Organic vs. Inorganic Nanoparticles: A Comprehensive Analysis of Toxicity Profiles for Safer Drug Development
This article provides a systematic comparison of the toxicity profiles of organic and inorganic nanoparticles, crucial for researchers and drug development professionals navigating the safety landscape of nanomedicine.
Organic vs. Inorganic Nanoparticles: A Comprehensive Analysis of Toxicity Profiles for Safer Drug Development
Abstract
This article provides a systematic comparison of the toxicity profiles of organic and inorganic nanoparticles, crucial for researchers and drug development professionals navigating the safety landscape of nanomedicine. It explores the fundamental physicochemical properties dictating nanotoxicity, details advanced in vitro and in vivo assessment methodologies, and outlines strategies for troubleshooting and optimizing nanoparticle safety. A direct comparative analysis highlights the distinct advantages and challenges associated with each nanoparticle class, synthesizing key takeaways to guide the rational design of safer, more effective nanotherapeutics and inform future regulatory frameworks.
Unraveling the Core: Physicochemical Properties and Mechanisms Driving Nanoparticle Toxicity
In the evolving landscape of nanotechnology, nanoparticles (NPs) are defined as particles with at least one dimension ranging from 1 to 100 nanometers, where unique physicochemical properties emerge that are distinct from their bulk counterparts [1] [2]. These materials have become foundational to modern biomedical research, enabling revolutionary advances in drug delivery, diagnostic imaging, and therapeutic interventions. The international scientific community, including organizations like the International Organization for Standardization (ISO) and the European Commission, recognizes nanomaterials as materials with external dimensions or internal structures at the nanoscale, typically within the 1-100 nm range, though definitions may vary slightly between regulatory bodies [1]. For biomedical applications specifically, nanoparticles used in drug delivery often fall within a slightly broader range of 10-200 nm to optimize biodistribution and targeting efficiency [3].
The classification of nanoparticles into organic and inorganic categories represents a fundamental distinction based on their core composition and structural organization. This classification directly influences their biological behavior, therapeutic potential, and toxicity profiles—factors of critical importance to researchers, scientists, and drug development professionals working to translate nanomedicine from laboratory research to clinical applications. Organic nanoparticles are primarily composed of carbon-based frameworks and include structures such as liposomes, polymeric nanoparticles, dendrimers, and micelles. In contrast, inorganic nanoparticles encompass non-carbon-based materials including metals, metal oxides, semiconductors, and silica-based nanostructures [1] [3] [4]. The strategic selection between organic and inorganic nanoparticles depends heavily on the specific biomedical application, desired pharmacokinetics, and acceptable safety profile, necessitating a thorough understanding of their comparative characteristics.
Composition and Structural Organization
The fundamental distinction between organic and inorganic nanoparticles originates from their atomic composition and structural architecture, which directly dictate their physical properties and biological interactions.
Organic Nanoparticles: Carbon-Based Architectures
Organic nanoparticles are predominantly composed of carbon-based molecules arranged in specific configurations to form nanostructures. The most prevalent categories include:
Liposomes: Spherical vesicles consisting of one or more phospholipid bilayers surrounding an aqueous core, typically ranging from 50-100 nm in diameter. Their amphiphilic nature allows for encapsulation of both hydrophilic (in the aqueous interior) and hydrophobic (within the lipid bilayer) therapeutic agents [4]. Common phospholipids include phosphatidylcholine (PC), phosphatidylethanolamine (PE), and phosphatidylserine, often stabilized with cholesterol to enhance structural integrity [4].
Polymeric Nanoparticles: These include nanospheres (matrix systems where drugs are dispersed throughout) and nanocapsules (reservoir systems where drugs are confined to an inner cavity surrounded by a polymeric membrane) [1]. They are typically synthesized from biodegradable polymers such as polylactic-co-glycolic acid (PLGA), poly(lactic acid) (PLA), or poly(ε-caprolactone) (PCL).
Dendrimers: Highly branched, monodisperse synthetic polymers with a tree-like architecture featuring a central core, interior branches, and terminal functional groups. This precise structure enables controlled drug conjugation and release kinetics [5].
Micelles: Self-assembled structures formed from amphiphilic block copolymers in aqueous solutions, typically 10-100 nm in diameter, with a hydrophobic core and hydrophilic shell suitable for delivering poorly water-soluble drugs [1].
Inorganic Nanoparticles: Non-Carbon Frameworks
Inorganic nanoparticles encompass a diverse range of non-carbon-based materials with unique electronic, magnetic, and optical properties:
Metal Nanoparticles: Include noble metals such as gold (Au), silver (Ag), and platinum (Pt) nanoparticles. Gold nanoparticles (AuNPs) are particularly notable for their tunable surface plasmon resonance, biocompatibility, and ease of surface functionalization [1] [4]. They can be synthesized in various shapes including spheres, rods, cubes, and triangles, each with distinct optical properties [4].
Metal Oxide Nanoparticles: Comprise materials such as iron oxide (Fe₃O₄ or γ-Fe₂O₃), zinc oxide (ZnO), titanium dioxide (TiO₂), and cerium oxide (CeO₂). Iron oxide nanoparticles (IONPs) exhibit superparamagnetic properties when smaller than 20 nm, making them valuable for magnetic resonance imaging (MRI) and magnetic hyperthermia applications [1] [4].
Semiconductor Nanoparticles: Quantum dots (QDs) such as cadmium selenide (CdSe) and zinc sulfide (ZnS) feature size-tunable fluorescence emission based on quantum confinement effects, making them powerful tools for bioimaging and biosensing [6].
Mesoporous Silica Nanoparticles (MSNPs): Characterized by their highly ordered porous structures with pore diameters of 2-50 nm, providing substantial surface area for drug loading and functionalization [4].
Upconversion Nanoparticles (UCNPs): Typically composed of lanthanide-doped crystals that can convert near-infrared light to higher-energy UV or visible light, enabling deep-tissue imaging and light-triggered therapies [7].
Table 1: Comparative Analysis of Organic vs. Inorganic Nanoparticles
| Characteristic | Organic Nanoparticles | Inorganic Nanoparticles |
|---|---|---|
| Core Composition | Carbon-based molecules (phospholipids, polymers) | Metals, metal oxides, semiconductors, silica |
| Structural Features | Bilayer membranes (liposomes), branched architectures (dendrimers), polymeric matrices | Crystalline or amorphous structures, quantum confinement (QDs), porous frameworks (MSNPs) |
| Size Range | 10-200 nm (typically for drug delivery) | 1-100 nm (highly size-dependent properties) |
| Biodegradability | Generally biodegradable and biocompatible | Variable; some resistant to degradation (AuNPs), others soluble (IONPs) |
| Surface Functionalization | Covalent attachment or lipid conjugation | Thiol, amine, or carboxyl group conjugation; silica coating |
| Optical Properties | Limited intrinsic optical properties | Strong plasmonic resonance (Au, Ag), fluorescence (QDs), upconversion (UCNPs) |
| Magnetic Properties | Generally non-magnetic | Superparamagnetism (IONPs) |
| Typical Synthesis Approaches | Self-assembly, emulsion techniques, solvent evaporation | Chemical reduction, co-precipitation, sol-gel, green synthesis |
Toxicity Profiles: Mechanisms and Comparative Analysis
Understanding the toxicity mechanisms of nanoparticles is essential for their safe application in biomedicine. Both organic and inorganic nanoparticles exhibit distinct biological interactions that influence their toxicological profiles.
Organic Nanoparticle Toxicity Mechanisms
Organic nanoparticles generally demonstrate favorable biocompatibility profiles but can still elicit toxic responses under certain conditions:
Immune Recognition and Reactivity: While designed to be stealthy, some polymeric nanoparticles may trigger immune recognition through opsonization, leading to complement activation and subsequent inflammatory responses [6]. Surface properties, particularly charge, significantly influence this interaction, with cationic surfaces often exhibiting higher immunogenicity [2].
Oxidative Stress Induction: Despite being less pronounced than in inorganic nanoparticles, certain organic nanocarriers can induce reactive oxygen species (ROS) generation through intracellular interactions, potentially leading to oxidative damage to cellular components including lipids, proteins, and DNA [6].
Metabolic Byproducts: Biodegradable polymers breakdown into metabolic byproducts that may accumulate or cause local pH changes, potentially disrupting cellular homeostasis. The rate and nature of degradation products must be carefully evaluated for chronic applications [6].
Inorganic Nanoparticle Toxicity Mechanisms
Inorganic nanoparticles typically exhibit more complex and material-specific toxicity pathways:
Reactive Oxygen Species (ROS) Generation: A primary toxicity mechanism for many inorganic nanoparticles involves the catalysis of ROS formation, including superoxide anion (O₂•⁻), hydroxyl radicals (•OH), and hydrogen peroxide (H₂O₂) [2] [6]. Metal nanoparticles like silver and metal oxides such as ZnO and CuO are particularly potent ROS inducers through Fenton-like reactions and surface reactivity [2]. Excessive ROS production overwhelms cellular antioxidant defenses, leading to oxidative stress, lipid peroxidation, protein denaturation, and DNA damage [2] [6].
Ion Release and Metal Toxicity: Many metallic nanoparticles undergo gradual dissolution in biological environments, releasing toxic ions that mediate cellular damage. For example, silver nanoparticles (AgNPs) release Ag⁺ ions that bind to thiol groups in proteins and enzymes, disrupting mitochondrial function and electron transport chains [2]. Similarly, cadmium-based quantum dots release Cd²⁺ ions, which are highly toxic to cells [6].
Protein Corona Formation and Cellular Interactions: When introduced into biological fluids, nanoparticles rapidly adsorb proteins onto their surfaces, forming a "protein corona" that alters their biological identity and cellular interactions [6]. The composition of this corona influences cellular uptake, biodistribution, and immunological responses, potentially masking targeting functionalities intentionally placed on the nanoparticle surface [6].
Mitochondrial Dysfunction: Nanoparticles can localize to mitochondria, disrupting membrane potential, impairing ATP production, and promoting apoptosis through cytochrome c release [8] [6]. This is particularly documented for cationic nanoparticles that preferentially target the negatively charged mitochondrial membrane.
Genotoxicity and Epigenetic Alterations: Certain nanoparticles can directly or indirectly cause DNA damage through ROS-mediated oxidation, physical interaction with nuclear material, or interference with DNA repair mechanisms [2] [6]. This may lead to chromosomal aberrations, micronuclei formation, and alterations in gene expression patterns.
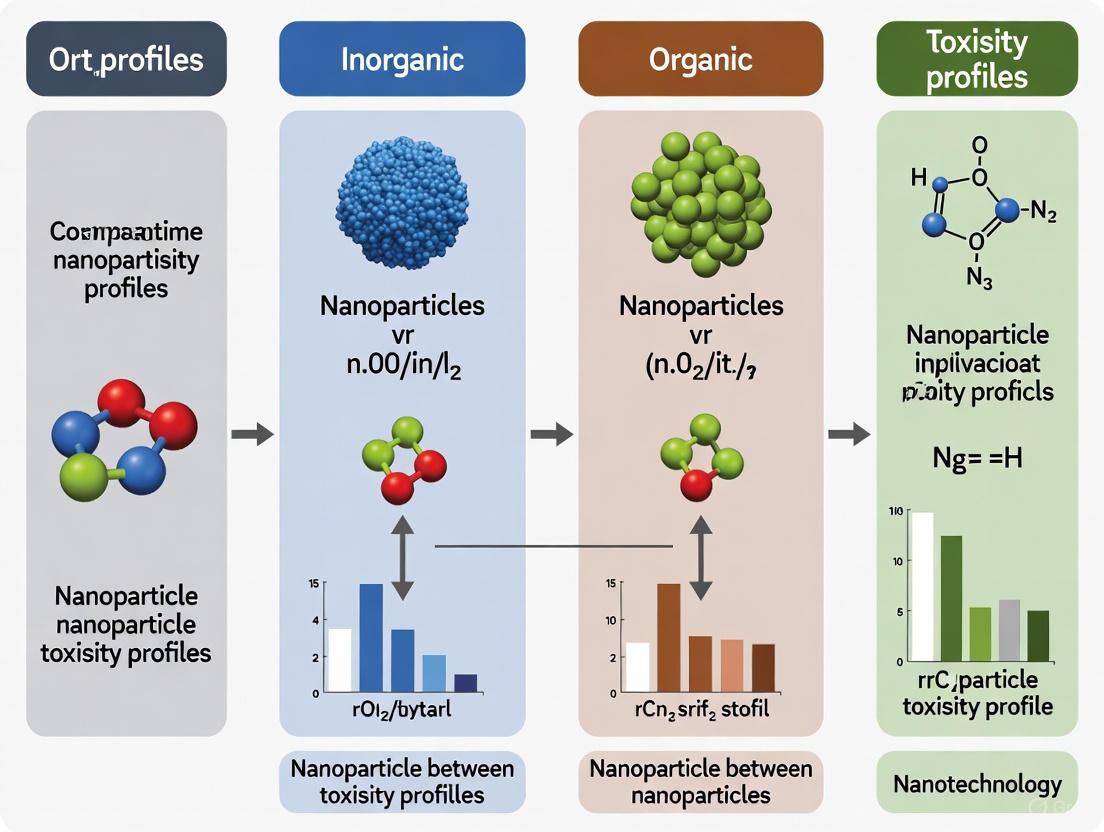
The following diagram illustrates the primary toxicity pathways shared by various nanoparticle types:
Figure 1: Primary toxicity mechanisms of nanoparticles at cellular and molecular levels
Factors Influencing Nanoparticle Toxicity
Multiple physicochemical parameters significantly influence nanoparticle toxicity profiles, regardless of their organic or inorganic classification:
Size: Smaller nanoparticles typically exhibit higher toxicity due to increased surface area-to-volume ratios, enhanced cellular uptake, and ability to penetrate biological barriers including the blood-brain barrier [2] [5]. Particles below 5.5 nm often undergo renal clearance, while larger particles accumulate in mononuclear phagocyte system organs (liver, spleen) [2].
Shape: Morphology affects cellular uptake mechanisms and toxicity; needle-like or high-aspect-ratio nanoparticles may cause physical membrane disruption, while spherical particles are generally internalized via endocytosis [2]. For instance, nanorod-shaped ZnO particles demonstrate higher toxicity to lung epithelial cells compared to spherical counterparts [2].
Surface Charge: Cationic nanoparticles typically exhibit greater cytotoxicity than anionic or neutral counterparts due to stronger electrostatic interactions with negatively charged cell membranes, enhancing cellular uptake and membrane disruption potential [2] [6].
Surface Chemistry and Functionalization: Surface modifications can dramatically alter toxicity profiles. PEGylation creates a steric barrier that reduces protein adsorption and opsonization, while targeting ligands may influence tissue-specific accumulation [2] [4].
Table 2: Physicochemical Parameters Affecting Nanoparticle Toxicity
| Parameter | Toxicity Influence | Experimental Evidence |
|---|---|---|
| Size | Smaller particles (<20 nm) generally more toxic due to higher reactivity and deeper tissue penetration | Particles <5.5 nm cleared renally; larger particles accumulate in liver/spleen [2] |
| Shape | High-aspect-ratio particles (rods, needles) may cause physical membrane damage | ZnO nanorods more toxic to lung cells than spherical particles [2] |
| Surface Charge | Cationic surfaces typically more toxic due to membrane interaction | Positively charged NPs show enhanced uptake and oxidative stress [2] |
| Chemical Composition | Metal ions leaching from NPs contribute significantly to toxicity | Ag⁺ ions from AgNPs bind to cellular thiol groups [2] |
| Surface Area | Higher surface area correlates with increased reactivity and ROS generation | NPs with larger surface area show greater bactericidal effects [1] |
| Solubility/Dissolution | Rate of dissolution affects ion release and persistence | More soluble metal oxides show higher acute toxicity [2] |
| Protein Corona | Alters cellular recognition, uptake, and biodistribution | Corona can mask targeting ligands on functionalized NPs [6] |
Experimental Methodologies for Toxicity Assessment
Standardized experimental protocols are essential for evaluating nanoparticle toxicity and generating comparable data across studies. The following section outlines key methodologies cited in current literature.
In Vitro Cytotoxicity Assessment
Cell culture studies represent the first tier of nanotoxicity evaluation due to advantages including cost-effectiveness, rapid results, ethical acceptability, and experimental control [6]. Standard protocols include:
Cell Viability Assays: MTT, XTT, and WST-1 assays measure mitochondrial reductase activity as an indicator of metabolic activity and cell viability. These colorimetric tests provide quantitative data on cytotoxicity but may suffer from interference with certain nanoparticles that directly reduce tetrazolium salts or absorb at measurement wavelengths [6]. Protocol: Seed cells in 96-well plates (5,000-10,000 cells/well), incubate for 24 hours, treat with nanoparticle suspensions across a concentration range (typically 0-200 μg/mL) for 24-72 hours, add MTT solution (0.5 mg/mL), incubate 2-4 hours, dissolve formazan crystals with DMSO, and measure absorbance at 570 nm with reference at 630-690 nm [6].
Membrane Integrity Assays: Lactate dehydrogenase (LDH) release quantifies plasma membrane damage by measuring the cytoplasmic enzyme LDH in cell culture supernatants. Protocol: Collect supernatant from nanoparticle-treated cells, incubate with NADH and pyruvate in appropriate buffer, and measure absorbance decrease at 340 nm due to NADH oxidation [6].
Oxidative Stress Detection: Dichloro-dihydro-fluorescein diacetate (DCFH-DA) assay measures intracellular ROS production. The non-fluorescent DCFH-DA diffuses into cells where intracellular esterases remove the diacetate group, and subsequent oxidation by ROS produces fluorescent DCF. Protocol: Load cells with 10-20 μM DCFH-DA for 30 minutes, treat with nanoparticles, and measure fluorescence at 485 nm excitation/535 nm emission [6].
Genotoxicity Assessment: Comet assay (single-cell gel electrophoresis) detects DNA strand breaks at the individual cell level. Protocol: Embed nanoparticle-treated cells in low-melting-point agarose on microscope slides, lyse cells to remove membranes and proteins, electrophorese under alkaline conditions, stain with DNA-binding fluorescent dye, and analyze for DNA migration patterns [6].
In Vivo Toxicity Evaluation
Animal studies provide critical information on biodistribution, accumulation, and systemic toxicity:
Biodistribution Studies: Utilize radiolabeled or fluorescently tagged nanoparticles to track tissue distribution over time. Typically performed in rodents via various administration routes (intravenous, oral, inhalation) with subsequent tissue collection and analysis at predetermined time points [6]. Inductively coupled plasma mass spectrometry (ICP-MS) provides quantitative elemental analysis for metal-based nanoparticles.
Histopathological Examination: Systematic microscopic evaluation of tissue sections from major organs (liver, spleen, kidneys, lungs, brain) after necropsy to identify nanoparticle-induced lesions, inflammation, fibrosis, or other pathological changes [8] [6].
Hematological and Biochemical Analysis: Blood collection for complete blood count, differential white cell analysis, and plasma biochemistry markers of organ function (liver enzymes, renal function parameters) to detect systemic toxicity [6].
Immunotoxicity Assessment: Flow cytometric analysis of immune cell populations, cytokine profiling, and evaluation of hypersensitivity responses to identify immunomodulatory effects [8].
The following workflow diagram outlines a comprehensive nanoparticle toxicity assessment strategy:
Figure 2: Comprehensive toxicity assessment workflow for nanoparticles
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogizes critical reagents, materials, and experimental systems employed in nanoparticle toxicity research, as referenced in the current literature:
Table 3: Essential Research Reagents and Experimental Systems for Nanoparticle Toxicity Studies
| Reagent/System | Function/Application | Specific Examples |
|---|---|---|
| Cell Line Models | In vitro toxicity screening | Human lung epithelial cells (A549), liver hepatocytes (HepG2), macrophages (THP-1), and primary cells for tissue-specific responses [6] |
| MTT/XTT/WST-1 Assays | Cell viability and metabolic activity assessment | Tetrazolium salt reduction measured spectrophotometrically; mitochondrial function indicator [6] |
| DCFH-DA Probe | Intracellular ROS detection | Fluorescence-based measurement of oxidative stress; excitation/emission at 485/535 nm [6] |
| LDH Assay Kit | Membrane integrity assessment | Quantifies lactate dehydrogenase release from damaged cells [6] |
| Comet Assay Reagents | DNA damage evaluation | Alkaline electrophoresis for detection of single-strand breaks in individual cells [6] |
| Animal Models | In vivo toxicity and biodistribution | Rodent models (mice, rats) for systemic toxicity assessment [8] [6] |
| ICP-MS | Quantitative elemental analysis | Detection and quantification of metal-based nanoparticles in biological tissues [6] |
| Dynamic Light Scattering | Hydrodynamic size and zeta potential | Particle size distribution and surface charge measurement in suspension [2] |
| Protein Corona Analysis | Characterization of bio-nano interactions | SDS-PAGE, mass spectrometry to identify adsorbed proteins [6] |
The comparative analysis of organic and inorganic nanoparticles reveals distinct advantages and limitations that inform their selection for specific biomedical applications. Organic nanoparticles, particularly liposomes and polymeric NPs, generally offer superior biocompatibility and biodegradability with established regulatory approval pathways, as evidenced by FDA-approved formulations like Doxil [4]. Their tunable release kinetics and functionalization capabilities make them particularly suitable for drug delivery applications where long-term safety is paramount. However, they often lack the inherent functionality for imaging and external activation possessed by many inorganic nanoparticles.
Inorganic nanoparticles provide unique physical properties—including magnetic responsiveness (IONPs), plasmonic characteristics (AuNPs), and fluorescent emissions (QDs)—that enable multifunctional applications in imaging, diagnostics, and triggered therapies [7] [4]. These advantages come with increased toxicological concerns, particularly regarding ion leaching, ROS generation, and long-term persistence in biological systems. Their toxicity profiles are highly dependent on specific physicochemical parameters including size, shape, surface chemistry, and coating strategies.
The emerging paradigm in nanomedicine involves combining the advantages of both material classes through hybrid approaches, such as inorganic nanoparticles encapsulated in organic coatings or organic-inorganic composite systems. These strategies aim to mitigate toxicity while preserving functionality. Future research directions should prioritize systematic structure-activity relationship studies, long-term fate investigations, and standardized toxicity assessment protocols to enable rational design of safer nanoparticles. As the field advances, the strategic selection between organic and inorganic platforms will continue to depend on a balanced consideration of therapeutic objectives, imaging requirements, and acceptable risk-benefit profiles tailored to specific clinical applications.
The expanding application of nanoparticles (NPs) in fields like medicine, consumer goods, and electronics necessitates a thorough understanding of their toxicological profiles [9] [10]. For researchers and drug development professionals, predicting and mitigating nanotoxicity is paramount for designing safer nanomedicines and products. The toxicity of NPs is not a function of a single parameter but is governed by a complex interplay of key physicochemical properties: size, shape, surface charge, and composition [11]. Furthermore, a fundamental distinction in nanotoxicology lies in the classification of NPs as organic or inorganic, as their core material dictates their basic biological interactions and persistence [12]. This guide provides a comparative analysis of how these properties influence the toxicity of organic and inorganic NPs, supported by experimental data and methodologies.
Comparative Analysis of Key Physicochemical Properties
The following sections and tables detail how each physicochemical property influences NP toxicity, with specific comparisons between organic and inorganic NPs.
Nanoparticle Size
Size directly influences cellular uptake, biodistribution, and the surface area available for biological interactions. Smaller NPs (typically < 20 nm) generally exhibit greater toxicity due to their ability to penetrate cellular barriers, access subcellular compartments, and generate higher reactive oxygen species (ROS) per unit mass [11].
Table 1: Impact of Nanoparticle Size on Toxicity
| NP Type | Specific NP | Size Compared | Experimental Model | Key Toxicological Findings |
|---|---|---|---|---|
| Inorganic | Gold (Au) [11] | 2, 6, 10, 16 nm | MCF-7 breast cancer cells | NPs <10 nm internalized into the cell nucleus; larger NPs remained in the cytoplasm. |
| Inorganic | Silver (Ag) [11] | 10, 40, 100 nm | In vivo (mice) | 10 nm NPs had higher tissue distribution and more severe hepatobiliary toxicity. |
| Inorganic | Titanium Dioxide (TiO₂) [11] | 6, 12, 15 nm | Zebrafish embryos | 6 nm NPs caused more oxidative stress and DNA damage under illumination. |
| Inorganic | Silver (Ag) [10] | 10 nm | In vivo (mice) | Smaller NPs improve tissue distribution and increase hepatobiliary toxicity. |
| General | Not Specified [13] | Smaller vs. Larger | Machine Learning Model | Smaller NPs have heightened toxicity due to larger surface-to-volume ratios. |
Nanoparticle Shape
The shape of a NP affects its kinetics of cellular uptake, circulation time in the body, and the nature of its interaction with cellular membranes [11].
Table 2: Impact of Nanoparticle Shape on Toxicity
| NP Type | Shape Compared | Experimental Model / Basis | Key Toxicological Findings |
|---|---|---|---|
| General | Spheres, rods, sheets, cubes [11] | Computational & Cellular Studies | Non-spherical NPs (e.g., rods, sheets) are internalized faster and in larger amounts than spherical NPs. |
| General | Spheres vs. Non-spherical [11] | In vivo biodistribution studies | Non-spherical NPs can have longer blood circulation time and higher accumulation in specific organs. |
Surface Charge and Chemistry
Surface charge, often indicated by zeta potential, governs the electrostatic interactions between NPs and negatively charged cell membranes. While cationic (positively charged) NPs are generally associated with higher toxicity and cellular uptake, recent evidence suggests surface charge density is a more precise predictor than zeta potential alone [14] [11].
Table 3: Impact of Surface Charge on Toxicity
| NP Type | Surface Property Tested | Experimental Model | Key Toxicological Findings |
|---|---|---|---|
| Organic (Carbon Dots) | Surface charge density [14] | THP-1 macrophages, A549/Calu-3 cells, mice | Cationic NPs with high surface charge density (Qek > 2.95 µmol/g) induced oxidative stress, IL-8 release, and airway inflammation. NPs with low density did not. |
| Organic (Carbon Dots) | Zeta potential [14] | THP-1 macrophages | Five cationic NPs with similar ζ-potential (+20 to +27 mV) showed vastly different toxicity, correlated with charge density, not ζ-potential. |
| General | Cationic vs. Anionic [14] | Literature Review | A positive ζ-potential is often associated with greater toxicity due to strong electrostatic interaction with cell membranes. |
Chemical Composition
The core material of a NP determines its intrinsic chemical reactivity, solubility, and potential for ion release, which are primary drivers of toxicity. This property fundamentally differentiates organic and inorganic NPs [12].
Table 4: Impact of Chemical Composition on Toxicity (Organic vs. Inorganic)
| NP Class | Composition Examples | Key Toxicological Mechanisms | Notes on Persistence & Biodegradation |
|---|---|---|---|
| Inorganic | Metal (Ag, Au) [11], Metal Oxides (ZnO, TiO₂, SiO₂) [9] | ROS generation via Fenton-like reactions, release of toxic ions (e.g., Ag⁺, Zn²⁺), permanent catalytic activity, oxidative stress [9] [11]. | Generally more persistent in the environment and biological systems; can undergo transformation (e.g., sulfidation) [15]. |
| Organic | Polymers (PLGA), Lipids, Dendrimers [12] | Interaction with cellular membranes, disruption of lipid bilayers, inflammation from degradation products [16]. | Typically biodegradable and less persistent; toxicity is often more dependent on surface functionalization [12] [16]. |
Experimental Protocols for Toxicity Assessment
To generate the data cited above, standardized experimental protocols are employed. Below are detailed methodologies for key tests.
1In VitroCytotoxicity and Mechanistic Assays
- Cell Culture: Use relevant cell lines (e.g., THP-1-derived macrophages, A549 or Calu-3 airway epithelial cells) [14]. Maintain cells in appropriate media and culture conditions.
- NP Exposure:
- Viability Assessment:
- Perform MTT or MTS assay. This measures mitochondrial activity by the reduction of tetrazolium salts to formazan dyes. Add reagent to wells after NP exposure, incubate, and measure absorbance. Viability is expressed as a percentage of the untreated control [14].
- Oxidative Stress Measurement:
- Use a fluorescent probe, such as H2DCFDA. After NP exposure, load cells with the probe, which is oxidized by intracellular ROS to a fluorescent product. Quantify fluorescence using a plate reader or flow cytometry [14].
- Inflammatory Response:
- Collect cell culture supernatant after NP exposure.
- Measure the concentration of pro-inflammatory cytokines like Interleukin-8 (IL-8) using an Enzyme-Linked Immunosorbent Assay (ELISA) kit according to the manufacturer's protocol [14].
- Cellular Uptake:
- For fluorescent NPs (e.g., carbon dots), use Flow Cytometry (FACS) or Confocal Laser Scanning Microscopy (CLSM). For FACS, trypsinize and analyze cells to quantify fluorescence intensity. For CLSM, fix cells and image to visualize NP localization [14].
2In VivoPulmonary Toxicity Assessment
- Animal Model: Use specific pathogen-free mice (e.g., C57BL/6) [14].
- NP Administration:
- Anesthetize mice.
- Administer a single dose of NPs (e.g., 50 µg in 50 µL of saline) via oropharyngeal aspiration. A control group receives saline only [14].
- Bronchoalveolar Lavage (BAL) and Analysis:
- At a set endpoint (e.g., 24 hours post-exposure), euthanize the animals.
- Cannulate the trachea and lavage the lungs with sterile saline.
- Centrifuge the BAL fluid (BALF). The supernatant can be used for cytokine analysis (e.g., ELISA).
- Resuspend the cell pellet and perform total cell counts. Prepare cytospin slides, stain (e.g., with Diff-Quick), and perform differential cell counts (macrophages, neutrophils, lymphocytes) under a microscope to quantify airway inflammation [14].
Visualization of Key Toxicity Pathways
The following diagram integrates the properties discussed into a common pathway for NP-induced toxicity, highlighting the central role of oxidative stress.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table lists key materials and tools used in the featured experiments for studying nanoparticle toxicity.
Table 5: Research Reagent Solutions for Nanotoxicity Studies
| Item | Function / Explanation | Example Use Case |
|---|---|---|
| THP-1 Cell Line | Human monocytic cell line that can be differentiated into macrophage-like cells. A key model for immune response and phagocytosis studies. | Assessing NP uptake, cytotoxicity, and inflammatory cytokine release in immune cells [14]. |
| A549 / Calu-3 Cell Lines | Human lung epithelial cell lines. Representative models for the respiratory tract, a primary exposure route. | Evaluating cytotoxicity and barrier function disruption in the lung [14]. |
| MTT / MTS Assay Kits | Colorimetric assays that measure the metabolic activity of cells, serving as an indicator of cell viability and proliferation. | Quantifying NP-induced cytotoxicity in vitro [14]. |
| H2DCFDA Fluorescent Probe | Cell-permeable dye that becomes fluorescent upon oxidation by reactive oxygen species (ROS). | Detecting and quantifying intracellular oxidative stress triggered by NPs [14]. |
| ELISA Kits (e.g., for IL-8) | Immunoassay kits for the precise quantification of specific proteins or cytokines in a sample. | Measuring the levels of pro-inflammatory cytokines in cell culture supernatant or bronchoalveolar lavage fluid (BALF) [14]. |
| Dynamic Light Scattering (DLS) | Instrumentation to measure the hydrodynamic size distribution and aggregation state of NPs in suspension. | Characterizing the stability and size profile of NPs in biological media [14]. |
| Zeta Potential Analyzer | Instrumentation to measure the surface charge (electrostatic potential) of NPs in suspension. | Determining NP surface charge, a key property influencing colloidal stability and cellular interaction [14]. |
The expanding application of nanoparticles (NPs) in biotechnology, medicine, and consumer products has necessitated a thorough understanding of their biological interactions and toxicological profiles [17]. Engineered nanomaterials (NMs), defined as materials with at least one external dimension between 1-100 nm, exhibit unique physicochemical properties that differ markedly from their bulk counterparts [5]. These very properties—small size, large surface area-to-volume ratio, and enhanced reactivity—that make NPs technologically valuable also raise concerns about their potential adverse effects on human health and the environment [17] [18]. When NPs enter biological systems, they can initiate a cascade of molecular events at the cellular level, primarily through induction of oxidative stress, inflammation, genotoxicity, and apoptosis [17] [19]. Understanding these fundamental mechanisms is crucial for researchers, scientists, and drug development professionals working toward the safe implementation of nanotechnologies. This review systematically compares the toxicity mechanisms of inorganic versus organic nanoparticles, providing experimental methodologies, key signaling pathways, and essential research tools for investigating nanomaterial toxicity.
Comparative Toxicity Mechanisms of Inorganic and Organic Nanoparticles
The table below summarizes the primary toxicity mechanisms associated with major classes of inorganic and organic nanoparticles, based on current literature:
Table 1: Comparative Toxicity Profiles of Selected Nanoparticles
| Nanoparticle Type | Oxidative Stress | Inflammation | Genotoxicity | Apoptosis | Key Mechanisms |
|---|---|---|---|---|---|
| Metal Oxide (ZnO) | High [18] | Moderate [18] | High [18] | High [18] | Dissolution releasing Zn²⁺ ions; ROS generation; mitochondrial dysfunction [17] [18] |
| Metal Oxide (TiO₂) | Moderate [19] | Moderate [19] | Moderate [19] | Moderate [19] | Photocatalytic ROS generation; DNA strand breaks; inflammatory cytokine activation [19] |
| Metal (Silver) | High [18] | High [18] | High [18] | High [18] | ROS generation; LDH leakage; DNA adduct formation; membrane damage [18] |
| Metal (Gold) | Low [18] | Low [18] | Low [18] | Low [18] | Generally inert; toxicity dependent on surface functionalization [18] |
| Carbon-Based (CNT) | High [17] | High [17] | Moderate [17] | High [17] | Mitochondrial damage; fiber-like pathogenicity; proinflammatory cytokine release [17] |
| Polymeric (Chitosan) | Low [5] | Low [5] | Low [5] | Low [5] | Generally biocompatible and biodegradable [5] |
The toxicity of nanoparticles is governed by multiple physicochemical parameters including size, shape, surface charge, coating, and chemical composition [5]. Smaller nanoparticles typically exhibit greater toxicity due to their increased surface area-to-volume ratio and enhanced reactivity [17] [20]. Surface coatings play a crucial role in modulating nanoparticle behavior; for instance, polyethylene glycol (PEG) coatings can reduce toxicity by stabilizing dispersion and altering bioavailability [20]. Inorganic metal and metal oxide nanoparticles often exert toxicity through ion release and Fenton-type reactions that generate reactive oxygen species (ROS) [17], while carbon-based materials may cause physical membrane damage and oxidative stress via mitochondrial disruption [17].
Key Cellular Toxicity Mechanisms
Oxidative Stress
Oxidative stress represents a primary mechanism of nanoparticle-induced toxicity, resulting from an imbalance between ROS production and the biological system's ability to detoxify these reactive intermediates [17]. NPs can generate ROS through several pathways: (1) prooxidant functional groups on reactive surfaces; (2) active redox cycling on transition metal-based NP surfaces; and (3) particle-cell interactions that disturb cellular components [17]. The hierarchical model of oxidative stress illustrates cellular responses to increasing levels of ROS: at mild oxidative stress levels, cells activate phase II antioxidant enzymes via Nrf2 induction; intermediate levels trigger proinflammatory responses through MAPK and NF-κB signaling; while severe oxidative stress causes mitochondrial dysfunction and cell death [17]. Metal-based nanoparticles like copper, iron, and silver can catalyze Fenton-type and Haber-Weiss reactions, generating highly reactive hydroxyl radicals (OH•) that damage cellular components [17].
Inflammation
NP-induced oxidative stress often functions as a torchbearer for inflammatory responses [17]. Inflammatory cells such as macrophages and neutrophils can become activated upon exposure to NPs, leading to increased production of ROS and proinflammatory cytokines [17]. Signaling pathways including nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) and mitogen-activated protein kinase (MAPK) cascades become activated, resulting in the increased expression of cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-8 (IL-8) [17] [19]. Chronic inflammation induced by nanoparticles can lead to more severe pathological conditions including fibrosis, granuloma formation, and tissue damage [17].
Genotoxicity
Nanoparticles can cause damage to genetic material through both direct and indirect mechanisms [19]. Direct genotoxicity may occur when NPs or their dissolved ions physically interact with DNA, causing strand breaks, cross-links, or base modifications [19]. Indirect genotoxicity can result from oxidative stress-induced DNA damage or from interference with DNA repair mechanisms [17]. The comet assay (single-cell gel electrophoresis) is frequently employed to detect DNA strand breaks, while micronucleus tests and chromosomal aberration assays identify chromosomal damage [18] [19]. Studies have demonstrated that co-exposure to multiple toxicants, such as TiO₂ nanoparticles and acrylamide, can synergistically enhance genotoxic effects, resulting in increased DNA strand breaks in brain tissues of experimental models [19].
Apoptosis
NP-induced oxidative stress and DNA damage can trigger programmed cell death through apoptotic pathways [19]. This process involves the upregulation of tumor suppressor protein p53, activation of caspase cascades, and characteristic DNA fragmentation [19]. Studies with TiO₂ nanoparticles have shown increased expression of apoptotic genes including P53, TNF-α, IL-6, and Presenillin-1 in neural tissues [19]. The laddered DNA fragmentation assay is commonly used to detect the internucleosomal DNA cleavage patterns characteristic of apoptosis [19]. The extent of apoptotic induction varies significantly among different nanoparticle types, with more reactive materials like silver and zinc oxide nanoparticles typically causing greater apoptotic responses compared to relatively inert nanoparticles like gold or certain polymeric NPs [18].
Experimental Protocols for Toxicity Assessment
Assessing Oxidative Stress
Intracellular ROS Measurement using DCFH-DA Assay The fluorescent probe 2',7'-dichlorodihydrofluorescein diacetate (DCFH-DA) is widely used to detect intracellular ROS generation [19]. The non-fluorescent DCFH-DA passively enters cells, where intracellular esterases remove the diacetate group, trapping the non-fluorescent DCFH within cells. ROS oxidize DCFH to the highly fluorescent compound DCF, which can be quantified.
Protocol:
- Culture cells in appropriate medium and seed in multi-well plates at optimal density
- Expose cells to nanoparticles at various concentrations for selected time points
- Remove medium and wash cells with phosphate-buffered saline (PBS)
- Incubate cells with DCFH-DA (10-20 μM in serum-free medium) for 30 minutes at 37°C in the dark
- Remove DCFH-DA solution and wash cells with PBS
- Measure fluorescence intensity using fluorescence microscopy, flow cytometry, or microplate reader (excitation 485 nm, emission 535 nm)
- Include appropriate controls: untreated cells (background), positive control (e.g., H₂O₂-treated cells)
Evaluating Genotoxicity
Alkaline Comet Assay for DNA Strand Breaks The alkaline comet assay (single-cell gel electrophoresis) detects DNA single- and double-strand breaks at the individual cell level [19].
Protocol:
- Prepare cell suspension from treated tissue or cell culture (approximately 10,000 cells)
- Mix cells with 0.5% low melting point agarose and layer onto pre-coated slides
- Immerse slides in cold lysis buffer (2.5 M NaCl, 100 mM EDTA, 10 mM Tris, 1% Triton X-100, 10% DMSO; pH 10) for at least 1 hour at 4°C
- Place slides in alkaline electrophoresis buffer (300 mM NaOH, 1 mM EDTA; pH >13) for 20-40 minutes to allow DNA unwinding
- Perform electrophoresis at 25 V, 300 mA for 20-30 minutes
- Neutralize slides with Tris buffer (0.4 M Trizma base; pH 7.5) and stain with DNA-binding dye (e.g., ethidium bromide, SYBR Green)
- Analyze using fluorescence microscopy; quantify DNA damage using parameters like tail length, % DNA in tail, and tail moment with specialized software
Detecting Apoptosis
DNA Laddering Assay Apoptotic cells exhibit characteristic internucleosomal DNA cleavage, producing a "ladder" pattern when separated by agarose gel electrophoresis [19].
Protocol:
- Homogenize tissue samples or collect cultured cells
- Lyse samples in Tris-EDTA buffer containing 0.5% SDS and 0.5 mg/mL RNase A; incubate at 37°C for 1 hour
- Add proteinase K (0.2 mg/mL) and incubate at 50°C overnight
- Extract DNA using phenol-chloroform-isoamyl alcohol mixture
- Precipitate DNA with ethanol and resuspend in TE buffer
- Quantify DNA concentration and load equal amounts (0.5-1 μg) on 1.5-2% agarose gel containing ethidium bromide
- Perform electrophoresis at 70-80 V for 1-2 hours
- Visualize DNA fragmentation pattern using UV transilluminator; apoptotic samples show characteristic ~180-200 bp laddering
Signaling Pathways in Nanoparticle Toxicity
The following diagrams illustrate key signaling pathways involved in nanoparticle-induced toxicity, created using Graphviz DOT language:
Cellular Response Pathways to Nanoparticle-Induced Oxidative Stress
Comprehensive Toxicity Assessment Methodology
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Reagents for Nanoparticle Toxicity Research
| Reagent/Chemical | Function/Application | Examples/Notes |
|---|---|---|
| DCFH-DA | Detection of intracellular ROS | Fluorescent probe oxidized by ROS to DCF; used in various cell types [19] |
| MTT/MTS/WST-1 | Cell viability and metabolic activity assays | Tetrazolium-based assays; measure mitochondrial function [18] |
| LDH Assay Kit | Cell membrane integrity assessment | Measures lactate dehydrogenase release upon membrane damage [18] |
| ELISA Kits | Quantification of cytokines and biomarkers | Detect TNF-α, IL-6, IL-8 and other inflammatory mediators [21] |
| Comet Assay Reagents | Detection of DNA strand breaks | Low melting point agarose, lysis buffers, fluorescent DNA dyes [19] |
| Apoptosis Detection Kits | Identification of apoptotic cells | Annexin V/propidium iodide staining; caspase activity assays [19] |
| Antioxidant Assays | Measurement of oxidative stress markers | Kits for GSH, SOD, CAT, GPx, lipid peroxidation products [17] [21] |
| qPCR Reagents | Gene expression analysis | Primers for p53, TNF-α, IL-6, Presenillin-1 and other relevant genes [19] |
The cellular mechanisms underlying nanoparticle toxicity involve complex, interconnected pathways centered around oxidative stress, inflammation, genotoxicity, and apoptosis. Inorganic nanoparticles, particularly metal and metal oxide varieties, often exhibit higher toxicity compared to their organic counterparts, primarily due to their ability to generate ROS via Fenton-type reactions and release toxic ions [17] [18]. The physicochemical properties of nanoparticles—size, shape, surface chemistry, and coating—critically influence their biological interactions and toxic potential [5] [20]. Comprehensive toxicity assessment requires integrated methodological approaches spanning ROS detection, genotoxicity evaluation, inflammatory response measurement, and cell death analysis. As nanotechnology continues to advance, understanding these fundamental toxicity mechanisms becomes increasingly important for the rational design of safer nanomaterials and for accurate risk assessment in both pharmaceutical development and environmental health contexts. Future research should focus on long-term exposure effects, interactions between different nanoparticle types, and the development of standardized testing protocols that better reflect realistic exposure scenarios.
The Role of Surface Chemistry and Functionalization in Biocompatibility and Cellular Interactions
In the field of nanomedicine and biomaterials, the interface between a synthetic material and a biological system is of paramount importance. The surface of a nanoparticle or implantable device is the primary site of interaction with proteins, cells, and tissues, ultimately determining the biological response and therapeutic efficacy. For researchers, scientists, and drug development professionals, understanding how surface chemistry and functionalization influence biocompatibility and cellular interactions is crucial for designing effective biomedical products. This guide provides a comparative examination of how surface properties govern biological responses, with particular attention to the distinct toxicity profiles of inorganic versus organic nanoparticles, supported by experimental data and methodologies.
Surface properties—including chemical composition, charge, hydrophobicity, and specific functional groups—directly dictate the amount, composition, and conformational changes of proteins that adsorb to the material within biological fluids. This initial layer of adsorbed proteins then mediates all subsequent cellular interactions, including inflammatory responses, uptake efficiency, and overall biocompatibility [22]. The ability to engineer surface characteristics through various modification techniques therefore provides a powerful strategy for controlling material-tissue interactions and improving clinical outcomes.
Surface Properties Governing Biocompatibility
Key Physicochemical Properties and Their Biological Impact
The table below summarizes the major surface properties that critically influence biocompatibility and cellular responses, based on extensive experimental observations.
Table 1: Key Surface Properties and Their Biological Impact
| Surface Property | Biological Impact | Experimental Evidence |
|---|---|---|
| Surface Charge (Zeta Potential) | Positively charged surfaces typically enhance cellular uptake but may increase toxicity and protein adsorption. Negatively charged or neutral surfaces often prolong circulation time but may reduce cellular internalization [23]. | Pdots-NH₂ (+3.73 mV) showed 80% cell viability vs. ~90% for Pdots-COOH (-18 mV) at 60 μg/mL in CaSki, 4T1, and BEAS-2B cell lines [24]. |
| Hydrophobicity/ Hydrophilicity | Hydrophilic surfaces generally reduce non-specific protein adsorption and improve biocompatibility. Hydrophobic surfaces tend to promote protein adsorption, often inducing conformational changes that expose inflammatory epitopes [22]. | Hydrophobic biomaterials show progressive, time-dependent conformational changes in adsorbed fibrinogen, exposing Receptor-Induced Binding Sites (RIBS) and increasing resistance to SDS elution [22]. |
| Surface Functional Groups | Specific terminal groups (e.g., -COOH, -NH₂, -OH) directly influence protein binding, cell adhesion, and inflammatory responses. Carboxyl and hydroxyl groups often improve biocompatibility compared to amine groups [22]. | Self-assembled monolayers (SAMs) with controlled functionalities demonstrate that surface chemistry directly influences the extent of foreign body reactions in vivo [22]. |
| Surface Topography & Roughness | Nanoscale roughness and patterns can direct cell alignment, migration, and differentiation (e.g., osteogenesis on rougher surfaces) [25]. | Sandblasting and acid etching of titanium implants create micro- and nano-roughness that enhances bone integration and mechanical interlocking [25]. |
The Protein Adsorption Cascade
The initial moments after a biomaterial is introduced to a biological environment are critical. Within minutes to hours, a layer of host proteins adsorbs onto the surface, a process governed by the material's surface properties [22]. The composition and, more importantly, the conformation of these adsorbed proteins then dictate all subsequent biological responses.
Hydrophobic surfaces, common in many conventional biomaterials, have a high affinity for a wide range of proteins like fibrinogen, albumin, and IgG. Upon adsorption to these surfaces, proteins often undergo conformational changes, exposing hydrophobic domains and cryptic inflammatory epitopes that are normally hidden in their native state [22]. For instance, adsorbed fibrinogen exposes RIBS epitopes (e.g., gamma112-119 and Aα 95-98), which serve as recognition sites for inflammatory cells like macrophages, thereby initiating a foreign body reaction [22].
The following diagram illustrates this critical sequence of events triggered by material surface properties.
Surface Modification Techniques and Functionalization
A variety of physical, chemical, and coating techniques have been developed to engineer material surfaces and elicit desired biological responses.
Table 2: Surface Modification and Functionalization Techniques
| Technique Category | Specific Methods | Key Mechanism & Outcome | Considerations for Research |
|---|---|---|---|
| Physical Methods | Plasma treatment, UV irradiation, Sandblasting [25] | Alters surface energy, introduces functional groups, creates micro/nano-topography without changing bulk chemistry. Plasma treatment can increase hydrophilicity. | Requires specialized equipment. Surface activation can be temporary (ageing effect). Excellent for controlling topography. |
| Chemical Methods | Chemical grafting, SAMs, Silanization, Oxidation [22] [25] | Covalently attaches specific functional groups (e.g., -NH₂, -COOH) or polymer chains (e.g., PEO) to the surface. Provides stable, well-defined coatings. | SAMs limited to gold/silver-coated surfaces [22]. Risk of toxic monomer residues in chemical grafting. |
| Coating & Immobilization | Layer-by-layer (LbL), Dip coating, Grafting ("to" or "from"), PEGylation [25] [23] | Applies thin layers of materials or bioactive molecules. PEGylation creates a "stealth" effect, reducing opsonization and extending circulation half-life [23]. | Bioactivity of immobilized molecules (e.g., peptides, antibodies) can depend on orientation and density. |
| Biofunctionalization | Immobilization of peptides (RGD), proteins, growth factors (VEGF, BMP-2) [25] | Confers specific bioactivity to direct cell behavior (e.g., adhesion, differentiation). RGD peptides promote integrin-mediated cell attachment. | Requires covalent chemistry (EDC/NHS) or affinity-based systems (biotin-streptavidin). Stability and presentation are critical. |
Comparative Toxicity: Inorganic vs. Organic Nanoparticles
The core material of a nanoparticle—whether inorganic or organic—imparts fundamental differences in its toxicity profile and mechanisms. Understanding these differences is essential for selecting the appropriate nanoplatform for a given biomedical application.
Toxicity Mechanisms and Influencing Parameters
Table 3: Comparative Toxicity Profiles of Inorganic vs. Organic Nanoparticles
| Parameter | Inorganic Nanoparticles | Organic Nanoparticles |
|---|---|---|
| Primary Materials | Metals (Ag, Au), Metal Oxides (TiO₂, ZnO), Quantum Dots, Silica [26] [5]. | Polymeric NPs (PLGA), Lipids, Dendrimers, Conjugated Polymer NPs (Pdots) [5] [23]. |
| Dominant Toxicity Mechanisms | - Ion release (e.g., Ag⁺, Zn²⁺) [5].- Generation of Reactive Oxygen Species (ROS) [5].- Direct membrane damage and organelle interaction. | - Incompatible or degradable material [23].- Interaction-based toxicity due to small size and large surface area [23].- Elicitation of adverse immune responses. |
| Key Structural Parameters Affecting Toxicity | Size, shape, crystal structure, agglomeration state, dissolution rate, surface charge, and chemical composition [5]. | Molecular weight, polymer composition, degradation profile, surface charge, and hydrophobicity [23]. |
| Surface Modification Impact | Crucial for mitigating toxicity. Coating with silica, polymers (PEG), or biomolecules (albumin) can reduce ion leaching and ROS generation [27] [28]. | Surface decoration is key to improving biocompatibility. PEGylation prevents protein adsorption; targeting ligands reduce off-target effects and required dose [23]. |
| Experimental Evidence | Metal/Metal Oxide NPs (e.g., Ag, ZnO) often show higher toxicity compared to their ionic counterparts, linked to particle-specific effects and ROS [5] [29]. | Systematic study on Pdots showed Pdots-NH₂ (cationic) had higher cytotoxicity and lower stability than anionic Pdots-COOH or Pdots-SH [24]. |
Experimental Data from Surface-Modified Pdots
A systematic investigation into semiconducting polymer nanoparticles (Pdots) with different surface modifications provides quantitative data on how functional groups influence properties and biocompatibility.
Table 4: Experimental Data for Surface-Functionalized Pdots [24]
| Pdot Type | Zeta Potential (mV) | PDI (Stability Indicator) | Cell Viability (at 60 μg/mL) | In Vivo Circulation |
|---|---|---|---|---|
| Pdots@COOH | -18.0 | Low (~0.1) | ~90% (CaSki, 4T1, BEAS-2B) | Superior |
| Pdots@SH | -18.0 | Low (~0.1) | ~90% (CaSki, 4T1, BEAS-2B) | Superior |
| Bare Pdots | -16.3 | Low (~0.1) | ~90% (CaSki, 4T1, BEAS-2B) | Good |
| Pdots@NH₂ | +3.7 | High (>0.2) | ~80% (CaSki, 4T1, BEAS-2B) | Poor |
Essential Research Reagent Solutions
For researchers designing experiments to evaluate surface chemistry and biocompatibility, the following toolkit is essential.
Table 5: Research Reagent Solutions for Surface and Biocompatibility Studies
| Reagent / Material | Function in Research | Application Example |
|---|---|---|
| Aminosilanes (e.g., APTES) | Introduces primary amine (-NH₂) groups onto silica and metal oxide surfaces for further bioconjugation [27]. | Creating positively charged surfaces to study the effect of charge on protein adsorption and cell adhesion. |
| Thio-Carboxylic Acids | Bifunctional crosslinker for noble metal NPs (Au, Ag); thiol group binds metal, carboxyl group allows ligand attachment [27] [28]. | Functionalizing gold nanoparticles with carboxylic acids for covalent coupling to antibodies or peptides. |
| Polyethylene Glycol (PEG) | "Stealth" polymer; creates a hydrophilic, steric barrier that reduces protein adsorption (opsonization) and immune clearance [23]. | PEGylating liposomal doxorubicin (Doxil) to prolong circulation half-life and enhance tumor accumulation via EPR. |
| DSPE-PEG-R Polymers | Amphiphilic polymers for nanoparticle functionalization; DSPE anchors in lipid membranes, PEG provides a spacer, R (e.g., -COOH, -NH₂) is the functional terminal group [24]. | Synthesizing surface-functionalized Pdots or liposomes with specific targeting ligands via carboxyl or amine chemistry. |
| EDC / NHS Chemistry | Zero-length crosslinkers for catalyzing covalent bond formation between carboxyl and amine groups. | Immobilizing RGD peptides on carboxyl-functionalized surfaces to promote specific integrin-mediated cell adhesion. |
Detailed Experimental Protocols
Protocol: Assessing Conformational Changes of Adsorbed Fibrinogen
This protocol is fundamental for evaluating the bioactivity of a material surface based on its interaction with a key blood protein [22].
- Surface Preparation: Create model surfaces with defined chemistry (e.g., using SAMs on gold or plasma-treated polymers). Characterize surface properties (wettability, charge) via contact angle goniometry and zeta potential.
- Protein Adsorption: Incubate surfaces with a solution of purified human fibrinogen (e.g., 1 mg/mL in PBS, pH 7.4) for a set period (e.g., 1-4 hours) at 37°C.
- SDS Elution Resistance Assay:
- After incubation, gently wash the surfaces with buffer to remove non-adherent protein.
- Treat the surfaces with a 1% SDS solution (a strong ionic detergent) for 30 minutes at room temperature.
- Collect the eluted proteins and quantify the remaining, tightly bound fibrinogen on the surface using a technique like scanning angle reflectometry or by staining and eluting for spectrophotometric measurement.
- Data Interpretation: A higher percentage of SDS-resistant fibrinogen indicates stronger, more denatured protein adhesion, which is correlated with increased inflammatory potential [22].
Protocol: Evaluating Cytotoxicity of Surface-Modified Nanoparticles (CCK-8 Assay)
This standard colorimetric assay measures cell metabolic activity as an indicator of cytotoxicity [24].
- Cell Seeding: Seed appropriate cell lines (e.g., cancer cell lines like 4T1 or primary cells relevant to the application) in a 96-well plate at a density of ~5,000-10,000 cells/well. Culture for 24 hours to allow cell attachment.
- Nanoparticle Exposure: Prepare a dilution series of the surface-modified nanoparticles (e.g., 0, 10, 20, 40, 60 μg/mL) in cell culture medium. Replace the medium in the wells with the nanoparticle-containing medium. Include wells with medium only (blank) and cells with medium only (control).
- Incubation: Incubate the plate for 24-48 hours at 37°C and 5% CO₂.
- Viability Measurement:
- Add 10 μL of CCK-8 reagent to each well.
- Incubate the plate for 1-4 hours at 37°C.
- Measure the absorbance at 450 nm using a microplate reader.
- Data Analysis: Calculate cell viability as a percentage: (Abssample - Absblank) / (Abscontrol - Absblank) * 100%. Compare the dose-response curves for different surface modifications.
The experimental workflow for a comprehensive biocompatibility assessment, from surface creation to in vitro and in vivo evaluation, is summarized below.
Assessing the Risk: Advanced Methodologies for Nanotoxicity Evaluation
In the field of nanotoxicology, particularly in the comparative analysis of inorganic versus organic nanoparticles, robust in vitro assessment models are indispensable for early safety screening. These models provide critical insights into biological interactions while offering advantages of reduced cost, time, and ethical concerns compared to in vivo studies. The reliability of drug development and nanomaterial safety assessment heavily depends on accurate prediction of toxicological endpoints, including effects on cellular proliferation, programmed cell death (apoptosis), oxidative stress balance, and genetic integrity (genotoxicity) [30]. Current challenges in the field include bridging the significant gap between simplified in vitro systems and complex clinical outcomes, which often contributes to drug approval failures [30]. This guide objectively compares the performance of various in vitro assessment methodologies, providing researchers with experimental data and protocols to enhance their toxicology screening strategies for nanoparticle safety profiling.
Comparative Performance of In Vitro Assays
Key Assay Types and Their Applications
The following table summarizes the primary assay categories used in nanoparticle toxicity assessment, their measurement principles, and key advantages and limitations.
Table 1: Overview of Major In Vitro Toxicity Assessment Assays
| Assay Category | Toxicity Endpoint | Measurement Principle | Key Advantages | Common Limitations |
|---|---|---|---|---|
| Proliferation Assays | Cell viability, growth rate, metabolic activity | Measures metabolic markers (MTT, XTT, WST), ATP content, or DNA synthesis | High-throughput capability, quantitative, cost-effective | May not distinguish between cytostasis and cytotoxicity; can be influenced by nanoparticle interference |
| Apoptosis Assays | Programmed cell death | Detects phosphatidylserine externalization (Annexin V), caspase activation, DNA fragmentation | Distinguishes apoptosis from necrosis, provides mechanistic insight | Requires multiple assays to confirm apoptotic pathway; early-stage detection challenging |
| Oxidative Stress Assays | Reactive oxygen species (ROS), antioxidant depletion | Measures ROS (DCFH-DA), antioxidant levels (GSH), lipid peroxidation (MDA) | Early indicator of toxicity, mechanistic relevance | ROS signals can be transient; assay can be confounded by auto-oxidation |
| Genotoxicity Assays | DNA damage, mutations, chromosomal aberrations | Detects DNA strand breaks (Comet), chromosomal damage (Micronucleus), mutation induction (Ames) | Direct measurement of genetic damage, high predictive value for carcinogenicity | Some assays require dividing cells; may need multiple tests for comprehensive assessment |
Quantitative Performance Metrics for Assay Selection
Selecting appropriate assays requires understanding key performance metrics that indicate reliability and suitability for screening. The following table outlines critical parameters for assay validation and comparison.
Table 2: Key Performance Metrics for In Vitro Toxicity Assays
| Performance Metric | Definition | Interpretation | Optimal Range for Screening |
|---|---|---|---|
| EC50/IC50 | Concentration producing half-maximal effect/response | Lower values indicate greater potency of a toxic compound | Compound-dependent; used for ranking toxicity potency [31] |
| Signal-to-Background (S/B) | Ratio of test compound signal to untreated control signal | Higher ratios indicate stronger assay response and robustness | High S/B desirable; specific thresholds vary by assay type [31] |
| Z'-Factor (Z') | Statistical parameter assessing assay quality and robustness | Incorporates both signal dynamic range and data variation | 0.5-1.0: Excellent to ideal; <0.5: Poor quality, unsuitable for screening [31] |
| Toxicity Separation Index (TSI) | Measures how well a test differentiates toxic from non-toxic compounds | Continuous number where 1.0 indicates perfect separation | >0.5 indicates predictive capability; closer to 1.0 is superior [32] |
| Toxicity Estimation Index (TEI) | Indicates how well toxic blood concentrations are estimated by in vitro alerts | Higher values indicate better in vitro-in vivo correlation | Improved by using lower effect concentrations (e.g., EC10) and combining endpoints [32] |
Advanced assay systems like the ToxTracker platform exemplify the integration of multiple endpoints, employing six GFP reporter cell lines to discriminate between different types of biological reactivity including DNA damage, oxidative stress, unfolded protein response, and p53-dependent stress [33]. This approach demonstrates outstanding sensitivity and specificity in validation studies using the ECVAM-recommended compound library [33].
Experimental Protocols for Key Assays
Integrated Oxidative Stress and Genotoxicity Assessment
Principle: This protocol simultaneously evaluates reactive oxygen species (ROS) generation and genotoxic potential of nanoparticles in mammalian cells, providing correlated endpoints for mechanistic toxicology.
Materials and Reagents:
- Cell line: Mouse embryonic stem (mES) cells or human cell lines (A549, HepG2, SH-SY5Y) depending on target tissue [34] [33]
- Nanoparticles: Test materials (inorganic: e.g., SiO2, Ag, TiO2; organic: e.g., polymeric, lipid-based)
- ROS detection: DCFH-DA dye (10 µM working concentration)
- Lysis buffer: RIPA buffer with protease inhibitors
- Antioxidant enzymes: SOD, CAT, GPx activity assay kits
- DNA damage markers: γH2AX immunofluorescence or Comet assay reagents
- Culture medium: Appropriate complete medium for selected cell line
- Equipment: Microplate reader, fluorescence microscope, flow cytometer
Procedure:
- Cell Culture and Exposure:
- Seed cells in 96-well plates (ROS, viability) and chamber slides (genotoxicity) at optimal density (e.g., 1×10⁴ cells/well)
- Incubate for 24 hours to allow attachment
- Prepare nanoparticle suspensions in serum-free medium with sonication to prevent aggregation
- Expose cells to serial nanoparticle concentrations (e.g., 1-200 µg/mL) for 4-24 hours
- Include positive controls: H2O2 (200 µM, 1h) for ROS, etoposide (25 µM, 24h) for genotoxicity
ROS Measurement:
- After exposure, wash cells with PBS
- Load with DCFH-DA (10 µM) in serum-free medium
- Incubate 30 minutes at 37°C in dark
- Wash with PBS and measure fluorescence (Ex/Em: 485/535 nm)
- Calculate fold increase relative to untreated control
Antioxidant Response Analysis:
- Lysate cells after treatment
- Measure antioxidant enzyme activities:
- Superoxide dismutase (SOD) via inhibition of cytochrome C reduction
- Catalase (CAT) via H2O2 decomposition at 240 nm
- Glutathione peroxidase (GPx) via NADPH oxidation at 340 nm
Genotoxicity Assessment:
- For γH2AX foci:
- Fix cells with 4% paraformaldehyde for 15 minutes
- Permeabilize with 0.5% Triton X-100 for 10 minutes
- Block with 5% BSA for 1 hour
- Incubate with anti-γH2AX primary antibody (1:1000) overnight at 4°C
- Incubate with fluorescent secondary antibody (1:2000) for 1 hour
- Counterstain with DAPI and visualize via fluorescence microscopy
- Count foci per nucleus (>10 foci/nucleus considered positive)
- For Comet assay:
- Embed cells in low-melting-point agarose on slides
- Lyse overnight in high-salt, detergent-based buffer
- Perform electrophoresis under alkaline conditions (pH>13)
- Stain with SYBR Gold and analyze tail moment using image analysis software
- For γH2AX foci:
Data Analysis:
- Determine EC50 values for ROS induction using non-linear regression
- Calculate correlation coefficients between ROS levels and DNA damage markers
- Establish concentration-response relationships for each endpoint
- Compare potency between inorganic and organic nanoparticles using TSI/TEI metrics [32]
Advanced Multiplexed Toxicity Screening (ToxTracker Assay)
Principle: This stem cell-based reporter assay simultaneously monitors activation of multiple specific stress response pathways, providing mechanistic insight into nanoparticle reactivity [33].
Materials and Reagents:
- ToxTracker mouse embryonic stem cell reporter lines: BSCL2-GFP (DNA damage), SRXN1-GFP (oxidative stress), additional reporters for UPR, p53 pathway [33]
- Nanoparticle suspensions in serum-free medium
- BRL-conditioned mES cell medium
- Gelatin-coated tissue culture plates
- Flow cytometry equipment for GFP quantification
Procedure:
- Cell Culture and Exposure:
- Maintain ToxTracker reporter mES cells in knockout medium with LIF on feeder layers
- For experiments, seed cells on gelatin-coated plates in BRL-conditioned medium without feeders
- Allow attachment for 24 hours
- Expose cells to nanoparticle suspensions for 24 hours
- Include appropriate controls and reference compounds
GFP Reporter Measurement:
- Harvest cells after exposure using trypsinization
- Resuspend in PBS containing 2% FCS
- Analyze GFP expression using flow cytometry
- Score as positive if GFP intensity exceeds threshold (2-3-fold above background)
Data Interpretation:
- Specific GFP expression patterns indicate different types of cellular damage:
- BSCL2-GFP activation: DNA replication stress and ATR/Chk1 pathway activation
- SRXN1-GFP activation: Oxidative stress and Nrf2 pathway activation
- Additional reporters: Unfolded protein response, p53 pathway activation
- Profile nanoparticles based on their activation of specific stress pathways
- Specific GFP expression patterns indicate different types of cellular damage:
Validation: This assay has demonstrated outstanding sensitivity (96%) and specificity (89%) using the ECVAM-recommended compound library, effectively discriminating between different mechanisms of toxicity [33].
Signaling Pathways in Nanoparticle-Induced Toxicity
The following diagram illustrates key interconnected signaling pathways activated by nanoparticle exposure in mammalian cells, highlighting points of intervention for assay detection.
Figure 1: Key Signaling Pathways in Nanoparticle Toxicity. This diagram illustrates the interconnected cellular signaling pathways activated by nanoparticle exposure, from initial cellular uptake to final toxicity outcomes. The pathways highlight how different assay endpoints detect specific events in the toxicity cascade.
Experimental Workflow for Comprehensive Assessment
The following diagram outlines a systematic workflow for conducting a comprehensive in vitro toxicity assessment of nanoparticles, integrating multiple endpoints.
Figure 2: Comprehensive In Vitro Toxicity Assessment Workflow. This workflow outlines the key steps in a systematic approach to evaluating nanoparticle toxicity, from initial characterization through multiple endpoint assessments to integrated data analysis.
Research Reagent Solutions for Toxicity Assessment
Table 3: Essential Research Reagents for In Vitro Toxicity Assessment
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Cell Line Models | Mouse embryonic stem (mES) cells, A549 (lung), HepG2 (liver), SH-SY5Y (neural) [34] [33] | Provide biologically relevant systems for toxicity screening | Stem cells offer pathway proficiency; differentiated cells provide tissue-specific responses |
| Viability/Proliferation Assay Kits | MTT, XTT, WST-1, ATP Lite | Quantify metabolic activity and cell number as surrogates for proliferation | Potential NP interference must be controlled; ATP assays often most reliable |
| Apoptosis Detection Kits | Annexin V/PI, Caspase-Glo, TUNEL | Detect programmed cell death via membrane changes and DNA fragmentation | Multiparametric approaches distinguish apoptosis from necrosis |
| Oxidative Stress Probes | DCFH-DA, MitoSOX, DHE, H2DCFDA | Measure reactive oxygen species generation in different compartments | DCFH-DA detects general ROS; MitoSOX specific for mitochondrial superoxide |
| Antioxidant Assays | GSH/GSSG ratio, SOD, CAT, GPx activity kits | Quantify cellular antioxidant defense capacity | GSH depletion often early indicator of oxidative stress |
| Genotoxicity Assays | Comet, Micronucleus, γH2AX, Ames | Detect DNA damage, chromosomal aberrations, mutations | Comet detects strand breaks; γH2AX indicates double-strand breaks |
| Advanced Reporter Systems | ToxTracker assay (6 GFP reporters) [33] | Multiplexed assessment of specific stress pathway activation | Discriminates between mechanisms of toxicity; high predictive value |
Comparative Data on Nanoparticle Toxicity
Physicochemical Properties Influencing Toxicity
The toxicity of nanoparticles, particularly inorganic variants, is heavily influenced by their physicochemical properties, which should be characterized prior to toxicity assessment.
Table 4: Nanoparticle Properties Affecting Toxicological Profiles
| Property | Toxicity Influence | Experimental Evidence |
|---|---|---|
| Size | Smaller nanoparticles typically show higher toxicity due to increased surface area and cellular uptake [35] | 10nm AgNP caused acute toxicity in mice not seen with 60nm or 100nm; 10-30nm AuNP crossed nuclear membrane, 60nm accumulated in spleen [35] |
| Shape | Cellular uptake and toxicity vary significantly with shape [35] | Spherical NPs internalized more than rods; star-shaped AuNP most cytotoxic; needle-shaped silica more toxic than spherical [35] |
| Surface Coating | Can either mitigate or exacerbate toxicity [35] | Silica-coated iron oxide NPs showed reduced alteration of iron homeostasis and oxidative stress compared to non-passivated NPs [35] |
| Aspect Ratio | High aspect ratio associated with fiber-like pathogenicity [35] | Carbon nanotubes with high aspect ratio caused granulomas and protein exudation in rat lungs [35] |
| Crystallinity | Different crystalline structures of same composition show varying toxicity [35] | Needle-shaped HCPT nanoparticles more potent in apoptotic response despite similar cellular uptake as prismatic forms [35] |
Comparison of Inorganic Nanoparticle Toxicity Profiles
Table 5: Comparative Toxicity Profiles of Selected Inorganic Nanoparticles
| Nanoparticle Type | Key Toxicological Mechanisms | Sensitive Cell Types/Assays | Potency Range (Approximate IC50) |
|---|---|---|---|
| Silica (SiNP) | ROS generation, NLRP3 inflammasome activation, lysosomal destabilization, mitochondrial dysfunction [36] | Macrophages (inflammation), lung epithelial cells (ROS), neural cells (oxidative stress) [36] | Varies by size/surface: 10-100 μg/mL (cellular viability) [36] |
| Silver (AgNP) | Strong oxidative stress, mitochondrial dysfunction, DNA damage, inflammation [35] | BALB/c mice (acute toxicity), various mammalian cell lines (ROS, genotoxicity) | Size-dependent: 10nm much more toxic than 60-100nm [35] |
| Gold (AuNP) | DNA damage (small sizes), organ accumulation varies with size [35] | Fetal osteoblast, osteosarcoma, pancreatic cells (shape-dependent toxicity) | Shape-dependent: star-shaped > rods > spheres [35] |
| Iron Oxide (SPION) | Oxidative stress, time-dependent cytotoxicity, ROS production [37] | Caco-2 intestinal cells, potential for neural toxicity | Varies by coating: ~50-200 μg/mL (cellular viability) [37] |
The emerging field of "nanotoxicomics" integrates advanced omics technologies (transcriptomics, proteomics, metabolomics) with traditional toxicology, enabling multilevel analysis of nanoparticle effects and supporting more accurate extrapolation from in vitro to in vivo systems [34]. This approach has identified specific biomarker patterns, including differential expression of genes related to oxidative stress (SOD1), inflammation (IL-6), and DNA damage (TP53), along with corresponding protein and metabolite alterations [34].
When comparing inorganic versus organic nanoparticles, inorganic particles often demonstrate more pronounced toxicity due to their potential for redox activity, metal ion release, and surface reactivity. However, surface functionalization can significantly modulate this toxicity, sometimes converting noxious particles to relatively nontoxic forms [35]. The comprehensive assessment approach outlined in this guide provides researchers with methodologies to systematically evaluate these differences and develop safer nanoparticle designs for biomedical applications.
The expanding application of nanotechnology in biomedicine necessitates a thorough understanding of the potential adverse effects of nanoparticles (NPs) on human health. In vivo toxicity assessment using animal models is a critical component of this evaluation, providing insights into the organ-specific toxicological endpoints that arise from exposure to these materials. This guide systematically compares the toxicity profiles of organic and inorganic nanoparticles, framing the analysis within the broader context of ongoing research into their distinct biological interactions. For researchers and drug development professionals, this synthesis of current data and methodologies provides a foundation for informed material selection and rigorous safety testing. The fundamental differences in the physicochemical properties of these two classes of nanoparticles—such as their biodegradability, chemical composition, and catalytic activity—underpin their divergent behaviors and toxicities in biological systems [4] [38].
Comparative Toxicity Profiles of Organic and Inorganic Nanoparticles
The toxicity of nanoparticles is governed by a complex interplay of their physicochemical characteristics and the biological environment. The table below summarizes the core differences in the properties and toxicological mechanisms of organic and inorganic nanoparticles, which lead to distinct outcomes in vivo.
Table 1: Fundamental Properties and Toxicity Mechanisms of Organic vs. Inorganic Nanoparticles
| Characteristic | Organic Nanoparticles | Inorganic Nanoparticles |
|---|---|---|
| Composition | Lipids, polymers, carbohydrates [4] | Metals (e.g., Ag, Au), metal oxides (e.g., TiO₂, ZnO, SiO₂) [4] [39] |
| Biodegradability | Typically biodegradable and biocompatible [4] | Often poorly soluble and persistent in biological systems [40] [38] |
| Primary Toxicity Mechanisms | Generally lower inherent cytotoxicity; toxicity often linked to encapsulated drug or immune reactions [4] [40] | Generation of Reactive Oxygen Species (ROS), oxidative stress, ion release, inflammasome activation [39] [36] [38] |
| Key Influencing Factors | Surface charge, lipid composition, polymer type [4] | Size, shape, crystal structure, surface chemistry, solubility [40] [39] [38] |
| Long-Term Fate | Metabolized and cleared from the body [4] | Potential for long-term accumulation in organs like the liver and spleen [40] |
A central theme in inorganic nanoparticle toxicity is their ability to induce ferroptosis, an iron-dependent form of regulated cell death. This process is triggered by a cascade involving iron dysregulation and profound lipid peroxidation [41]. Furthermore, the persistence of some inorganic nanoparticles, such as certain metal oxides, raises concerns about chronic exposure and bioaccumulation that are less pronounced for their biodegradable organic counterparts [40].
Organ-Specific Toxicological Endpoints in Animal Models
In vivo studies across various animal models have revealed that nanoparticle exposure can lead to a spectrum of organ-specific adverse effects. The following table synthesizes key findings from the literature on major target organs.
Table 2: Organ-Specific Toxicological Endpoints Following Nanoparticle Exposure in Animal Models
| Target Organ | Documented Effects from Inorganic NPs | Documented Effects from Organic NPs | Common Assessment Endpoints |
|---|---|---|---|
| Liver | Oxidative stress, inflammation, accumulation, pigmentation of villi, liver damage (AgNPs) [39] [42] | Generally lower toxicity, but accumulation can affect organ function [40] | Histopathology, levels of ALT/AST enzymes, oxidative stress markers (e.g., ROS, MDA), tissue metal accumulation [42] [43] |
| Kidneys | Kidney toxicity (ZnO NPs, AgNPs) [42] | Reduced toxicity compared to inorganic NPs [4] | Histopathology, biomarkers (creatinine, BUN), accumulation levels [42] |
| Lungs | Lung inflammation, oxidative stress, damage, pulmonary injury and fibrosis (SiNPs) [40] [36] | Limited data, but generally considered less inflammatory than inorganic NPs | Bronchoalveolar lavage (BAL) fluid analysis (inflammatory cells, cytokines), histopathology [40] [39] |
| Brain | Potential to cross BBB; neurotoxicity, oxidative stress, protein aggregation (SiNPs) [36] | Can be engineered to cross BBB for drug delivery, with potential for unintended toxicity [40] | Behavioral assays, markers of oxidative stress in neural tissue, histopathological analysis of brain regions [36] |
| Gastrointestinal Tract | Lymphocyte infiltration, disruption of intestinal barrier, altered gut microbiota (AgNPs) [42] | Can improve drug permeation and protect drugs from stomach acidity [4] | Histology of intestinal villi, analysis of gut microbiome, markers of intestinal inflammation [42] |
| Cardiovascular System | Cardiovascular inflammation, heart problems [40] | Reduced cardiotoxicity of encapsulated drugs (e.g., Doxil) [4] | Heart rate variability, biomarkers of cardiac injury (e.g., troponin), histopathology [40] |
| Immune System | Activation of NLRP3 inflammasome, release of pro-inflammatory cytokines (IL-1β, IL-6, TNF-α), persistent immune modulation [39] [36] | Can be designed to evade immune recognition (e.g., PEGylation) [4] [40] | Cytokine profiling, immunophenotyping of immune cells, histology of lymphoid tissues [39] |
The table illustrates that inorganic nanoparticles, particularly metal and metal oxide NPs, are frequently associated with more severe organ-level toxicity, primarily driven by oxidative stress and inflammation. For instance, silver nanoparticles (AgNPs) have been shown to accumulate in the liver and kidneys, causing oxidative stress and histological damage [42]. Silica nanoparticles (SiNPs) can induce pulmonary fibrosis and have the potential to cross the blood-brain barrier, leading to neurotoxic effects [36]. In contrast, organic nanoparticles like liposomes are notable for their ability to reduce the toxicity of encapsulated drugs, as demonstrated by the significantly reduced cardiotoxicity of Doxil (PEGylated liposomal doxorubicin) compared to the free drug [4].
Experimental Protocols for In Vivo Assessment
A standardized approach to in vivo toxicity testing is crucial for generating reliable and comparable data. The following workflow outlines a typical sub-acute exposure study in a rodent model, which is commonly used for initial safety assessment.
Diagram 1: In Vivo Toxicity Study Workflow.
Detailed Methodologies
The general workflow is operationalized through the following detailed protocols, which are critical for assessing the toxicological endpoints associated with nanoparticle exposure:
Animal Model Selection and Grouping: The study typically employs rodents like Sprague-Dawley rats or C57BL/6 mice. Following a period of acclimatization, animals are randomly assigned to groups: a vehicle control group (e.g., receiving saline or the suspension medium), one or more treatment groups receiving different doses of the nanoparticle, and sometimes a benchmark control group. Group sizes are determined to ensure statistical power, often n=10 or more [42] [43].
Dosing Regimen and Administration: Doses are selected based on preliminary range-finding studies or existing literature. A common route is oral gavage for dietary or consumer product exposure. For a 28-day sub-acute study, daily administration is standard. Doses may be expressed as mg per kg body weight per day. For example, studies have used doses of ZnO NPs ranging from 30 to 500 mg kg⁻¹ diet in fish, and AgNPs at 250 mg kg⁻¹ body weight in rats [42] [43].
In-life Monitoring and Clinical Observations: Animals are monitored daily for mortality and clinical signs of toxicity, which include changes in behavior, posture, activity level, and fur condition. Body weight and food/water consumption are measured and recorded at regular intervals (e.g., twice weekly) as indicators of systemic health [42].
Terminal Procedures and Sample Collection: At the end of the exposure period, animals are humanely euthanized. Blood is collected via cardiac puncture for hematological and clinical chemistry analysis. Key organs (e.g., liver, kidneys, spleen, lungs, brain, and heart) are immediately excised, weighed, and processed for further analysis. The relative organ weight (organ-to-body weight ratio) is a sensitive indicator of toxicity [42] [43].
Histopathological Examination: Sections of collected organs are fixed, embedded in paraffin, sectioned, and stained with Hematoxylin and Eosin (H&E). A pathologist then examines these sections under a microscope in a blinded manner to identify cellular damage, necrosis, inflammatory cell infiltration, fibrosis, and other pathological lesions [36] [42].
Biochemical and Molecular Analysis:
- Oxidative Stress Markers: Tissues are homogenized, and assays are performed to measure lipid peroxidation (e.g., Malondialdehyde (MDA) levels), activities of antioxidant enzymes like Superoxide Dismutase (SOD), Catalase (CAT), and levels of reduced Glutathione (GSH) [38] [43].
- Inflammation Markers: Serum or tissue homogenates are analyzed using ELISA or multiplex immunoassays to quantify pro-inflammatory cytokines such as IL-1β, IL-6, IL-8, and TNF-α [39] [36].
- Genotoxicity Assays: Tissues like blood or bone marrow can be used for tests like the micronucleus assay or comet assay to detect DNA strand breaks and chromosomal damage [39].
Key Toxicity Signaling Pathways
The toxicity of inorganic nanoparticles is often mediated through specific, interconnected cellular pathways. The diagram below illustrates the two major mechanisms: oxidative stress and inflammasome activation.
Diagram 2: Key Toxicity Pathways of Inorganic Nanoparticles.
The Oxidative Stress Pathway is initiated when nanoparticles are taken up by cells and localize in organelles like the mitochondria, leading to the direct or indirect generation of Reactive Oxygen Species (ROS). This, coupled with the depletion of antioxidants, creates a state of oxidative stress that damages lipids, proteins, and DNA, ultimately triggering cell death via apoptosis or ferroptosis [41] [39] [38]. Concurrently, the Inflammasome Activation Pathway begins with the phagocytosis of nanoparticles and their accumulation in lysosomes, causing lysosomal membrane permeabilization and the release of cathepsin B. This event activates the NLRP3 inflammasome, which in turn activates caspase-1, leading to the maturation and secretion of potent pro-inflammatory cytokines IL-1β and IL-18 [39] [36]. These two pathways are interconnected, as oxidative stress can potentiate and enhance inflammasome activation.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues critical reagents and materials required for conducting the in vivo and ex vivo assessments described in this guide.
Table 3: Essential Research Reagents for Nanoparticle Toxicity Assessment
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Animal Models | In vivo testing of biodistribution, toxicity, and efficacy. | Sprague-Dawley Rats, C57BL/6 Mice, Common Carp (Cyprinus carpio) [42] [43] |
| Standard Nanoparticles | Reference materials for benchmarking and comparative toxicity studies. | TiO₂ (anatase/rutile), ZnO, AgNPs, SiO₂ (amorphous), PEGylated liposomes (e.g., Doxil) [4] [39] [42] |
| ELISA Kits | Quantification of protein biomarkers and cytokines in serum and tissue homogenates. | Kits for IL-1β, IL-6, TNF-α, Caspase-1 [39] [36] |
| Antibody Panels | Immunohistochemistry and flow cytometry for identifying cell types and protein expression. | Antibodies for immune cell markers (CD4, CD8, CD11b), oxidative stress markers (e.g., 4-HNE) |
| Oxidative Stress Assay Kits | Measurement of oxidative damage and antioxidant capacity. | Lipid Peroxidation (MDA) Assay Kits, SOD Activity Assay Kits, GSH/GSSG Assay Kits [38] [43] |
| Histology Supplies | Tissue processing, staining, and pathological examination. | Formalin, Paraffin Embedding Media, H&E Staining Kits, Antibodies for specific protein targets (IHC) [42] |
| Genotoxicity Assay Kits | Assessment of DNA damage. | Comet Assay Kit, Micronucleus Assay Reagents [39] |
The rapid expansion of nanotechnology has necessitated the development of sophisticated toxicological assessment methods capable of evaluating the safety profiles of diverse nanoparticles (NPs). Traditional toxicity testing, reliant on animal studies and apical endpoints, is increasingly misaligned with the need for human-relevant, high-throughput safety data that can keep pace with innovation [44] [45]. This comparison guide objectively evaluates two transformative approaches revolutionizing nanotoxicology: high-throughput screening (HTS) and omics-based methodologies. For researchers investigating the fundamental thesis comparing inorganic versus organic nanoparticle toxicity profiles, understanding the capabilities, applications, and limitations of these technological paradigms is essential for designing robust, predictive safety assessments.
High-throughput screening employs automated, miniaturized assays to rapidly test thousands of chemical compounds or nanomaterials for biological activity [46]. The global HTS market, valued to increase by USD 18.8 billion from 2024 to 2029 at a CAGR of 10.6%, reflects its growing adoption in pharmaceutical and toxicological screening [47]. Concurrently, omics technologies (transcriptomics, metabolomics, proteomics) provide deep molecular characterization of toxicity mechanisms by measuring system-wide molecular changes following NP exposure [44] [45]. Both approaches represent pillars of Next-Generation Risk Assessment (NGRA), which integrates emerging tools to support more human-relevant safety decisions while reducing animal testing [44].
This guide provides a systematic comparison of these platforms through standardized data presentation, experimental protocols, and visualization tools specifically contextualized for inorganic and organic nanoparticle toxicity profiling.
Technology Comparison: Capabilities and Applications
Technical Specifications and Performance Metrics
Table 1: Core Technology Characteristics and Applications
| Feature | High-Throughput Screening (HTS) | Omics-Based Approaches |
|---|---|---|
| Throughput Capacity | 10,000-100,000 compounds per day (HTS); >300,000 (uHTS) [46] | Moderate throughput (typically 10s-100s of samples per study) [44] |
| Primary Applications in Nanotoxicology | Primary screening, hit identification, toxicological triage [48] [46] | Mechanism elucidation, biomarker discovery, molecular point of departure (POD) derivation [44] [45] |
| Key Detectable Endpoints | Cell viability, enzymatic activity, receptor binding, phenotypic changes [46] | Genome-wide expression changes (transcriptomics), metabolic shifts (metabolomics), protein abundance/ modification (proteomics) [44] |
| Data Output Type | Quantitative activity metrics (IC50, EC50), fluorescence/luminescence signals [46] | Multidimensional molecular profiles (gene lists, pathway alterations, molecular signatures) [44] [45] |
| Automation Compatibility | Fully automated with robotic liquid handling, plate readers, and automated incubators [47] [48] | Variable; RNA-seq library prep increasingly automated, data analysis pipeline automation essential [45] |
| Regulatory Adoption Status | Established in pharmaceutical screening; growing in toxicology (Tox21) [46] | Emerging (e.g., EPA's Transcriptomic Assessment Product (ETAP) program) [44] [45] |
Performance in Nanotoxicity Testing
Table 2: Performance Metrics for Nanoparticle Toxicity Assessment
| Performance Metric | High-Throughput Screening | Omics-Based Approaches |
|---|---|---|
| Sensitivity | Detects ~µM-nM cellular effects; can miss subtle pathway perturbations | Extremely sensitive; detects molecular changes before overt toxicity [44] [45] |
| Physiological Relevance | Moderate (2D cultures) to High (3D organoids, organ-on-chip) [48] | High (when applied to relevant models); provides mechanistic context [44] |
| Cost Per Sample | Low to moderate (after initial capital investment) [47] | Moderate to high (sequencing, mass spectrometry) [45] |
| Time to Results | Rapid (hours to days for screening phase) [46] | Moderate (days to weeks including data processing) [44] |
| False Positive/Negative Rate | Can be significant without proper counter-screens and cheminformatics triage [46] | Lower for mechanistic assessment; dependent on statistical thresholds and bioinformatics [45] |
| Concordance with Traditional Toxicology | Variable; improving with 3D models and complex endpoints [48] | High; molecular PODs typically within 2-3 fold of traditional PODs [44] [45] |
Experimental Protocols for Nanoparticle Toxicity Assessment
High-Throughput Screening Protocol for Nanotoxicity
Protocol Title: Multiparametric Cytotoxicity Screening of Nanoparticles in 2D and 3D Culture Systems
1. Experimental Design and Plate Layout:
- Utilize 384-well microplates for screening efficiency. Include minimum 6 negative control wells (vehicle only) and 6 positive control wells (known cytotoxic compound) per plate [46].
- Test each nanoparticle type in a 8-point concentration series (typically 0.1-100 µg/mL for initial screening) with three technical replicates per concentration.
- Randomize nanoparticle plate placement to minimize positional effects.
2. Sample Preparation:
- Prepare nanoparticle stock suspensions in relevant biological media.
- Sonicate suspensions (e.g., 30-60 minutes in water bath sonicator) immediately before use to minimize aggregation [10].
- Perform characterization of hydrodynamic size and zeta potential in dosing media using dynamic light scattering.
3. Cell Seeding and Treatment:
- Seed cells at optimized density (e.g., 1,000-5,000 cells/well for 384-well format) in appropriate medium.
- For 3D cultures, use specialized plates and allow spheroid formation (typically 24-72 hours) before nanoparticle exposure [48].
- Treat cells with nanoparticle suspensions using automated liquid handlers capable of nanoliter dispensing [48].
4. Endpoint Measurement:
- Cell Viability: Measure using ATP-content based assays (e.g., CellTiter-Glo) after 24-72 hours exposure.
- Oxidative Stress: Quantify reactive oxygen species (ROS) using CM-H2DCFDA dye after 6-24 hours exposure.
- Membrane Integrity: Assess via lactate dehydrogenase (LDH) release assay at 24 hours.
- High-Content Imaging: For phenotypic screening, stain cells with Hoechst (nuclei), Phalloidin (cytoskeleton), and MitoTracker (mitochondria) followed by automated imaging and analysis [48].
5. Data Analysis:
- Normalize raw data to vehicle control (0% effect) and positive control (100% effect).
- Calculate half-maximal inhibitory concentrations (IC50) using four-parameter logistic curve fitting.
- Apply statistical filters (e.g., Z'-factor >0.5) for assay quality assessment [46].
Omics-Based Toxicity Assessment Protocol
Protocol Title: Transcriptomic Point of Departure (tPOD) Derivation for Nanoparticle Risk Assessment
1. In Vivo Study Design:
- Employ 5-28 day repeated dose regimen in rodents (typically 8 or more dose groups) [44] [45].
- Include vehicle control and multiple nanoparticle concentrations spanning expected no-effect to low-effect levels.
- Collect potential target organs (liver, kidney, lung, etc.) for RNA isolation at study termination.
2. Sample Processing and RNA Sequencing:
- Homogenize tissues in TRIzol or similar RNA-stabilizing reagent.
- Isolve total RNA using silica-column based methods with DNase treatment.
- Assess RNA quality (RNA Integrity Number >7.0 required).
- Prepare sequencing libraries using ultra-high-throughput methods (e.g., DRUG-seq, BRB-seq) enabling 3' RNA-seq in 384-well plate format [45].
- Sequence on appropriate platform (e.g., Illumina NovaSeq) to depth of 10-20 million reads per sample.
3. Bioinformatics Analysis:
- Perform quality control (FastQC), alignment (STAR), and gene-level quantification (featureCounts).
- Identify differentially expressed genes (DEGs) using appropriate statistical models (e.g., limma-voom) with FDR <0.05.
- Conduct benchmark dose (BMD) modeling using BMDExpress v3.0 or similar software [44] [45].
- Perform pathway enrichment analysis (Gene Ontology, KEGG) on dose-responsive genes.
4. tPOD Derivation:
- Calculate median BMD for gene ontology biological process sets with at least 3 significant genes.
- Derive tPOD as the lower 95% confidence limit of the lowest median BMD [44].
- Compare tPOD with traditional apical endpoints for concordance assessment.
Signaling Pathways in Nanoparticle Toxicity
The application of omics technologies has elucidated several key molecular pathways through which nanoparticles exert toxic effects. These mechanisms are crucial for understanding differences between inorganic and organic nanoparticle toxicity profiles.
Figure 1: Key Toxicity Pathways of Nanoparticles
Oxidative Stress and Inflammatory Pathways
As visualized in Figure 1, nanoparticle toxicity primarily initiates with cellular internalization, followed by organelle-specific interactions. Inorganic nanoparticles like silica nanoparticles (SiNPs) and metal oxides frequently induce reactive oxygen species (ROS) generation through direct surface reactivity or mitochondrial disruption [10] [36]. This oxidative stress triggers a cascade including DNA damage, lipid peroxidation, and activation of pro-inflammatory pathways [10]. The NLRP3 inflammasome activation represents a crucial inflammatory mechanism, where lysosomal destabilization following nanoparticle uptake releases cathepsin B, promoting IL-1β and IL-18 maturation [36]. These pathways manifest differently between inorganic and organic nanoparticles, with metal-based nanoparticles typically generating more significant ROS through Fenton-like reactions [41].
Novel Cell Death Mechanisms
Ferroptosis, an iron-dependent form of regulated cell death characterized by lethal lipid peroxidation, has emerged as a key toxicity mechanism for certain nanoparticles [41]. Nanoparticles can trigger ferroptosis through iron dysregulation combined with oxidative stress, presenting both toxicity concerns and potential therapeutic applications in oncology. The susceptibility to ferroptosis varies between nanoparticle types, with inorganic iron-containing nanoparticles potentially exhibiting enhanced ferroptosis induction compared to organic counterparts.
Workflow Integration for Comprehensive Assessment
Figure 2: Integrated HTS-Omics Workflow
Figure 2 illustrates a complementary integrated approach where HTS serves as a rapid triaging tool to identify nanoparticles of concern, which subsequently undergo deep mechanistic investigation using omics technologies. This workflow efficiently leverages the throughput advantages of HTS with the mechanistic depth of omics approaches [48] [44]. For instance, HTS can identify nanoparticles causing mitochondrial dysfunction or ROS production, while subsequent transcriptomics can reveal specific pathway perturbations and enable derivation of transcriptomic points of departure (tPODs) for risk assessment [45].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents and Platforms for Implementation
| Category | Specific Products/Platforms | Primary Function in Nanotoxicity Assessment |
|---|---|---|
| HTS Automation | Thermo Fisher Scientific robotic workcells; PerkinElmer liquid handlers | Automated nanoliter-scale dispensing and plate handling for screening thousands of nanoparticle formulations [47] [48] |
| Cell-Based Assay Kits | CellTiter-Glo (Promega); MultiTox-Fluor (Promega); H2DCFDA dye | Multiparametric assessment of cell viability, cytotoxicity, and reactive oxygen species generation [46] |
| Omics Technologies | DRUG-seq/BRB-seq kits (Alithea Genomics); Illumina RNA-seq platforms; BMDExpress software | High-throughput transcriptomic profiling and benchmark dose modeling for molecular point of departure derivation [45] |
| Advanced Cell Models | 3D organoid systems; organ-on-chip devices (Emulate); iPSC-derived cells | Physiologically relevant models for improved human toxicity prediction [48] |
| Data Analysis Platforms | TIBCO Spotfire; Genedata Screener; R/Bioconductor packages | HTS data analysis, visualization, and omics data processing [46] |
| Nanoparticle Characterization | Dynamic light scattering (DLS) systems; nanoparticle tracking analysis (NTA) | Critical physicochemical characterization of nanoparticle size, distribution, and stability in biological media [10] |
High-throughput screening and omics-based approaches offer complementary strengths for elucidating differences in inorganic versus organic nanoparticle toxicity profiles. HTS provides unparalleled throughput for rapid material triaging and hazard identification, while omics technologies deliver deep mechanistic insights and enable quantitative risk assessment through molecular points of departure. The integration of these platforms, as illustrated in the workflows and protocols presented, represents the state-of-the-art in nanotoxicology assessment. For researchers navigating this landscape, strategic selection of appropriate methodologies based on testing phase (discovery vs. mechanistic investigation) and regulatory requirements will maximize the predictive power of toxicity assessments while accelerating the development of safer nanomaterial designs.
The rapid expansion of nanotechnology in biomedical applications has intensified the need for reliable toxicity assessment methods that can accurately predict in vivo outcomes from in vitro data. For researchers and drug development professionals, bridging this correlation gap is particularly critical when evaluating the distinct toxicity profiles of inorganic versus organic nanoparticles. While inorganic nanoparticles like silver and silica offer unique functional properties, their potential mechanisms of toxicity—including oxidative stress, inflammasome activation, and DNA damage—differ significantly from their organic counterparts. Current new approach methodologies (NAMs) aim to provide faster, more cost-effective chemical evaluations while reducing reliance on animal testing, but their utility depends on demonstrating consistent correlation with in vivo results. This comparison guide examines experimental frameworks that successfully benchmark in vitro against in vivo toxicity outcomes, providing researchers with validated protocols and computational tools to enhance predictive accuracy in nanomaterial safety assessment.
Comparative Toxicity Profiles: Inorganic vs. Organic Nanoparticles
Table 1: Fundamental Characteristics Influencing Nanoparticle Toxicity
| Parameter | Inorganic Nanoparticles | Organic Nanoparticles |
|---|---|---|
| Core Composition | Metals (Ag, Au, Fe), metal oxides (SiO₂, TiO₂), ceramics [12] | Polymers, lipids, proteins [12] |
| Primary Toxicity Mechanisms | ROS generation, oxidative stress, mitochondrial dysfunction, DNA damage, inflammasome activation [36] [49] | Differentiated cellular uptake, lipid disruption, polymer degradation products |
| Size Influence | Higher toxicity at smaller sizes due to increased surface area-to-volume ratio [13] | Variable size-toxicity relationship dependent on polymer composition |
| Surface Charge Impact | Zeta potential significantly influences cytotoxicity; higher positive charges often increase toxicity [13] | Surface charge effects moderated by biocompatible coatings |
| Cellular Uptake Efficiency | Generally high uptake potential; can cross biological barriers including BBB [36] | Variable uptake dependent on surface functionalization |
| Environmental Persistence | Typically higher persistence and potential for bioaccumulation | Generally biodegradable with lower persistence |
Table 2: Experimental Benchmarking of Select Nanoparticles
| Nanoparticle Type | In Vitro Model | In Vivo Model | Key Correlated Endpoints | Benchmark Dose Correlation |
|---|---|---|---|---|
| Silver NPs (AgNPs) | Human lung epithelial cells [49] | Not specified in study | Temporal gene expression patterns (ribosomal biogenesis → DNA repair → apoptosis) [49] | Sequential pathway activation conserved across models |
| Silica NPs (SiNPs) | Immortalized cell lines, primary human bronchial epithelial cells at ALI [50] | Mouse respiratory tract [50] | Transcriptomic points of departure (PODs), inflammatory pathways [50] | PODs within an order of magnitude when considering internal concentrations |
| Volatile Organic Compounds | BEAS-2B and primary human bronchial epithelial cells at ALI [50] | Mouse lung and nasal septal tissues [50] | Gene expression changes, oxidative stress responses | Transcriptomic PODs showed similar sensitivity to apical endpoints |
Experimental Protocols for Toxicity Benchmarking
Air-Liquid Interface (ALI) Exposure Systems for Inhalation Toxicity
Protocol Overview: This methodology bridges in vitro and in vivo inhalation toxicity assessment by exposing human airway cells to aerosols at the air-liquid interface, better mimicking physiological conditions compared to traditional submerged cultures [50].
Detailed Methodology:
- Cell Culture: Utilize immortalized human airway cells (e.g., BEAS-2B) and/or differentiated normal primary human bronchial epithelial cells (pHBECs) grown on permeable transwell inserts.
- ALI Exposure: Maintain cells at air-liquid interface for proper differentiation before exposure. Use a novel ALI cell culture exposure system (CCES) with controlled atmosphere.
- Exposure Parameters: Expose cells to six concentrations of test compounds (e.g., VOCs, nanoparticle aerosols) at half-log increments for 2 hours at 37°C with 12.5 mL/min flow rate per insert.
- Post-Exposure Incubation: Return cells to 37°C incubator for 4 hours before assessing cytotoxicity and collecting cell lysates for transcriptomic analysis.
- Endpoint Assessment: Evaluate cell viability, cytotoxicity, and conduct transcriptomic analysis using RNA sequencing to identify differentially expressed genes and biological pathways.
- Parallel In Vivo Validation: Conduct acute exposures in mice using identical test compounds with real-time respiratory monitoring via head-out plethysmography.
Critical Considerations: This protocol demonstrated that despite differences in gene expression profiles between human cells and mouse tissues, benchmark doses derived from the most sensitive biological pathways showed comparability, especially when considering internal concentrations [50].
Temporal Transcriptomics for Dynamic Toxicity Assessment
Protocol Overview: This systems biology approach tracks the evolution of toxicity mechanisms over time, particularly valuable for understanding the sequential pathway activation by inorganic nanoparticles like AgNPs [49].
Detailed Methodology:
- Time-Course Exposure: Expose human lung epithelial cells to test nanoparticles (e.g., AgNPs) and collect samples at multiple time points (1h, 6h, 24h, 48h) to capture dynamic responses.
- Transcriptomic Analysis: Conduct RNA sequencing to identify differentially expressed genes (DEGs) at each time point.
- Bioinformatic Processing: Perform gene ontology (GO) enrichment analysis to identify biological processes affected at different exposure durations.
- Network Analysis: Construct protein-protein interaction (PPI) networks using STRING database to identify hub genes and central pathways.
- Dynamic Modeling: Use CellDesigner for pathway visualization and COPASI for kinetic modeling of gene interactions, estimating rate constants from time-course gene expression data.
- Validation: Compare in vitro predictions with in vivo outcomes focusing on temporal progression of stress responses.
Critical Considerations: This approach revealed temporal evolution in AgNP toxicity mechanisms, with early activation of ribosomal biogenesis and stress pathways (6h) transitioning to DNA repair and cell cycle regulation at later stages (24-48h) [49].
In Vitro to In Vivo Extrapolation (IVIVE) Workflow
Protocol Overview: This computational framework translates in vitro bioactivity data to human exposure estimates, enabling prioritization of chemicals for further testing [51].
Detailed Methodology:
- Data Aggregation: Collect in vitro bioactivity data from sources like EPA's CompTox Chemicals Dashboard for developmental toxicity endpoints.
- Reverse Dosimetry: Apply in vitro distribution models (e.g., Armitage model) and physiologically-based pharmacokinetic (PBPK) models to estimate external exposures from in vitro bioactive concentrations.
- Bioactive Dose Comparison: Compare NAM-based human oral equivalent doses (hOED) with known in vivo endpoints (e.g., LOAELs) to establish correlation.
- Priority Ranking: Classify chemicals as high, medium, or low priority for developmental toxicants based on the comparison between in vitro bioactivity and in vivo effect levels.
Critical Considerations: In a study of 23 chemicals with developmental toxicity assays, 7 showed lower hOEDs for developmental assays than for all available assays, suggesting that using all in vitro data to derive hOED provides the most conservative approach [51].
Signaling Pathways in Nanoparticle Toxicity
Figure 1: Temporal Evolution of Nanoparticle Toxicity Pathways. This diagram illustrates the sequential activation of cellular stress pathways following nanoparticle exposure, based on temporal transcriptomic analysis of AgNPs [49] and mechanistic studies of SiNPs [36].
Computational Approaches for Toxicity Prediction
Table 3: Computational Tools for Toxicokinetic and Physicochemical Property Prediction
| Software Tool | Prediction Capabilities | Performance Metrics | Applicability |
|---|---|---|---|
| OPERA | PC properties, environmental fate parameters, toxicity endpoints [52] | R² average = 0.717 for PC properties [52] | Broad chemical space including drugs and industrial chemicals |
| Random Forest/LightGBM | NP toxicity based on concentration, size, zeta potential [13] | Identified inverse relationship between NP concentration and cell viability [13] | Nanomaterial toxicity screening |
| IVIVE Workflow | Developmental toxicity prioritization using PBPK modeling [51] | Correctly prioritized known developmental toxicants [51] | Chemical risk assessment without animal testing |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagents and Experimental Platforms
| Item | Function | Application Context |
|---|---|---|
| Air-Liquid Interface (ALI) Systems | Mimics physiological inhalation exposure for in vitro models [50] | Inhalation toxicity testing of nanoparticles and volatile compounds |
| BEAS-2B Cell Line | Immortalized human bronchial epithelial cells for airway toxicity studies [50] | Portal of entry toxicity assessment for inhaled nanomaterials |
| Primary Human Bronchial Epithelial Cells (pHBECs) | Differentiated normal primary cells with relevant tissue functions [50] | Physiologically relevant airway models for inhalation toxicology |
| STRING Database | Protein-protein interaction network analysis for pathway identification [49] | Systems biology analysis of toxicity mechanisms from transcriptomic data |
| CellDesigner & COPASI | Pathway visualization and dynamic simulation of molecular responses [49] | Kinetic modeling of temporal toxicity progression |
| Transcriptomic Platforms | RNA sequencing for gene expression analysis and benchmark dose calculation [50] | Identification of sensitive toxicity pathways and points of departure |
The benchmarking data presented in this guide demonstrates significant progress in correlating in vitro and in vivo toxicity outcomes, particularly for inorganic nanoparticles where mechanistic pathways are increasingly well-characterized. The integration of advanced exposure systems like ALI cultures with temporal transcriptomics and computational modeling provides a multifaceted approach to toxicity prediction that accounts for both kinetic and dynamic aspects of nanoparticle-biological interactions. For researchers evaluating the comparative toxicity profiles of inorganic versus organic nanoparticles, the experimental protocols and computational tools outlined here offer validated frameworks for enhancing predictive accuracy. While challenges remain in fully capturing the complexity of in vivo responses—particularly for organic nanoparticles with more diverse composition profiles—the consistent correlation of transcriptomic points of departure and pathway activation patterns between systems provides confidence in these new approach methodologies. As these benchmarking strategies continue to evolve, they promise to accelerate the development of safer nanomaterial designs while reducing reliance on traditional animal testing.
Designing for Safety: Strategies to Mitigate and Manage Nanoparticle Toxicity
The expansion of nanotechnology into biomedical applications, from targeted drug delivery to tissue engineering, has made the assessment and mitigation of nanoparticle (NP) toxicity a paramount concern for researchers and regulatory bodies [5] [2]. The very physicochemical properties that make nanoparticles technologically fascinating—such as their high surface area-to-volume ratio, enhanced reactivity, and tunable optical and electronic behaviors—can also provoke adverse biological effects, including oxidative stress, inflammatory responses, and cellular damage [2]. The toxicity profile of a nanoparticle is not a fixed property but is profoundly influenced by its material composition (organic vs. inorganic), its inherent structural parameters (size, shape), and, most critically, its surface characteristics [5] [12]. Consequently, surface modification and the application of biocompatible coatings have emerged as central strategies in the design of safer, more effective nanomaterials. This guide objectively compares these strategies, framing them within the broader research context of inorganic versus organic nanoparticle toxicity profiles, to aid professionals in selecting and developing the most appropriate and low-risk materials for biomedical applications.
Inorganic vs. Organic Nanoparticles: A Comparative Toxicity Profile
Nanoparticles are broadly classified into organic, inorganic, and carbon-based categories, each with distinct material properties, applications, and associated toxicity concerns [12]. Understanding these fundamental differences is crucial for selecting a base material and applying the appropriate safety-by-design strategy.
Table 1: Comparative Overview of Organic and Inorganic Nanoparticles for Biomedical Applications.
| Feature | Organic Nanoparticles | Inorganic Nanoparticles |
|---|---|---|
| Composition | Polymers, lipids, proteins [12] [53] | Metals (Au, Ag), metal oxides (Fe₂O₃, ZnO, TiO₂), ceramics (hydroxyapatite) [12] [53] |
| Key Applications | Drug delivery (e.g., liposomes, micelles), controlled release systems [53] | Drug delivery, bioimaging, cancer theranostics, hyperthermia, antimicrobial agents [5] [53] |
| Advantages | Biodegradable, biocompatible, low intrinsic toxicity [53] | High stability, tunable physicochemical/magnetic/optical properties, high drug-loading capacity [53] |
| Primary Toxicity Concerns | Poor stability, short shelf-life, low drug encapsulation efficacy [53] | Ion release (e.g., Zn²⁺, Ag⁺), generation of Reactive Oxygen Species (ROS), oxidative stress, surface reactivity [5] [2] [53] |
| Common Surface Modification Strategies | PEGylation, functionalization with targeting ligands [53] | Coating with polymers (e.g., PEG), silica, or biomolecules; ligand functionalization [54] [53] |
A critical mechanistic difference underpins the toxicity concerns: many inorganic nanoparticles, such as those made from silver or zinc oxide, can release toxic ions or directly catalyze reactions that generate reactive oxygen species (ROS), leading to oxidative damage of cellular components [2]. In contrast, organic nanoparticles, while generally safer, face challenges related to structural integrity and performance [53]. This dichotomy necessitates tailored approaches to surface engineering for each material class.
Fundamental Mechanisms of Nanoparticle Toxicity
To effectively design mitigation strategies, one must understand the primary mechanisms through which nanoparticles induce toxicological effects. The following pathway outlines a common sequence of events leading to cellular damage.
Diagram 1: Key cellular toxicity pathway triggered by nanoparticles. The pathway is often initiated by oxidative stress, a central mechanism influenced by NP physicochemical properties [5] [2].
The key physicochemical parameters of nanoparticles that directly influence these toxicity mechanisms include [5] [2]:
- Size: Smaller particles (< 100 nm) have a larger surface area-to-volume ratio, increasing their reactivity and potential for cellular uptake and ROS generation.
- Shape: Needle or plate-like particles can cause more physical damage to cell membranes than spherical ones.
- Surface Charge: Positively charged (cationic) particles exhibit stronger electrostatic interactions with negatively charged cell membranes, leading to higher cellular uptake and greater cytotoxicity.
- Surface Chemistry and Reactivity: The chemical nature of the surface can catalyze ROS-producing reactions or release toxic ions (e.g., Ag⁺ from silver nanoparticles).
Surface Modification Strategies for Reduced Toxicity
Surface engineering aims to control the nano-bio interface to mitigate the adverse effects outlined above. These strategies can be categorized into bio-inert and bioactive approaches.
Table 2: Comparison of Surface Modification and Coating Strategies.
| Strategy | Mechanism of Action | Key Examples | Effect on Toxicity & Performance |
|---|---|---|---|
| Polymer Coatings (e.g., PEG) | Forms a hydrophilic steric barrier that reduces protein adsorption (fouling) and immune recognition [54] [53]. | Polyethylene Glycol (PEG), Poly(2-ethyl-2-oxazoline) [54] | Decreases opsonization, increases blood circulation time, reduces cytotoxicity and immune activation [53]. |
| Surface Functionalization | Covalent grafting of specific molecules to alter surface chemistry and charge [54]. | Self-Assembled Monolayers (SAMs), covalent grafting of amines or thiols [54] | Shields reactive surface, allows tuning of surface charge (to reduce cationic toxicity), and enables targeting [54] [2]. |
| Biomimetic Coatings | Coating with molecules that mimic the body's natural environment to promote biocompatibility [54] [55]. | Peptide coatings, endothelial cell membrane mimics, phosphorylcholine-based polymers [54] [55] | Reduces thrombogenicity on blood-contacting implants, resists protein adsorption, and can promote healthy endothelialization [55]. |
| Inert Material Coating | Encapsulation in a stable, biocompatible, and less reactive material [53]. | Silica (SiO₂) coating, ceramic coatings (e.g., hydroxyapatite) [12] [53] | Isolates a toxic core (e.g., heavy metal NP) from the biological environment, preventing ion leaching and reducing direct toxicity [53]. |
The following diagram illustrates how these surface modifications create a protective interface that alters the nanoparticle's interaction with biological systems.
Diagram 2: The role of surface coatings in creating a protective interface that mitigates the toxicity of the nanoparticle core by controlling its interaction with the biological environment [54] [55] [53].
Experimental Protocols for Evaluating Coating Efficacy
Robust experimental validation is required to assess the success of any surface modification in reducing toxicity. The following are standard methodologies used in the field.
Protocol for In Vitro Cytotoxicity Assessment (MTT/XTT Assay)
Objective: To quantitatively measure cell viability after exposure to modified and unmodified nanoparticles [2].
- Cell Seeding: Seed adherent cells (e.g., human mesenchymal stem cells or macrophage cell lines) in a 96-well plate at a standardized density (e.g., 10,000 cells/well) and culture for 24 hours to allow adhesion.
- Nanoparticle Exposure: Prepare a concentration series of the test nanoparticles (coated and unmodified) in cell culture medium. Replace the medium in the wells with the nanoparticle suspensions. Include wells with only medium (blank) and cells with medium only (untreated control).
- Incubation: Incubate the plate for 24-48 hours at 37°C and 5% CO₂.
- Viability Reagent Addition: Add a tetrazolium dye solution (MTT or XTT) to each well and incubate for 2-4 hours. Metabolically active cells reduce the dye to a colored formazan product.
- Signal Measurement: For MTT, solubilize the formed formazan crystals with a solvent (e.g., DMSO) and measure the absorbance at 570 nm using a microplate reader. For XTT, measure the absorbance of the soluble formazan directly.
- Data Analysis: Calculate cell viability as a percentage of the untreated control. The half-maximal inhibitory concentration (IC₅₀) can be determined from the dose-response curve. A successful coating will show a higher IC₅₀ value, indicating reduced cytotoxicity.
Protocol for Hemocompatibility Testing
Objective: To evaluate the thrombogenic potential of blood-contacting materials, such as vascular stents or grafts [55].
- Sample Preparation: Incubate the coated and unmodified material samples in phosphate-buffered saline (PBS) or plasma.
- Whole Blood Incubation: Draw fresh human blood containing an anticoagulant (e.g., sodium citrate). Add the blood to the samples and incubate under gentle agitation at 37°C for a set period (e.g., 1 hour).
- Plasma Separation: Centrifuge the samples to obtain platelet-poor plasma.
- Thrombin-Antithrombin (TAT) Complex ELISA: Use a commercial Enzyme-Linked Immunosorbent Assay (ELISA) kit to measure the concentration of TAT complexes in the plasma. This serves as a marker for thrombin generation, a key step in the coagulation cascade.
- Data Analysis: Compare TAT complex levels between test samples and controls (negative and positive). A bio-inert or bioactive coating that resists coagulation will result in significantly lower TAT levels compared to an unmodified control material [55].
The Scientist's Toolkit: Essential Reagents for Surface Engineering
Table 3: Key Research Reagent Solutions for Surface Modification and Toxicity Testing.
| Reagent / Material | Function in Research |
|---|---|
| Polyethylene Glycol (PEG) | The gold-standard polymer for creating stealth coatings that reduce protein fouling and improve nanoparticle circulation time [54] [53]. |
| Polyethylenimine (PEI) | A cationic polymer often used for gene delivery; also studied in graft copolymers to create stable, multifunctional antifouling surfaces [54]. |
| Silane Coupling Agents | Used to functionalize the surface of inorganic nanoparticles (e.g., silica, metal oxides) with reactive groups (amine, thiol, carboxyl) for further covalent grafting [54]. |
| Polydopamine (PDA) | A versatile bio-inspired polymer that forms adherent coatings on virtually any material surface, serving as a platform for secondary reactions and functionalization [54]. |
| Hydroxyapatite (HA) | A bioactive ceramic coating material used to improve the osseointegration of orthopedic implants and as a component in drug delivery systems [12] [53]. |
| Tetrazolium Salts (MTT/XTT) | Water-soluble or insoluble salts used in colorimetric assays to quantitatively measure cell metabolic activity and viability as an indicator of cytotoxicity [2]. |
The strategic application of surface modifications and biocompatible coatings represents a powerful and necessary approach to mitigating the inherent toxicity risks of nanoparticles, particularly those composed of inorganic materials. The choice between a bio-inert coating like PEG for stealth properties or a bioactive coating like hydroxyapatite for improved integration is dictated by the target application. As the field advances, the principles of Green Toxicology—which advocate for testing early and incorporating safety considerations during the design phase—are becoming increasingly important [56]. The future of safe nanotechnology lies in the continued development of sophisticated, multifunctional coatings and the adoption of rigorous, standardized testing protocols that enable researchers to balance the remarkable therapeutic potential of nanoparticles with an unwavering commitment to safety.
Nanoparticles (NPs) are engineered structures with dimensions up to 100 nanometers, possessing unique properties due to their high surface area-to-volume ratio. [12] They are broadly classified into inorganic nanoparticles (metal oxides, quantum dots, gold) and organic nanoparticles (lipidic, polymeric, protein-based). [12] The core material is a primary determinant of their application and biological interactions. While inorganic NPs are often prized for their structural rigidity and optical properties, and organic NPs for their biodegradability, their respective profiles concerning immunogenicity, biodistribution, and long-term fate present a complex landscape that researchers must navigate. [12] This guide objectively compares these two classes by synthesizing experimental data on the three critical challenges that define their safety and efficacy in biomedical applications.
Comparative Immunogenic Reactions
The interaction between nanoparticles and the immune system is a primary determinant of their safety and applicability. Experimental data reveal significant differences in how inorganic and organic nanoparticles provoke immune responses.
Mechanisms of Immune Activation
Immune recognition often begins with nanoparticle opsonization by serum proteins, leading to phagocytic clearance and potential inflammatory responses. [57] A key mechanism for inorganic metal and metal oxide NPs is the induction of oxidative stress via reactive oxygen species (ROS) production. [38] ROS can trigger the activation of nuclear factor kappa B (NF-κB) signaling, upregulating pro-inflammatory cytokines like IL-1, IL-6, IL-8, and tumor necrosis factor-α (TNF-α), leading to inflammation and cell death. [38] Surface characteristics play a critical role; for instance, positively charged particles demonstrate stronger binding with negatively charged cell membranes, often resulting in greater toxicity and immune activation compared to neutral or negatively charged counterparts. [38]
Experimental Data and Comparison
Direct comparative studies provide quantifiable insights into immunogenicity. One investigation assessed the acute inflammatory response in mice following intravenous administration of various NPs, measuring T-cell activation biomarkers. [58]
Table 1: Comparative Immune Cell Activation by Different Nanoparticles
| Nanoparticle Type | CD69+ in CD8+ T Cells (Mean %) | CD25+ Expression (Mean %) | Key Inflammatory Cytokines Elevated |
|---|---|---|---|
| Gold (Inorganic) | 0.40 ± 0.16 | Not Specified | IL-6, TNF-α |
| Quantum Dot Nanocarbons (Inorganic) | Not Specified | 0.23 ± 0.04 | Not Specified |
| Nanodiamond + anti-CD62L (Organic) | Moderate | 0.09 ± 0.04 | IL-6, TNF-α |
| Unconjugated Nanodiamond (Organic) | 0.12 ± 0.09 | Not Specified | Minimal |
Source: Adapted from Frontiers in Nanotechnology, 2025. [58]
The data indicates that unconjugated nanodiamonds (a carbon-based organic NP) exhibited favorable tolerability with minimal inflammatory response and significantly lower memory T cell activation compared to gold nanoparticles and quantum dot nanocarbons (inorganic). [58] Another study highlighted that iron oxide nanoparticles, while generally considered low-toxicity, can still accumulate in organs of the reticuloendothelial system and induce oxidative stress. [18] The method of administration, whether intradermal, intramuscular, or intravenous, also significantly influences the type and magnitude of the immune response elicited, a critical factor in experimental design. [59]
Diagram 1: Simplified Pathway of Nanoparticle-Induced Immunogenic Reaction. Inorganic NPs often have a stronger propensity to trigger the ROS-to-NF-κB axis. [38]
Off-Target Accumulation and Biodistribution
Off-target accumulation not only reduces the therapeutic efficacy of nanoparticle delivery systems but also poses significant toxicity risks. The physicochemical properties of NPs, which vary between inorganic and organic classes, are critical determinants of their in vivo journey.
Key Properties Governing Distribution
The size, shape, surface charge (zeta potential), and surface coating of a nanoparticle are the primary factors affecting its biodistribution. [60] [57] [38] Smaller particles (typically <10 nm) are rapidly cleared by renal filtration, while larger ones (>100 nm) are often sequestered by the liver and spleen. [57] [61] Shape influences cellular uptake and flow dynamics; for instance, spherical particles are often internalized more efficiently than rod-shaped ones. [38] Surface charge is crucial, with positively charged particles typically exhibiting higher cellular uptake but also potentially greater toxicity. [38] A dense coating of polyethylene glycol (PEG) is a common strategy to create a "stealth" effect, reducing opsonization and prolonging circulation time for both inorganic and organic NPs. [60] [57]
Comparative Biodistribution Data
Data-driven models and experimental studies highlight trends in off-target accumulation. A multivariate linear regression-physiologically based pharmacokinetic (MLR-PBPK) framework identified that for a wide range of non-dissolvable nanoparticles, zeta potential, size, and coating were the most influential predictors of biodistribution, while the core material and shape had lesser impacts. [60] This suggests that surface engineering can modulate distribution patterns across material classes.
Experimental data from mouse models provides organ-specific accumulation patterns, as shown in Table 2.
Table 2: Primary Off-Target Accumulation Sites of Nanoparticles
| Nanoparticle Type | Primary Accumulation Organs (Highest to Lower) | Key Supporting Experimental Data |
|---|---|---|
| Gold NPs (Inorganic) | Left Lung, Liver, Spleen | Biodistribution in mice showed persistent localization in the left lung. [58] |
| Iron Oxide NPs (Inorganic) | Liver, Spleen, Lungs, Brain | Studies show accumulation in reticuloendothelial system organs. [18] [12] |
| Quantum Dot Nanocarbons (Inorganic) | Kidney, Liver, Blood, Heart | Prominent persistence in the kidney, liver, blood, and heart. [58] |
| Nanodiamonds (Organic) | Heart, Liver, Spleen, Lungs | After IV injection, primary accumulation in the heart, with significant levels in liver and spleen. [58] |
| Liposomal & Polymeric NPs (Organic) | Liver, Spleen | Passive targeting to highly vascularized organs; influenced by PEGylation. [57] [61] |
The data indicates that inorganic nanoparticles like gold and quantum dots can accumulate in a diverse range of organs, including the lungs and kidneys. In contrast, organic nanoparticles like nanodiamonds and liposomal systems predominantly accumulate in the liver, spleen, and heart, consistent with clearance by the mononuclear phagocyte system. [18] [58] [61] A significant finding is that nearly 60% of intravenously injected nanodiamonds can accumulate in the liver. [58]
Diagram 2: Simplified Workflow of Nanoparticle Biodistribution and Common Off-Target Sites. The primary accumulation organs can vary significantly between different NP types. [60] [58]
Long-Term Fate and Potential Toxicity
The long-term fate of nanoparticles—encompassing biodegradation, persistence, and chronic toxicity—is pivotal for clinical translation and environmental safety. Fundamental differences exist between inorganic and organic nanoparticles in their biological persistence and clearance pathways.
Clearance Mechanisms and Persistence
The body primarily clears nanoparticles through hepatic (liver) and renal (kidney) pathways. [58] The feasibility of these pathways depends on NP size and composition.
- Organic Nanoparticles: Many, such as those made from lipids or polymers, are designed to be biodegradable. They can be broken down into metabolic by-products and cleared from the body, reducing the risk of long-term accumulation. [12]
- Inorganic Nanoparticles: Metals (e.g., gold, silver) and metal oxides (e.g., iron oxide, titanium dioxide) are often non-biodegradable or dissolve slowly. [60] They may persist in tissues for extended periods. For example, the estimated half-life of some nanoparticles in human lungs is about 700 days. [18] Chronic exposure to persistent nanoparticles raises concerns about organ toxicity, as seen with silver nanoparticles detected in the brain, liver, and spleen after exposure. [18]
Chronic Toxicity and Genotoxicity
The long-term presence of nanoparticles, particularly non-degradable inorganic ones, can lead to sustained toxic effects. The predominant mechanism is chronic oxidative stress via ROS production, which can cause damage to DNA, proteins, and lipids. [38] This can result in genotoxicity through both primary (direct interaction with DNA or replication machinery) and secondary (via persistent inflammation) mechanisms. [38] For instance:
- Aluminum Oxide NPs: Have shown dose-dependent genotoxic effects in rat blood cells and mouse lymphoma cells. [18]
- Zinc Oxide NPs: Chronic exposure in models resulted in oxidative DNA damage in the liver and changes in enzyme profiles. [18]
- Silver NPs: Associated with DNA adduct formation in human lung cancer cell lines. [18]
Table 3: Long-Term Fate and Toxicity Indicators of Nanoparticles
| Nanoparticle Type | Persistence & Clearance | Documented Long-Term Toxicity Endpoints |
|---|---|---|
| Gold NPs (Inorganic) | Relatively inert core, long-term persistence in organs like lungs. [58] | Can induce inflammatory responses; toxicity dependent on dose, stabilizer, and surface charge. [18] |
| Silver NPs (Inorganic) | Accumulates in brain, liver, lungs, spleen; slow clearance. [18] | Cytotoxicity, ROS generation, LDH leakage, DNA damage. [18] [38] |
| Iron Oxide NPs (Inorganic) | Bioaccumulates in RES organs; considered to have relatively low toxicity. [18] [12] | Can contribute to cellular iron pool, potential for oxidative stress. [18] |
| Liposomal/Polymeric NPs (Organic) | Typically biodegradable; designed for controlled clearance. [12] [61] | Generally lower chronic toxicity; potential for lipidosis or polymer-related immune reactions. |
| Nanodiamonds (Organic) | Clearance via bladder/urinary tract; persistent accumulation in heart. [58] | Favorable long-term tolerability with minimal chronic immune activation in studies. [58] |
Essential Experimental Protocols for Comparison
To generate comparable data on the key challenges, standardized and rigorous experimental protocols are essential. Below is a synthesis of methodologies cited in the literature.
Protocol 1: In Vivo Toxicity and Biodistribution Profiling
This protocol is foundational for assessing off-target accumulation and acute toxicity. [58]
- Animal Model: Use female C57BL/6 mice, sorted by body weight into experimental groups.
- Nanoparticle Administration: Prepare sterile dispersions of the test nanoparticles (e.g., gold NPs, nanodiamonds, quantum dots). Administer via a single intravenous injection at multiple dose concentrations (e.g., 5, 10, 20, and 40 mg/kg).
- Sample Collection: Euthanize animals at predetermined time points post-injection (e.g., 2, 24, and 96 hours). Collect blood (for cytokine analysis and immune profiling) and harvest major organs (heart, liver, spleen, lung, kidney).
- Biodistribution Analysis: Quantify nanoparticle concentration in homogenized organ tissues using appropriate techniques (e.g., inductively coupled plasma mass spectrometry (ICP-MS) for metal-based NPs, fluorescence imaging for labeled NPs).
- Immune Response Assessment: Analyze blood samples using flow cytometry to quantify T-cell activation markers (e.g., CD69, CD25) and ELISA to measure pro-inflammatory cytokine levels (e.g., IL-6, TNF-α).
Protocol 2: In Vitro Cytotoxicity and Genotoxicity Assessment
These assays are crucial for initial screening and mechanistic studies. [18] [62]
- Cell Culture: Employ relevant mammalian cell lines (e.g., human mesenchymal stem cells, hepatic HepG2 cells, leukemic HL-60 cells) under standard conditions.
- NP Exposure: Expose cells to a range of nanoparticle concentrations (e.g., from 10 to 400 µg/mL) for 24-72 hours.
- Viability/Cytotoxicity Assay: Use tetrazolium-based assays like MTT or MTS to measure cell viability. Alternatively, measure lactate dehydrogenase (LDH) release as an indicator of cell membrane integrity. [18]
- Oxidative Stress Measurement: Quantify intracellular reactive oxygen species (ROS) using fluorescent probes (e.g., DCFH-DA).
- Genotoxicity Assessment: Perform the comet assay (single-cell gel electrophoresis) to detect DNA strand breaks. Use the cytokinesis-blocked micronucleus assay to assess chromosome damage.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for Nanoparticle Toxicity and Biodistribution Studies
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| C57BL/6 Mouse Model | In vivo model for assessing biodistribution, tolerability, and immune response. [58] | Female mice are often used; allows for comparison with a large body of published literature. |
| PEG (Polyethylene Glycol) | Surface coating to create "stealth" NPs, reducing opsonization and prolonging circulation half-life. [60] [57] | A dominant coating in published studies; improves pharmacokinetics of both inorganic and organic NPs. [60] |
| MTT/MTS/WST-1 Assay Kits | Tetrazolium-based colorimetric assays to measure cell viability and proliferation in vitro. [18] | Note: Some NPs can interfere with assay materials, requiring validation with multiple methods. [18] |
| LDH (Lactate Dehydrogen) Assay Kit | Measures LDH release from damaged cells, quantifying cytotoxicity and membrane integrity. [18] | Useful complement to viability assays. |
| ELISA Kits for Cytokines | Quantify levels of pro-inflammatory cytokines (e.g., IL-6, TNF-α, IL-1β) in serum or cell culture supernatant. [18] [58] | Critical for evaluating immunogenic reactions. |
| Flow Cytometry Antibodies | Profile and quantify immune cell populations and activation states (e.g., CD4, CD8, CD69, CD25). [58] | Essential for detailed immunophenotyping in response to NP exposure. |
| Comet Assay Kit | Standardized kit for performing the single-cell gel electrophoresis assay to detect DNA damage. [18] | A standard technique for assessing NP genotoxicity. [18] |
| ICP-MS (Inductively Coupled Plasma Mass Spectrometry) | Highly sensitive technique to quantify metal-based nanoparticle concentration in tissues for biodistribution. | Gold standard for tracking inorganic NPs like gold, iron oxide, and silver in biological matrices. |
The objective comparison of inorganic and organic nanoparticles reveals a trade-off between functionality and biological safety. Inorganic nanoparticles, such as gold and quantum dots, offer unique physical properties for imaging and therapy but tend to pose higher risks of immunogenicity and persistent accumulation in sensitive organs like the lungs and kidneys. Organic nanoparticles, including nanodiamonds and liposomal systems, generally exhibit more favorable tolerability profiles, lower inflammatory potential,, and the capacity for biodegradation, though they are still prone to off-target accumulation in the liver and spleen.
The choice between these two classes is not a simple binary decision but a strategic one. The data indicates that surface engineering (coating, charge, ligand density) can be as influential as the core material itself in determining biological fate. [60] [57] Therefore, the future of safe and effective nanoparticle design lies in a rational approach that prioritizes a deep understanding of the structure-activity relationship, leveraging the strengths of each material class while meticulously mitigating its inherent challenges through precise physicochemical modulation.
The integration of nanotechnology into healthcare has introduced revolutionary advancements in medical treatments and diagnostics, creating a new category of Nanotechnology-Enabled Health Products (NHPs) [63]. These products promise enhanced therapeutic efficacy through improved drug solubility, targeted delivery, and reduced side effects [64]. However, their development occurs within a complex regulatory environment that struggles to keep pace with scientific innovation, creating significant barriers to clinical application [63] [65]. This regulatory challenge is further complicated by fundamental safety concerns, particularly the distinct toxicity profiles exhibited by different nanoparticle classes. A growing body of evidence suggests that inorganic nanoparticles often present different toxicological challenges compared to their organic counterparts, necessitating specialized evaluation frameworks that current regulatory systems are still developing [66] [10] [26].
The global nanotechnology sector is experiencing substantial growth, with projections estimating an annual growth rate ranging from 9.2% to 36.4% up to 2030 [63]. The nanomaterials market, valued at $7.1 billion USD in 2020, is anticipated to escalate to $13.60 billion by 2027, driven primarily by increasing demand for nanomaterials in health products, particularly drug delivery systems [63]. This rapid expansion underscores the urgent need for clear, standardized regulatory pathways that can ensure patient safety without stifling innovation.
Global Regulatory Frameworks for Nanomedicines
Regional Regulatory Approaches and Classification Systems
The regulatory landscape for nanomedicines varies significantly across major jurisdictions, with the European Union and United States systems often setting the benchmark for international standards [63]. A key challenge regulators face is that NHPs do not constitute a distinct regulatory category but are primarily classified as either medicinal products or medical devices based on their principal mechanism of action [63].
Table 1: Comparative Regulatory Frameworks for Nanomedicines
| Region | Regulatory Body | Legal Framework | Classification Approach | Key Challenges |
|---|---|---|---|---|
| European Union | European Medicines Agency (EMA) | Directive 2001/83/EC [63] | Based on primary mechanism of action (PIM vs. physical) [63] | Lack of nanomedicine-specific definition and tailored requirements [67] |
| United States | Food and Drug Administration (FDA) | FDA regulations | Product-specific approach without formal nanotechnology definition [68] | Case-by-case review creates uncertainty for manufacturers [65] |
| Global | Various | Varies by country | Adapted from EU or US systems [63] | Inconsistent requirements create barriers to global approval [65] |
In the EU, the legislative framework for medicinal products is delineated by Directive 2001/83/EC, which provides a detailed definition of a medicinal product but lacks specific provisions for nanomedicines [63]. The European Commission defines nanomaterials as substances with particles measuring between 1-100 nm for half their external diameters, whether natural or synthesized [68]. Meanwhile, the FDA lacks formal definitions for terminology such as "nanotechnology," "nanomaterial," and "nanoscale," instead evaluating products on a case-by-case basis [68]. This regulatory fragmentation creates significant challenges for manufacturers seeking global market approval and highlights the need for internationally harmonized standards.
The Regulatory Gap for Nanomedicines
Despite the increasing number of approved nano-based pharmaceutical products—with approximately 100 nanomedicine applications and products approved by the FDA—a well-defined regulatory framework specifically for nanomedicines remains absent [64] [65]. This regulatory gap presents major challenges for stakeholders across the pharmaceutical and healthcare industries, limiting clinical translation of promising nanomedicines [65].
The absence of clear regulatory guidelines complicates the path to registering nanomedicines with regulatory bodies [67]. While some products have overcome these obstacles and reached the market—such as the polyethylene glycol-coated nanoliposomal doxorubicin formulations Doxil (FDA approved in 1995) and Caelyx (EMA approved in 1996)—the process remains challenging for novel nanomedicines [63]. Key regulatory challenges include difficulties in nanomaterial characterization, safety assessment, and quality control, which conventional regulatory frameworks are not fully equipped to address [65] [67].
Toxicity Profiles: Inorganic vs Organic Nanoparticles
Mechanisms of Inorganic Nanoparticle Toxicity
Inorganic nanoparticles, including metal and metal oxide nanoparticles, exhibit unique toxicity mechanisms that differ significantly from conventional pharmaceuticals or larger particles. Their small size and large surface area facilitate increased interaction with biological systems, leading to potential toxic effects through several well-documented mechanisms [66] [10].
Table 2: Toxicity Mechanisms of Selected Inorganic Nanoparticles
| Nanoparticle Type | Primary Toxicity Mechanisms | Key Influencing Factors | Biological Consequences |
|---|---|---|---|
| Silver (AgNPs) | ROS generation, oxidative stress, calcium dysregulation [66] | Size, concentration, surface charge [66] | Liver/kidney toxicity, oxidative damage [66] |
| Titanium Dioxide (TiO₂ NPs) | ROS production, apoptosis, impaired DNA repair [66] | Crystalline structure, exposure route [66] | Genotoxicity, inflammation [66] |
| Gold (AuNPs) | Oxidative stress [66] | Size, surface functionalization [66] | Cytotoxicity in fibroblasts [66] |
| Quantum Dots (CdS, CdTe) | ROS generation, apoptosis, cadmium ion release [66] [69] | Surface coatings, core composition [69] | DNA damage, mitochondrial impairment [66] |
A primary mechanism underlying inorganic nanoparticle toxicity involves reactive oxygen species (ROS) accumulation, which can overwhelm cellular antioxidant defenses and lead to oxidative stress [66] [10]. This oxidative damage affects lipids, proteins, and DNA, potentially triggering inflammatory responses, apoptosis, and genotoxicity [66]. For example, silver nanoparticles (AgNPs) demonstrate size-dependent toxicity, with 10 nm AgNPs exhibiting more significant toxicity than larger counterparts (20-100 nm) due to increased surface area and ROS production per unit mass [66].
The surface properties of inorganic nanoparticles significantly influence their biological interactions. Cationic surfaces generally show higher cytotoxicity than anionic surfaces, and surface functionalization can dramatically alter cellular responses [66]. Quantum dots, particularly those containing cadmium (CdS, CdTe), present specific toxicity concerns due to potential heavy metal ion release, which can induce apoptosis through mitochondrial damage and DNA fragmentation [69].
Organic Nanoparticle Safety Profiles
Organic nanoparticles, including liposomes, polymeric nanoparticles, and dendrimers, typically exhibit more favorable safety profiles compared to inorganic counterparts, though they present their own unique challenges [64]. These nanomaterials are often designed using biocompatible and biodegradable materials, enhancing their tissue compatibility and reducing long-term accumulation concerns [64] [70].
Liposomes, for instance, are synthetic vesicles formed from lipid bilayers that can encapsulate both water-soluble and lipid-soluble drugs [64]. Their biological similarity to cell membranes contributes to their reduced immunogenicity, though composition and surface characteristics can still influence their toxicity profile [64]. Polymeric nanoparticles offer tunable characteristics and improved thermodynamic stability for therapeutic cargo, with safety largely dependent on the choice of polymer and degradation products [64].
The surface modification of organic nanoparticles through PEGylation or other functionalization strategies can further enhance their safety by reducing opsonization and extending circulation time, thereby minimizing unintended interactions with healthy tissues [64] [70]. However, organic nanoparticles may still trigger immune responses or cause toxicity at higher concentrations, emphasizing the need for comprehensive safety assessment regardless of their organic nature [68].
Methodologies for Assessing Nanoparticle Toxicity
Standardized Experimental Protocols
Evaluating nanoparticle toxicity requires specialized methodologies that account for their unique properties. Standardized protocols are essential for generating comparable data across studies and facilitating regulatory review.
Cytotoxicity Assessment (MTT Assay): The MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay provides a quantitative measure of cell viability following nanoparticle exposure [69]. The protocol involves:
- Seeding cells in 96-well plates at appropriate density and allowing adherence for 24 hours
- Treating cells with serial dilutions of nanoparticles for predetermined exposure periods
- Adding MTT solution and incubating to allow formazan crystal formation by viable cells
- Dissolving crystals with solvent and measuring absorbance at 570 nm
- Calculating cell viability relative to untreated controls [69]
This method was effectively employed to demonstrate that surface-modified CdS nanoparticles exhibit reduced toxicity compared to unmodified counterparts, with cysteine-modified CdS showing the lowest toxicity due to detoxifying action and larger particle size [69].
Oxidative Stress Evaluation: Measuring reactive oxygen species (ROS) production is crucial for understanding nanoparticle toxicity mechanisms:
- Cells are incubated with nanoparticle suspensions for relevant exposure times
- DCFH-DA fluorescent probe is added and enters cells
- Intracellular esterases cleave DCFH-DA to non-fluorescent DCFH
- ROS oxidize DCFH to fluorescent DCF
- Fluorescence intensity is measured, correlating with ROS levels [66] [10]
This approach has demonstrated that AgNPs generate more ROS than bulk silver, explaining their enhanced toxicity [66].
Inflammatory Response Assessment: Nanoparticle-induced inflammation is evaluated through cytokine profiling:
- Exposing immune cells or relevant cell lines to nanoparticles
- Collecting culture supernatants at various time points
- Quantifying inflammatory cytokines (TNF-α, IL-1β, IL-6, IL-8) using ELISA
- Comparing levels to positive controls and untreated cells [66] [10]
Carbon nanotubes, for instance, have been shown to trigger cytokine release from macrophages and mesothelial cells through this method [66].
Advanced and Emerging Evaluation Models
Beyond traditional 2D cell cultures, advanced models are emerging to provide more physiologically relevant toxicity data:
3D Organoids: These self-organizing 3D tissue cultures replicate aspects of human physiology, offering improved prediction of in vivo responses compared to conventional models [10]. They allow assessment of nanoparticle penetration, tissue-level distribution, and organ-specific toxicity.
In Vivo Models: Rodent studies remain essential for evaluating systemic toxicity, biodistribution, and organ-specific effects [10]. Parameters assessed include histopathological changes, biochemical markers of organ function, and immune responses across multiple exposure routes.
The following workflow illustrates the integrated experimental approach for nanotoxicity assessment:
Diagram 1: Integrated Workflow for Nanotoxicity Assessment. This comprehensive approach evaluates nanoparticles from basic characterization through advanced modeling to in vivo validation.
Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting nanomedicine toxicity and efficacy studies:
Table 3: Essential Research Reagents for Nanomedicine Evaluation
| Reagent/Material | Function | Application Examples |
|---|---|---|
| MTT Assay Kit | Measures cell viability via mitochondrial activity | Cytotoxicity screening of nanoparticles [69] |
| DCFH-DA Probe | Detects intracellular reactive oxygen species | Oxidative stress assessment [66] [10] |
| ELISA Kits (TNF-α, IL-1β, IL-6, IL-8) | Quantifies inflammatory cytokines | Immunotoxicity evaluation [66] [10] |
| Cell Culture Models | Provides biological systems for toxicity screening | Caco-2 (intestinal), A549 (lung), HepG2 (liver) [66] [10] |
| 3D Organoid Culture Systems | Advanced tissue models for physiological relevance | Predictive toxicology beyond 2D models [10] |
| Surface Modification Reagents | Alters nanoparticle-biomolecule interactions | Toxicity reduction through functionalization [69] [68] |
The regulatory landscape for nanomedicines remains fragmented and inconsistently applied across global jurisdictions, creating significant challenges for research and development [63] [65]. This complexity is compounded by the fundamentally different toxicity profiles exhibited by inorganic versus organic nanoparticles, necessitating tailored evaluation approaches that current regulatory frameworks are still developing [66] [10] [26].
The path forward requires international harmonization of regulatory requirements, with specific guidance on characterization standards, toxicity testing protocols, and quality control measures tailored to nanomedicines [65] [67]. Additionally, developing predictive toxicological models that can accurately assess the long-term safety of both inorganic and organic nanoparticles will be crucial for ensuring patient safety while facilitating the translation of promising nanomedicines to clinical application [10] [68]. As the field continues to evolve, collaboration between regulators, researchers, and industry stakeholders will be essential for establishing a regulatory environment that protects public health without impeding medical innovation.
The application of nanoparticles in drug delivery represents a revolutionary advance in modern medicine, offering unprecedented opportunities for enhancing therapeutic efficacy. This promise, however, is tempered by significant concerns regarding potential toxicity, creating a critical balancing act for researchers and clinicians. Nanoparticles, typically ranging from 1 to 100 nanometers in size, exhibit unique physicochemical properties that differ markedly from their bulk counterparts, owing to their high surface area-to-volume ratio and quantum effects [10]. These properties enable improved drug solubility, prolonged circulation time, enhanced permeability and retention at target sites, and the ability to cross biological barriers [4] [53]. The central challenge in clinical translation lies in leveraging these advantageous properties while minimizing unintended adverse biological consequences, which requires a thorough understanding of the distinct profiles of organic and inorganic nanomaterials.
The current landscape of nanomedicine reveals a diverse array of nanoparticle platforms, broadly categorized into organic and inorganic systems. Organic nanoparticles—including liposomes, polymeric nanoparticles, dendrimers, and micelles—are primarily composed of biodegradable and biocompatible materials [4] [9]. In contrast, inorganic nanoparticles—such as gold, silver, silica, and iron oxide nanoparticles—are valued for their superior stability, tunable degradation rates, and unique optical, magnetic, and electronic properties [53] [5]. While both categories show immense promise for drug delivery applications, their divergent compositions, biological interactions, and metabolic fates necessitate distinct approaches to safety assessment and regulatory consideration. This review systematically compares these nanoparticle classes, focusing on their respective efficacy and safety profiles to inform their rational development for clinical applications.
Comparative Analysis of Organic and Inorganic Nanoparticles
The selection between organic and inorganic nanoparticles for drug delivery applications requires careful consideration of their fundamental properties, which directly influence both therapeutic performance and biological safety. The table below provides a structured comparison of these two nanoparticle classes based on critical parameters relevant to clinical translation.
Table 1: Comparative Properties of Organic and Inorganic Nanoparticles for Drug Delivery
| Property | Organic Nanoparticles | Inorganic Nanoparticles |
|---|---|---|
| Composition | Lipids, polymers, surfactants (e.g., phosphatidylcholine, PLGA) [4] | Metals, metal oxides, silica (e.g., gold, silver, iron oxide, silica) [5] [9] |
| Typical Sizes | 10-200 nm [4] | 1-100 nm [10] |
| Drug Loading Capacity | Variable; can suffer from low encapsulation efficacy [53] | Generally high; especially mesoporous silica with tunable pores [4] [53] |
| Stability & Shelf Life | Poorer stability; shorter shelf life [53] | Highly stable; hydrophilic [53] |
| Surface Functionalization | Moderate; depends on chemical groups | High ease of functionalization (e.g., AuNPs with thiols) [5] [53] |
| Biodegradability | Generally biodegradable [53] | Variable degradation; can be non-biodegradable [66] |
| Unique Properties | Amphiphilic structure (liposomes); biocompatibility [4] | Magnetic, optical, catalytic properties (e.g., SPR in AuNPs) [5] [53] |
| Regulatory Status | Several FDA-approved (e.g., Doxil) [4] | Fewer FDA approvals; primarily iron oxide for MRI [4] |
This comparative analysis reveals fundamental trade-offs that researchers must navigate. Organic nanoparticles benefit from established biocompatibility and biodegradability, with several platforms having already achieved clinical approval. For instance, Doxil—a PEGylated liposomal doxorubicin formulation—demonstrates reduced cardiotoxicity compared to free doxorubicin while maintaining efficacy through the enhanced permeability and retention effect [4]. However, limitations in stability and drug loading capacity can restrict their application scope. Conversely, inorganic nanoparticles offer superior stability, higher drug loading—particularly mesoporous silica nanoparticles with their tunable pore structures—and unique functionalities like imaging capabilities [4] [53]. These advantages, however, come with greater concerns regarding long-term fate, potential accumulation, and material-specific toxicity, presenting more significant hurdles in the regulatory pathway.
Toxicity Mechanisms and Safety Profiles
Understanding the toxicity profiles of nanoparticles requires examination of their interactions with biological systems at molecular, cellular, and organ levels. The mechanisms of toxicity differ significantly between organic and inorganic nanoparticles, influencing both their risk assessment and mitigation strategies.
Inorganic Nanoparticle Toxicity
Inorganic nanoparticles exhibit diverse toxicity pathways primarily driven by their composition, dissolution properties, and surface characteristics. The table below summarizes key toxicity mechanisms and their biological consequences for major classes of inorganic nanoparticles.
Table 2: Toxicity Mechanisms of Selected Inorganic Nanoparticles
| Nanoparticle Type | Key Toxicity Mechanisms | Biological Consequences | References |
|---|---|---|---|
| Silver (AgNPs) | ROS generation, oxidative stress, calcium dysregulation, release of Ag+ ions | Cytotoxicity, oxidative damage to liver/kidneys/lung, antimicrobial activity | [66] |
| Gold (AuNPs) | Oxidative stress, inflammation depending on size and surface charge | Eye pigmentation progression, cytotoxicity in fibroblasts (in vitro) | [66] |
| Silica (SiNPs) | Lysosomal membrane permeabilization, NLRP3 inflammasome activation, ROS, mitochondrial dysfunction | Inflammation (lung fibrosis), genotoxicity, neurotoxicity, autophagy | [36] |
| Quantum Dots (QDs) | ROS generation, lipid peroxidation, release of toxic ions (Cd2+) | Apoptosis, DNA damage, catalase activity increase | [66] |
| Titanium Dioxide (TiO2 NPs) | ROS production, impaired DNA repair processes, apoptosis | Genotoxicity in lung cell lines, inflammation | [66] |
| Carbon Nanotubes | ROS-associated signaling, cytokine release (TNF-α, IL-1β, IL-8, IL-6) | Inflammation, DNA damage, mesothelioma-like pathology | [66] |
A critical emerging mechanism for inorganic nanoparticles is their ability to induce ferroptosis, an iron-dependent form of regulated cell death characterized by overwhelming lipid peroxidation [41]. This pathway develops through a cascade beginning with iron dysregulation and oxidative stress, ultimately triggering fatal lipid peroxidation. While this mechanism can be harnessed therapeutically for cancer treatment, its unintended activation in healthy tissues represents a significant biosafety challenge that requires systematic evaluation [41]. The induction and intensity of these toxicity pathways are heavily influenced by various physicochemical parameters, including size, surface charge, agglomeration state, and functionalization.
Organic Nanoparticle Toxicity
Organic nanoparticles generally exhibit more favorable toxicity profiles due to their biodegradable nature, but nonetheless present distinct safety considerations. Lipid-based nanoparticles like liposomes can trigger complement activation-related pseudoallergy (CARPA) in some patients, while polymeric nanoparticles may generate degradation products with inflammatory potential [4]. The relatively lower toxicity of organic nanoparticles is reflected in their more advanced regulatory approval status, with multiple systems like liposomal doxorubicin (Doxil) and lipid nanoparticle-mRNA vaccines having received clinical approval [4]. However, challenges remain regarding their stability, shelf life, and potential immune reactions that require careful monitoring.
Physicochemical Properties Governing Toxicity and Efficacy
The biological behavior and resulting safety profiles of nanoparticles are predominantly governed by their physicochemical properties, which influence cellular uptake, biodistribution, clearance, and molecular interactions. The most critical parameters include:
Size: Smaller nanoparticles (≤10 nm) demonstrate enhanced cellular uptake and tissue penetration but exhibit broader tissue distribution and potential renal clearance [10]. For instance, 10 nm silver nanoparticles show higher hepatobiliary toxicity and more widespread tissue distribution compared to larger counterparts (20-100 nm) [10] [66].
Shape: Aspect ratio significantly influences toxicity, with high-aspect-ratio materials like long carbon nanotubes (≥10 μm) potentially causing mesothelioma-like pathology, similar to asbestos fibers [66].
Surface Charge: Cationic surfaces generally exhibit higher cytotoxicity compared to anionic or neutral surfaces due to enhanced interaction with negatively charged cell membranes [66].
Surface Functionalization: Coatings and functional groups dramatically alter biological interactions. For example, dextran-coated cerium oxide nanoparticles induce dose-dependent apoptotic processes in human lung fibroblasts [71], while surface engineering of silica nanoparticles can mitigate their toxicity through reduced inflammatory responses [36].
The following diagram illustrates how these physicochemical properties influence cellular uptake and subsequent toxicity mechanisms for inorganic nanoparticles:
Figure 1: Physicochemical Properties Drive Toxicity Pathways. This diagram illustrates how key properties of inorganic nanoparticles influence cellular uptake and initiate interconnected toxicity mechanisms including oxidative stress, inflammation, and organelle damage.
Experimental Models for Assessing Nanotoxicity
Robust assessment of nanoparticle safety profiles requires sophisticated experimental models that can accurately predict biological responses. The following diagram outlines a comprehensive workflow for evaluating nanoparticle toxicity, integrating both in vitro and in vivo approaches:
Figure 2: Integrated Workflow for Nanotoxicity Assessment. This experimental workflow encompasses nanoparticle synthesis, characterization, and evaluation using complementary in vitro and in vivo models to assess multiple toxicity endpoints.
Detailed Experimental Protocols
Protocol 1: Assessing Oxidative Stress and Mitochondrial Dysfunction
Objective: To evaluate nanoparticle-induced oxidative stress and mitochondrial impairment in mammalian cells [66] [71].
Cell Culture: H9C2 cardiomyocytes or MRC-5 human lung fibroblasts are maintained in DMEM with 10% FBS at 37°C in 5% CO₂.
Nanoparticle Treatment:
- Prepare stock suspensions of nanoparticles in sterile PBS with 0.1% BSA and sonication.
- Expose cells to varying concentrations (e.g., 10-100 μg/mL) of nanoparticles for 24-48 hours.
- Include positive control (e.g., 100 μM H₂O₂) and negative control (vehicle only).
ROS Measurement:
- Wash cells with PBS and incubate with 10 μM DCFH-DA in serum-free media for 30 minutes at 37°C.
- Measure fluorescence intensity (excitation 485 nm, emission 535 nm) using a microplate reader.
- Express results as percentage increase in fluorescence compared to untreated controls.
Mitochondrial Membrane Potential (ΔΨm):
- Incubate cells with 2 μM JC-1 dye for 20 minutes at 37°C.
- Analyze using flow cytometry or fluorescence microscopy.
- Calculate red/green fluorescence ratio, with decreased ratio indicating mitochondrial depolarization.
ATP and NAD+/NADH Measurement:
- Extract intracellular ATP using commercial kits based on luciferase-luciferin reaction.
- Measure NAD+/NADH ratios using enzymatic cycling assays.
- Normalize all values to total protein content.
Protocol 2: Evaluating Inflammatory Response in Immune-Competent Models
Objective: To assess nanoparticle-induced inflammation using advanced tri-culture intestinal models [71].
Tri-culture Model Establishment:
- Culture Caco-2 and HT29-MTX-E12 cells in 75:25 ratio on Transwell inserts (apical compartment) until fully differentiated (21 days).
- Differentiate THP-1 monocytes into macrophages using 100 nM PMA in basolateral compartment.
- For inflamed model: Pre-treat barrier cells with 10 ng/mL IFN-γ and macrophages with IFN-γ + 1 μg/mL LPS for 48 hours.
Nanoparticle Exposure:
- Apply fluorescently-labeled nanoparticles (e.g., 40 nm PMA with COOH or NH₂ surface) at low (143 μg/cm²) and high (571 μg/cm²) concentrations.
- Expose for 24 or 48 hours.
- Use sedimentation, diffusion, and dosimetry (ISDD) modeling to calculate delivered dose.
Cytotoxicity Assessment:
- Measure lactate dehydrogenase (LDH) release in basolateral medium using colorimetric assay.
- Calculate percentage cytotoxicity relative to total LDH content (from lysed cells).
Cytokine Profiling:
- Collect basolateral medium and analyze IL-1β, IL-6, IL-8, and TNF-α using ELISA.
- Normalize cytokine levels to total protein content.
Barrier Integrity Assessment:
- Measure transepithelial electrical resistance (TEER) before and after exposure.
- Perform immunofluorescence staining for tight junction proteins (ZO-1, occludin).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Nanoparticle Toxicology Studies
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Cell Lines | In vitro toxicity screening | Immortalized lines (e.g., A549, BEAS-2B lung cells; BALB/3T3 fibroblasts) [66] [9] |
| Primary Cells | More physiologically relevant models | Primary macrophages, hepatocytes, neural cells [9] |
| ROS Detection Probes | Measure oxidative stress | DCFH-DA, dihydroethidium; read at Ex/Em 485/535 nm [66] |
| JC-1 Dye | Assess mitochondrial membrane potential | Fluorescence shifts from red (aggregates) to green (monomers) with depolarization [71] |
| ELISA Kits | Quantify inflammatory cytokines | TNF-α, IL-1β, IL-6, IL-8 measurements [36] [71] |
| LDH Assay Kit | Evaluate cytotoxicity | Colorimetric measurement of released LDH [71] |
| Apoptosis Detection Kits | Quantify programmed cell death | Annexin V/PI staining with flow cytometry [66] |
| Comet Assay Reagents | Detect DNA damage | Alkaline conditions for single-strand breaks detection [66] |
| 3D Culture Matrices | Advanced disease modeling | Extracellular matrix hydrogels for organoid cultures [10] |
| Transwell Systems | Barrier function studies | Permeable supports for intestinal, BBB models [71] |
The path to successful clinical translation of nanoparticle-based drug delivery systems requires meticulous balancing of efficacy and safety considerations. This comparative analysis reveals that organic nanoparticles currently hold advantages in biodegradability and regulatory acceptance, while inorganic nanoparticles offer superior stability, functionality, and drug loading capacity. Critical to the development of both platforms is recognizing that their biological interactions and toxicity profiles are intrinsically linked to controllable physicochemical parameters including size, shape, surface charge, and functionalization.
Future progress will depend on several key approaches: First, the implementation of "safer-by-design" strategies that proactively address potential toxicity through intelligent material selection and surface engineering [36]. Second, the development of more sophisticated testing platforms that better recapitulate human physiology, such as immune-competent co-culture models and organ-on-a-chip systems [10] [71]. Third, the exploration of natural compounds like quercetin and selenium as potential protective agents against nanoparticle-induced toxicity [71]. Finally, standardized assessment frameworks that systematically evaluate emerging toxicity mechanisms such as ferroptosis [41] and epigenetic modifications [66] will be essential for comprehensive safety profiling. Through these coordinated efforts, the field can advance nanoparticle-based therapeutics that maximize therapeutic efficacy while minimizing potential harm, ultimately fulfilling the promise of nanomedicine for patient care.
Head-to-Head: A Direct Comparative Analysis of Organic and Inorganic Nanoparticle Toxicity
Inorganic nanoparticles (NPs), including those made from metals and metal oxides, have become pivotal in advancing nanotechnology across biomedical, environmental, and industrial sectors. Their unique physicochemical properties, such as high surface area-to-volume ratio and distinctive optical and magnetic characteristics, drive their widespread application. However, these same properties raise significant concerns regarding their potential toxicity. Understanding the toxicity profiles of these NPs is crucial for safely integrating them into consumer products and therapeutic applications. This guide objectively compares the toxicity of four prominent inorganic nanoparticles—Silver (AgNPs), Gold (AuNPs), Iron Oxide (FexOy NPs), and Zinc Oxide (ZnONPs)—by synthesizing current experimental data. Framed within broader research on inorganic versus organic nanoparticle toxicity, this analysis provides drug development professionals and scientists with a detailed comparison of toxicological mechanisms, key influencing factors, and relevant experimental methodologies.
Comparative Toxicity Profiles of Key Inorganic Nanoparticles
The table below summarizes the toxicity profiles of silver, gold, iron oxide, and zinc oxide nanoparticles, highlighting their primary mechanisms and target systems.
Table 1: Comparative Toxicity Profiles of Inorganic Nanoparticles
| Nanoparticle | Primary Toxic Mechanisms | Key Physicochemical Properties Influencing Toxicity | Observed Toxic Effects (Experimental Models) | Environmental & Health Concerns |
|---|---|---|---|---|
| Silver (AgNPs) | - Generation of Reactive Oxygen Species (ROS) [72] [73].- Release of Ag+ ions [72] [73].- Induction of oxidative stress and inflammation [73]. | - Size [73].- Surface charge [73].- Concentration [72]. | - Growth inhibition in zebrafish (Danio rerio) [72].- Oxidative stress (disrupted SOD, GR activity) in zebrafish liver [72].- Histopathological alterations in liver and intestine [72].- Cytotoxicity and genotoxicity in human lung cells [73]. | |
| Gold (AuNPs) | - Potential to induce DNA damage[cite |
Nanoparticles are broadly classified into inorganic, carbon-based, and organic categories, each with distinct toxicological profiles. Organic nanoparticles, including lipid, polymer, and liposome-based systems, are primarily composed of carbon-based frameworks and are generally perceived to have more favorable safety profiles than their inorganic counterparts due to their biodegradability and biocompatibility [12]. This review objectively compares the performance and safety of these organic nanoparticle systems within the broader context of nanotoxicology research, where a key thesis is that organic nanoparticles typically exhibit reduced long-term accumulation toxicity compared to inorganic nanoparticles, which can persist in biological systems and release toxic ions [74] [12] [5].
The toxicity of nanoparticles is fundamentally governed by their physicochemical properties—size, shape, surface chemistry, and composition—which influence their interactions with biological systems [74] [5]. While inorganic nanoparticles can generate significant reactive oxygen species (ROS) and cause oxidative stress, organic nanoparticles face different safety challenges, including immunogenicity, reactogenicity, and carrier-specific toxicity [5] [75]. Understanding these distinctions is crucial for researchers and drug development professionals selecting appropriate nanocarrier systems for specific therapeutic applications.
Performance and Safety of Major Organic Nanoparticle Classes
Lipid-Based Nanoparticles
Lipid nanoparticles (LNPs) represent a technologically advanced evolution from liposomal systems, characterized by a more complex, less-ordered internal structure that enables efficient nucleic acid encapsulation [76]. Their performance and safety are heavily influenced by individual components, each contributing distinct functionalities and potential toxicities.
Table 1: Key Components of Lipid Nanoparticles and Their Safety Considerations
| Component | Function | Safety Considerations | Recent Advances |
|---|---|---|---|
| Ionizable Lipids | Encapsulate nucleic acids via electrostatic interactions; facilitate endosomal escape through pH-dependent protonation [76] [75]. | May interact with Toll-like receptors (TLRs), posing inflammatory response risks [75]. | Stereochemistry optimization (e.g., (S,S) stereoisomer of ALC-315 shows reduced toxicity); novel lipids like FS01 with superior safety profiles [77] [75]. |
| Phospholipids | Provide structural integrity to the LNP [76] [75]. | Generally biocompatible; composition affects membrane fluidity and stability. | Use of cone-shaped phospholipids like DOPE to enhance membrane fusion and delivery efficiency [75]. |
| Cholesterol | Modulates membrane fluidity, enhances stability, and improves nucleic acid encapsulation [76] [75]. | Natural biological component with minimal inherent toxicity. | Hydroxycholesterol derivatives (e.g., 7α-hydroxycholesterol) improve endosomal escape; cationic cholesterol derivatives alter organ tropism [75]. |
| PEGylated Lipids | Enhance colloidal stability, reduce protein adsorption, and prolong circulation half-life [76] [75]. | Potential immunogenicity; anti-PEG antibodies can cause accelerated blood clearance (ABC) upon repeated administration [75]. | Optimization of PEG chain length and architecture; exploration of PEG alternatives like polysialic acids and zwitterionic polymers [76] [75]. |
Recent research has identified several innovative approaches to enhance LNP performance while mitigating safety concerns. The development of albumin-recruiting LNPs demonstrates significantly reduced liver accumulation and improved lymphatic drainage, potentially enhancing vaccine safety profiles [77]. Furthermore, strategies incorporating biodegradable lipids (e.g., 4A3-SC8) or adding galectin-blocking drugs like thiodigalactoside have shown promise in reducing inflammation associated with RNA delivery, dramatically reducing lung inflammation in ARDS mouse models without harmful side effects [77].
The cellular barriers to efficient LNP delivery have been meticulously characterized through live-cell and super-resolution microscopy, revealing that only a fraction of internalized LNPs trigger endosomal damage conducive to cytosolic RNA release, and surprisingly, many damaged endosomes contain no detectable RNA payload due to component segregation during endosomal sorting [78]. These findings highlight multiple mechanistically distinct barriers to efficient LNP delivery that must be addressed through rational design strategies.
Liposome-Based Systems
Liposomes represent one of the most established organic nanoparticle platforms, with a well-documented history of clinical application. These phospholipid-based vesicles spontaneously self-assemble into bilayered structures enclosing aqueous compartments, enabling co-delivery of both hydrophilic and hydrophobic therapeutics [76] [79].
Table 2: Clinically Marketed Liposomal Formulations and Their Applications
| Drug Name | Active Ingredient | Application | Key Advantages |
|---|---|---|---|
| Arikayce | Amikacin | Lung infections | Enhanced pulmonary delivery; reduced systemic exposure [79]. |
| Doxil | Doxorubicin | Cancer therapy | PEGylated stealth liposome; reduced cardiotoxicity compared to free drug [76]. |
| Vyxeos | Cytarabine/daunorubicin | Acute myeloid leukemia | Fixed-ratio combination therapy; improved efficacy [76]. |
| DepoCyt | Cytarabine | Neoplastic meningitis | Sustained-release formulation for intrathecal use [76]. |
The safety profile of liposomes is significantly influenced by their structural characteristics. Size and lamellarity critically determine biodistribution and clearance pathways, with liposomes in the 50-200 nm range demonstrating optimal circulation half-lives and tissue penetration [76]. Surface modification with anti-fouling polymers like polyethylene glycol (PEG) creates "stealth" characteristics that mitigate rapid clearance by the mononuclear phagocyte system (MPS), though alternative materials including polysialic acids, glycoproteins, and zwitterionic polymers are being explored to address potential PEG immunogenicity [76].
For pulmonary delivery, liposomes face the sophisticated multi-level defense system of the lungs, including physical barriers (mucus and ciliary clearance), biochemical barriers (antimicrobial substances), and cellular immune defenses [79]. The aerodynamic diameter (AD) of liposomal formulations largely determines their deposition pattern, with particles between 1-5 µm optimally depositing in lower airways and alveoli through gravitational sedimentation [79]. This precise targeting is particularly valuable for treating respiratory diseases while minimizing systemic exposure.
Polymer-Based Nanoparticles
While the search results provide limited specific data on polymer nanoparticles, they are classified as organic-based nanomaterials primarily composed of organic matter excluding inorganic-based or carbon-based materials [5]. Comparative analyses indicate that poly(lactic-co-glycolic acid) (PLGA) nanoparticles may exhibit lower biocompatibility and higher immunotoxicity compared to some inorganic nanoparticles, highlighting important safety considerations for polymeric systems [80].
The toxicity of polymer nanoparticles is influenced by multiple physiochemical parameters including size, surface charge, and chemical composition [5]. These factors affect their interactions with plasma membranes, cellular uptake, and potential for generating reactive oxygen species (ROS). Surface functionalization strategies can modulate these interactions but may introduce additional complexity in manufacturing and scalability [80].
Experimental Approaches for Safety Assessment
Key Methodologies in Nanotoxicity Evaluation
Advanced approaches in nanotoxicity assessment employ sophisticated in vitro and in vivo models to elucidate mechanisms of nanoparticle-induced toxicity at cellular and molecular levels [74]. Key methodologies include:
- High-throughput screening techniques that enable rapid toxicity profiling across multiple nanoparticle formulations [74]
- Alternative animal models including zebrafish and C. elegans for preliminary toxicity assessment [74]
- Live-cell and super-resolution microscopy to track nanoparticle intracellular trafficking and endosomal escape efficiency [78]
- Mechanistic studies focusing on oxidative stress, inflammation, genotoxicity, and neurotoxicity pathways [74]
Standardized protocols for nanoparticle synthesis and characterization have been developed to improve reproducibility in toxicity assessment. For instance, researchers have established standardized microfluidic mixing methods using cost-effective equipment to synthesize lipid nanoparticles with high encapsulation efficiency (96-100%) and demonstrated user-to-user reproducibility even with inexperienced personnel [77].
Experimental Protocols for Safety Testing
Protocol 1: Assessing Endosomal Escape Efficiency This protocol evaluates the capability of nanoparticles to deliver their cargo to the cytosol, a critical factor for nucleic acid-based therapies [78]:
- Cell Preparation: Seed appropriate cell lines (e.g., HEK293, HeLa) in imaging-compatible dishes and culture until 70-80% confluent.
- Nanoparticle Treatment: Incubate cells with fluorescently labeled nanoparticles (50 nM siRNA-LNPs or 0.75 µg/mL mRNA-LNPs) for 1-4 hours.
- Galectin Staining: Transfect cells with galectin-9 fluorescent markers to detect endosomal membrane damage.
- Live-Cell Imaging: Use fast live-cell microscopy to track de novo recruitment of galectin-9 to endosomes containing nanoparticles.
- Image Analysis: Quantify the proportion of galectin-9 positive endosomes that contain nanoparticle cargo (hit rate) using single vesicle tracking and fluorescence quantification.
- Functional Validation: Correlate imaging data with biological activity through gene silencing or protein expression assays.
Protocol 2: In Vivo Reactogenicity and Immunogenicity Assessment This protocol evaluates inflammatory responses and immune activation following nanoparticle administration [75]:
- Animal Dosing: Administer nanoparticles to appropriate animal models (typically mice or rats) via relevant route (e.g., intramuscular, intravenous).
- Local Reaction Monitoring: Assess injection site for pain, redness, and swelling at 0, 6, 24, and 48 hours post-administration.
- Systemic Response Evaluation: Monitor body temperature, weight change, and clinical signs of toxicity.
- Cytokine Profiling: Measure serum levels of pro-inflammatory cytokines (IL-6, TNF-α, IFN-γ) at multiple time points.
- Immune Cell Activation: Analyze immune cell populations in draining lymph nodes and spleen using flow cytometry.
- Anti-Drug Antibody Detection: Assess potential antibody formation against nanoparticle components, particularly PEG, using ELISA.
Visualization of Key Concepts
LNP Intracellular Trafficking and Barriers
Diagram 1: LNP Intracellular Trafficking Pathways. This flowchart illustrates the cellular journey of lipid nanoparticles, highlighting key barriers to efficient cytosolic delivery, including endosomal entrapment, component segregation, and membrane repair mechanisms that limit functional nucleic acid delivery [78] [75].
Toxicity Mechanisms of Organic Nanoparticles
Diagram 2: Organic Nanoparticle Toxicity Mechanisms. This diagram outlines primary toxicity pathways for organic nanoparticles, including immune activation, oxidative stress, and inflammatory responses that can lead to adverse effects such as the accelerated blood clearance phenomenon [5] [75].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Organic Nanoparticle Development
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| Ionizable Lipids | pH-dependent charge switching for endosomal escape | DLin-MC3-DMA, ALC-315, C12-200, FS01 [77] [75] |
| Phospholipids | Structural backbone of lipid-based nanoparticles | DSPC, DOPE, phosphatidylcholines (PC) [76] [75] |
| Cholesterol Derivatives | Membrane stability and fluidity modulation | 7α-hydroxycholesterol, Hchol, cationic cholesterol [75] |
| PEGylated Lipids | Steric stabilization, circulation half-life extension | DMG-PEG, DSG-PEG [76] [75] |
| Fluorescent Labels | Nanoparticle tracking and intracellular visualization | BODIPY-MC3, AlexaFluor 647, Cy5 [78] |
| Membrane Damage Sensors | Detection of endosomal membrane disruption | Galectin-9, galectin-3 [78] |
| Microfluidic Equipment | Standardized nanoparticle synthesis | Syringe pumps, commercial microfluidic chips [77] |
Organic nanoparticles—particularly lipid-based systems, liposomes, and polymer nanoparticles—offer versatile platforms for therapeutic delivery with generally favorable safety profiles compared to inorganic alternatives. However, each class presents distinct performance and safety considerations that must be balanced against therapeutic objectives.
The future of organic nanoparticle safety assessment will likely focus on several key areas: First, intrinsically functional nanocarriers that leverage bioactive lipid components rather than complex external modifications may simplify designs while improving targeting specificity [76]. Second, advanced characterization techniques, including super-resolution microscopy and single-vesicle tracking, will provide deeper insights into intracellular trafficking barriers [78]. Finally, standardized toxicity screening platforms that better predict human responses will accelerate the development of safer nanocarriers [74].
As the field progresses, a multidisciplinary approach integrating materials science, toxicology, and pharmacology will be essential to address the complex safety challenges of organic nanoparticles and realize their full potential in biomedical applications [74].
Nanoparticles (NPs), structures with dimensions of 1 to 100 nanometers, are broadly classified into two categories based on their core composition: organic and inorganic [12]. This classification is fundamental, as the core material dictates their fundamental properties, applications, and toxicological profiles [12]. Organic nanoparticles are composed primarily of carbon-based frameworks and include structures such as liposomes, polymeric nanoparticles, dendrimers, and micelles [12] [4]. These are often synthesized from materials like phospholipids, poly(lactic-co-glycolic acid) (PLGA), or chitosan [73]. In contrast, inorganic nanoparticles are formed from non-carbon-based elements and consist of a solid, crystalline core made from metals or metal oxides [3] [12]. Prominent examples include gold nanoparticles (AuNPs), iron oxide nanoparticles (IONPs), silica nanoparticles (SiNPs), and quantum dots (e.g., CdSe) [81] [12] [53]. The distinct nature of their building blocks confers unique sets of advantages and challenges for each class, making them suitable for different niches in nanomedicine, particularly in drug delivery. Understanding their comparative profiles is essential for selecting the appropriate nanocarrier for a specific therapeutic application.
Comparative Analysis: Advantages and Limitations
The choice between organic and inorganic nanoparticles involves a careful trade-off between stability, functionality, biocompatibility, and complexity of design. The table below summarizes their relative advantages and limitations.
Table 1: Comparison of Organic vs. Inorganic Nanoparticles for Drug Delivery
| Aspect | Organic Nanoparticles | Inorganic Nanoparticles |
|---|---|---|
| Core Composition | Carbon-based (e.g., lipids, polymers) [12] | Metals & Metal Oxides (e.g., gold, iron oxide, silica) [12] [53] |
| Structural Stability | Lower physical stability; susceptible to degradation [53] | High physicochemical stability; robust solid core [53] |
| Biodegradability | Generally biodegradable and biocompatible [12] [53] | Often non-biodegradable; potential for long-term accumulation [3] |
| Drug Loading | Encapsulation within a polymeric matrix or lipid core [4] | High loading capacity; surface conjugation or pore encapsulation (e.g., MSNPs) [4] [53] |
| Functionalization | Moderate; surface can be PEGylated or ligand-grafted [4] | Highly tunable surface; easy modification with ligands, antibodies, polymers [3] [53] |
| Unique Properties | Limited intrinsic functionality | Intrinsic optical, magnetic, catalytic properties (e.g., SPR, superparamagnetism) [81] [12] |
| Scalability & Cost | Generally cost-effective and easier to scale [3] | Complex synthesis; can be costly to produce at scale [3] |
| Primary Toxicity Concerns | Immunogenicity, cytotoxicity from polymer degradation products [73] | Oxidative stress, ROS generation, ion leaching, organ accumulation [38] [73] |
Analysis of Comparative Merits and Drawbacks
Organic nanoparticles are prized for their biocompatibility and safety profiles. Liposomes, for instance, are amphiphilic, allowing them to carry both hydrophilic and hydrophobic drugs, and their composition is often similar to that of cell membranes, promoting biodegradability [4]. A key advantage is their ability to reduce toxicity and adverse side effects of encapsulated drugs, as exemplified by Doxil, a PEGylated liposomal doxorubicin formulation that significantly reduces cardiotoxicity [4]. However, limitations include poor stability in storage, short shelf life, and relatively low drug encapsulation efficiency for some types [53].
Inorganic nanoparticles offer distinct advantages rooted in their material science. Their high stability ensures integrity during circulation, and their ease of functionalization allows for precise targeting [53]. Most notably, they possess intrinsic physicochemical properties that enable combined theranostics (therapy + diagnostics). For example, IONPs serve as MRI contrast agents, while AuNPs can be used for photothermal therapy and imaging due to their surface plasmon resonance [81] [12] [53]. The primary drawbacks are their potential toxicity and poor biodegradability. Mechanisms of toxicity include the generation of Reactive Oxygen Species (ROS), which can lead to oxidative stress, inflammation, and DNA damage [38] [73]. Some metal-based NPs can release toxic ions or accumulate in organs, raising concerns for long-term use [38].
Toxicity Profiles: Mechanisms and Influencing Factors
The toxicity of nanoparticles is a critical consideration for their clinical translation. The underlying mechanisms and the factors that influence toxicity differ significantly between organic and inorganic classes.
Mechanisms of Toxicity
The toxicity of inorganic nanoparticles is frequently linked to oxidative stress. When internalized by cells, they can generate reactive oxygen species (ROS), such as free radicals, which overwhelm the cell's antioxidant defenses [38] [73]. This oxidative stress can cause severe cellular damage, including lipid peroxidation, protein oxidation, and DNA strand breaks, ultimately leading to inflammation, mitochondrial dysfunction, and apoptosis (programmed cell death) [38] [73]. A secondary genotoxicity mechanism can occur via persistent inflammatory responses, where activated immune cells release ROS and cytokines, damaging nearby cells and genetic material [38]. Additionally, some metallic NPs (e.g., AgNPs) can leach ions that directly harm cellular components [38].
Organic nanoparticles generally have a lower potential for inducing oxidative stress. Their toxicity is more often related to their biodegradation products and interactions with the immune system. For example, certain polymeric NPs may release acidic degradation products that can cause local irritation or inflammatory responses [73]. Some lipid-based nanoparticles, while considered safe, have the potential to trigger immunotoxic responses or complement activation-related pseudoallergy (CARPA) [73]. The use of cationic surfactants or lipids can increase cytotoxicity by disrupting cell membrane integrity [73].
Factors Influencing Toxicity
The toxicological profile of any nanoparticle is not intrinsic but is heavily influenced by its physicochemical properties.
- Size: Smaller nanoparticles have a larger surface area-to-volume ratio, increasing their reactivity and potential to penetrate biological barriers, leading to higher toxicity [38] [73]. Particles below 10 nm can easily cross the blood-brain barrier [38].
- Shape: The shape of a nanoparticle affects its cellular uptake and interaction. Needle-shaped and high-aspect-ratio fibers have been shown to be more toxic than spherical particles [38].
- Surface Charge: Cationic (positively charged) nanoparticles are typically more toxic than anionic or neutral ones because they exhibit stronger electrostatic interactions with the negatively charged cell membrane, causing more disruption [38] [73].
- Chemical Composition: The core material is a primary determinant. For instance, silver nanoparticles (AgNPs) are known for their antimicrobial activity but can be cytotoxic to human cells, while gold nanoparticles (AuNPs) are generally more biocompatible [73] [53].
Table 2: Key Physicochemical Properties Affecting Nanoparticle Toxicity
| Property | Toxicological Impact | Experimental Evidence |
|---|---|---|
| Size | Smaller particles have higher reactivity, deeper tissue penetration, and increased cellular uptake [38] [73]. | AgNPs of 4.7 nm produced more ROS than 42 nm AgNPs in hepatic and leukemic cell lines [38]. |
| Shape | Shape influences macrophage clearance, cellular internalization, and physical damage [38]. | Needle and plate-shaped hydroxyapatite particles were more toxic than spherical and rod-shaped ones in BEAS-2B cells [38]. |
| Surface Charge | Positive charge enhances membrane interaction and endocytic uptake, increasing cytotoxicity and inflammatory responses [38] [73]. | Cationic lipid NPs using CTAB surfactant show higher cytotoxicity than neutral or anionic counterparts [73]. |
The following diagram illustrates the primary signaling pathways through which inorganic nanoparticles trigger cellular toxicity.
Typical Applications in Drug Delivery
The distinct properties of organic and inorganic nanoparticles have led to their adoption in different drug delivery applications.
Organic Nanoparticles excel in systemic delivery where high biocompatibility and biodegradability are paramount.
- Liposomes: The first FDA-approved nanodrug, Doxil, is a PEGylated liposome for cancer therapy, leveraging the Enhanced Permeability and Retention (EPR) effect for passive tumor targeting [4].
- Polymeric NPs: Made from PLGA or chitosan, they are workhorses for controlled and sustained release of various therapeutics, including proteins and nucleic acids [73].
Inorganic Nanoparticles are chosen for applications requiring additional functionality beyond simple drug carriage.
- Mesoporous Silica Nanoparticles (MSNPs): Their high surface area and tunable pores make them excellent for high drug loading and stimuli-responsive release (e.g., pH-sensitive drug delivery) [4] [53].
- Gold Nanoparticles (AuNPs): Used for targeted cancer theranostics, combining drug delivery with photothermal therapy due to their efficient light-to-heat conversion [53].
- Iron Oxide Nanoparticles (IONPs): FDA-approved for use as MRI contrast agents and for magnetic hyperthermia treatment, often combined with targeted drug delivery [12] [4].
Experimental Protocols for Toxicity Assessment
Robust assessment of nanoparticle toxicity is essential. Below is a generalized protocol for in vitro cytotoxicity assessment, a cornerstone of nanotoxicology.
Standard In Vitro Cytotoxicity and Oxidative Stress Assay
Objective: To evaluate the cell viability and ROS production in a human cell line (e.g., HEK293 kidney cells or HepG2 liver cells) after exposure to organic or inorganic nanoparticles.
Materials and Reagents:
- Test Nanoparticles: Suspensions of organic (e.g., PLGA NPs) and inorganic (e.g., AgNPs, IONPs) nanoparticles at a range of concentrations.
- Cell Line: Adherent human cell line relevant to the exposure route.
- Cell Culture Reagents: Dulbecco's Modified Eagle Medium (DMEM), Fetal Bovine Serum (FBS), penicillin-streptomycin, trypsin-EDTA.
- Assay Kits: MTT or WST-1 cell viability assay kit; DCFDA/H₂DCFDA cellular ROS detection assay kit.
- Equipment: CO₂ incubator, biological safety cabinet, centrifuges, microplate reader, fluorescence microscope.
Methodology:
- Cell Seeding: Seed cells in a 96-well plate at a density of 1x10⁴ cells/well and culture for 24 hours to allow adherence.
- NP Exposure Preparation: Serially dilute nanoparticle stock suspensions in culture medium. Characterize the hydrodynamic size and zeta potential of NPs in the medium prior to exposure.
- Treatment: Remove the medium from the wells and replace it with the NP-containing medium. Include a negative control (medium only) and a positive control (e.g., hydrogen peroxide for ROS assay). Incubate for 24 hours.
- Cell Viability Assay (MTT):
- Add MTT reagent to each well and incubate for 4 hours.
- Solubilize the formed formazan crystals with a solvent (e.g., DMSO).
- Measure the absorbance at 570 nm using a microplate reader. Cell viability is expressed as a percentage of the negative control.
- ROS Detection Assay (DCFDA):
- Load cells with DCFDA dye in serum-free medium and incubate.
- Expose the dye-loaded cells to NPs for a shorter duration (e.g., 2-6 hours).
- Measure fluorescence intensity (Excitation ~485 nm, Emission ~535 nm). Increased fluorescence indicates higher ROS levels.
- Data Analysis: Plot dose-response curves for viability and ROS. Calculate IC₅₀ values and statistically compare the effects of different NP types.
Table 3: The Scientist's Toolkit - Key Reagents for Toxicity Assessment
| Research Reagent / Material | Function in Experiment |
|---|---|
| MTT / WST-1 Assay Kit | Measures cell metabolic activity as a proxy for cell viability. The reagent is reduced by mitochondrial enzymes in living cells to a colored formazan product [38]. |
| DCFDA/H₂DCFDA Kit | Cell-permeable dye that is deacetylated by cellular esterases and then oxidized by ROS to a fluorescent compound, allowing quantification of intracellular ROS levels [38] [73]. |
| PBS (Phosphate Buffered Saline) | Used for washing cells and for preparing nanoparticle suspensions to maintain physiological pH and osmolarity. |
| DMEM with FBS | Standard cell culture medium providing nutrients and growth factors to maintain cells during the exposure period. |
The following diagram visualizes the workflow for this integrated toxicity assessment.
The side-by-side comparison reveals that the dichotomy between organic and inorganic nanoparticles is not about superiority, but about suitability for a specific task. Organic nanoparticles, exemplified by liposomes and polymeric NPs, offer a well-established pathway for enhancing drug solubility, circulation time, and targeted delivery with a strong focus on biocompatibility and biodegradability. Their limitations in stability and functional versatility are often acceptable trade-offs for many systemic drug delivery applications. Conversely, inorganic nanoparticles provide a robust, multi-functional platform where the drug delivery vehicle is also a diagnostic or therapeutic agent in its own right. Their unique optical, magnetic, and electronic properties enable innovative approaches in theranostics and stimuli-responsive therapy, though these advantages come with a more complex toxicological profile that requires rigorous evaluation and sophisticated surface engineering to mitigate risks. For researchers and drug development professionals, the selection criteria must be guided by the therapeutic objective: if the goal is a safe, biodegradable carrier for a known drug, organic NPs are often the default. If the application demands additional functionalities like imaging, external-triggered release, or hyperthermia, inorganic NPs present a compelling, albeit more complex, alternative. Future development will likely focus on hybrid nanoparticles that aim to combine the best attributes of both classes while minimizing their individual limitations.
The application of nanotechnology in medicine has revolutionized drug delivery, diagnosis, and therapeutic interventions. Since the concept gained prominence in the 1980s, the field has witnessed remarkable growth, with the global nanomedicine market projected to reach $358 billion by 2032 [82]. Currently, over 100 nanomedicine products have received regulatory approval, with an additional 563 in various stages of clinical development [64] [82]. This rapid expansion reflects significant scientific and commercial interest in nanomedicine. However, the transition from laboratory research to clinical application has revealed a critical challenge: the dual-faced nature of nanoparticles (NPs) that offers enhanced therapeutic benefits while presenting unique toxicity profiles. This paradox is particularly pronounced when comparing organic and inorganic nanoparticles, whose distinct physicochemical properties dictate both their therapeutic efficacy and their biological safety [83] [84].
The toxicity assessment of nanomedicines represents a complex frontier in pharmaceutical development. While nanocarriers can reduce the toxicity of their active pharmaceutical ingredients by altering biodistribution, they can also relocate toxicity from one organ system to another or introduce new toxicities related to their own components [85]. For instance, the liposomal formulation of doxorubicin (Doxil) mitigates the cardiotoxicity associated with free doxorubicin but introduces new dermatological toxicity in the form of palmar-plantar erythrodysesthesia [85]. Similarly, reformulation of the same drug using cyanoacrylate nanoparticles eliminated both cardiotoxicity and dermatological toxicity but resulted in nephrotoxicity due to altered renal accumulation [85]. These observations underscore the critical importance of comprehensive toxicological profiling throughout the drug development pipeline, from preclinical studies to post-marketing surveillance.
This analysis systematically examines FDA-approved nanomedicines and extracts critical lessons from preclinical investigations, with particular emphasis on the comparative toxicity profiles of organic and inorganic nanoparticles. By synthesizing data from clinical outcomes, preclinical studies, and emerging safety assessment technologies, we provide a framework for optimizing the design of safer nanomedicines.
FDA-Approved Nanomedicines: Clinical Profiles and Toxicity Lessons
Approved Formulations and Their Clinical Impact
The U.S. Food and Drug Administration (FDA) has approved numerous nanomedicines across various therapeutic categories, with cancer treatment representing the dominant indication (approximately 40% of all nanomedicine clinical trials) [82]. These approved formulations can be broadly categorized into several structural classes, each with distinct advantages and documented safety profiles.
Table 1: Major Categories of FDA-Approved Nanomedicines and Representative Examples
| Nanoparticle Type | Composition | Representative FDA-Approved Products | Primary Applications | Notable Toxicity Findings |
|---|---|---|---|---|
| Liposomes | Lipid bilayers | Doxil, Daunoxome, Ambisome | Drug delivery, anticancer, antifungals | Hand-and-Foot Syndrome (Doxil) [85] |
| Polymeric NPs | Polymeric materials | Abraxane (albumin-bound paclitaxel) | Cancer therapy | Reduced anaphylaxis vs. Cremophor-formulated paclitaxel [85] |
| Polymer-Drug Conjugates | Polymer-protein conjugates | PEGylated interferons, Adynovate | Protein delivery, hemophilia | Immunogenicity related to PEG component [85] |
| Antibody-Drug Conjugates | mAb-therapeutic conjugates | Adcetris, Kadcyla | Targeted cancer therapy | Off-target cytotoxic effects |
| Inorganic NPs | Iron oxide, silica | Ferumoxytol, other iron oxide NPs | Imaging, anemia treatment | Complement activation-related pseudoallergy [86] |
Liposomal formulations represent one of the most successful categories of approved nanomedicines. Doxil, a PEGylated liposomal doxorubicin, exemplifies both the benefits and challenges of nanomedicine. While it successfully mitigates the cardiotoxicity associated with free doxorubicin through altered biodistribution, it introduces a new dermatological toxicity—palmar-plantar erythrodysesthesia (Hand-and-Foot Syndrome)—due to accumulation in skin dendritic cells [85]. This phenomenon of "toxicity relocation" highlights how nanoparticle-driven alterations in drug disposition can unexpectedly shift adverse effects to new anatomical sites rather than eliminating them entirely.
Another instructive case comes from the reformulation of paclitaxel. The original formulation (Taxol) utilized Cremophor EL as a solvent, which frequently caused severe hypersensitivity reactions requiring premedication and prolonged infusion times. The nanoalbumin-formulated paclitaxel (Abraxane) eliminated this excipient-related toxicity, demonstrating improved safety profile without inducing anaphylactoid reactions [85]. This case underscores how nanomedicine can address excipient-related toxicities while maintaining therapeutic efficacy.
Immunological Considerations for Approved Nanomedicines
The interaction between nanomedicines and the immune system represents a critical determinant of both safety and efficacy. Contrary to early approaches that focused solely on hiding nanoparticles from immune recognition, contemporary understanding recognizes that strategic engagement with the immune system can enhance therapeutic outcomes [85]. For instance, Doxil has been shown to stimulate anticancer immune responses, leading to improved efficacy when combined with immune-checkpoint inhibitors in colorectal cancer models [85].
However, immune recognition can also drive adverse effects. Nanoparticles can trigger inflammatory responses through multiple mechanisms, including complement activation, reactive oxygen species (ROS) generation, and chemokine induction [85]. Lipid-based nanocarriers commonly induce chemokine IL-8, which recruits leukocytes and contributes to inflammatory responses [85]. Similarly, cationic polymeric molecules like dendrimers can activate intracellular complement, which plays a critical role in regulating T-cell activation [85] [86]. These immunomodulatory effects necessitate careful evaluation during nanomedicine development, particularly as combinations with immunotherapies become more prevalent.
Preclinical Studies: Inorganic vs. Organic Nanoparticle Toxicity
Differential Toxicity Profiles
Preclinical studies have revealed fundamental differences in the toxicity profiles of inorganic versus organic nanoparticles, largely attributable to their distinct material properties, biodegradation pathways, and biological interactions. While organic nanoparticles (including liposomes, polymeric NPs, and lipid-based systems) generally exhibit favorable biodegradability profiles, they can still induce immune reactions and alter the biodistribution of their payloads with consequent toxicological implications [85] [87].
Inorganic nanoparticles (including gold, silica, and iron oxide NPs) present unique challenges due to their potential for prolonged persistence in biological systems. These materials often demonstrate delayed clearance and different degradation pathways compared to their organic counterparts [83]. For instance, mesoporous silica nanoparticles (MSNPs), while promising for their excellent drug loading capacity and controlled release profiles, have raised concerns regarding their long-term fate in biological systems [88]. The degradation products of inorganic NPs can potentially trigger oxidative stress and disrupt cellular processes through DNA damage, membrane disruption, and apoptosis [83].
Table 2: Comparative Toxicity Profiles of Organic and Inorganic Nanoparticles Based on Preclinical Studies
| Toxicity Parameter | Organic Nanoparticles | Inorganic Nanoparticles |
|---|---|---|
| Primary Clearance Pathways | Metabolic degradation, renal clearance | RES uptake, delayed degradation |
| Common Toxicities | Immunogenicity, complement activation, toxicity relocation | Oxidative stress, granulomatous inflammation, organ accumulation |
| Key Influencing Factors | Lipid composition, surface PEGylation, size | Core material, surface chemistry, aspect ratio |
| Degradation Profile | Generally biodegradable with predictable pathways | Variable degradation; potential for persistent residues |
| Immune Interactions | Opsonization, complement activation, immunomodulation | ROS generation, inflammasome activation, protein corona effects |
Mechanistic Insights into Nanotoxicity
At the cellular level, both organic and inorganic nanoparticles can trigger oxidative stress through generation of reactive oxygen species (ROS), though through somewhat different mechanisms [83] [84]. Inorganic nanoparticles often directly participate in redox reactions due to their metallic composition or surface properties, while organic nanoparticles typically induce oxidative stress indirectly through immune cell activation or mitochondrial disruption.
The mechanism of genotoxicity also differs between nanoparticle classes. Studies have shown that inorganic nanoparticles like silver and zinc oxide can cause DNA damage through direct interaction or secondary oxidative stress [83]. In contrast, organic nanoparticles less frequently cause direct genotoxicity but may indirectly affect genetic material through chronic inflammation or oxidative stress pathways [85] [84].
The concept of "nanotoxicity" extends beyond cellular damage to include complex bio-interactions at the systemic level. Nanoparticles can alter the pharmacokinetics and biodistribution of their therapeutic payloads, potentially leading to unexpected patterns of toxicity. Furthermore, individual components of nanoparticles and commonly used excipients are not immunologically inert and contribute to the overall immune responses to nanotechnology-formulated products [85]. For example, the PEG component of many stealth nanoparticles has been associated with the development of anti-PEG antibodies that can accelerate blood clearance and reduce efficacy upon repeated administration.
Advanced Methodologies for Toxicity Assessment
Experimental Protocols for Nanotoxicity Evaluation
Comprehensive assessment of nanoparticle toxicity requires a multifaceted approach that evaluates both cellular and systemic responses. Standardized protocols have emerged for evaluating key toxicity parameters:
Cytotoxicity Assessment: In vitro cytotoxicity is typically evaluated using cell viability assays (MTT, XTT, WST-1) after 24-72 hours of exposure to nanoparticles across a concentration range (often 0-100 μg/mL) [83] [88]. The ISO 10993-5 standard, which classifies samples with less than 70% viability as toxic, provides a benchmark for these assessments [83]. Additional endpoints include membrane integrity (LDH release), apoptosis/necrosis (Annexin V/PI staining), and oxidative stress markers (DCFH-DA for ROS, GSH depletion).
Hemocompatibility Testing: For intravenous formulations, assessment of blood compatibility is essential. This includes evaluation of complement activation (C3a, C5a, SC5b-9 measurements), hemolysis (plasma hemoglobin), and platelet activation (flow cytometry for P-selectin) [86]. Recent studies have identified iptacopan, an FDA-approved complement inhibitor, as particularly effective in reducing nanoparticle-induced complement activation in preclinical models [86].
Immunotoxicity Screening: Comprehensive immunotoxicity assessment includes evaluation of cytokine release (IL-1β, IL-6, IL-8, TNF-α), phagocyte activation (oxidative burst, surface marker expression), and complement activation pathways (classical, alternative, lectin) [85] [86]. Human whole blood models provide a more complete picture of immune interactions than isolated cell systems.
In Vivo Biodistribution and Toxicity: Preclinical in vivo studies typically utilize rodent models to evaluate organ-specific accumulation and toxicity. Techniques include quantitative biodistribution using radiolabeled nanoparticles, histological assessment of major organs (liver, spleen, kidneys, lungs), and clinical pathology (serum biochemistry, hematology) [87] [88]. Special attention is paid to organs of the mononuclear phagocytic system (liver, spleen), which tend to accumulate nanoparticles.
Innovative Approaches: PBPK Modeling and Machine Learning
Traditional toxicity assessment methods are increasingly supplemented with innovative computational approaches. Notably, integrating physiologically-based pharmacokinetic (PBPK) modeling with machine learning (ML) has emerged as a powerful framework for predicting nanotoxicity [83].
PBPK models quantify nanoparticle exposure across different organs by simulating absorption, distribution, metabolism, and excretion processes. When combined with ML algorithms trained on large curated datasets of nanoparticle properties and toxicity outcomes, this integrated approach can predict organ-specific toxicity risks based on physicochemical parameters [83]. In one recent development, a machine-learning framework was trained on a curated dataset of 8,190 samples from 425 studies to predict nanoparticle toxicity both in vitro and in vivo [83]. The model identified critical toxicity determinants including particle size, concentration, surface coating, ζ-potential, and exposure time.
The following diagram illustrates this integrated PBPK-ML workflow for nanotoxicity prediction:
This computational approach represents a Novel Alternative Method (NAM) that can streamline safety assessment and enable rational design of safer nanoparticles by establishing quantitative structure-toxicity relationships [83].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Nanomedicine Toxicity Assessment
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Cetyltrimethylammonium bromide (CTAB) | Structure-directing surfactant | Template for mesoporous silica NP synthesis [88] |
| Polyethylene glycol (PEG) | Stealth coating polymer | Improves circulation half-life, reduces opsonization [64] [85] |
| Pluronic F127 | Block copolymer surfactant | Template for nanoparticle synthesis, stabilizer [88] |
| Tetraethyl orthosilicate (TEOS) | Silica precursor | Synthesis of mesoporous silica nanoparticles [88] |
| Iptacopan | Complement inhibitor | Mitigates nanoparticle-induced complement activation [86] |
| MTT/XTT/WST-1 assays | Cell viability indicators | In vitro cytotoxicity screening [83] |
| DCFH-DA | ROS-sensitive fluorescent probe | Measurement of oxidative stress [83] |
| Annexin V/PI | Apoptosis/necrosis markers | Flow cytometry analysis of cell death mechanisms [84] |
The experimental workflow for comprehensive nanotoxicity assessment integrates these reagents in a systematic fashion, as illustrated below:
The analysis of FDA-approved nanomedicines and preclinical studies yields several strategic insights for developing safer nanoparticle-based therapeutics. First, the relocation of toxicity observed with reformulated drugs underscores the necessity for comprehensive organ-specific toxicity assessment beyond simply evaluating known toxicities of the active pharmaceutical ingredient. Second, the distinct toxicity profiles of organic versus inorganic nanoparticles highlight the importance of material-specific safety evaluation protocols. Finally, the emerging understanding of nanoparticle-immune system interactions suggests both challenges and opportunities for leveraging these interactions therapeutically.
The integration of advanced computational approaches like PBPK-ML modeling represents a paradigm shift in nanotoxicity assessment, moving from descriptive toxicology to predictive safety science [83]. These tools, combined with robust experimental validation and careful attention to individual component toxicology, will accelerate the development of sophisticated nanomedicines with optimized therapeutic indices. As the field progresses toward more complex multifunctional nanoparticles, these lessons from both approved products and preclinical investigations will provide an essential foundation for responsible innovation in nanomedicine.
Conclusion
The journey toward clinically successful nanomedicines hinges on a deep and nuanced understanding of nanoparticle toxicity. This analysis confirms that toxicity is not an intrinsic property of a material class but is profoundly influenced by a suite of modifiable physicochemical properties. While inorganic nanoparticles often face scrutiny due to their potential for metal ion leaching and ROS generation, and organic nanoparticles challenge researchers with stability and immunogenicity concerns, both classes can be engineered for enhanced safety. Future progress depends on a multidisciplinary approach, integrating advanced material science with robust, standardized toxicological assessments. Closing the translational gap will require a concerted focus on developing predictive models, comprehensive long-term toxicity data, and adaptive regulatory frameworks that keep pace with innovation, ultimately ensuring the development of nanotherapeutics that are not only effective but also unequivocally safe for patients.
References
- 1. Organic and inorganic nanomaterials: fabrication, properties ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10162010/]
- 2. Nanomaterial toxicity: a comprehensive review of ... [https://link.springer.com/article/10.1007/s44475-025-00003-2]
- 3. Biogenic nanoparticles as a promising drug delivery system [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762933/]
- 4. Organic vs. Inorganic Nanomaterials for Drug Delivery ... [https://www.azonano.com/article.aspx?ArticleID=5855]
- 5. Structural parameters of nanoparticles affecting their toxicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9970140/]
- 6. An overview on nanoparticles used in biomedicine and ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224720316051]
- 7. Inorganic Nanoparticles-Based Systems in Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9833678/]
- 8. Long-term toxic effects of nanoparticles on human microbiota [https://www.sciencedirect.com/science/article/abs/pii/S0946672X25001361]
- 9. Human and environmental impacts of nanoparticles: a scoping review of the current literature | BMC Public Health | Full Text [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-023-15958-4]
- 10. Nanoparticles‐induced potential toxicity on human health [https://pmc.ncbi.nlm.nih.gov/articles/PMC10349198/]
- 11. Toxicity of metal-based nanoparticles: Challenges in the ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.1001572/full]
- 12. A Comprehensive Review of Nanoparticles: From Classification to Application and Toxicity [https://www.mdpi.com/1420-3049/29/15/3482]
- 13. Machine learning-driven nanoparticle toxicity [https://pubmed.ncbi.nlm.nih.gov/40393320/]
- 14. Density of surface charge is a more predictive factor of the ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-020-00747-7]
- 15. Natural inorganic nanoparticles--formation, fate, and toxicity in the environment - PubMed [https://pubmed.ncbi.nlm.nih.gov/26435358/]
- 16. Recent Advances in the Gastrointestinal Fate of Organic and Inorganic Nanoparticles in Foods - PubMed [https://pubmed.ncbi.nlm.nih.gov/35407216/]
- 17. Mechanisms of Nanoparticle-Induced Oxidative Stress and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3762079/]
- 18. Toxicity of Nanoparticles and an Overview of Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4689276/]
- 19. Estimation of genotoxicity, apoptosis and oxidative stress ... [https://www.nature.com/articles/s41598-022-23302-w]
- 20. Toxicity and transport of nanoparticles in agriculture: effects ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1622228/full]
- 21. Review Biomarkers of oxidative stress, inflammation, and ... [https://www.sciencedirect.com/science/article/pii/S0147651323011491]
- 22. SURFACE CHEMISTRY INFLUENCE IMPLANT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3230929/]
- 23. Recent advances in surface decoration of nanoparticles ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2024.1456939/full]
- 24. Biocompatibility and Biological Effects of Surface-Modified ... [https://www.mdpi.com/1420-3049/28/5/2034]
- 25. 4.4 Surface Modification and Functionalization [https://fiveable.me/cell-and-tissue-engineering/unit-4/surface-modification-functionalization/study-guide/iidfFqVP9GtjQIWA]
- 26. Pharmacokinetics and toxicity of inorganic nanoparticles ... [https://www.sciencedirect.com/science/article/pii/S1773224724006488]
- 27. Nanoparticle Surface Functionalization: How to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7726445/]
- 28. Nanoparticle Surface Functionalization: How to Improve ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.587012/full]
- 29. 25 years of research and regulation: Is nanotechnology ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1629813/full]
- 30. In vitro toxicity model: Upgrades to bridge the gap between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7202182/]
- 31. Understanding Assay Performance Metrics [https://indigobiosciences.com/understanding-assay-performance-metrics/]
- 32. Performance metrics of in vitro tests - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6785777/]
- 33. The Extended ToxTracker Assay Discriminates Between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5009621/]
- 34. Understanding the Molecular Toxicity of Metal-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595969/]
- 35. Toxicity of Nanoparticles in Biomedical Application [https://pmc.ncbi.nlm.nih.gov/articles/PMC8376461/]
- 36. Silica nanoparticle toxicity: cellular mechanisms, ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1629722/full]
- 37. Multimodal approach to nanoparticle toxicity assessment ... [https://pubmed.ncbi.nlm.nih.gov/41204622/]
- 38. Toxicological assessment and risk management of ... [https://link.springer.com/article/10.1007/s44347-025-00023-7]
- 39. The potential adverse human health effects of metal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628871/]
- 40. Nanotechnologies: 6. What are potential harmful effects of... [https://ec.europa.eu/health/scientific_committees/opinions_layman/en/nanotechnologies/l-2/6-health-effects-nanoparticles.htm]
- 41. Toxic mechanisms of nanoparticle-induced ferroptosis and ... [https://pubmed.ncbi.nlm.nih.gov/41161466/]
- 42. Is nano safe in foods? Establishing the factors impacting the... [https://www.nature.com/articles/s41538-017-0005-1?error=cookies_not_supported&code=79bacac3-872e-4552-8b42-17a9638e4aa4]
- 43. of Comparative , toxicity and nanoparticulate zinc... organic inorganic [https://pubmed.ncbi.nlm.nih.gov/30625650/]
- 44. Navigating complexity in modern toxicology: the role of omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599865/]
- 45. Omics in Short-Term Toxicology Studies: Are We Ready to ... [https://alitheagenomics.com/blog/omics-in-short-term-toxicology-studies-are-we-ready-to-replace-traditional-approaches]
- 46. High-Throughput Screening - Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-principles-applications-and-advancements-405121]
- 47. High Throughput Screening (HTS) Market Size 2025-2029 [https://www.technavio.com/report/high-throughput-screening-market-industry-analysis]
- 48. High-throughput Screening Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/high-throughput-screening-market]
- 49. A systems biology approach to understand temporal ... [https://www.nature.com/articles/s41540-025-00561-7]
- 50. Bridging In Vitro and In Vivo Inhalation Toxicity [https://www.sciencedirect.com/science/article/abs/pii/S0269749125017166]
- 51. Evaluation of a high-throughput in-vitro-to-in-vivo ... [https://pubmed.ncbi.nlm.nih.gov/40434282/]
- 52. Comprehensive benchmarking of computational tools for ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-024-00931-z]
- 53. Exploration of inorganic nanoparticles for revolutionary ... [https://link.springer.com/article/10.1186/s11671-023-03943-0]
- 54. Surface modifications of biomaterials in different applied ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10331796/]
- 55. Research and prospects of strategies for surface-modified ... [https://link.springer.com/article/10.1007/s44258-025-00056-4]
- 56. Green Toxicology: a strategy for sustainable chemical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5380705/]
- 57. Engineering nanoparticles to overcome barriers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5689503/]
- 58. Toxicity and biodistribution comparison of functionalized ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1512622/full]
- 59. From the properties of nanocores to the differential effects ... [https://www.sciencedirect.com/science/article/pii/S0169409X23001448]
- 60. Data-Driven Prediction of Nanoparticle Biodistribution from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312149/]
- 61. Multifunctional nanoparticle-mediated combining therapy ... [https://www.nature.com/articles/s41392-023-01668-1]
- 62. Toxicity Classification of Oxide Nanomaterials: Effects ... [https://www.nature.com/articles/s41598-018-21431-9]
- 63. Frontiers | Regulatory pathways and guidelines for nanotechnology-enabled health products: a comparative review of EU and US frameworks [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1544393/full]
- 64. Nanopharmaceuticals and nanomedicines currently on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6391637/]
- 65. Regulating nanomedicines: challenges, opportunities, and ... [https://pubmed.ncbi.nlm.nih.gov/40657903/]
- 66. Inorganic Nanoparticles: Toxic Effects, Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9675927/]
- 67. Updated Regulatory Considerations for Nanomedicines - PubMed [https://pubmed.ncbi.nlm.nih.gov/28641516/]
- 68. the transformative potential of nanotechnology in medicine [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1556426/full]
- 69. Effect of organic-ligands on the toxicity profiles of CdS ... [https://www.sciencedirect.com/science/article/pii/S0927776514007310]
- 70. Nanomedicine: How nanomaterials are transforming drug ... [https://www.sciencedirect.com/science/article/pii/S2949829524000901]
- 71. Top 11 Nanotoxicology papers published in 2025 [https://scispace.com/journals/nanotoxicology-34mmqqt3/2025]
- 72. Toxicological effects of dietary silver nanoparticles (AgNPs) ... [https://www.sciencedirect.com/science/article/abs/pii/S0025326X2500829X]
- 73. The Toxicological Profile of Active Pharmaceutical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12115128/]
- 74. Recent approaches in nanotoxicity assessment for drug ... [https://www.sciencedirect.com/science/article/pii/S2590098625000016]
- 75. Recent Advances in Lipid Nanoparticles and Their Safety ... [https://www.mdpi.com/2076-393X/12/10/1148]
- 76. More than a delivery system: the evolving role of lipid-based ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04508d]
- 77. Lipid Nanoparticle News and Research Summary (July 29 [https://www.precigenome.com/post/lipid-nanoparticle-news-and-research-summary-july-29-august-18-2025?srsltid=AfmBOoojYvYWnUKSx98B2C-1s5Heu2_yg-7QXi9Z84ZuKQpAaKLhOak3]
- 78. Cellular and biophysical barriers to lipid nanoparticle ... [https://www.nature.com/articles/s41467-025-60959-z]
- 79. Liposome-Based Nanoparticle Delivery Systems for Lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535190/]
- 80. A comprehensive review of using nanomaterials in cancer ... [https://pubmed.ncbi.nlm.nih.gov/40502964/]
- 81. Self-assembled inorganic nanomaterials for biomedical ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04537h]
- 82. Nanomedicine Statistics and Facts (2025) [https://media.market.us/nanomedicine-statistics/]
- 83. Rational Design of Safer Inorganic Nanoparticles via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11875313/]
- 84. The nano-paradox: addressing nanotoxicity for sustainable ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03371-5]
- 85. Lessons learned from immunological characterization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9592561/]
- 86. FDA-approved drugs can help enhance the safety of ... [https://www.news-medical.net/news/20250709/FDA-approved-drugs-can-help-enhance-the-safety-of-nanomedicines.aspx]
- 87. Overview of Preclinical and Clinical Trials of Nanoparticles ... [https://www.mdpi.com/1999-4923/17/7/899]
- 88. Fabrication, biodistribution, and toxicological evaluation of ... [https://japsonline.com/abstract.php?article_id=4559&sts=2]