to specific organs [63] These approaches allow screening of hundreds of formulations in a single animal, overcoming limitations of traditional low-throughput methods [62].
Troubleshooting Guides
Problem: High Efficiency but Significant Inflammation in Lead Formulations
Issue: Formulations show excellent RNA expression but trigger unacceptable inflammatory responses through endosomal damage pathways.
Solution: Focus screening on ionizable lipids that create ESCRT-recruitable membrane holes rather than large, irreparable ruptures.
Step-by-Step Protocol:
- Primary Screening: Implement a galectin recruitment assay using live-cell imaging of galectin-9-GFP expressed in target cells.
- Counter-Screening: Test hits from primary screening in an ESCRT recruitment assay monitoring markers like ALIX or CHMP4B.
- Hit Validation: Select formulations that show minimal galectin recruitment but maintain ESCRT association.
- Inflammation Profiling: Measure pro-inflammatory cytokines (IL-6, TNF-α, IFN-β) in target cells and relevant immune cells.
- In Vivo Confirmation: Validate in disease models using therapeutically relevant mRNA doses and routes of administration.
Expected Outcomes: LNPs formulated with specific ionizable lipid classes can create intermediate-sized holes reparable by ESCRT, driving strong mRNA expression while minimizing inflammation [2].
Problem: Poor Correlation Between In Vitro Screening and In Vivo Performance
Issue: Formulations that perform well in cellular models fail to show adequate tissue targeting or expression in animal models.
Solution: Implement direct in vivo screening methodologies that bypass in vitro limitations.
Step-by-Step Protocol:
- Library Design: Prepare a diverse library of LNP formulations varying ionizable lipids, phospholipids, and PEG-lipids.
- Barcode Integration: Encapsulate unique peptide- or DNA-barcoded mRNAs in each formulation.
- Pooled Administration: Mix multiple barcoded formulations and administer to a single animal.
- Tissue Processing: Harvest target tissues at appropriate timepoints post-administration.
- LC-MS/MS Analysis: Quantify peptide barcode levels to identify top-performing formulations [62].
- Lead Validation: Reformulate top hits with therapeutic mRNA for confirmation studies.
Expected Outcomes: Identification of formulations with true tissue-specific targeting capability, significantly reduced animal use, and accelerated screening timeline.
Key Experimental Protocols
Protocol 1: Quantifying Endosomal Damage and Cargo Release
Objective: Simultaneously monitor LNP-induced endosomal damage and RNA cargo release in live cells.
Materials:
- Galectin-9-GFP expressing cell line
- Fluorescently labeled RNA (AlexaFluor 647 for siRNA, Cy5 for mRNA)
- LNPs with labeled ionizable lipid (BODIPY-MC3) and labeled RNA
- Confocal or super-resolution microscope with live-cell imaging capability
Methodology:
- Seed cells in glass-bottom imaging dishes 24 hours before experimentation.
- Add dual-labeled LNPs (containing both BODIPY-MC3 and fluorescent RNA) at optimized concentration.
- Perform time-lapse imaging every 30-60 seconds for 2-4 hours.
- Track individual endosomes from point of LNP uptake through galectin recruitment.
- Quantify fluorescence intensity of both lipid and RNA channels before and after damage events.
- Calculate the "hit rate" - percentage of galectin-positive endosomes containing detectable RNA cargo [1].
Data Interpretation:
- Successful release: Galectin recruitment followed by RNA signal decrease in endosome with concurrent increase in cytosol.
- Failed release: Galectin recruitment without RNA release, or RNA-containing endosomes without galectin recruitment.
Protocol 2: High-Throughput Screening of LNP Libraries for Endosomal Escape Efficiency
Objective: Rapidly screen large LNP libraries for endosomal escape capability while monitoring membrane damage.
Materials:
- Automated liquid handling system (e.g., NanoGenerator Flex-S Plus)
- Library of LNP formulations with varied ionizable lipids
- Reporter cell line with cytosolic GFP activation upon RNA delivery
- High-content imaging system
- Galectin-9-RFP expressing cell line
Methodology:
- Use automated platform to formulate 48-96 LNP samples per run with minimal reagent volumes.
- Seed reporter cells in 384-well plates and add LNP formulations using automated dispensing.
- At 24 hours post-transfection, fix cells and image using high-content imager.
- Quantify GFP-positive cells (successful delivery) and galectin-9-RFP foci (membrane damage) per well.
- Calculate delivery efficiency-to-damage ratio for each formulation.
- Select leads with high delivery efficiency but minimal galectin recruitment [63].
Data Analysis:
- Normalize delivery efficiency to LNP uptake using labeled lipids.
- Cluster formulations based on delivery-damage profiles.
- Prioritize formulations in the high-delivery, low-damage quadrant.
Research Reagent Solutions
Table: Essential Materials for HTS of LNPs with Reduced Endosomal Damage
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Ionizable Lipids | MC3, ALC-0315, SM-102, cKK-E12 | Core LNP component enabling RNA encapsulation and endosomal escape; primary determinant of membrane damage [63] [2] |
| ESCRT-Recruiting Lipids | Asymmetric A3-lipids, specific ionizable lipid classes | Create smaller, reparable endosomal holes that minimize galectin activation and inflammation [2] |
| Membrane Damage Sensors | Galectin-9-GFP, Galectin-3-RFP | Detect and quantify endosomal membrane damage in live and fixed cells [1] [2] |
| ESCRT Machinery Markers | ALIX antibodies, CHMP4B-GFP | Identify formulations that recruit repair machinery instead of triggering inflammation [2] |
| Barcoding Systems | Peptide-encoding mRNAs, DNA barcodes | Enable pooled in vivo screening of multiple LNP formulations in single animals [63] [62] |
| Automated Formulation Platforms | NanoGenerator Flex-S Plus, IJM NanoScaler Pro | High-throughput, reproducible LNP production with minimal reagent consumption [63] |
Critical Quality Attributes and Process Parameters
Table: Key Parameters for Screening LNPs with Reduced Endosomal Damage
| Parameter Category | Specific Parameter | Measurement Technique | Impact on Endosomal Damage |
|---|---|---|---|
| Critical Process Parameters (CPPs) | Ionizable lipid structure & pKa | Titration assays, LC-MS | Determines endosomal membrane interaction and hole size [63] [2] |
| Lipid ratios (ionizable:phospholipid:sterol:PEG) | HPLC, compositional analysis | Affects LNP stability, unpacking, and endosomal interaction kinetics [64] | |
| N/P ratio (amine to phosphate) | Spectrophotometry, fluorescence | Influences RNA loading and release characteristics in endosomes [64] | |
| Critical Quality Attributes (CQAs) | Size and PDI | Dynamic light scattering (DLS) | Affects cellular uptake pathway and endosomal processing [63] [64] |
| Encapsulation efficiency | RiboGreen assay | Impacts how much RNA is available for cytosolic delivery [63] | |
| Galectin recruitment index | Live-cell microscopy, high-content imaging | Direct measure of endosomal membrane damage [1] [2] | |
| ESCRT recruitment potential | Super-resolution microscopy, immunofluorescence | Indicator of reparable vs. irreparable membrane damage [2] | |
| Biological Performance Metrics | Cytosolic delivery efficiency | Functional protein expression, reporter assays | Ultimate measure of successful endosomal escape [1] |
| Inflammatory cytokine profile | ELISA, multiplex assays (IL-6, TNF-α, IFN-β) | Quantification of immune activation due to endosomal damage [2] | |
| Endosomal cargo release efficiency | Single vesicle tracking, fluorescence quantification | Measures fraction of RNA actually released from damaged endosomes [1] |
Pathway and Workflow Visualizations
Diagram: Endosomal Processing Pathways for LNPs - This diagram illustrates the critical branching point where LNPs either trigger inflammatory galectin pathways or reparable ESCRT-mediated damage, determining both delivery efficiency and safety profiles.
Diagram: HTS Workflow for LNPs with Reduced Endosomal Damage - This workflow integrates in vitro and in vivo screening approaches to identify LNP formulations that maximize RNA delivery while minimizing endosomal damage and inflammation.
Moving beyond trial-and-error lipid design requires integrating advanced HTS platforms with mechanistic understanding of endosomal processing. By implementing the protocols and troubleshooting guides outlined above, researchers can systematically identify LNP formulations that balance efficient RNA delivery with minimal endosomal damage. The key innovation lies in screening not just for delivery efficiency, but specifically for endosomal damage pathways, focusing on the balance between galectin-recruiting and ESCRT-recruiting membrane interactions. This approach enables development of safer, more effective RNA therapeutics with reduced inflammatory potential, particularly critical for applications in sensitive patient populations and inflammatory disease states.
Troubleshooting Guide: FAQs on LNPs and Pre-Existing Inflammation
Why do Lipid Nanoparticles (LNPs) exacerbate pre-existing inflammation, and what is the core mechanism?
LNPs can severely worsen pre-existing inflammatory conditions through a mechanism rooted in their core function: endosomal escape. This process, while necessary for delivering RNA therapeutics, causes endosomal membrane damage, which the cell interprets as a danger signal [65] [2].
Core Mechanism: The ionizable lipid in LNPs is designed to create pores in the endosomal membrane to release the RNA cargo into the cytosol. This action can cause physical damage to the endosome [2].
- Large, irreparable holes in the endosomal membrane are recognized by cytosolic proteins called galectins (e.g., galectin-3, galectin-9). This recognition triggers a potent downstream inflammatory signaling cascade, leading to the release of cytokines like IL-6, TNF-α, and IL-1β [2].
- This inflammatory response is dramatically amplified if inflammation is already present. For instance, in mice with LPS-induced acute lung injury, administering LNPs led to a 4–28-fold increase in inflammatory cytokines compared to healthy controls [66].
Key Experimental Evidence: Studies in mouse models of acute lung injury (ALI) or idiopathic pulmonary fibrosis (IPF) showed that a single high dose of mRNA-LNPs could cause severe lung "hepatization" (a pathology where the lung resembles inflamed liver tissue), immune cell infiltration, and even 100% mortality after repeated dosing in IPF mice [66].
How can I design LNPs to minimize inflammation, especially for use in inflammatory disease models?
The key is to engineer LNPs that achieve efficient endosomal escape while minimizing the sensing of endosomal damage. Two primary strategies have emerged:
- Use Rapidly Biodegradable Ionizable Lipids: These lipids are designed to create smaller, more transient pores in the endosomal membrane. These smaller holes can be repaired by the cell's own Endosomal Sorting Complex Required for Transport (ESCRT) machinery. By avoiding large, irreparable holes, the LNP bypasses the galectin-sensing pathway and subsequent inflammatory signaling [65] [2].
- Incorporate Novel Anti-Inflammatory Components: Research shows that adding specific compounds to the LNP formulation can directly counter the inflammatory pathway.
- Ursolic Acid: When incorporated as a fifth component in a phosphoramide-derived LNP (creating a Non-Inflammatory LNP, or NIF-LNP), ursolic acid was found to activate the V-ATPase complex. This enhances endosome acidification and promotes efficient endosomal escape and mRNA expression without triggering significant reactogenicity. This formulation showed a 40-fold enhancement in lung protein expression without causing significant inflammation compared to LNPs with ALC-0315 [66].
- Galectin Inhibition: Studies show that directly inhibiting galectins can abrogate LNP-associated inflammation both in vitro and in vivo [2].
My LNP formulation works well in healthy animal models but fails in disease models. What factors should I re-evaluate?
This common issue often stems from the heightened immune state in disease models. You should re-evaluate your LNP's lipid composition beyond the ionizable lipid.
- Helper Lipids Matter: The choice of phospholipid and sterol can significantly influence both protein expression and the quality of the immune response, and this effect can differ between healthy and inflamed environments [67].
- Phospholipids: LNPs containing DOPE may enhance certain immune responses (like total IgG and IgG1), while DSPC-based LNPs might show the highest initial protein expression in healthy models [67].
- Sterols: Replacing cholesterol with β-sitosterol can significantly enhance protein expression in vitro. However, β-sitosterol-incorporated LNPs also induce elevated levels of both pro- and anti-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6, IL-1RA), potentially via inflammasome activation. This could be detrimental in an already inflamed setting [67].
The table below summarizes how helper lipid choices can lead to different biological outcomes.
Table 1: Impact of Helper Lipids on LNP Performance and Immunogenicity
| Lipid Component | Example | Observed Impact on LNP Performance | Potential Impact on Immune Response |
|---|---|---|---|
| Phospholipid | DOPE | Can promote membrane fusion and endosomal escape due to its tendency to form hexagonal phases [67]. | Enhanced total IgG and IgG1 responses in immunization studies [67]. |
| Phospholipid | DSPC | Contributes to high particle stability and integrity due to rigid, tightly packed lamellar structures [67]. | In vivo expression and immunogenicity profile can differ from DOPE-containing LNPs [67]. |
| Sterol | β-Sitosterol | Can enhance luciferase protein expression in vitro compared to cholesterol [67]. | Induces elevated levels of both pro- (TNF-α, IL-1β, IL-6) and anti-inflammatory (IL-1RA) cytokines [67]. |
Are the inflammatory effects driven by the mRNA cargo or the LNP delivery system itself?
The inflammatory effects are primarily driven by the LNP delivery system itself, specifically the ionizable lipid component. However, the mRNA cargo can also contribute.
- LNP-Driven Inflammation: Empty LNPs (with no RNA cargo) and LNPs loaded with a non-RNA, negatively charged polymer can trigger robust inflammatory cytokine release (e.g., IL-1α, IL-6, TNF-α). This confirms that the lipid component itself is intrinsically immunogenic [2] [68]. The ionizable lipid SM-102, for example, has been shown to potently activate the NLRP3 inflammasome, leading to robust IL-1β release [68].
- mRNA-Driven Inflammation: Unmodified mRNA can be recognized as a foreign pathogen by cellular RNA sensors (e.g., RIG-I, MDA-5, TLRs), activating innate immunity and type I interferon responses [69] [70]. Using modified nucleosides like N1-methylpseudouridine (m1Ψ) can reduce this activation [69].
- Synergistic Effect: The combined effect of the mRNA cargo and the LNP components can create a synergistic inflammatory response. The specific ionizable lipid used can influence the magnitude of the antiviral response triggered by both unmodified and modified mRNA [69].
Essential Experimental Protocols for Inflammation Assessment
Protocol 1: Evaluating LNP-Induced Inflammation and Exacerbation in Pre-Existing Inflammation
This protocol is adapted from studies that demonstrated LNP-induced inflammation and its exacerbation in mouse models of acute inflammation [71] [66].
Objective: To assess the innate immune response and inflammatory exacerbation potential of a novel LNP formulation in mice with pre-existing inflammation.
Materials:
- Animals: Wild-type mice (e.g., C57BL/6).
- Inflammogen: Lipopolysaccharide (LPS).
- Test Articles: LNP formulation(s) of interest, control LNP, vehicle control (e.g., PBS).
- Reagents: ELISA kits for cytokines (e.g., IL-6, TNF-α, IL-1β, MIP-2), protein quantification assay (e.g., BCA), reagents for bronchoalveolar lavage (BAL).
Method:
- Induce Pre-Existing Inflammation: Administer LPS to mice via intratracheal (e.g., 1 mg/kg) or intravenous (e.g., 2 mg/kg) injection [71].
- Administer LNP: At a predetermined time post-LPS (e.g., 4 hours [71]), administer the test LNP intravenously at a therapeutically relevant dose (e.g., 0.32 mg/kg mRNA [71]).
- Collect Samples: At the experimental endpoint (e.g., 2-24 hours post-LNP administration), collect blood (for serum), BAL fluid, and tissues (e.g., lung, liver).
- Analyze Inflammatory Markers:
- Cytokine Levels: Quantify pro-inflammatory cytokines in serum and BAL fluid using ELISA.
- BAL Analysis: Measure total protein concentration (indicator of capillary leak) and perform cell counts (to assess leukocyte infiltration) [2] [66].
- Histopathology: Examine lung tissues for signs of inflammation, immune cell infiltration, and damage (e.g., hepatization, alveolar thickening) [66].
Expected Outcome: Inflamed mice treated with LNPs will show significantly elevated levels of inflammatory markers (e.g., IL-6 in serum, MIP-2 in liver) compared to inflamed mice treated with a vehicle control or healthy mice treated with the same LNP [71].
Protocol 2: Testing the Role of Endosomal Damage and Galectins
This protocol leverages the mechanistic link between endosomal damage sensing and inflammation [2].
Objective: To determine if a novel LNP's inflammatory profile is mediated by galectin sensing of endosomal damage.
Materials:
- Cell Line: Macrophage cell line (e.g., RAW 264.7) or primary macrophages.
- Test Articles: LNP formulation(s) of interest.
- Inhibitor: Pharmacological galectin inhibitor (e.g., GB1107 for galectin-3).
- Reagents: qPCR reagents, ELISA kits for cytokines (IL-6, TNF-α), cell viability assay.
Method:
- Pre-treatment: Pre-treat macrophages with a galectin inhibitor or vehicle control for a set time.
- LNP Exposure: Expose the cells to the test LNPs (e.g., at 400 ng/mL lipid concentration [2]) for 6-24 hours.
- Analysis:
- Gene Expression: Harvest cells and analyze the expression of inflammatory genes (e.g., Il6, Tnf, Ifnb) via qPCR.
- Protein Secretion: Collect cell culture supernatant and measure cytokine secretion via ELISA.
- Viability: Assess cell viability to ensure the effects are not due to cytotoxicity.
Expected Outcome: If the LNP triggers inflammation primarily via galectin sensing, the galectin inhibitor will significantly reduce the upregulation of inflammatory cytokines and genes compared to the vehicle control group [2].
Signaling Pathway: LNP-Induced Endosomal Damage and Inflammation
The following diagram illustrates the key signaling pathways by which LNPs trigger inflammation through endosomal damage, and the proposed strategies for mitigation.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Studying LNP-Induced Inflammation
| Reagent | Function / Role in Research | Example / Note |
|---|---|---|
| Ionizable Lipids | The primary driver of endosomal escape and inflammation. Different structures are tested for biodegradability and reduced immunogenicity. | cKK-E12, SM-102, ALC-0315 (benchmark lipids); PL32 (a phosphoramide-derived lipid with high efficiency) [2] [67] [66]. |
| Helper Lipids | Modulate LNP stability, fluidity, and immune profile. Systematic screening is crucial. | DSPC, DOPC, DOPE (phospholipids); Cholesterol, β-sitosterol (sterols) [67]. |
| Anti-Inflammatory Additives | Compounds added to formulations to directly counteract inflammatory pathways. | Ursolic Acid: Activates V-ATPase for enhanced, non-inflammatory delivery [66]. Galectin Inhibitors: Abrogate inflammation in vitro and in vivo [2]. |
| N1-methylpseudouridine (m1Ψ) | A modified nucleoside incorporated into mRNA to reduce innate immune recognition by RNA sensors (e.g., TLRs, RIG-I) [69]. | Used in licensed mRNA vaccines to lower reactogenicity from the mRNA cargo [69] [70]. |
| LPS (Lipopolysaccharide) | A toll-like receptor 4 agonist used to establish robust, acute pre-existing inflammation in animal models for testing LNP exacerbation [71]. | Allows for the creation of controlled in vivo models of inflammation (e.g., acute lung injury). |
| Cytokine Detection Kits | Essential for quantifying inflammatory responses in cell culture media, serum, and BAL fluid. | ELISA kits for IL-6, TNF-α, IL-1β, IFN-β are frequently used to profile the inflammatory response [2] [71] [66]. |
Experimental Workflow: From LNP Formulation to In Vivo Assessment
The diagram below outlines a standard workflow for screening and evaluating novel LNP formulations for their inflammatory potential.
Bench to Bedside: Evaluating Next-Generation LNPs in Disease Models
FAQs: Bridging the IVIVC Gap in Lipid Nanoparticle Research
FAQ 1: Why do my LNPs show excellent mRNA expression in vitro but poor performance in vivo? This common discrepancy arises because conventional in vitro tests often fail to recapitulate the complex biological environment encountered in vivo. A key factor is the use of serum-starved conditions in vitro, which drastically reduces transfection efficiency compared to the serum-rich in vivo environment [72]. Furthermore, in vivo, LNPs interact with biomolecules that form a "protein corona" on their surface, which dynamically reshapes their biological identity, influencing immune system interactions, biodistribution, and cellular uptake [73]. Standard in vitro dissolution models overlook this critical phenomenon [73].
FAQ 2: How does endosomal escape, a desired function of LNPs, cause unintended inflammation? Endosomal escape is a double-edged sword. To release mRNA into the cytoplasm, the ionizable lipid in LNPs must disrupt the endosomal membrane. This process creates holes in the endosome [2]. The size of these holes determines the inflammatory response:
- Large, irreparable holes expose glycans to the cytosol, which are detected by sensors called galectins. This recognition triggers a potent inflammatory cascade, leading to the secretion of pro-inflammatory cytokines like IL-6 and TNF-α [2].
- Smaller holes can be repaired by the cellular ESCRT (Endosomal Sorting Complexes Required for Transport) machinery. LNPs designed to create these smaller, reparable holes can achieve high mRNA expression while minimizing inflammation [2].
FAQ 3: What are the major intracellular barriers that limit LNP delivery efficiency? Even after cellular uptake, multiple barriers prevent RNA from reaching the cytosol. Live-cell microscopy has revealed several key inefficiencies [1]:
- Not all internalized LNPs trigger endosomal damage conducive to escape.
- There is significant segregation between the ionizable lipid and the RNA payload during endosomal sorting.
- Surprisingly, many damaged endosomes marked by galectin recruitment contain no detectable RNA cargo.
- Even in damaged endosomes that do contain RNA, only a small fraction of the total cargo is released into the cytosol.
FAQ 4: How can I better predict the in vivo safety and efficacy of my LNP formulations during in vitro screening? To improve predictive power, move beyond simplistic transfection efficiency assays. Integrate more biologically relevant readouts into your screening pipeline:
- Monitor Endosomal Damage: Use galectin recruitment (e.g., galectin-9) as a marker for harmful, inflammatory endosomal rupture [2] [1].
- Use Physiologically Relevant Conditions: Perform in vitro transfections in complete media with serum, not serum-starved conditions, to better mimic the in vivo environment and improve IVIVC [72].
- Analyze the Protein Corona: Characterize the layer of proteins adsorbed onto LNPs after exposure to plasma, as this "biological identity" dictates subsequent interactions in the body [73].
Quantitative Data: Correlating LNP Properties with Biological Outcomes
The tables below summarize experimental data that highlight the complex relationship between LNP composition, experimental conditions, and biological outcomes.
Table 1: Impact of Ionizable Lipid and Transfection Protocol on Efficacy
| Factor | Experimental Observation | Quantitative Result | Implication for IVIVC |
|---|---|---|---|
| Ionizable Lipid (in vivo) | Protein expression in mice after i.m. injection of different LNPs [74] | ALC-0315 & SM-102 > MC3 & C12-200 (Significantly higher) | In vitro performance does not predict in vivo ranking. |
| Ionizable Lipid (in vitro) | Protein expression in HEK293, HeLa, THP-1 cells [74] | SM-102 > ALC-0315, MC3, C12-200 | |
| Transfection Protocol | Transfection efficiency in multiple cell lines (HEK293, Huh-7, etc.) [72] | Complete media showed 4- to 26-fold higher efficiency vs. serum-starved method | Standard serum-starvation creates a false negative in vitro environment. |
Table 2: Quantifying LNP-Induced Inflammation and Cargo Release
| Parameter | Measurement | Biological Significance | |
|---|---|---|---|
| Inflammation (in vivo) | Dose-dependent increase in BAL protein & leukocytes in mice after LNP instillation [2] | LNPs can induce severe inflammation, comparable to disease models. | |
| Cargo Release Efficiency | Percentage of galectin-9-positive damaged endosomes containing detectable RNA cargo [1] | siRNA-LNPs: ~70%mRNA-LNPs: ~20% | A large fraction of LNP-induced endosomal damage does not lead to cargo release, highlighting a major inefficiency. |
| mRNA Loading Capacity | Weight percentage of mRNA in standard vs. novel LNP systems [75] | Standard LNP: <5%L@Mn-mRNA: ~96% | Higher loading capacity can reduce the required lipid dose, potentially mitigating toxicity. |
Experimental Protocols for Assessing Endosomal Damage and Improving IVIVC
This protocol is designed to replace the standard serum-starved method, providing a more reliable in vitro model for screening LNP formulations.
Key Steps:
- Cell Culture Preparation: Seed relevant cell lines (e.g., HEK293, HeLa, RAW 264.7) in standard complete growth media supplemented with 10% FBS. Do not serum-starve the cells before or during transfection.
- LNP Treatment: Dilute the mRNA-LNPs directly in complete media. Add this mixture to the cells.
- Incubation and Analysis: Incubate cells under standard conditions (37°C, 5% CO₂) for 24-48 hours. Quantify mRNA expression level via flow cytometry (for e.g., EGFP mRNA) or a microplate reader (for e.g., luciferase activity).
Troubleshooting: If transfection efficiency remains low, verify that the LNP formulation process maintains an appropriate N/P ratio (typically around 6 for commercial formulations) and that particle size/PDI are within the acceptable range.
This protocol allows for the qualitative and quantitative assessment of LNP-induced endosomal damage, a key predictor of inflammatory potential.
Key Steps:
- Cell Preparation and Transfection: Seed appropriate cells (e.g., macrophage cell lines, primary cells) on imaging-grade dishes. Transfert with LNPs using the complete media protocol.
- Live-Cell Staining: Transfert cells with a fluorescently tagged galectin construct (e.g., Galectin-9-GFP) or use immunostaining post-fixation.
- Image Acquisition and Analysis: Use live-cell or super-resolution microscopy to visualize the recruitment of galectin to endosomal membranes.
- Quantification: Count the number of galectin-positive foci per cell and correlate these with the presence of fluorescently labeled LNPs or RNA cargo within the same vesicle.
Troubleshooting: The magnitude of galectin recruitment can vary. Faint signals may indicate smaller, reparable membrane perturbations, while strong, distinct signals indicate larger, irreparable ruptures.
Visualizing Key Pathways and Workflows
LNP Endosomal Damage and Immune Signaling
LNP Endosomal Damage and Immune Signaling
Enhanced In Vitro Transfection Workflow
Enhanced In Vitro Transfection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating LNP IVIVC and Endosomal Damage
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Ionizable Lipids (e.g., SM-102, ALC-0315, MC3, novel lipids) [74] [76] | Core functional component of LNPs for encapsulating nucleic acids and facilitating endosomal escape. | The chemical structure (e.g., tail length) directly influences efficacy, targeting, and inflammatory potential [2] [76]. |
| Galectin Fluorescent Tags (e.g., Galectin-9-GFP) [2] [1] | A sensitive biosensor for detecting endosomal membrane damage in live or fixed cells. | Prefer galectin-9 for its high sensitivity in detecting LNP-induced damage. Strong signal indicates inflammatory ruptures. |
| Complete Cell Culture Media (with 10% FBS) [72] | Provides a physiologically relevant environment for in vitro transfection, improving correlation with in vivo outcomes. | Critical: Avoid serum-starvation. Using complete media can increase transfection efficiency by 4- to 26-fold. |
| Helper Lipids (DSPC, Cholesterol, DMG-PEG2000) [74] [72] | Structural components that stabilize the LNP, regulate fluidity, and prevent aggregation. | Ratios can be optimized (e.g., 45:15:38.5:1.5) to enhance stability and delivery efficiency for specific ionizable lipids [76]. |
| Fluorescently Labeled RNA (e.g., Cy5-mRNA, AF647-siRNA) [1] | Enables tracking of LNP cargo uptake, intracellular trafficking, and endosomal release via microscopy. | Be aware of fluorophore quenching effects, which differ between siRNA and mRNA, affecting signal interpretation [1]. |
Lipid Nanoparticles (LNPs) are the cornerstone of modern mRNA-based therapeutics, but their efficacy is fundamentally constrained by a single, critical biological bottleneck: endosomal escape. Even after successful cellular uptake, the majority of LNP cargo is degraded within endosomes, with estimates suggesting that only 1-2% of nucleic acids successfully escape into the cytoplasm to exert their therapeutic effect [38]. This challenge is compounded by the fact that the endosomal escape process itself can trigger unwanted inflammatory responses if it causes excessive endosomal membrane damage [40].
This technical support article provides a head-to-head comparative analysis of a novel class of lipids—Branched Endosomal Disruptor (BEND) lipids—against established commercial LNP standards. Framed within the broader thesis of preventing endosomal damage, this resource equips researchers with the data, protocols, and troubleshooting knowledge to evaluate these next-generation delivery systems for their own experimental workflows.
Technology Deep Dive: BEND Lipids vs. Commercial Standards
What Are BEND Lipids?
BEND lipids are a novel class of ionizable lipids (ILs) engineered with a specific structural motif: terminally branched lipid tails [33] [31]. This architecture is designed to enhance the lipid's ability to disrupt the endosomal membrane, facilitating the release of therapeutic cargo like mRNA and CRISPR-Cas9 ribonucleoprotein (RNP) complexes into the cytosol [34]. The synthetic platform for BEND lipids is modular, allowing for the generation of lipids with various tail lengths and branching groups (e.g., isopropyl, tert-butyl, sec-butyl) to systematically explore structure-function relationships [33].
Established Commercial LNP Standards
The current commercial landscape is dominated by LNPs utilizing ionizable lipids like ALC-031 (Pfizer-BioNTech's Comirnaty) and SM-102 (Moderna's Spikevax) [33]. Furthermore, lipids such as Acuitas's ALC-315 continue to be benchmark standards for newer applications, including cancer vaccines [77]. These linear or less-branched lipids have proven clinical efficacy but may operate at the limits of their endosomal escape efficiency.
Direct Performance Comparison: Quantitative Data
The following tables summarize key quantitative findings from recent head-to-head studies comparing BEND lipids to commercial and other pre-clinical standards.
Table 1: In Vitro and In Vivo Performance Metrics
| Performance Metric | BEND Lipids | Commercial/Linear Standards | Experimental Context |
|---|---|---|---|
| mRNA Transfection Efficiency | Up to 10-fold increase in luminescence vs. commercial standards [31] | Baseline activity | Firefly luciferase (FLuc) mRNA delivery in vitro [33] |
| Hepatic Gene Editing Efficiency | Significantly enhanced | Lower efficiency | CRISPR-Cas9 RNP delivery in vivo [33] |
| T Cell Transfection | Enhanced efficiency [33] | Lower efficiency | Primary human T cell engineering [33] |
| Inflammatory Profile | Data not reported in search results | Can trigger severe inflammation via galectin sensing of endosomal damage [40] | Related to endosomal damage |
Table 2: Formulation and Physicochemical Properties
| Property | BEND Lipids | Commercial/Linear Standards | Notes |
|---|---|---|---|
| Encapsulation Efficiency | >80% [33] | >80% (Modern standards can achieve >90% [78]) | All LNP types generally show high encapsulation with modern techniques. |
| Average Particle Size | 70 - 160 nm [33] | Similar range (e.g., 70-160 nm) | Size is formulation-dependent, not a key differentiator. |
| pKa | ~6.0 [33] | ~6.0-6.5 (optimized standards) | pKa is tuned for all effective LNPs for endosomal disruption. |
Key Takeaway: The primary advantage of BEND lipids is not in the physical formulation of the LNP, but in the significantly enhanced biological activity conferred by the branched-tail architecture, which leads to superior endosomal escape and subsequent therapeutic output.
Experimental Protocols for Performance Evaluation
To replicate these comparative studies, follow the methodologies below.
Protocol: Formulating LNPs for Head-to-Head Comparison
Method: Microfluidic Mixing [33] Goal: Produce consistent, well-characterized LNP formulations for testing.
- Lipid Stock Preparation: Prepare ethanol solutions of your ionizable lipid (BEND or standard), helper lipid (DOPE), cholesterol, and PEG-lipid (C14-PEG2000).
- Aqueous Phase Preparation: Dilute mRNA or complex RNP in an acidic aqueous buffer (e.g., 10 mM citrate, pH 4.0).
- Mixing: Use a herringbone microfluidic device. Set the flow rate ratio (aqueous to ethanol) to 3:1. Keep total flow rate constant (e.g., 12 mL/min).
- Dialyzing: Immediately after mixing, dialyze the resulting LNP suspension against a large volume of PBS (pH 7.4) for at least 4 hours at 4°C to remove ethanol and raise the pH.
- Characterization: Measure particle size, PDI, ζ-potential (should be neutral/slightly negative), and encapsulation efficiency for all formulated LNPs before proceeding to biological assays.
Protocol: In Vitro mRNA Transfection Efficiency
Method: Luciferase Expression Assay [33] Goal: Quantify functional mRNA delivery.
- Cell Seeding: Seed HeLa cells or other relevant cell lines (e.g., HEK293) in a 96-well plate at 20,000 cells/well and culture overnight.
- Dosing: Apply LNP formulations (BEND vs. standards) containing encapsulated firefly luciferase (FLuc) mRNA. A typical dose is 20-100 ng mRNA per well.
- Incubation: Incubate cells with LNPs for 24 hours in standard culture conditions.
- Lysis and Measurement: Lyse cells using a passive lysis buffer. Add luciferase substrate to the lysate and measure luminescence immediately using a plate reader.
- Analysis: Normalize luminescence readings to total protein content (e.g., via BCA assay). Compare relative light units (RLUs) between BEND and standard LNP groups.
Protocol: In Vivo Gene Editing Efficiency
Method: CRISPR-Cas9 RNP Delivery in Mice [33] Goal: Assess the ability of LNPs to deliver gene-editing machinery functionally.
- LNP Formulation: Formulate LNPs encapsulating CRISPR-Cas9 ribonucleoprotein (RNP) complexes targeting a hepatic gene (e.g., Ttr or Pcsk9).
- Animal Dosing: Administer LNPs to mice intravenously via the tail vein. A standard dose is 0.5-1 mg/kg mRNA or 1-2 mg/kg RNP.
- Tissue Collection: After 3-7 days, euthanize the animals and harvest the liver.
- Editing Analysis: Extract genomic DNA from liver tissue. Quantify gene editing efficiency using next-generation sequencing (NGS) or T7 Endonuclease I (T7E1) mismatch cleavage assay on the PCR-amplified target region.
Mechanisms and Pathways: BEND Lipids and Endosomal Damage
Understanding the mechanism is key to troubleshooting and rational design. The following diagram illustrates the pathways of endosomal escape and damage sensing, highlighting where BEND lipids are proposed to act.
Diagram: BEND Lipids and Endosomal Damage Pathways. BEND lipids are hypothesized to create pores that facilitate cargo escape. Excessive damage triggers galectin-mediated inflammation, while smaller holes may be repaired by ESCRT machinery. Next-generation ionizable lipids are being designed to exploit the latter, safer pathway [40].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for LNP Formulation and Testing
| Reagent / Material | Function / Explanation | Example / Note |
|---|---|---|
| Ionizable Lipids | The key functional component; changes charge at endosomal pH to enable membrane disruption and escape. | BEND lipids (experimental) [33]; ALC-031, SM-102 (commercial standards). |
| Helper Lipid | Supports the LNP bilayer structure and can promote non-bilayer phases that facilitate fusion/escape. | DOPE (18:1 Δ9-cis phosphoethanolamine) is commonly used [33]. |
| Cholesterol | Stabilizes the LNP structure and enhances cellular uptake by incorporating into lipid bilayers. | Pharmaceutical grade; typically constitutes ~40% of lipid molar ratio [33]. |
| PEGylated Lipid | Shields the LNP surface, reduces aggregation, controls particle size, and modulates pharmacokinetics. | C14-PEG2000 (DMG-PEG2000 is a common variant) [33]. |
| Microfluidic Device | Enables reproducible, scalable formulation of LNPs with narrow size distribution. | Herringbone or staggered herringbone mixer [33]. |
| Firefly Luciferase (FLuc) mRNA | A standard reporter mRNA for quantitatively measuring transfection efficiency in vitro and in vivo. | Encapsulated in LNPs; expression is measured via luminescence [33]. |
| CRISPR-Cas9 RNP | A pre-assembled complex of Cas9 protein and guide RNA for evaluating gene-editing delivery. | Used for assessing delivery of large, functional cargo [33]. |
Troubleshooting Guide & FAQs
Q1: Our BEND lipid formulations show high encapsulation but poor functional output in vitro. What could be wrong?
- A: This points to a failure in endosomal escape or post-escape processes.
- Check the pKa: Ensure the pKa of your BEND LNP is optimally tuned (around 6.0-6.5) for protonation in the endosomal compartment. An incorrect pKa will hinder the "proton sponge" effect and membrane disruption.
- Validate Branching: Confirm the successful synthesis and incorporation of the terminally branched lipids. Analytical techniques like NMR or MS are crucial.
- Try Different Excipient Ratios: While a standard ratio is 35:16:46.5:2.5 (IL:DOPE:Chol:PEG-lipid), fine-tuning this, especially the helper lipid (DOPE) percentage, can significantly impact endosomal escape.
Q2: We observe high inflammatory responses with our LNP formulations in mouse models. How can this be mitigated?
- A: Inflammation is a known issue linked to endosomal damage [40].
- Investigate the Lipid Structure: As the diagram shows, excessive endosomal damage triggers galectin sensors. Your BEND lipid variant might be creating overly large, irreparable holes. Consider testing BEND lipids with different branching groups or tail lengths that might create smaller, ESCRT-repairable pores.
- Explore Next-Gen Lipids: Refer to the latest literature on ionizable lipids specifically designed to recruit the ESCRT machinery for membrane repair, which has been shown to reduce inflammation [40].
- Pre-medication: As a translational strategy, note that studies in non-human primates have shown premedication with steroids and antihistamines can improve tolerability, though it may reduce expression levels [77].
Q3: How can we achieve targeted delivery beyond the liver with these systems?
- A: Hepatic tropism is a default for many LNPs, but extrahepatic delivery is an active area of innovation.
- Incorporate SORT Molecules: The SORT (Selective Organ Targeting) technology is a proven method. Adding a supplemental cationic or anionic lipid to the standard four-component LNP can redirect particles to lungs, spleen, or other tissues.
- Surface Functionalization: Conjugate targeting ligands (e.g., DARPins, antibodies, peptides) to the LNP surface. Acuitas, for example, has shown success using DARPin-conjugated LNPs for targeted delivery to T-lymphocytes [77].
- Mucous Penetration: For airway targets like in cystic fibrosis, look into LNPs engineered with mucous-penetrant properties [77].
In lipid nanoparticle (LNP) research, a significant challenge is the inflammatory response triggered by endosomal membrane damage during the essential process of endosomal escape. Galectins, a family of β-galactoside-binding cytosolic proteins, have been identified as key sensors of this endosomal damage [40] [2]. When LNPs disrupt endosomal membranes, intracellular glycans become exposed to the cytosol. Galectins recognize this exposure and initiate potent inflammatory signaling pathways [2]. This inflammatory response presents a major obstacle for therapeutic LNP applications, particularly in patients with pre-existing inflammatory conditions [2].
Targeting galectins, especially galectin-3, offers a promising complementary pharmacological strategy to mitigate LNP-induced inflammation without compromising RNA delivery efficiency. Research demonstrates that galectin inhibition abrogates LNP-associated inflammation both in vitro and in vivo, providing a pathway to safer RNA therapeutics [40] [2]. This technical resource center provides troubleshooting guidance and methodological support for researchers implementing galectin inhibition strategies in their LNP studies.
Key Concepts: Mechanisms and Troubleshooting
Frequently Asked Questions
Q1: What is the fundamental connection between LNPs, endosomal damage, and galectins? LNPs achieve RNA delivery through endosomal escape, which involves creating pores in endosomal membranes. This process inevitably causes endosomal membrane damage [2]. Cytosolic galectin proteins sense this damage by binding to exposed glycans on the damaged endosomal membranes, subsequently activating downstream inflammatory pathways [40] [2]. The size of the membrane damage matters: large, irreparable holes trigger robust galectin-mediated inflammation, while smaller holes can be repaired by cellular machinery like the ESCRT pathway [2].
Q2: Why should I consider galectin inhibition for my LNP experiments? Galectin inhibition addresses the inflammatory side effects of LNP-mediated delivery without reducing therapeutic efficacy. Studies show that inhibiting galectins, particularly galectin-3, significantly reduces pro-inflammatory cytokine production (e.g., IL-6, TNF-α) and immune cell infiltration associated with LNP administration [79] [2]. This approach is especially valuable for applications where pre-existing inflammation is a concern, or where repeated LNP dosing is required.
Q3: Which galectin inhibitors are most validated for experimental use? Several inhibitors show strong experimental support:
- TD139: A small-molecule galectin-3 inhibitor demonstrated to reduce microglia reactivity and delay retinal damage in light-induced degeneration models [79].
- GB1107: Shown to reduce tumor growth in human lung adenocarcinoma models and synergize with immune checkpoint inhibition [80].
- K2 and L2: Novel non-carbohydrate small molecules that potently inhibit galectin-3-mediated cancer cell activities in vitro and in vivo [81].
Troubleshooting Common Experimental Challenges
Problem: Incomplete suppression of LNP-induced inflammation despite galectin inhibition. Solution: Consider that your LNPs might be creating heterogeneous endosomal damage. Only large, irreparable holes are sensed by galectins [2]. Complement pharmacological inhibition with LNP engineering: explore ESCRT-recruiting ionizable lipids that create smaller, reparable holes to minimize galectin activation [2].
Problem: Off-target effects or toxicity concerns with galectin inhibitors. Solution:
- For carbohydrate-based inhibitors: Monitor for carbohydrate-mediated off-target interactions [80].
- Consider novel non-carbohydrate inhibitors like K2 and L2, which bind specifically to the galectin-3 CRD domain and show no detectable cytotoxicity in preclinical models [81].
- Implement appropriate controls, including galectin knockout cells (via CRISPR/Cas9) to verify inhibitor specificity [81].
Problem: Variable efficiency in different cell types. Solution: Assess the baseline galectin expression in your target cells via Western blot or qPCR. Efficiency correlates with expression levels [79] [81]. Primary macrophages and microglia show particularly strong galectin-3 upregulation in response to inflammatory stimuli [79].
Problem: Difficulty distinguishing endosomal escape efficacy from inflammatory response. Solution: Implement dual readout systems:
- For escape efficiency: Use functional cargo delivery assays (e.g., luciferase mRNA expression, siRNA knockdown efficiency) [1].
- For inflammation: Monitor galectin recruitment via live-cell imaging of galectin-9-GFP and quantify cytokine secretion (IL-6, TNF-α) via ELISA [2] [1].
Experimental Protocols & Methodologies
Protocol: Evaluating Galectin Inhibition in Conjunction with LNP Delivery
Objective: Assess the efficacy of galectin inhibitors in reducing LNP-induced inflammation while maintaining RNA delivery efficiency.
Materials:
- Galectin inhibitor (e.g., TD139, GB1211, K2/L2) [79] [80] [81]
- LNP formulation (with and without RNA cargo)
- Target cells (e.g., RAW 264.7 macrophages, primary microglia)
- ELISA kits for IL-6, TNF-α, IL-1β [81]
- Galectin-9-GFP plasmid for damage sensing [1]
- qRT-PCR reagents for galectin-3 expression analysis [79]
Procedure:
- Pre-treatment: Expose cells to galectin inhibitor (e.g., 15 mg/kg TD139 or equivalent in vitro concentration) 2-4 hours prior to LNP administration [79].
- LNP Exposure: Add LNPs at therapeutically relevant doses (e.g., 400 ng/mL for in vitro studies) [2].
- Inflammation Assessment: (24 hours post-treatment)
- Delivery Efficiency Quantification: (Timepoint dependent on cargo)
- Galectin Recruitment Imaging: Live-cell imaging of galectin-9-GFP recruitment to endosomes post-LNP treatment [1].
Expected Outcomes: Effective galectin inhibitors should significantly reduce cytokine secretion (typically by 40-70%) and galectin-9 puncta formation while maintaining >80% of the functional cargo delivery compared to inhibitor-free controls [2] [1].
Protocol: Validating Galectin-3 Inhibition Using Binding Assays
Objective: Confirm direct binding and functional inhibition of galectin-3 by novel compounds.
Materials:
- Recombinant human galectin-3 protein [81]
- Potential inhibitor compounds (e.g., K2, L2) [81]
- Asialofetuin (ASF) as a galectin-3 ligand [81]
- Anti-galectin-3 antibody and peroxidase-conjugated secondary antibody [81]
- Intrinsic Tryptophan Fluorescence Spectroscopy equipment [81]
Procedure:
- Ligand Binding Assay:
- Coat 96-well plates with 20 μg/mL ASF overnight [81].
- Block plates with 1% BSA in PBS for 1 hour.
- Incubate with 5 μg/mL galectin-3 mixed with varying concentrations of inhibitor compounds.
- Detect bound galectin-3 using anti-galectin-3 antibody and peroxidase-conjugated secondary antibody.
- Calculate inhibition percentage compared to no-inhibitor controls.
- Binding Affinity Measurement:
- Use Intrinsic Tryptophan Fluorescence Spectroscopy with galectin-3 (10 μM) and titrate inhibitors (0-224 μM) [81].
- Determine dissociation constants (Kd) from fluorescence quenching data.
- Molecular Docking Analysis:
- Perform docking studies using programmes like Autodock Vina or DynamicBind with galectin-3 crystal structure (PDB: 3T1L) [81].
- Identify potential binding interactions using Protein-Ligand Interaction Profiler (PLIP).
Interpretation: Effective inhibitors should show dose-dependent reduction in galectin-3 binding to ASF with IC50 values in the micromolar range. Confirmed binding to the canonical S-face of galectin-3 carbohydrate-recognition domain indicates specific inhibition [81].
Research Reagent Solutions
Table: Essential Reagents for Galectin Inhibition Research
| Reagent/Category | Specific Examples | Key Function & Application | Experimental Notes |
|---|---|---|---|
| Small Molecule Inhibitors | TD139 [79]GB1107 [80]K2/L2 [81] | Pharmacological inhibition of galectin-3; reduce inflammation in LNP studies | TD139: used at 15 mg/kg in vivo [79]; K2/L2: non-carbohydrate, show no cytotoxicity [81] |
| Genetic Tools | Galectin-3 KO mice [79]CRISPR/Cas9 galectin-3 knockout plasmids [81]shRNA vectors [80] | Genetic validation of galectin roles; create galectin-deficient cell lines | KO mice show reduced microglia reactivity and delayed retinal degeneration [79] |
| Detection Reagents | Anti-galectin-3 antibodies [79]Galectin-9-GFP constructs [1]Cytokine ELISA kits [81] | Detect galectin expression/recruitment; quantify inflammatory response | Galectin-9-GFP is highly sensitive for detecting endosomal damage [1] |
| LNP Components | ESCRT-recruiting ionizable lipids [2]cKK-E12 [2] | Engineer less inflammatory LNPs; create controlled endosomal damage | ESCRT-recruiting lipids create smaller, reparable holes minimizing galectin response [2] |
| Binding Assay Components | Recombinant galectin-3 [81]Asialofetuin (ASF) [81] | Validate direct inhibitor binding; measure inhibition potency | ELISA-style binding assay establishes dose-response relationships [81] |
Signaling Pathways and Workflows
LNP-Induced Inflammation and Galectin Inhibition Pathway
This diagram illustrates the dual strategic approach to mitigating LNP-induced inflammation: (1) pharmacological inhibition of galectin sensing and signaling (blue elements), and (2) engineering LNPs that create smaller, reparable membrane holes that recruit ESCRT machinery instead of galectins (green pathway) [40] [2].
Experimental Workflow for Testing Galectin Inhibitors
This workflow outlines the key steps for evaluating galectin inhibitors in LNP studies, emphasizing parallel assessment of both functional delivery (green) and inflammatory response (red) to ensure reduced inflammation doesn't come at the cost of delivery efficiency [79] [1] [81].
Table: Experimental Data from Key Galectin Inhibition Studies
| Study Context | Inhibitor Used | Key Efficacy Metrics | Outcome & Significance |
|---|---|---|---|
| Light-induced retinal degeneration [79] | TD139 (15 mg/kg) | - Reduced microglia reactivity- Delayed retinal damage- Decreased pro-inflammatory cytokines | Significant protection against photoreceptor degeneration; highlights galectin-3 as drug target for immunomodulatory therapies. |
| LNP-induced inflammation [2] | Galectin inhibition (genetic & pharmacological) | - >3-fold reduction in BAL protein- >1.8-fold reduction in BAL leukocytes- Reduced IL-6, TNF-α | Abrogated LNP-associated inflammation in vitro and in vivo across multiple delivery routes. |
| Cancer cell invasion & angiogenesis [81] | K2 and L2 (novel non-carbohydrate inhibitors) | - Inhibition of cancer cell adhesion & invasion- Reduced tumor growth & metastasis in vivo- No detectable cytotoxicity | Potent inhibition of galectin-3-mediated activities; promising for cancer and inflammation therapy. |
| Tumor growth & immune synergy [80] | GB1107 | - Reduced tumor growth in lung adenocarcinoma- Synergy with anti-PD-1 therapy- Enhanced T-cell infiltration | Improved response to immunotherapy; demonstrates value of combination therapies. |
| Endosomal damage sensing [1] | N/A (Imaging study) | - Only 67-74% of galectin-9+ vesicles contained siRNA- Only ~20% contained mRNA cargo | Revealed segregation of LNP components during endosomal sorting; key barrier to delivery efficiency. |
Galectin inhibition represents a powerful complementary strategy to address the inflammatory consequences of LNP-mediated endosomal damage. The experimental frameworks, troubleshooting guides, and methodological details provided here offer researchers a comprehensive toolkit for implementing these approaches. As the field advances, the combination of smarter LNP design principles with targeted pharmacological interventions like galectin inhibition will be crucial for developing safer, more effective RNA therapeutics capable of treating even inflammatory disease conditions.
Therapeutic Validation in Inflammatory Disease Models
Core Concepts and Troubleshooting FAQs
FAQ: Why do my Lipid Nanoparticles (LNPs) cause excessive inflammation in preclinical disease models?
Answer: LNP-induced inflammation is frequently caused by endosomal membrane damage during the "endosomal escape" phase of delivery. When the ionizable lipid in LNPs becomes protonated in the acidic endosome, it can create large, irreparable holes in the endosomal membrane [2]. The cell recognizes this damage via cytosolic proteins called galectins (particularly galectin-9), which in turn triggers a potent pro-inflammatory response, including the secretion of cytokines like IL-6, IL-1α, and TNF-α [2] [1]. This inflammation can exacerbate pre-existing disease conditions and confound therapeutic validation.
Troubleshooting Guide:
- Verify Ionizable Lipid Selection: Use ionizable lipids from the class that creates smaller, reparable endosomal holes. These lipids recruit the ESCRT machinery for membrane repair, significantly reducing inflammation [2].
- Monitor Membrane Damage Markers: Implement assays to detect galectin recruitment. High levels of galectin-positive endosomal damage indicate a pro-inflammatory formulation [1].
- Check Cargo-Independent Effects: Test empty LNPs (without RNA cargo). If inflammation persists, the lipid formulation itself is the likely culprit, not the nucleic acid payload [2].
FAQ: The in vitro performance of my LNPs does not predict their in vivo efficacy. What are the key barriers causing this discrepancy?
Answer: Poor correlation between in vitro and in vivo results stems from multiple intracellular barriers that are difficult to model in simple cell cultures. Key inefficiencies include [1]:
- Inefficient Endosomal Escape: Only a fraction of internalized LNPs successfully cause endosomal membrane damage conducive to cargo release.
- Payload Segregation: The RNA payload and ionizable lipid can segregate within the endosomal system, meaning a damaged endosome may not contain the therapeutic cargo.
- Low Hit Rate: Especially for mRNA-LNPs, a majority of damaged endosomes (marked by galectin-9) contain no detectable mRNA, severely limiting delivery efficiency.
Troubleshooting Guide:
- Employ Advanced Imaging: Use live-cell and super-resolution microscopy to track both the LNP lipid component and the RNA cargo simultaneously. This helps visualize payload segregation and identify the exact point of failure [1].
- Quantify Functional Delivery: Move beyond simple cellular uptake metrics. Use functional readouts like protein expression assays to confirm the biological activity of the delivered nucleic acid [45].
- Select Lipids for ESCRT Recruitment: Prioritize ionizable lipids that trigger the ESCRT-mediated repair pathway. These formulations cause less membrane damage and can improve the correlation between cellular damage and successful delivery [2].
FAQ: How can I accurately measure the impact of my LNP-based therapy on disease activity in an Inflammatory Bowel Disease (IBD) model?
Answer: Accurately quantifying disease activity in complex models like IBD requires a combination of computational modeling and machine learning. Relying solely on subjective clinical scores can be misleading.
Troubleshooting Guide:
- Use Simulated Biomarkers: Leverage Quantitative Systems Pharmacology (QSP) models to generate comprehensive, simulated data on gut-level inflammatory markers (e.g., immune cell and cytokine dynamics) that are difficult to measure repeatedly in vivo [82].
- Train a Predictive Model: Use the simulated biomarker data from the QSP model to train a machine learning algorithm. This algorithm can then predict standardized clinical scores (e.g., Mayo Score for UC or CDAI for CD) based on objective, mechanistic data, providing a more reliable assessment of therapeutic efficacy [82].
- Correlate with Objective Biomarkers: While biomarkers like fecal calprotectin (FCP) are useful, they do not always correlate perfectly with disease activity. A combined QSP-ML approach provides a more holistic view [82].
Experimental Protocols for Validation
Protocol: Evaluating Endosomal Damage and Escape
This protocol uses live-cell imaging to assess the early cellular response to LNPs, which is critical for understanding their inflammatory potential and delivery efficiency.
Methodology:
- Cell Preparation: Seed appropriate cell lines (e.g., RAW 264.7 macrophages or primary macrophages) in imaging-compatible dishes.
- Transfection: Treat cells with LNPs containing fluorescently labeled RNA (e.g., Cy5-mRNA). A therapeutically relevant dose of 400 ng/mL for 6 hours is a common starting point [2].
- Staining: Transfert cells with a plasmid expressing a fluorescently tagged galectin-9 protein (e.g., Galectin-9-GFP) to act as a sensitive sensor for endosomal membrane damage [1].
- Image Acquisition: Use fast live-cell microscopy to capture images every 5-10 seconds for at least 1 hour post-transfection. Track the co-localization of the RNA signal (Cy5) and the galectin-9 signal (GFP).
- Quantitative Analysis:
- Calculate the percentage of galectin-9-positive endosomes that also contain the fluorescent RNA signal (the "hit rate") [1].
- A low hit rate for your mRNA-LNP formulation (e.g., around 20%) indicates significant payload segregation and inefficient escape, pointing to a key area for formulation improvement.
Protocol: Quantifying Inflammatory Response to LNPs In Vivo
This protocol measures the innate immune response to LNP administration, a critical safety and efficacy checkpoint.
Methodology:
- Animal Dosing: Administer LNPs to animal models (e.g., mice) via your intended route (e.g., intratracheal instillation for lung-focused studies). Use a range of therapeutically relevant mRNA doses (e.g., 2.5 μg to 10 μg per mouse) [2].
- Sample Collection: At a predetermined endpoint (e.g., 24 hours post-administration), collect relevant biofluids. For respiratory models, collect Bronchoalveolar Lavage (BAL) fluid. Also, collect plasma for systemic analysis.
- Analysis:
- BAL Fluid: Quantify total protein concentration (indicator of capillary leak) and leukocyte count (indicator of immune cell infiltration) [2].
- Cytokine Profiling: Use ELISA or multiplex assays on BAL fluid and plasma to measure key pro-inflammatory cytokines such as IL-6, TNF-α, IL-1α, and MCP-1 [2].
- Interpretation: Compare results to negative (saline) and positive (e.g., LPS) controls. Significant elevation in these parameters indicates a strong inflammatory response to the LNP formulation.
Data Presentation: LNP Formulation and Performance
The table below summarizes quantitative data on how different ionizable lipids impact LNP performance and inflammation, based on preclinical studies. This data is crucial for selecting the right lipid for your application.
Table 1: Impact of Ionizable Lipids on LNP Performance and Inflammation
| Ionizable Lipid | Key Characteristic | Inflammatory Profile | Delivery Efficiency / Performance |
|---|---|---|---|
| cKK-E12 | Well-studied, drives strong RNA expression [2] | High inflammation; induces severe lung "hepatization," dose-dependent increases in BAL protein/leukocytes, and pro-inflammatory cytokines (IL-6, TNF-α) [2] | High expression, but efficacy may be offset by toxicity in inflammatory models [2] |
| ESCRT-Recruiting Lipids | Creates smaller, reparable endosomal holes [2] | Low inflammation; ESCRT machinery repairs damage, minimizing galectin response and cytokine secretion [2] | High expression from cargo mRNA; suitable for treating inflammatory disease models [2] |
| SM-102 | Used in commercial vaccines [45] | Intermediate inflammation (context-dependent) | High in vitro expression; high in vivo protein expression; strong vaccine immune responses [45] |
| ALC-0315 | Used in commercial vaccines [45] | Intermediate inflammation (context-dependent) | Lower in vitro expression than SM-102; high in vivo protein expression; strong vaccine immune responses [45] |
| MC3 (DLin-MC3-DMA) | First approved for siRNA therapy (Patisiran) [1] | Can trigger galectin-9 recruitment, indicating membrane damage and inflammatory potential [1] | Lower in vivo expression compared to SM-102/ALC-0315; well-established for liver siRNA delivery [45] [1] |
The table below synthesizes key metrics for evaluating LNP-induced inflammation and delivery efficiency from experimental data.
Table 2: Key Quantitative Metrics for LNP-Induced Inflammation and Delivery
| Metric | Description | Experimental Readout | Implication for Therapeutic Validation |
|---|---|---|---|
| Galectin-9 "Hit Rate" | Percentage of galectin-9 positive damaged endosomes that actually contain RNA cargo [1] | ~70% for siRNA-LNPs; ~20% for mRNA-LNPs [1] | A low hit rate indicates major payload loss and inefficient delivery, a key barrier to efficacy. |
| BAL Protein Increase | Measure of capillary leak and tissue inflammation in the lungs [2] | >3-fold increase vs. saline control in pig lungs [2] | Indicates significant tissue-level inflammation, which could worsen pre-existing inflammatory diseases. |
| Pro-inflammatory Cytokines | Secretion of cytokines like IL-6 and TNF-α in response to LNP administration [2] | ~2.5-fold (IL-6) and ~4-fold (TNF-α) increase in BAL fluid [2] | Confirms activation of innate immune pathways; high levels are undesirable for treating inflammatory diseases. |
Signaling Pathways and Experimental Workflows
The Dual Pathway of LNP Endosomal Escape and Inflammation
This diagram illustrates the central mechanism by which LNPs cause inflammation, highlighting the two divergent outcomes based on the properties of the ionizable lipid.
Workflow for Evaluating LNP Delivery Efficiency
This workflow outlines a comprehensive experimental strategy to identify the specific barriers limiting LNP delivery in a target cell or tissue.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating LNP-Induced Endosomal Damage
| Reagent / Tool | Function / Application | Key Characteristic |
|---|---|---|
| Ionizable Lipids (ESCRT-Recruiting) | Core LNP component to minimize inflammation | Creates small, reparable endosomal holes, avoiding galectin sensing [2]. |
| Galectin-9 Fluorescent Tag (e.g., GFP) | Live-cell imaging sensor for endosomal membrane damage | Most sensitive sensor for LNP-induced damage; marks vesicles with large, irreparable holes [2] [1]. |
| Fluorescently Labeled RNA (Cy5, AF647) | Tracking RNA cargo location and release | Allows quantification of cargo segregation from lipids and "hit rate" in damaged endosomes [1]. |
| Microfluidic Formulator | Manufacturing uniform, stable LNPs with high encapsulation efficiency | Enables reproducible, scalable LNP production with precise size control (e.g., 50-200 nm) and >90% encapsulation [20]. |
| Validated PopPK Models (e.g., Ustekinumab) | Model-Informed Precision Dosing in disease models | Tools like the Xu et al. or Adedokun et al. models help optimize dosing regimens for biologics in complex diseases like IBD [83]. |
| iPSC-Derived Human Cells (Microglia, Astrocytes) | Physiologically relevant in-vitro disease models | Provides a translational platform for evaluating LNP performance and immunogenicity in human-derived, disease-relevant cell types [84]. |
Frequently Asked Questions (FAQs)
FAQ 1: Why is endosomal escape a critical barrier for LNP-based RNA therapeutics? After cellular uptake, LNPs are trafficked through the endosomal-lysosomal system. If they do not escape from the endosome, they risk being degraded by the acidic environment and hydrolytic enzymes in lysosomes. It is estimated that only 1%-2% of siRNA encapsulated in commercially available LNPs successfully escapes the endosome to reach the cytosol; the majority are trafficked for degradation or recycling. Efficient endosomal escape is therefore essential for the therapeutic efficacy of RNA cargo, as the cytosol is its primary site of action [7].
FAQ 2: What are the key functional roles of the four main lipid components in LNPs? Modern LNP formulations are typically composed of four key lipid components, each with a distinct function [7] [85]:
- Ionizable Lipid: Critical for RNA encapsulation and facilitating endosomal escape. It is neutral at physiological pH but becomes positively charged in the acidic endosomal environment, promoting membrane disruption.
- Phospholipid (Helper Lipid): Acts as a structural component of the nanoparticle bilayer.
- Cholesterol: Enhances the stability and rigidity of the LNP structure and aids in membrane fusion.
- PEGylated Lipid: Provides a protective surface layer that improves nanoparticle stability, reduces aggregation, and increases circulation half-life by minimizing immune system recognition.
FAQ 3: What is the "PEG Dilemma"? The "PEG Dilemma" refers to the trade-off between the benefits and drawbacks of PEGylated lipids [7]. While PEGylation provides "stealth" properties that prolong circulation time, it also creates a hydrophilic barrier that can reduce interactions with cell membranes. This results in reduced cellular uptake and endosomal escape efficiency. Research is ongoing to find biodegradable alternatives, such as polyoxazolines and polysarcosines [7].
FAQ 4: How does LNP-induced endosomal damage trigger inflammation? Recent research indicates that the process of endosomal escape can cause damage to the endosomal membrane [2]. Large, irreparable holes in the membrane are sensed by cytosolic proteins called galectins, which initiate a potent inflammatory signaling cascade. This inflammation is a significant safety concern, particularly for treating patients with pre-existing inflammatory conditions [2].
FAQ 5: What is the relationship between galectins, the ESCRT machinery, and endosomal escape? The cellular response to LNP-induced membrane damage depends on the size of the membrane perturbation [2] [1]:
- Galectin-Positive Damage: Large, irreparable holes recruit galectin proteins (e.g., galectin-9) and are conducive to RNA release into the cytosol. However, they also trigger inflammation.
- ESCRT-Recruited Damage: Smaller membrane disruptions can be repaired by the Endosomal Sorting Complexes Required for Transport (ESCRT) machinery. LNPs engineered to create these smaller holes can achieve effective RNA expression while minimizing inflammatory responses, offering a path to safer therapeutics [2].
Troubleshooting Guides
Problem: Low Transfection or Knockdown Efficiency
Potential Causes and Solutions:
Cause 1: Suboptimal Ionizable Lipid Structure. The chemical structure of the ionizable lipid directly influences its fusogenic activity and ability to promote a phase transition in the endosomal membrane [7].
- Solution: Optimize the ionizable lipid design. Shift from cylindrical-shaped lipids to more cone-shaped structures. This can be achieved by:
Cause 2: The "PEG Dilemma" - Poor Cellular Uptake. The PEG shield is hindering interaction with target cells [7].
- Solution: Systematically optimize the molar ratio of PEG-lipid in the formulation. Consider using biodegradable PEG alternatives or cleavable PEG-lipids that shed the PEG coat upon reaching the target site.
Cause 3: Inefficient Helper Lipid. The helper lipid is not adequately supporting membrane fusion.
Problem: High Cytotoxicity or Unwanted Inflammatory Response
Potential Causes and Solutions:
Cause 1: Persistent Cationic Charge. The use of permanently cationic lipids (as opposed to ionizable ones) can disrupt cellular membranes indiscriminately, leading to cytotoxicity and activation of pro-inflammatory cytokines via TLR4 activation [7].
Cause 2: Induction of Large, Irreparable Endosomal Holes. The current LNP formulation may be causing excessive endosomal membrane damage, triggering galectin-mediated inflammation [2].
- Solution: Develop next-generation ionizable lipids that create smaller, reparable membrane holes. These "ESCRT-recruiting" lipids allow for effective RNA release while enabling the cell's ESCRT machinery to repair the damage, thereby avoiding galectin sensing and subsequent inflammation [2].
Problem: Inconsistent Results Between Batches or Cell Lines
Potential Causes and Solutions:
Cause 1: Inconsistent LNP Formulation or Buffer Conditions. The buffer used during LNP formulation and dilution can significantly impact the assembly, stability, and transfection efficiency of mRNA-LNPs [86].
- Solution: Standardize buffer conditions. Research indicates that sodium potassium magnesium calcium and glucose solution (SPMCG) can be a favorable buffer for packaging and maintaining LNP integrity. Avoid buffers that may promote aggregation or hydrolysis [86].
Cause 2: Variable LNP Uptake and Payload Segregation. The internalization pathways and subsequent intracellular trafficking of LNPs can be highly variable. Recent super-resolution microscopy reveals that the ionizable lipid and RNA payload can segregate within the endosomal system, meaning a damaged endosome may not necessarily contain the RNA cargo [1].
- Solution: Employ advanced characterization techniques. Use live-cell microscopy with fluorescently labeled lipids and RNA to track the correlation between LNP uptake, endosomal damage (e.g., galectin-9 recruitment), and cargo release in your specific cell model. This can help identify the specific bottleneck [1].
Table 1: Key Quantitative Metrics in LNP Endosomal Escape
| Metric | Typical Value/Status | Context & Implications |
|---|---|---|
| Endosomal Escape Efficiency | ~1-2% of siRNA [7] | Major bottleneck for LNP efficacy; over 98% of payload is often degraded. |
| Ionizable Lipid Optimal pKa | ~6.0 - 6.5 [1] | Ensures protonation and positive charge acquisition specifically in the acidic early endosome. |
| Superior EE of EVs | >10-fold higher than some commercial LNPs [7] | Natural extracellular vesicles (EVs) provide a blueprint for designing more efficient synthetic LNPs. |
| ESCRT vs. Galectin Damage | ESCRT: Smaller, reparable holes.Galectin: Large, inflammatory holes. [2] | Engineering LNPs that recruit ESCRT is a promising strategy to reduce inflammation while maintaining delivery. |
| Hit Rate of RNA in Damaged Endosomes | siRNA: ~70%mRNA: ~20% [1] | A significant fraction of endosomes damaged by LNPs contain no detectable RNA payload, highlighting intracellular segregation. |
Table 2: Comparative Analysis of Key Lipid Components for Endosomal Escape
| Lipid Type | Role in Endosomal Escape | Examples | Advantages | Disadvantages/Challenges |
|---|---|---|---|---|
| Ionizable Lipids | Primary driver; protonates in endosome, disrupts membrane via phase transition. | DLin-MC3-DMA, SM-102, ALC-0315 [7] | High efficiency; reduced cytotoxicity vs. cationic lipids; tunable pKa. | Can trigger inflammatory response via membrane damage; requires complex synthesis. |
| Cationic Lipids | Permanently positive charge interacts with anionic endosomal membrane. | DOTAP, DOTMA, DDAB [86] [85] | Simple formulation; high uptake; inherent adjuvant properties. | High cytotoxicity; non-specific membrane disruption; activates immune response. |
| Fusogenic Helper Lipids | Promotes transition from lamellar to inverted hexagonal phase for membrane fusion. | DOPE [86] [85] | Significantly enhances escape efficiency; biocompatible. | May reduce stability if not properly balanced with other components. |
| PEGylated Lipids | Surface shield; impacts uptake and escape by limiting non-specific interactions. | DMG-PEG, DSPE-PEG [7] | Improves stability and circulation time ("stealth" effect). | Creates the "PEG Dilemma," reducing cellular uptake and endosomal escape. |
Key Signaling Pathways and Cellular Processes
The following diagram illustrates the two primary pathways LNPs can take after endocytosis, leading to either successful RNA delivery or degradation and inflammation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying LNP Endosomal Escape
| Reagent / Material | Function in Research | Specific Application Example |
|---|---|---|
| Ionizable Lipids | The core functional component for enabling endosomal escape. | DLin-MC3-DMA (benchmark), SM-102 (Moderna vaccine), cKK-E12 (research model). Used to study structure-activity relationships [7] [2]. |
| Fusogenic Helper Lipids | Enhances membrane fusion and escape efficiency. | DOPE is widely used to promote the lamellar-to-hexagonal (L-HII) phase transition critical for fusion [86] [85]. |
| Galectin Reporter Systems | Visualizes and quantifies endosomal membrane damage. | Expression of fluorescently tagged galectin-9 (e.g., Gal9-GFP) in live cells to identify endosomes with large, irreparable damage [2] [1]. |
| Fluorescently Labeled RNA | Allows tracking of LNP cargo intracellularly. | Using Cy5-mRNA or AlexaFluor 647-siRNA to correlate LNP localization, endosomal damage, and actual RNA release via live-cell microscopy [1]. |
| ESCRT Machinery Reporters | Monitors endosomal membrane repair processes. | Fluorescently tagged proteins like CHMP4B (an ESCRT-III component) to identify LNPs that cause smaller, reparable holes [2]. |
| Microfluidic Mixers | Enables reproducible, scalable LNP formulation. | Devices from companies like Precision Nanosystems or Dolomite used for highly controlled mixing of lipid and RNA phases, ensuring consistent LNP size and encapsulation [7]. |
Conclusion
The path toward preventing LNP-induced endosomal damage is converging on two powerful, complementary strategies: engineering smarter lipids that create smaller, reparable membrane openings, and co-opting the cell's innate repair mechanisms. The development of ESCRT-recruiting and novel branched ionizable lipids demonstrates that high therapeutic mRNA expression can be uncoupled from severe inflammatory responses. These advances, validated in sophisticated disease models, mark a significant paradigm shift. Future work must focus on translating these design principles into clinically viable formulations, expanding the reach of RNA therapeutics to treat chronic and inflammatory diseases where the safety margin is paramount. The ongoing exploration of natural delivery systems, like extracellular vesicles, continues to provide a blueprint for innovation, promising a new generation of LNPs that are not just effective delivery vehicles, but also benign cellular guests.
References
- 1. Cellular and biophysical barriers to lipid nanoparticle ... [https://www.nature.com/articles/s41467-025-60959-z]
- 2. Limiting endosomal damage sensing reduces inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12352612/]
- 3. Next-Generation mRNA-LNPs: Strategies to Reduce Anti ... [https://www.biochempeg.com/article/453.html]
- 4. The kinetics of endosomal disruption reveal differences in ... [https://pubmed.ncbi.nlm.nih.gov/40684993/]
- 5. Engineering Endosomal Escape Without Side Effects - PubMed [https://pubmed.ncbi.nlm.nih.gov/38659905/]
- 6. Galectins - Essentials of Glycobiology - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK579987/]
- 7. Endosomal escape mechanisms of extracellular vesicle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11648457/]
- 8. Nanoparticles: molecular targets and cell signalling [https://pubmed.ncbi.nlm.nih.gov/20502881/]
- 9. Inflammatory response of nanoparticles: Mechanisms ... [https://www.sciencedirect.com/science/article/abs/pii/S004565352401720X]
- 10. Recent Advances in Lipid Nanoparticles and Their Safety ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11510967/]
- 11. Lipid Nanoparticle Development for A Fluvid mRNA ... [https://www.nature.com/articles/s41541-025-01153-6]
- 12. A high-throughput Galectin-9 imaging assay for quantifying ... [https://www.nature.com/articles/s42003-021-01728-8]
- 13. Nanoscopy for endosomal escape quantification - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9419860/]
- 14. Endosomal Marker Antibodies [https://www.thermofisher.com/us/en/home/life-science/antibodies/primary-antibodies/organelle-marker-antibodies/endosomal-marker-antibodies.html]
- 15. Distribution and Co-localization of endosome markers in cells [https://www.sciencedirect.com/science/article/pii/S2405844019360359]
- 16. The kinetics of endosomal disruption reveal differences in ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925006686]
- 17. Endosomal escape: A bottleneck for LNP-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10945858/]
- 18. Advanced Strategies for Overcoming Endosomal/Lysosomal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10208951/]
- 19. Overcoming thermostability challenges in mRNA–lipid ... [https://www.nature.com/articles/s42003-024-06235-0]
- 20. A complete guide to understanding Lipid nanoparticles (LNP) [https://insidetx.com/resources/reviews/complete-guide-to-understanding-lipid-nanoparticles-lnp/]
- 21. Lipid Nanoparticles (LNPs): A complete guide for researchers [https://ozbiosciences.com/blog/lipid-nanoparticles-lnps-a-complete-guide-for-researchers-n107]
- 22. Frequently Asked Questions - Lipid Nanoparticles (LNPs) ... [https://diantpharma.com/?page_id=1308]
- 23. PotM: Ionizable Cationic Lipids for Drug Delivery [https://iris-biotech.de/global/blog/potm-ionizable-cationic-lipids-for-drug-delivery.html]
- 24. The ESCRT machinery - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3314914/]
- 25. The ESCRT pathway - The Emr Lab [https://emr.wicmb.cornell.edu/the-escrt-pathway/]
- 26. Review The ESCRT Pathway [https://www.sciencedirect.com/science/article/pii/S1534580711002073]
- 27. ESCRT [https://en.wikipedia.org/wiki/ESCRT]
- 28. Disrupting the α-synuclein-ESCRT interaction with a ... [https://www.nature.com/articles/s41467-023-37464-2]
- 29. The Escrt Complexes: Structure and Mechanism of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1648078/]
- 30. Recurrent evolution of an inhibitor of ESCRT-dependent virus ... [https://pubmed.ncbi.nlm.nih.gov/35245459/]
- 31. Escaping the Endosome: BEND Lipids Improve LNP mRNA ... [https://blog.seas.upenn.edu/escaping-the-endosome-bend-lipids-improve-lnp-mrna-delivery-and-gene-editing/]
- 32. Bend lipids improve LNP mRNA delivery and gene editing [https://www.sciencedaily.com/releases/2025/01/250128123934.htm]
- 33. Branched endosomal disruptor (BEND) lipids mediate ... [https://www.nature.com/articles/s41467-024-55137-6]
- 34. Branched endosomal disruptor (BEND) lipids mediate delivery ... [https://pubmed.ncbi.nlm.nih.gov/39856035/]
- 35. New ionizable lipids for non-viral mRNA delivery with ... [https://pubs.rsc.org/en/content/articlelanding/2025/md/d5md00115c]
- 36. Engineering of extracellular vesicles for efficient ... [https://www.nature.com/articles/s41467-025-59377-y]
- 37. Linkage between endosomal escape of LNP-mRNA and loading into EVs for transport to other cells | Nature Communications [https://www.nature.com/articles/s41467-019-12275-6]
- 38. Endo/Lysosomal-Escapable Lipid Nanoparticle Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300936/]
- 39. The Importance of Apparent pKa in the Development of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8148296/]
- 40. Limiting endosomal damage sensing reduces inflammation ... [https://www.nature.com/articles/s41565-025-01974-5]
- 41. Challenges and opportunities in computational studies for ... [https://www.nature.com/articles/s44386-025-00024-3]
- 42. Overcoming the prediction limitation of small datasets ... [https://www.sciencedirect.com/science/article/pii/S2211383525007269]
- 43. A careful look at lipid nanoparticle characterization [https://www.nature.com/articles/s41598-024-52685-1]
- 44. Navigating the challenges of lipid nanoparticle formulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10791113/]
- 45. Exploring the Challenges of Lipid Nanoparticle Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031360/]
- 46. Stealth nanoparticles in oncology: Facing the PEG dilemma [https://www.sciencedirect.com/science/article/abs/pii/S0168365922005867]
- 47. Recent advances in stealth coating of nanoparticle drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3288878/]
- 48. The Polyethyleneglycol Dilemma [https://www.jstage.jst.go.jp/article/bpb/36/6/36_b13-00059/_html/-char/en]
- 49. Limiting endosomal damage sensing reduces inflammation ... [https://pubmed.ncbi.nlm.nih.gov/40789922/]
- 50. Diversity of PEGylation methods of liposomes and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6457174/]
- 51. The benefits and risks of PEGylation in nanomedicine [https://www.nature.com/articles/s41565-025-01951-y]
- 52. Stealth Liposomes (PEGylated Liposomes) as Drug Carrier ... [https://www.biochempeg.com/article/68.html]
- 53. Endosomal escape and current obstacles in ionizable lipid ... [https://www.sciencedirect.com/science/article/pii/S0378517325011007]
- 54. Mesoscopic Structure of Lipid Nanoparticles Studied by Small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12113147/]
- 55. Simple Scattering: Lipid nanoparticle structural data ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2024.1321364/full]
- 56. RAP opportunity [https://ra.nas.edu/RAPLab10/opportunity/opportunity.aspx?LabCode=50&ROPCD=506451&RONum=C0839]
- 57. Study on molecular orientation and stratification in RNA ... [https://www.nature.com/articles/s42004-025-01526-x]
- 58. Structural Profiling of Lipid Nanoparticles at Sub-10 nm ... [https://chemrxiv.org/engage/chemrxiv/article-details/6882874f728bf9025e12d2c5]
- 59. Endosomal Escape: Key Challenge in LNP Therapeutics [https://insidetx.com/resources/reviews/endosomal-escape-a-critical-challenge-in-lnp-mediated-therapeutics/]
- 60. Lipid Nanoparticles Formulated with a Novel Cholesterol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315899/]
- 61. Rational design of lipid nanoparticles for enabling gene ... [https://www.sciencedirect.com/science/article/pii/S2329050125001135]
- 62. A high-throughput approach of screening nanoparticles for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10475836/]
- 63. High-Throughput Screening Applications for Lipid ... [https://www.precigenome.com/post/high-throughput-screening-applications-for-lipid-nanoparticle-development-and-optimization?srsltid=AfmBOorIKY5MKcRJx1ciK80QDeYbKHShnU5YIrZNbJ3b4FSVWem94qBg]
- 64. A guide to RNA-LNP formulation screening [https://insidetx.com/resources/reviews/a-guide-to-rna-lnp-formulation-screening/]
- 65. Lipid Nanoparticle-Associated Inflammation is Triggered by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11042321/]
- 66. Boosting RNA nanotherapeutics with V-ATPase activating ... [https://www.nature.com/articles/s41467-025-61688-z]
- 67. Redefining LNP composition: phospholipid and sterol-driven ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00150a]
- 68. Pro-inflammatory concerns with lipid nanoparticles - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047613/]
- 69. Synergistic effect of nucleoside modification and ionizable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479783/]
- 70. Immunogenicity of lipid nanoparticles and its impact on the ... [https://www.nature.com/articles/s12276-023-01086-x]
- 71. Added to pre-existing inflammation, mRNA-lipid ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365921006805]
- 72. Protocol for in vitro transfection of mRNA-encapsulated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597280/]
- 73. In vitro and in vivo correlation of injectable lipid-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549719/]
- 74. Exploring the Challenges of Lipid Nanoparticle Development [https://www.mdpi.com/2076-393X/13/4/339]
- 75. Engineering of mRNA vaccine platform with reduced lipids ... [https://www.nature.com/articles/s41467-025-63965-3]
- 76. Low-liver-accumulation lipid nanoparticles enhance the ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06924-2]
- 77. Acuitas Therapeutics Unveils Next-Generation Lipid ... [https://crisprmedicinenews.com/press-release-service/card/acuitas-therapeutics-unveils-next-generation-lipid-nanoparticle-advancements-at-the-2025-mrna-health/]
- 78. Lipid Nanoparticles LNP Market Outlook 2025-2032 [https://www.intelmarketresearch.com/lipid-nanoparticles-2025-2032-904-965]
- 79. Genetic targeting or pharmacological inhibition of galectin-3 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482176/]
- 80. Inhibition of galectins in cancer: Biological challenges for their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9872792/]
- 81. Targeting galectin-3 in cancer by novel and unique inhibitors ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01356-6]
- 82. Frontiers | Combining mechanistic modeling with machine learning as... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1479666/full]
- 83. External Evaluation of Population Pharmacokinetic Models of... [https://pubmed.ncbi.nlm.nih.gov/40178486/]
- 84. Concept Life Sciences | Advancing neuroinflammation and... [https://www.conceptlifesciences.com/news-and-blog/advancing-neuroinflammation-and-neurodegeneration-research-at-neuroscience-2025]
- 85. Lipid nanoparticles for mRNA delivery [https://www.nature.com/articles/s41578-021-00358-0]
- 86. Optimization of Lipid Nanoformulations for Effective mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9259059/]