Optimizing Nanocarrier Distribution at Single-Cell Resolution: Pathways to Precision Therapeutics
This article explores the frontier of controlling nanocarrier distribution with single-cell precision, a critical challenge in targeted drug delivery.
Optimizing Nanocarrier Distribution at Single-Cell Resolution: Pathways to Precision Therapeutics
Abstract
This article explores the frontier of controlling nanocarrier distribution with single-cell precision, a critical challenge in targeted drug delivery. It examines the foundational principles governing nanocarrier design and in vivo journey, highlighting the limitations of conventional biodistribution analysis methods. The content details a groundbreaking methodological pipeline, SCP-Nano, which integrates tissue clearing, light-sheet microscopy, and deep learning to achieve whole-body, single-cell resolution mapping of nanocarriers. It further addresses key troubleshooting and optimization strategies for mitigating off-target effects and enhancing specificity, and concludes with validation frameworks and a comparative analysis of nanocarrier platforms. Designed for researchers, scientists, and drug development professionals, this resource provides a comprehensive roadmap for advancing the development of precise and safe nanocarrier-based therapeutics.
The Foundation of Single-Cell Targeting: Principles and Challenges of Nanocarrier Biodistribution
In single-cell research, achieving precise intracellular delivery is paramount. The journey of a nanocarrier from administration to its intracellular target is predominantly governed by three key physicochemical properties: size, surface charge, and hydrophobicity. These properties act as a master control panel, directly influencing cellular uptake pathways, intracellular trafficking, and ultimately, the therapeutic efficacy of the delivered cargo. A systems-level understanding of these parameters is essential to overcome biological barriers and optimize distribution for single-cell applications [1] [2]. This guide provides troubleshooting resources to help researchers navigate the complex bio-nano interface.
Troubleshooting Guides: Optimizing Key Properties
Troubleshooting Size-Related Issues
The size of a nanocarrier is a critical determinant of its cellular internalization mechanism and rate [3] [4].
Table 1: Size-Related Challenges and Solutions
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low Cellular Uptake | Size too small (<50 nm) leading to insufficient phagocytic stimulus [3]. | Increase particle size to the optimal range of 100-200 nm for phagocytic pathways [3] [4]. |
| Rapid Clearance by MPS | Size too large (>200 nm) for intravenous administration, leading to mechanical filtration and high opsonization [3] [4]. | Reduce particle size to below 200 nm and consider surface PEGylation to reduce opsonin adsorption [4]. |
| Poor Target Tissue Penetration | Large size hindering diffusion through tissue extracellular matrix [4]. | Utilize smaller particles (<100 nm) and consider shape engineering (e.g., rod-shaped) for improved penetration [4]. |
| Polydisperse Formulations | Aggregation or inconsistent synthesis methods [5]. | Optimize preparation methods; implement purification techniques like asymmetric flow field-flow fractionation (AF4) [5]. |
Key Experimental Protocol: Measuring Particle Size and Distribution via Dynamic Light Scattering (DLS) DLS determines the hydrodynamic diameter of particles based on their Brownian motion in a suspension [5] [6].
- Sample Preparation: Dilute the nanocarrier suspension in an appropriate, filtered buffer to obtain a clear, slightly opalescent solution. Ensure the viscosity of the dispersion medium is known [5] [7].
- Instrument Calibration: Use a standard of known size (e.g., latex beads) to calibrate the DLS instrument.
- Measurement: Load the sample into a disposable cuvette and place it in the instrument. Set the measurement temperature (typically 25°C).
- Data Analysis: Perform the measurement in triplicate. The instrument's software will provide the z-average diameter (a intensity-weighted mean size) and the Polydispersity Index (PDI). A PDI value below 0.2 is generally considered monodisperse [5] [7]. For polydisperse samples, a distribution analysis provides a more accurate picture of the subpopulations present.
Troubleshooting Surface Charge (Zeta Potential) Issues
The surface charge, quantified as zeta potential, dictates electrostatic interactions with cell membranes and proteins, affecting stability and uptake [5] [6].
Table 2: Surface Charge-Related Challenges and Solutions
| Problem | Possible Cause | Recommended Solution | ||||||
|---|---|---|---|---|---|---|---|---|
| Particle Aggregation in Storage | Low zeta potential magnitude ( | ζ | < 20 mV) leading to insufficient electrostatic repulsion [5]. | Modify surface chemistry to increase the absolute zeta potential. For cationic particles, ensure | ζ | > +20 mV; for anionic, | ζ | > -20 mV [5]. |
| Non-Specific Cellular Uptake & Toxicity | Highly positive surface charge causing non-specific binding to anionic cell membranes [4] [1]. | Shield the positive charge using PEG or other hydrophilic polymers; aim for a near-neutral or slightly negative charge for reduced non-specific interaction [4]. | ||||||
| Rapid Clearance from Bloodstream | Surface charge promoting opsonin protein adsorption [3] [4]. | Create a stealth surface with neutral, hydrophilic coatings (e.g., PEG) to minimize protein corona formation and phagocytosis [3] [4]. | ||||||
| Inefficient Endosomal Escape | Lack of ionizable cationic lipids that become protonated in the acidic endosomal environment [1]. | Incorporate ionizable lipids with pKa ~6.5 to facilitate the "proton sponge" effect and disrupt the endosomal membrane [1]. |
Key Experimental Protocol: Determining Zeta Potential via Electrophoretic Light Scattering Zeta potential is measured by applying an electric field across the sample and measuring the velocity of particle movement (electrophoretic mobility) using laser Doppler velocimetry [5] [7].
- Sample Preparation: Dilute nanocarriers in a low-concentration salt solution (e.g., 1 mM KCl) or a specific buffer that matches the intended application. The ionic strength and pH of the dispersion medium must be controlled and reported, as they significantly influence the result [5].
- Measurement: Use a disposable folded capillary cell or a dedicated zeta cell. The instrument calculates the zeta potential from the measured electrophoretic mobility.
- Data Analysis: Conduct a minimum of three measurements and report the average value and standard deviation. The accuracy and precision for a suitable sample should be better than 10% on a calibrated instrument [7].
Troubleshooting Hydrophobicity-Related Issues
Hydrophobicity influences protein adsorption, cellular adhesion, and the mechanism of membrane translocation [1] [2].
Table 3: Hydrophobicity-Related Challenges and Solutions
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Rapid Opsonization and Clearance | Hydrophobic surfaces strongly adsorb blood plasma proteins (opsonins) [3] [4]. | Conjugate hydrophilic polymers (e.g., PEG) to create a hydration layer that sterically shields the hydrophobic core [3] [4]. |
| Membrane Embedment without Translocation | Excessively hydrophobic ligands causing nanoparticles to become trapped within the lipid bilayer [1] [2]. | Fine-tune ligand chemistry by incorporating hydrophilic segments (e.g., PEG) or using less hydrophobic alkyl chains to promote full translocation [1] [2]. |
| Poor Loading of Hydrophilic Drugs | Hydrophobic core or matrix incompatible with water-soluble agents. | Switch to nanocarriers with aqueous compartments (e.g., liposomes, nanocapsules) or use surfactants to create nanoemulsions [3]. |
| Low Colloidal Stability in Aqueous Media | High surface hydrophobicity driving aggregation to minimize water contact. | Use stabilizers and surfactants (e.g., polysorbates) during formulation to enhance dispersibility [5]. |
Key Experimental Protocol: Assessing Hydrophobicity via Hydrophobic Interaction Chromatography (HIC) This method probes surface hydrophobicity based on interaction with a hydrophobic stationary phase.
- Column Selection: Pack a column with a HIC medium (e.g., butyl or phenyl Sepharose).
- Equilibration: Equilibrate the column with a high-salt buffer (e.g., 1.5 M ammonium sulfate) to promote binding.
- Sample Application & Elution: Apply the nanocarrier sample. Elute using a descending salt gradient or with a salt-free buffer. The strength of hydrophobic interaction is inversely related to the salt concentration required for elution.
- Detection: Monitor elution via UV-Vis, fluorescence, or light scattering detectors. More hydrophobic particles will elute at lower salt concentrations.
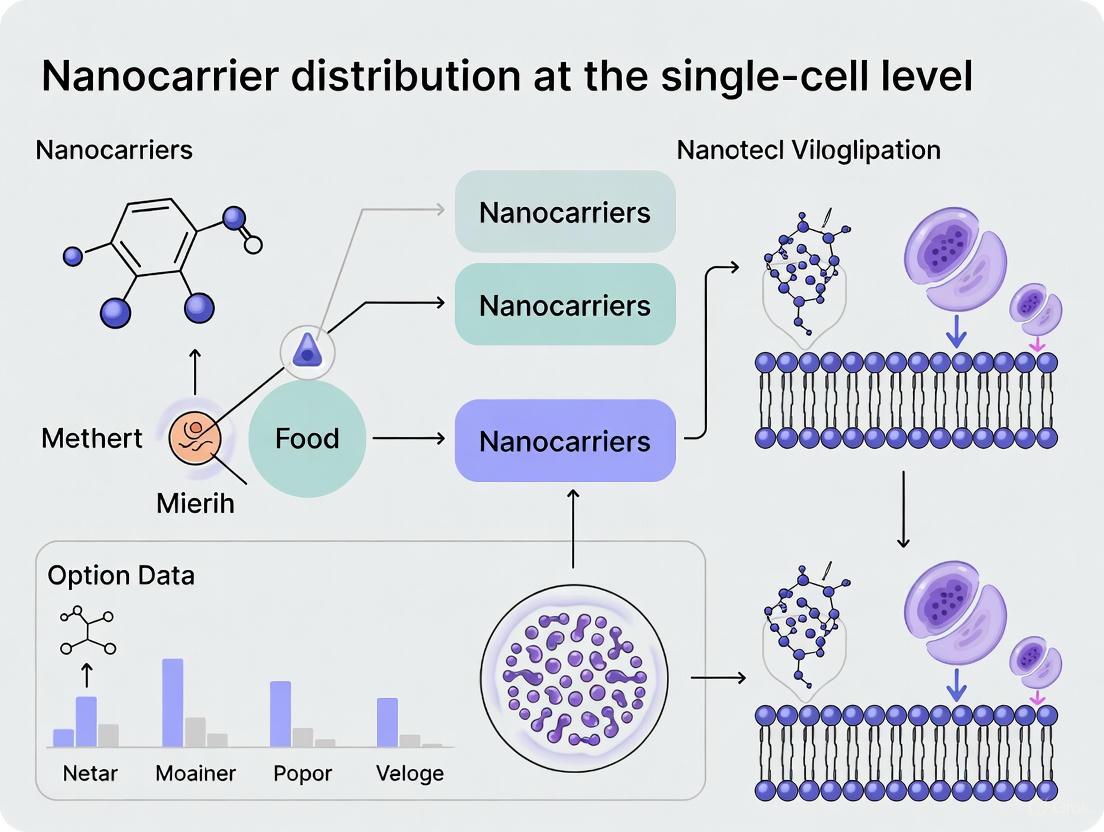
Visualizing the Synergistic Effect on Cellular Entry
The cellular entry pathway is not determined by a single property but by the synergy between size, surface charge, and ligand chemistry (hydrophobicity). Computational studies have identified four primary translocation outcomes, which dictate subsequent intracellular trafficking and fate [1] [2].
Diagram: Synergistic Control of Nanocarrier Entry Pathways. The cellular entry pathway is determined by the interplay of size, surface charge, and ligand hydrophobicity, leading to distinct intracellular fates [1] [2].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Reagents for Nanocarrier Synthesis and Characterization
| Reagent/Material | Function/Purpose | Example Use Case |
|---|---|---|
| Ionizable Lipids | Key functional component of LNPs; protonates in acidic endosomes to enable membrane disruption and cytosolic release. | mRNA vaccine delivery (e.g., DLin-MC3-DMA) [8]. |
| Phospholipids (e.g., DPPC) | Form the primary bilayer structure of liposomes, providing a biocompatible scaffold. | Model cell membrane studies; creating the main structural matrix of lipid-based nanocarriers [1] [2]. |
| Polyethylene Glycol (PEG)-Lipids | Shield the surface to reduce protein adsorption (stealth effect), prolong circulation time, and prevent aggregation. | Surface PEGylation of liposomes and LNPs to enhance stability and reduce MPS uptake (e.g., in Doxil) [4] [8]. |
| Cholesterol | Incorporated into lipid bilayers to enhance membrane stability and rigidity, modulating fluidity and permeability. | A standard component in LNP formulations to improve structural integrity and in vivo stability [8]. |
| Dynamic Light Scattering (DLS) Instrument | Measures hydrodynamic particle size distribution and polydispersity index (PDI) in solution. | Routine quality control of nanocarrier size and stability after synthesis [5] [6]. |
| Zeta Potential Analyzer | Determines the surface charge of particles in suspension, predicting colloidal stability. | Assessing the success of surface modifications and the potential for aggregation [5] [7]. |
| Transmission Electron Microscopy (TEM) | Provides high-resolution imaging of nanocarrier morphology, size, and internal structure. | Visualizing the core-shell structure of nanocapsules or the lamellarity of liposomes [5] [6]. |
Frequently Asked Questions (FAQs)
Q1: My nanocarriers are the right size (~150 nm) but are still not being internalized by my target cell line. What could be wrong? A: Size is only one factor. Check the surface charge. Highly negative surfaces may experience electrostatic repulsion from the anionic cell membrane. Consider modifying the surface with cationic lipids or cell-penetrating peptides to enhance adhesion. Also, verify that your target cells are professional phagocytes if relying on that pathway; many are not [3] [4].
Q2: I am trying to achieve cytosolic delivery for gene editing, but my cargo remains trapped in endosomes. How can I promote endosomal escape? A: This is a common hurdle. Your nanocarriers are likely entering via the "outer wrapping" pathway (endocytosis). To shift towards "free translocation," you need to:
- Incorporate ionizable lipids with a pKa around 6.5. These become protonated in the acidic endosome, leading to membrane destabilization.
- Optimize the synergy: Smaller sizes and higher surface charge/ionization promote pore formation and direct translocation across the membrane, bypassing endosomes [1] [2].
Q3: How does the PEG density on my lipid nanoparticles affect their performance? A: PEG density is a critical balance. While PEG reduces opsonization and extends circulation time, excessive PEGylation can create a steric barrier that inhibits cellular uptake and endosomal escape—a phenomenon known as the "PEG dilemma." Use a minimal amount of PEG-lipid necessary for stability, and consider using cleavable PEG links that shed after the nanocarrier reaches the target site [4] [8].
Q4: My nanoparticle formulation is unstable and aggregates over time. What are the primary factors to check? A: Instability is often linked to surface properties. First, measure the zeta potential. An absolute value below 20-25 mV indicates insufficient electrostatic repulsion to prevent aggregation. Second, assess the surface hydrophobicity, as hydrophobic patches can drive aggregation. Solutions include increasing surface charge via formulation or adding steric stabilizers like PEG [5] [6].
Frequently Asked Questions
FAQ 1: Why can't I detect my nanocarriers in low-dose applications, like vaccines, using conventional imaging? Conventional whole-body imaging techniques, such as bioluminescence imaging, lack the sensitivity for very low doses. Their signal contrast drops drastically at the low doses (e.g., 0.0005 mg kg−1) typical of therapeutic vaccines, making cellular-level detection impossible [9].
FAQ 2: My nanocarriers show good in vitro performance but poor in vivo efficacy. What could be happening? This is often due to unforeseen nano-bio interactions and off-target accumulation. Upon injection, nanocarriers encounter biological barriers and can accumulate in non-target tissues. For example, intramuscularly injected lipid nanoparticles (LNPs) have been found to reach heart tissue, leading to local proteome changes [9]. Comprehensive biodistribution analysis at the single-cell level is needed to identify these off-target sites.
FAQ 3: How does the protein corona affect my nanocarrier's journey? When nanocarriers enter the in vivo environment, they inevitably acquire a coating of proteins called the "protein corona". This corona can mask targeting moieties, alter the nanocarrier's cellular interactions, and change its intended biodistribution, potentially reducing its targeting specificity and efficacy [9] [5].
FAQ 4: What are the key nanocarrier properties that influence cellular uptake and biodistribution? The size, surface charge (zeta potential), and surface hydrophobicity of your nanocarrier are critical [5]. To avoid rapid clearance and promote target interaction:
- Size: Ideal size is between 10 nm (to avoid renal clearance) and 200 nm (for tumor extravasation) or 500 nm (to avoid MPS uptake) [10].
- Surface Charge: A near-neutral charge (-10 mV to +10 mV) helps avoid opsonization and MPS recognition [10].
Troubleshooting Guides
Problem 1: Inefficient Cellular Uptake in Target Tissues
Potential Causes and Solutions:
- Cause: Lack of Active Targeting.
- Solution: Functionalize the nanocarrier surface with targeting moieties (e.g., antibodies, peptides) that specifically bind to receptors highly expressed on your target cells. This moves from passive to active targeting, increasing specificity [10].
- Cause: Suboptimal Physicochemical Properties.
- Solution: Re-formulate nanocarriers to achieve a size below 200 nm and a neutral surface charge to enhance circulation time and tissue penetration [10]. Consult the table below on characterization techniques.
Problem 2: Rapid Clearance from Bloodstream
Potential Causes and Solutions:
- Cause: Opsonization and Uptake by the Mononuclear Phagocyte System (MPS).
- Solution: Modify the nanocarrier surface with biocompatibility polymers like polyethylene glycol (PEG) in a process called "PEGylation" or use albumin coatings. This creates a "stealth" effect, reducing opsonin binding and MPS recognition [10].
Problem 3: Inconsistent Experimental Results Due to Nanocarrier Heterogeneity
Potential Causes and Solutions:
- Cause: Poorly controlled nanocarrier synthesis leads to a broad size distribution (high PDI).
- Solution: Implement rigorous physicochemical characterization. Use techniques like Dynamic Light Scattering (DLS) to monitor batch-to-batch consistency and Asymmetrical Flow Field-Flow Fractionation (AF4) to fractionate polydisperse samples before analysis [5].
Critical Nanocarrier Characterization Data
Table 1: Essential In Vitro Characterization Techniques for Nanocarriers [5]
| Property | Key Techniques | Brief Principle | Advantages & Limitations |
|---|---|---|---|
| Size & PDI | Dynamic Light Scattering (DLS) | Measures particle diameter based on Brownian motion | Fast, statistical data; sensitive to impurities, unreliable for polydisperse samples |
| Asymmetrical Flow Field-Flow Fractionation (AF4) | Separates samples by size in a channel prior to detection | Excellent for complex, polydisperse samples; requires method establishment for each nanocarrier type | |
| Surface Charge | Zeta Potential Measurement | Applies current and uses laser Doppler velocimetry to measure particle movement | Predicts colloidal stability; highly sensitive to pH and ionic strength, requires dilution |
| Morphology | Atomic Force Microscopy (AFM) | Scans surface with a probe tip for topographic mapping | Provides ultra-high resolution without special sample treatment; slow scanning, requires expertise |
| Electron Microscopy (SEM/TEM) | Uses an electron beam for imaging | High-resolution particle sizing and morphology; minimal information on surface chemistry |
Table 2: Advanced In Vivo Biodistribution Analysis Methods [9] [11]
| Method | Resolution | Key Feature | Throughput | Best for Detecting |
|---|---|---|---|---|
| SCP-Nano (DISCO clearing + AI) | Single-cell | Maps entire mouse body in 3D; high sensitivity for very low doses | Medium (whole organism) | Comprehensive off-target identification at cell level |
| Mass Cytometry (CyTOF) | Single-cell | Uses metal-tagged antibodies; minimal signal overlap | High | Quantifying nano-bio interactions in complex cell mixtures |
| Imaging Flow Cytometry | Single-cell | Combines flow cytometry with microscopy | High | Visual confirmation of nanoparticle internalization per cell |
| Conventional Whole-Body Imaging (e.g., CT, MRI) | Organ-level | Non-invasive, live imaging | Low | Low-sensitivity, macroscopic biodistribution |
Experimental Protocols
This integrated pipeline comprehensively quantifies nanocarrier targeting throughout a whole mouse body with single-cell resolution.
Workflow Overview:
Key Steps:
- Nanocarrier Administration: Inject fluorescence-labeled nanocarriers (e.g., LNPs, liposomes, AAVs) via the chosen route (intravenous, intramuscular, etc.).
- Tissue Clearing: Use the optimized DISCO clearing method. Critical Note: The protocol eliminates urea and sodium azide and reduces dichloromethane incubation time to preserve fluorescence signal.
- Imaging: Image the entire cleared mouse body using light-sheet fluorescence microscopy at a resolution of ~1-2 µm (lateral) and ~6 µm (axial).
- AI Quantification: Analyze the large-scale 3D image data using the trained deep learning model (3D U-Net) to detect and quantify tens of millions of targeted cell instances reliably across different tissues.
This method allows for the quantification of nanoparticle associations with specific cell phenotypes in a complex mixture at high speed.
Workflow Overview:
Key Steps:
- Nanocarrier Labeling: Incorporate a stable elemental isotope (e.g., lanthanide metals) into the nanocarrier during synthesis.
- Cell Incubation & Staining: Incubate labeled nanocarriers with a single-cell suspension. Subsequently, stain the cells with a panel of antibodies conjugated to different metal isotopes to define cell phenotypes.
- Data Acquisition: Introduce cells into the mass cytometer (CyTOF), where they are nebulized into single-cell droplets, vaporized, and ionized.
- Data Analysis: Quantify all metal isotopes simultaneously for each cell. Correlate the elemental signal from the nanocarrier with specific cell phenotype markers to determine which cell types are associated with the nanocarriers.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanocarrier Development and Tracking [9] [5] [10]
| Reagent / Material | Function / Role | Common Examples / Notes |
|---|---|---|
| Ionizable Lipids | Core component of LNPs; enables encapsulation and endosomal escape of nucleic acids (mRNA, siRNA). | MC3 (clinically approved). Critical for LNP-based vaccines and therapies [9]. |
| PEGylated Lipids | Surface modifier used in liposomes and LNPs; provides a "stealth" coating to reduce MPS clearance and increase circulation time [10]. | Doxil formulation. PEGylation is a key strategy to improve pharmacokinetics. |
| Branched Polyethylenimine (PEI) | A cationic polymer used to form polyplexes for nucleic acid delivery; promotes condensation and cellular uptake. | Can be used for DNA/RNA delivery; optimization of molecular weight is needed to balance efficacy and toxicity [9]. |
| Adeno-Associated Viruses (AAVs) | Viral vectors for gene delivery; offer high transduction efficiency and potential for long-term gene expression. | Various serotypes (e.g., AAV2, Retro-AAV) have different tissue tropism (e.g., adipocytes) [9]. |
| Fluorescent Dyes (e.g., Alexa Fluor) | Critical for labeling and tracking nanocarriers or their payloads in vitro and in vivo. | Conjugated to payload (mRNA) or lipid component. Must be chosen and handled to preserve signal during clearing [9]. |
| Elemental Tags (Lanthanides) | Metal isotopes used for labeling nanocarriers in mass spectrometry-based detection (e.g., CyTOF). | Provides a non-overlapping, quantitative signal for high-throughput single-cell analysis of uptake [11]. |
| Targeting Ligands | Surface moieties that bind to specific cell-surface receptors to facilitate active targeting. | Antibodies, peptides, or other small molecules. Conjugated to the nanocarrier surface to improve specificity [10]. |
Frequently Asked Questions
1. What are the primary sensitivity limitations of whole-body imaging techniques like PET for nanocarrier analysis? Conventional whole-body imaging techniques, such as positron emission tomography (PET), lack the sensitivity to work with the low doses of nanocarriers employed in many applications, such as preventive and therapeutic vaccines. They cannot identify the millions of individual cells targeted by nanocarriers in three dimensions and struggle to detect low-intensity off-target sites at clinically relevant doses [9].
2. How does the resolution of conventional imaging compare to the needs of single-cell nanocarrier research? Techniques like PET, computed tomography (CT), and magnetic resonance imaging (MRI) lack the resolution to identify individual cells. They provide organ-level data but cannot resolve biodistribution at the cellular level, which is crucial for understanding nano-bio interactions and off-target effects in nanocarrier development [9].
3. What are the key drawbacks of using 2D histology for biodistribution studies? Traditional histology relies on thin, pre-selected two-dimensional tissue sections. While it offers subcellular resolution and high sensitivity, this approach is not suitable for comprehensive whole-animal analysis. It risks missing critical off-target events that occur outside the selected slices and provides an incomplete picture of distribution patterns [9].
4. What is a major challenge related to the inherent heterogeneity of biological systems? A significant challenge facing traditional pathology and 2D analysis is the concern about sample representativeness caused by intrinsic heterogeneity in lesions, particularly in highly heterogeneous tissues like tumors. This can lead to inaccurate tissue sampling and inter-observer variation in diagnosis [12].
5. Are there integrated technologies that overcome these limitations? Yes, emerging technologies are being developed to bridge these gaps. For instance, the SCP-Nano pipeline integrates whole-mouse tissue clearing, light-sheet microscopy, and a dedicated deep-learning analysis to map nanocarrier biodistribution throughout the entire mouse body with single-cell resolution and high sensitivity, overcoming the limitations of both conventional imaging and histology [9].
Troubleshooting Guide: Addressing Key Experimental Challenges
This guide helps diagnose and resolve common problems encountered when using conventional methods for nanocarrier biodistribution analysis.
Table 1: Troubleshooting Common Experimental Limitations
| Problem | Underlying Cause | Potential Solution | Considerations & Alternative Methods |
|---|---|---|---|
| Inability to detect nanocarriers at low, clinically relevant doses [9] | Limited sensitivity of PET, CT, and optical imaging. | • Increase injection dose (may cause toxicity and not reflect clinical use). • Use more sensitive radioisotopes or brighter fluorescent tags. | Consider switching to high-sensitivity methods like tissue clearing with light-sheet microscopy (e.g., SCP-Nano) that can detect doses as low as 0.0005 mg kg⁻¹ [9]. |
| Missing critical off-target nanocarrier accumulation [9] | reliance on pre-selected 2D histological sections; low contrast in whole-body imaging. | • Increase the number of histological sections analyzed (time-consuming). • Use hybrid imaging (e.g., PET/CT) for better anatomical context [12]. | Implement a whole-body, 3D analysis method like SCP-Nano to comprehensively map all targeted cells without pre-selection bias [9]. |
| Lacking cellular-resolution data from whole-body experiments [9] | inherent resolution limits of PET, CT, and MRI. | • Perform ex vivo histology on dissected organs (destructive and not whole-body). | Adopt a 3D imaging pipeline that maintains single-cell resolution across the entire organism. Correlate low-resolution whole-body images with high-resolution histological data from specific regions [9]. |
| Difficulty quantifying cell-level biodistribution accurately and at scale | reliance on manual counting or simple thresholding in images, which is prone to error and not scalable. | • Use commercial software (e.g., Imaris), though performance may be suboptimal (F1 scores <0.50 reported) [9]. | Implement a robust deep learning-based quantification pipeline trained for your specific nanocarrier and tissue type to reliably detect and quantify tens of millions of targeted cells [9]. |
Experimental Protocol: Single-Cell Precision Nanocarrier Identification (SCP-Nano)
The following workflow outlines the SCP-Nano method, an integrated pipeline designed to overcome the limitations of conventional biodistribution analysis [9].
Objective: To comprehensively map and quantify the biodistribution of fluorescently labeled nanocarriers throughout an entire mouse body at single-cell resolution.
Workflow for High-Resolution Biodistribution Analysis
Materials and Reagents:
- Fluorescently labeled nanocarriers (e.g., LNPs, liposomes, AAVs).
- Mice (appropriate model for your study).
- Fixative (e.g., paraformaldehyde).
- Reagents for optimized DISCO clearing protocol (note: urea and sodium azide are omitted, and dichloromethane incubation time is reduced to preserve fluorescence) [9].
- Phosphate-buffered saline (PBS).
Methodology:
- Nanocarrier Administration: Inject fluorescently labeled nanocarriers into mice via the desired route (e.g., intravenous, intramuscular) at therapeutically relevant doses [9].
- Tissue Preparation and Clearing:
- At the chosen time point, perfuse mice transcardially with PBS followed by fixative to preserve tissue architecture.
- Dissect out the entire mouse body or organs of interest.
- Subject the samples to the optimized DISCO tissue clearing protocol. Critical steps include the omission of urea and sodium azide and reduced incubation time in dichloromethane to maximize fluorescence preservation throughout the mouse body [9].
- 3D Image Acquisition:
- Image the cleared whole-mouse body using light-sheet fluorescence microscopy.
- Aim for a resolution of approximately 1–2 µm (lateral) and 6 µm (axial) to achieve single-cell resolution across the entire body [9].
- AI-Based Image Analysis:
- Process the large-scale 3D imaging data using the SCP-Nano deep learning pipeline.
- The pipeline uses a 3D U-Net architecture to segment and identify nanocarrier-positive cells reliably.
- This model has been shown to achieve a high average instance F1 score (0.7329), significantly outperforming existing methods [9].
- Data Quantification and Visualization:
- Use the pipeline's output to quantify nanocarrier delivery at the organ, tissue, and single-cell level.
- Generate 3D maps of nanocarrier distribution for comprehensive analysis.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials for Advanced Single-Cell Biodistribution Studies
| Item | Function / Description | Example Application |
|---|---|---|
| Lipid Nanoparticles (LNPs) | A leading nanocarrier platform for protecting and delivering macromolecular drugs like mRNA [9]. | Used as the delivery vehicle for SARS-CoV-2 spike mRNA in vaccines; can be loaded with EGFP mRNA for tracking in biodistribution studies [9]. |
| Adeno-Associated Viruses (AAVs) | Viral vectors with potential for gene therapy; different serotypes exhibit distinct tissue tropism [9]. | Used to transduce specific cell populations (e.g., AAV2 variant Retro-AAV transduces adipocytes) for gene delivery studies [9]. |
| Tissue Clearing Reagents | Chemicals used to render tissues transparent by matching refractive indices of components. | Essential for the DISCO method, enabling deep light penetration for 3D microscopy of whole organs or bodies [9]. |
| Fluorescent Tags (e.g., Alexa Fluor dyes) | Molecules conjugated to nanocarriers or their cargo to enable optical detection. | Tagging mRNA or lipid components of LNPs with Alexa Fluor 647 or 750 allows visualization after tissue clearing and imaging [9]. |
| Deep Learning Models (3D U-Net) | Artificial intelligence models designed for segmenting 3D biological imaging data. | The core of the SCP-Nano pipeline, used to accurately identify and quantify millions of nanocarrier-targeted cells in a high-throughput, unbiased manner [9]. |
The development of precise nanocarriers for drug delivery, gene therapy, and vaccine applications represents a frontier in modern medicine. A significant obstacle in this field is the "single-cell targeting gap"—the critical inability of conventional technologies to comprehensively analyze nanocarrier biodistribution at the resolution of individual cells across entire living organisms. This gap hinders the rational design of next-generation nanocarriers that maximize therapeutic efficacy for target tissues while minimizing off-target effects [9] [11].
Existing methods for analyzing nanocarrier biodistribution, such as positron emission tomography (PET), computed tomography (CT), and magnetic resonance imaging (MRI), lack the resolution to identify the millions of individual cells targeted by nanocarriers in three dimensions. These techniques also often lack the sensitivity to work with the low doses employed in applications like preventive and therapeutic vaccines [9]. Conversely, traditional histological approaches offer subcellular resolution and high sensitivity but rely on thin, pre-selected two-dimensional tissue sections, making them unsuitable for whole-animal analysis [9]. This technological limitation creates a critical knowledge gap in understanding the true distribution, efficacy, and potential toxicity of nanomedicines.
Key Technologies Bridging the Resolution Gap
SCP-Nano: Whole-Body Single-Cell Mapping
The Single Cell Precision Nanocarrier Identification (SCP-Nano) pipeline represents an integrated experimental and deep learning approach to comprehensively quantify the targeting of nanocarriers throughout the whole mouse body at single-cell resolution [9] [13]. This method enables the visualization and quantification of nanocarrier distribution with unprecedented sensitivity, working at doses as low as 0.0005 mg kg⁻¹—far below the detection limits of conventional whole-body imaging techniques [9].
Experimental Workflow of SCP-Nano:
Diagram 1: SCP-Nano whole-body mapping workflow.
wildDISCO: Whole-Body Immunostaining
The wildDISCO method uses standard antibodies with fluorescent markers to create detailed 3D maps of entire mouse bodies, providing unprecedented visualization of biological systems. This technique involves perfusing antibodies throughout the vasculature of a non-living animal, followed by optical clearing and light-sheet fluorescence microscopy [14]. The resulting data provides body-wide maps of specific molecules, structures, or cells of interest, creating valuable contextual information for understanding nanocarrier distribution within intact biological systems.
Essential Research Reagent Solutions
Table 1: Key research reagents and materials for high-resolution nanocarrier mapping
| Reagent/Material | Function | Application Example |
|---|---|---|
| Lipid Nanoparticles (LNPs) | Protect and deliver RNA therapeutics; clinically approved delivery system | mRNA vaccine delivery; study biodistribution after different injection routes [9] |
| Adeno-Associated Viruses (AAVs) | Highly efficient gene delivery vectors; different serotypes have distinct tissue tropisms | Gene therapy; mapping transduction patterns across tissues [9] [13] |
| DNA Origami Structures | Programmable nanoscale structures with precise control over shape and function | Customized drug delivery; study of design principles affecting biodistribution [9] [13] |
| Optical Tissue Clearing Reagents | Render tissues transparent while preserving fluorescence | Enabling deep-tissue imaging for whole-organism analysis (DISCO method) [9] [14] |
| Fluorescently-Labeled Antibodies | Target-specific markers for structural and cellular identification | wildDISCO: mapping nervous system, lymphatic vessels, and immune cells [14] |
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the minimum dose of nanocarriers that SCP-Nano can detect, and why is this significant?
SCP-Nano can detect nanocarriers at doses as low as 0.0005 mg kg⁻¹, which is approximately 100-1,000 times lower than the detection limits of conventional imaging techniques like bioluminescence imaging [9]. This is particularly significant for vaccine development, where such low doses are typically used, and conventional methods fail to provide adequate contrast or resolution.
Q2: How does SCP-Nano handle the enormous data generated from whole-body imaging?
SCP-Nano employs a robust deep learning pipeline based on a 3D U-Net architecture with six encoding and five decoding layers. This AI approach partitions whole-body imaging data into discrete units for analysis within typical memory constraints, achieving an average instance F1 score of 0.7329 for segmenting targeted cells across diverse tissues [9].
Q3: Can these methods identify unexpected nanocarrier accumulation in off-target tissues?
Yes. For example, SCP-Nano revealed that intramuscularly injected LNPs carrying SARS-CoV-2 spike mRNA can reach heart tissue, leading to proteome changes that suggest immune activation and blood vessel damage [9]. This capability allows researchers to identify potentially problematic off-target accumulation before clinical trials.
Q4: What types of nanocarriers can be analyzed with these high-resolution methods?
The technology generalizes to various nanocarriers, including lipid nanoparticles (LNPs), liposomes, polyplexes, DNA origami, and adeno-associated viruses (AAVs) [9]. For instance, SCP-Nano revealed that an AAV2 variant transduces adipocytes throughout the body, information crucial for designing targeted gene therapies.
Troubleshooting Common Experimental Challenges
Table 2: Troubleshooting guide for high-resolution nanocarrier mapping experiments
| Problem | Potential Cause | Solution | Reference |
|---|---|---|---|
| Poor fluorescence signal after tissue clearing | Signal loss due to harsh clearing reagents | Optimize DISCO protocol: eliminate urea and sodium azide; reduce dichloromethane incubation time | [9] |
| Suboptimal cell segmentation in AI analysis | Inadequate training data or model architecture | Use virtual reality-based annotation for training; employ 3D U-Net with leaky ReLU activation | [9] |
| Inconsistent antibody penetration in whole-body staining | Large antibody size preventing homogeneous distribution | Use membrane permeability enhancers to facilitate deep, even penetration without aggregation | [14] |
| Difficulty correlating distribution with biological effects | Lack of spatial proteomic data integration | Combine SCP-Nano with spatial proteomics to reveal molecular changes in target tissues | [9] |
| Low annotation accuracy for rare cell types | Imbalanced cell-type distributions in data | Use methods with high macro F1 scores (like STAMapper) that proficiently identify rare cell types | [15] |
Advanced Computational Methods for Spatial Mapping
STAMapper for Cell-Type Annotation
For spatial transcriptomics data, STAMapper provides a heterogeneous graph neural network to accurately transfer cell-type labels from single-cell RNA-sequencing data to single-cell spatial transcriptomics data. This method demonstrates significantly higher accuracy compared to competing methods (scANVI, RCTD, and Tangram), particularly for datasets with fewer than 200 genes [15]. The method constructs a heterogeneous graph where cells and genes are modeled as distinct node types connected based on expression patterns.
Computational Architecture of STAMapper:
Diagram 2: STAMapper computational workflow for cell-type annotation.
CMAP for Spatial Cell Mapping
Cellular Mapping of Attributes with Position (CMAP) is another algorithm designed to precisely predict single-cell locations by integrating spatial and single-cell transcriptome datasets. This approach enables the reconstruction of genome-wide spatial gene expression profiles at single-cell resolution through a three-level mapping process: DomainDivision, OptimalSpot, and PreciseLocation [16]. CMAP has demonstrated a 99% cell usage ratio and successfully mapped 2,215 out of 2,242 cells in benchmark tests, significantly outperforming other methods like CellTrek and CytoSPACE [16].
Future Directions and Implementation Considerations
The integration of high-resolution imaging, tissue clearing, and artificial intelligence represents a paradigm shift in nanocarrier research. These technologies enable researchers to address previously intractable questions about nanocarrier behavior at the single-cell level throughout entire organisms. The future of this field will likely involve:
- Increased multiplexing: Simultaneous use of numerous antibodies or markers to model multiple complex systems together [14].
- Enhanced AI integration: Using high-quality, large-scale imaging data to train deep learning algorithms that can predict disease progression and treatment efficacy without additional animal experiments [14].
- Broader accessibility: Development of user-friendly tools that democratize advanced analysis, such as DELiVR for brain cell mapping, which eliminates the need for coding expertise [14].
For research groups seeking to implement these technologies, establishing local core facilities with specialized instruments—including microfluidic devices for library preparation, fluorescent microscopes, flow cytometers, and computational hardware—is essential. Additionally, investment in training for single-cell laboratory techniques, data analysis, and sustainable funding is critical for building institutional capacity in this transformative field [17].
SCP-Nano: A Breakthrough Pipeline for Whole-Body, Single-Cell Nanocarrier Imaging and AI Quantification
Frequently Asked Questions (FAQs)
What is SCP-Nano and what is its primary function? SCP-Nano (Single Cell Precision Nanocarrier Identification) is an integrated experimental and deep learning pipeline designed to comprehensively quantify the targeting of nanocarriers throughout an entire mouse body at single-cell resolution. It combines optical tissue clearing, light-sheet microscopy, and deep-learning algorithms to map and quantify nanocarrier biodistribution with high sensitivity. [9] [13]
What types of nanocarriers can be analyzed using SCP-Nano? The platform generalizes to various types of nanocarriers, including Lipid Nanoparticles (LNPs), liposomes, polyplexes, DNA origami structures, and adeno-associated viruses (AAVs). [9] [13]
What is the key advantage of SCP-Nano over conventional imaging techniques? SCP-Nano can detect nanocarriers at doses as low as 0.0005 mg kg−1, which is far below the detection limits of conventional whole-body imaging techniques like bioluminescence, PET, CT, or MRI. It also provides single-cell resolution across the entire organism, unlike traditional methods. [9] [18]
What was a significant finding made possible by SCP-Nano? Using SCP-Nano, researchers demonstrated that intramuscularly injected LNPs carrying SARS-CoV-2 spike mRNA can reach heart tissue. Subsequent proteomic analysis of the heart revealed changes in protein composition, suggesting immune activation and possible blood vessel damage. [9] [13] [19]
Troubleshooting Guide
Issue 1: Poor Fluorescence Signal After Tissue Clearing
- Potential Cause: Signal degradation from harsh clearing chemicals.
- Solution: Use the optimized DISCO clearing protocol. Eliminate urea and sodium azide from the process and reduce dichloromethane (DCM) incubation time to better preserve the fluorescence signal of tagged mRNAs. [9]
Issue 2: Suboptimal AI-Based Cell Segmentation
- Potential Cause: Use of generic segmentation tools not tailored for this specific data.
- Solution: Implement the dedicated SCP-Nano deep learning pipeline. The provided 3D U-Net architecture, trained on manually annotated 3D patches from diverse tissues, significantly outperforms existing methods like Imaris or DeepMACT, achieving an average instance F1 score of 0.73. [9]
Issue 3: Inconsistent Biodistribution Results
- Potential Cause: Variability in injection routes affecting LNP tropism.
- Solution: Strictly control and document the administration route (e.g., intravenous, intramuscular, intranasal). SCP-Nano has revealed that distribution patterns are highly dependent on the injection route. [9]
Detailed Experimental Protocols
Protocol 1: Whole-Mouse Body Processing and Imaging for SCP-Nano
This protocol describes the steps for preparing and imaging a whole mouse body to visualize nanocarrier distribution at single-cell resolution. [9]
- Nanocarrier Administration: Inject fluorescence-labeled nanocarriers into the mouse model (e.g., via intramuscular or intravenous route) at the desired dose.
- Perfusion and Fixation: Perfuse the mouse with a fixative solution (e.g., paraformaldehyde) to preserve tissue structure.
- Optimized Tissue Clearing: Process the entire mouse body using the refined DISCO clearing method. Key modifications include:
- Omitting urea and sodium azide from clearing solutions.
- Reducing the incubation time in dichloromethane (DCM).
- Light-Sheet Microscopy: Image the transparent whole mouse body using a light-sheet microscope. The achieved resolution is approximately 1–2 µm (lateral) and approximately 6 µm (axial), enabling single-cell resolution across the entire body.
Protocol 2: AI-Based Quantification of Targeted Cells
This protocol outlines the process for analyzing the large-scale imaging data to detect and quantify nanocarrier-targeted cells. [9]
- Data Partitioning: Partition the whole-body imaging data into smaller, manageable 3D patches to fit computational memory constraints.
- Deep Learning Segmentation: Analyze the patches using the trained 3D U-Net model. This architecture features six encoding and five decoding layers with a leaky ReLU activation function.
- Instance Identification and Quantification: Use the
cc3dlibrary to identify each segmented cell or cluster instance. Calculate the size and intensity contrast of each instance relative to its local background. - Data Aggregation and Visualization: Compute organ-level statistics and create 3D maps of nanocarrier density within organs or volumes of interest.
Research Reagent Solutions
Table 1: Essential Materials and Reagents for SCP-Nano Experiments
| Item Name | Type/Model | Primary Function in the Protocol |
|---|---|---|
| Lipid Nanoparticles (LNPs) | MC3-based (clinical grade) | Model nanocarrier for delivering mRNA therapeutics. [9] |
| Fluorescent Tags | Alexa Fluor 647, Alexa 750 | Tagging mRNA or lipid components to enable optical detection. [9] |
| DISCO Clearing Reagents | Custom formulation | Renders entire mouse bodies transparent for deep-tissue imaging. [9] |
| Light-Sheet Microscope | Not Specified | Generates high-resolution 3D images of cleared tissues. [9] [13] |
| Deep Learning Model | 3D U-Net Architecture | Detects and quantifies nanocarrier-targeted cells from 3D image data. [9] |
Experimental Workflow and Signaling Pathway Visualizations
SCP-Nano Whole-Process Workflow
LNP-Induced Cardiac Proteome Changes
Optimized Tissue Clearing and Light-Sheet Microscopy for Sensitive 3D Imaging
Troubleshooting Common Experimental Issues
Signal Loss During Tissue Clearing
Problem: Diminished fluorescence signal after the tissue clearing process, jeopardizing data quality.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Fluorophore Instability | Verify specific dye used (e.g., Alexa Fluor 647). Test clearing protocol on a control slice. | Optimize the DISCO protocol by eliminating urea and sodium azide and reducing dichloromethane (DCM) incubation time [9]. |
| Incomplete Clearing | Sample appears opaque or cloudy. High background noise in images. | For aqueous methods, ensure adequate incubation time (can take weeks for large samples). For solvent-based methods, confirm proper dehydration steps prior to clearing [20]. |
| Sample Over-Clearing | Sample becomes fragile; cellular structures may degrade. | Standardize and strictly adhere to incubation times. For delicate samples, consider milder hyperhydrating methods like ScaleS [20]. |
Light-Sheet Microscopy Imaging Artifacts
Problem: Images exhibit stripes, shadows, or uneven illumination.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Light-Sheet Striping | Observe static, repeating dark and bright lines in the image along the illumination axis. | Utilize a microscope system with built-in destriping via light-sheet pivoting. An ultrafast scanning mirror can create a homogeneous illumination profile [21]. |
| Sample-Induced Scattering | Artifacts worsen in deeper tissue regions. | Employ multi-view imaging (e.g., with a Luxendo MuVi SPIM). Rotate the sample, acquire images from different angles, and fuse them computationally [21]. |
| Poor Sheet Alignment | Signal and resolution are optimal only in a thin plane. | Follow manufacturer's alignment protocol. Use fluorescent beads embedded in agarose to visually align the light-sheet with the focal plane of the detection objective. |
Frequently Asked Questions (FAQs)
General Workflow
Q1: Why should I use tissue clearing for nanocarrier biodistribution studies instead of conventional histology? Traditional histology relies on thin 2D sections, making it unsuitable for comprehensive 3D mapping of nanocarriers throughout entire organs or organisms. Tissue clearing, coupled with light-sheet microscopy, allows for the visualization and quantification of nanocarrier delivery at single-cell resolution across vast tissue volumes, revealing off-target sites that 2D sections can easily miss [9] [20].
Q2: My research involves both live cell imaging and cleared tissues. Do I need two different microscopes? No. Certain light-sheet systems, like the Luxendo MuVi SPIM, are designed for this purpose. A simple exchange of the central optical unit (e.g., the octagon) allows you to switch between imaging live samples (e.g., organoids) and large, cleared samples (e.g., whole organs) on the same instrument within minutes [21].
Technical Optimization
Q3: How can I improve the axial resolution of my light-sheet images? Axial resolution can be improved by implementing a multi-view imaging approach. By imaging the sample from different angles and applying subsequent image processing steps—including registration, fusion, and deconvolution—you can create an isotropic dataset with nearly equal resolution in the X, Y, and Z dimensions [21].
Q4: What is the major advantage of light-sheet microscopy over confocal microscopy for large samples? The primary advantages are significantly reduced phototoxicity and photobleaching, along with much faster 3D image acquisition. Light-sheet microscopy illuminates only the thin plane being imaged, whereas confocal microscopy illuminates the entire sample volume, generating out-of-focus light that is then rejected by a pinhole. This makes light-sheet microscopy far superior for long-term live imaging and for managing the large datasets from cleared tissues [21].
Q5: Can I perform long-term live imaging with light-sheet microscopy? Yes. Systems equipped with environmental control modules can precisely manage temperature (e.g., 20°C to 39°C), CO₂ (0%-15%), O₂ (1%-21%), and humidity (20%-99%) for continuous acquisitions lasting up to several days [21].
Experimental Protocols
Optimized DISCO Tissue Clearing for Fluorescent Nanocarriers
This protocol is optimized for preserving the fluorescence of tagged mRNAs and lipids in nanocarriers like LNPs during whole-body clearing [9].
Key Reagent Solutions:
- Dehydration Solutions: Methanol in distilled water (20%, 40%, 60%, 80%, 100%, v/v).
- Delipidation/Decolorization Solution: Dichloromethane (DCM). (Note: Incubation time must be optimized and minimized to preserve fluorescence).
- Refractive Index Matching Solution: DiBenzyl Ether (DBE).
Detailed Workflow:
- Perfusion and Fixation: Perfuse the mouse transcardially with PBS followed by 4% paraformaldehyde (PFA). Dissect out organs or use the whole body and post-fix by immersion in 4% PFA at 4°C for 24 hours.
- Dehydration: Immerse the sample in a graded series of methanol in water (20%, 40%, 60%, 80%, 100%, 100%) at 4°C. Incubate for 1 hour per step.
- Decolorization and Delipidation: Incubate the sample in 100% dichloromethane (DCM) at room temperature. Critical Step: The original DISCO protocol is modified here by reducing the DCM incubation time (e.g., to 2-3 hours) to prevent fluorescence quenching [9].
- Refractive Index Matching: Transfer the sample to DiBenzyl Ether (DBE) for storage and imaging. The sample should become transparent within hours.
- Mounting for Microscopy: Mount the cleared sample in a custom-made chamber or quartz cuvette filled with DBE for imaging with an inverted light-sheet microscope [21].
SCP-Nano AI-Based Quantification Workflow
This protocol details the steps for quantifying nanocarrier-targeted cells from large light-sheet imaging datasets [9].
Workflow Overview:
Key Steps:
- Data Preparation: Partition the terabyte-sized whole-body imaging data into smaller, discrete 3D patches (e.g., 200x200x200 to 300x300x300 voxels) for processing within standard GPU memory constraints [9].
- Annotation for Training: Create a ground-truth training dataset using a Virtual Reality (VR)-based annotation tool, which has been shown to be superior to 2D screen-based annotation for 3D data. Annotate patches from diverse tissues (spleen, liver, lymph nodes, etc.) [9].
- Model Training: Train a 3D U-Net architecture with six encoding and five decoding layers, using a leaky ReLU activation function. Use five-fold cross-validation to monitor performance and avoid overfitting. The benchmark for success is an average instance F1 score of >0.73 on an independent test dataset [9].
- Prediction and Analysis: Apply the trained model to new whole-body data. Use the
cc3dlibrary to identify each segmented cell or cluster instance and compute statistics like size and intensity contrast relative to the background for organ-level quantification [9].
The Scientist's Toolkit
Key Research Reagent Solutions
| Item | Function/Description | Application Example in Nanocarrier Research |
|---|---|---|
| Lipid Nanoparticles (LNPs) | Clinically approved nanocarriers (e.g., based on MC3 lipid) for protecting and delivering macromolecular drugs like mRNA [9]. | Delivery of SARS-CoV-2 spike mRNA; studying route-dependent biodistribution (intramuscular vs. intravenous) [9]. |
| Adeno-Associated Viruses (AAVs) | Viral vector nanocarriers for efficient gene delivery. Different serotypes (e.g., AAV2 variant Retro-AAV) have distinct tissue tropisms [9]. | Identifying off-target tissue transduction, such as adipocyte targeting by an AAV2 variant [9]. |
| DNA Origami | Programmable nanocarriers offering ease of production and modification [9]. | Studying the biodistribution of a novel, highly customizable nanocarrier platform [9]. |
| Optimized DISCO Solutions | A solvent-based clearing protocol modified by eliminating urea and reducing DCM time to preserve fluorescence [9]. | Enabling sensitive 3D imaging of LNP distribution at single-cell resolution across entire mouse bodies [9]. |
| DiBenzyl Ether (DBE) | A high-refractive index (∼1.55) organic solvent used as the final immersion medium in DISCO and uDISCO clearing [9] [20]. | Rendering dehydrated and delipidated samples transparent for light-sheet microscopy. |
| High RI Aqueous Solutions | Solutions like RapiClear or SeeDB2 that match tissue RI without harsh solvents, preserving lipids [20]. | Clearing smaller samples (e.g., organoids, tissue slabs) when lipid staining is required. |
Frequently Asked Questions (FAQs)
Q1: What are the most common causes of shape mismatch errors in 3D U-Net implementations, and how can I resolve them?
Shape mismatch errors frequently occur when the input dimensions are not divisible by 2^N, where N is the number of downsampling layers in the network [22]. In a standard U-Net with 5 downsampling layers, your input dimensions must be divisible by 32 (2^5). For example, an input size of 376×128 will cause concatenation errors because 376 is not divisible by 32 [22].
Solutions:
- Input Resizing/Cropping: Resize or crop your input volumes to compatible dimensions (e.g., 384×128).
- Architecture Modification: Use custom padding in convolutional layers or adjust the number of downsampling operations.
- Layer Verification: Ensure decoder layers precisely match corresponding encoder layers in spatial dimensions before concatenation.
Q2: My 3D U-Net produces poor segmentation on crowded cells or complex morphologies. How can I improve accuracy?
Traditional 3D U-Net architectures often struggle with crowded cells and complex biological structures [23] [24]. The u-Segment3D framework addresses this by leveraging superior 2D segmentation models from multiple orthogonal views to generate a consensus 3D segmentation, often outperforming native 3D approaches for complex morphologies [23].
Implementation Strategy:
- Utilize u-Segment3D: Apply established 2D segmentation models (Cellpose, μSAM) on orthogonal views [23]
- Optimize Architecture: For native 3D U-Nets, increase network width for tasks with numerous segmentation classes, as wider networks show significant benefits for high label complexity (>10 classes) [25]
- Leverage Alternative Algorithms: Consider algorithms like CellSNAP for specific imaging modalities like quantitative phase imaging (QPI), which excels with clumped cells and complex morphologies [24]
Computational requirements vary significantly based on architecture choices [25]. The "bigger is better" approach often yields minimal gains with substantial computational costs.
Resource Optimization Guidelines:
- Memory Efficiency: For high-resolution images (voxel spacing <0.8mm), prioritize increasing resolution stages to expand receptive field [25]
- Parameter Efficiency: For anatomically regular structures (high sphericity >0.6), deeper networks provide significant benefits; for intricate shapes, depth offers diminishing returns [25]
- Architecture Selection: Consider automated approaches like GA-UNet, which achieves competitive performance with merely 0.24%-0.67% of original U-Net parameters [26]
Q4: How can I adapt 3D U-Nets for specialized applications like nanocarrier tracking at single-cell resolution?
The SCP-Nano pipeline demonstrates an integrated approach combining tissue clearing, light-sheet microscopy, and deep learning for single-cell resolution tracking throughout entire organisms [9] [13].
Key Adaptation Strategies:
- Pipeline Integration: Combine tissue clearing methods (e.g., optimized DISCO protocol) with 3D U-Net segmentation
- Sensitivity Optimization: Implement detection algorithms that don't rely on single-value thresholding but make predictions based on contextual patterns [9]
- Validation: Correlate with histological sections to confirm signal preservation after tissue clearing [9]
Troubleshooting Guides
Input Shape and Dimension Issues
Table: Common 3D U-Net Shape Errors and Solutions
| Error Type | Example Error Message | Root Cause | Solution |
|---|---|---|---|
| Concatenation Dimension Mismatch | ValueError: A Concatenate layer requires inputs with matching shapes except for the concatenation axis. Received: input_shape=[(None, 46, 16, 512), (None, 47, 16, 512)] [22] |
Input dimensions not divisible by 2^N where N is downsampling steps | Adjust input dimensions to be divisible by 2^N or use custom padding |
| Padding Incompatibility | ValueError: CudaNdarray_CopyFromCudaNdarray: need same dimensions for dim 1, destination=13, source=14 [27] |
Potential bugs with padding='same' in 3D layers |
Use padding='valid' with manual dimension calculation or explicit input padding |
| Skip Connection Mismatch | Dimension errors during decoder-encoder concatenation | Inconsistent cropping or resizing between encoder and decoder paths | Implement identical cropping or use reflection padding |
Performance and Optimization Problems
Table: 3D U-Net Performance Optimization Strategies
| Performance Issue | Diagnosis Steps | Recommended Solutions |
|---|---|---|
| Low segmentation accuracy on crowded cells | Evaluate cell density and morphology complexity | Implement u-Segment3D consensus approach [23] or CellSNAP algorithm [24] |
| Slow inference time | Measure inference speed vs. model size | Use smaller architectures (e.g., S4D3W16) which often perform competitively with larger models [25] |
| Poor generalization to new cell types | Analyze training data diversity | Incorporate data augmentation or leverage foundation models (Cellpose, μSAM) [23] |
| High memory consumption | Monitor GPU memory during training | Reduce batch size, use mixed-precision training, or implement gradient checkpointing |
Experimental Protocols
Protocol 1: SCP-Nano Pipeline for Nanocarrier Distribution Analysis
Application: Single-cell resolution tracking of nanocarriers throughout entire organisms [9] [13]
Materials:
- Fluorescence-labeled nanocarriers (LNPs, liposomes, polyplexes, DNA origami, AAVs)
- Mouse model
- Optimized DISCO tissue clearing reagents (urea-free, reduced DCM incubation)
- Light-sheet microscope
- High-performance computing resources with GPU
Methodology:
- Administration: Inject fluorescence-labeled nanocarriers (doses as low as 0.0005 mg kg−1) via chosen route (intramuscular, intravenous, intranasal)
- Tissue Processing: Apply optimized DISCO clearing protocol (eliminate urea and sodium azide, reduce DCM incubation) to preserve fluorescence [9]
- Imaging: Acquire whole-body images at ~1-2μm lateral and ~6μm axial resolution using light-sheet microscopy
- AI Analysis: Process data through SCP-Nano 3D U-Net pipeline:
- Partition whole-body data into manageable units
- Apply trained 3D U-Net with six encoding/five decoding layers (leaky ReLU activation)
- Identify targeted cells/clusters using cc3d library
- Calculate organ-level statistics and nanocarrier density
Validation: Correlate with histological sections pre- and post-clearing to confirm signal preservation [9]
Protocol 2: u-Segment3D for Complex Cell Morphologies
Application: 3D segmentation of crowded cells or complex structures using 2D segmentation models [23]
Materials:
- 3D image volume (any modality: cell aggregates, tissue, embryos, vasculature)
- Pre-trained 2D segmentation model (Cellpose, μSAM, CellSAM, or transformer models)
- u-Segment3D toolbox (Python package)
Methodology:
- 2D Segmentation: Apply 2D instance segmentation to all orthogonal views (x-y, x-z, y-z slices)
- Consensus Generation: Input 2D segmentations to u-Segment3D framework:
- Framework reconstructs 3D gradient vectors of distance transform representation
- Performs gradient descent and spatial connected component analysis
- Generates consensus 3D instance segmentation
- Validation: Compare with ground truth manual segmentations
Advantages: Eliminates need for extensive 3D training data; leverages superior 2D segmentation performance [23]
Research Reagent Solutions
Table: Essential Materials for 3D Cell Segmentation and Nanocarrier Research
| Reagent/Resource | Function/Application | Key Characteristics | Example Use Cases |
|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Nanocarrier for drug/gene delivery | MC3-ionizable lipid, PEG coating, fluorescent tagging [9] | mRNA vaccine delivery, targeted therapy [9] [13] |
| DISCO Tissue Clearing Reagents | Tissue transparency for whole-organism imaging | Urea-free formulation, reduced DCM incubation [9] | Whole-body nanocarrier tracking, single-cell resolution imaging [9] |
| DNA Origami Structures | Programmable nanocarriers | Customizable structure, precise functionalization [13] | Targeted immune cell delivery, programmable drug release [13] |
| Adeno-Associated Viruses (AAVs) | Gene therapy delivery vehicles | Tissue-specific tropism, high transduction efficiency [9] | Gene therapy development, tissue-specific targeting [9] [13] |
| Quantitative Phase Imaging (QPI) | Label-free cell imaging | Refractive index measurement, non-destructive [24] | Cell dynamics study, drug-cell interactions [24] |
U-Net Architecture Selection Guidelines
Table: Task-Specific 3D U-Net Architecture Recommendations
| Task Characteristic | Recommended Architecture | Performance Benefit | Computational Cost |
|---|---|---|---|
| High-resolution images (voxel spacing <0.8mm) | Increased stages (S5, S6) | Significant improvement (p<0.05) [25] | Moderate increase (10-20% per stage) [25] |
| High label complexity (>10 classes) | Wider networks (W32, W64) | Substantial improvement [25] | Significant increase (~2× per width doubling) [25] |
| Anatomically regular structures (sphericity >0.6) | Deeper networks (D3) | Strong benefit [25] | Moderate increase (30-40%) [25] |
| Resource-constrained environments | GA-UNet or smaller U-Net variants | Competitive performance with 0.24%-0.67% parameters [26] | Drastic reduction (up to 8.8× faster inference) [26] [25] |
Frequently Asked Questions (FAQs)
Q1: What are the key composition factors that influence nanocarrier encapsulation efficiency and biodistribution? The composition of nanocarriers is a critical determinant of their performance. For Lipid Nanoparticles (LNPs), the four-component system allows for precise tuning. The ionizable lipid (typically ~50 mol%) is crucial for nucleic acid encapsulation and endosomal escape, while the PEG-lipid (as low as 0.5-1.5 mol%) controls nanoparticle size and stability, and helps prolong circulation time. Helper phospholipids (e.g., DSPC, ~10 mol%) and cholesterol (~38-39 mol%) contribute to the structural integrity and stability of the particle, facilitating stable encapsulation and reducing drug leakage [28] [29]. For other nanocarriers like DNA origami, the sequence design and incorporation of stabilizing elements (like ITR hairpins) are key for maintaining integrity and enabling gene expression [30].
Q2: How can I accurately quantify nanocarrier biodistribution and off-target effects at single-cell resolution? Conventional whole-body imaging techniques like bioluminescence often lack the sensitivity and resolution for low-dose studies (e.g., vaccine doses) and cannot identify individual targeted cells. The SCP-Nano pipeline overcomes this by combining an optimized tissue-clearing method (a refined DISCO protocol) with light-sheet microscopy and a dedicated deep-learning analysis model (based on a 3D U-Net architecture). This integrated approach allows for the mapping and quantification of fluorescence-labeled nanocarrier biodistribution throughout an entire mouse body at single-cell resolution, identifying millions of individual targeting events with high sensitivity [9].
Q3: Why is my DNA origami failing to express delivered genes in mammalian cells? A primary prerequisite for gene expression from DNA origami is the unfolding of the nanostructure within the intracellular environment to make the encoded gene accessible. If your origami is too stable, for instance, through internal cross-linking (e.g., UV point welding), gene expression can be almost completely suppressed. Ensure that your origami design can denature inside the cell. Furthermore, gene expression efficiency can be significantly enhanced by incorporating specific functional sequences into your synthetic scaffold design, such as virus-inspired inverted terminal repeat (ITR) hairpin motifs, Kozak sequences, and woodchuck post-transcriptional regulatory elements (WPRE) [30].
Q4: What strategies can improve the endosomal escape of non-viral nanocarriers? Endosomal sequestration remains a major barrier. Several strategies exist, often centered on the design of ionizable lipids in LNPs, which become positively charged in the acidic endosomal environment, promoting membrane disruption [28]. Recent research shows that modifying helper components can also be highly effective. For example, replacing standard cholesterol in LNPs with natural analogues bearing a C-24 alkyl chain (e.g., β-sitosterol) can create morphologically distinct nanoparticles (e.g., polyhedral vs. spherical) that exhibit enhanced intracellular diffusivity and more efficient endosomal escape, leading to dramatically higher transfection [29]. For DNA origami, functionalization with endosomolytic agents or pH-responsive elements can be explored.
Q5: How can I achieve tissue-specific targeting with my nanocarrier? Targeting can be passive or active. Passive targeting, such as the natural accumulation of some LNPs in the liver and spleen, can be influenced by particle size and surface properties like PEGylation [28] [31]. Active targeting involves functionalizing the nanocarrier surface with targeting moieties that bind to receptors on specific cells. This is a universal strategy applicable to most nanocarrier types. Examples include using antibodies, aptamers (e.g., MUC-1 aptamer for breast cancer cells), or peptides (e.g., cell-penetrating peptides) on the surface of LNPs, DNA origami, gold nanoparticles, or other nanocarriers [32] [33]. Note that in vivo, a protein corona can form on the nanocarrier, which may mask these targeting ligands and alter biodistribution [9].
Q6: What are the cargo size limitations for different nanocarriers, and how can I work around them? Cargo capacity varies significantly and is a key factor in nanocarrier selection. The table below summarizes the limitations and common solutions.
| Nanocarrier | Typical Cargo Capacity | Strategies to Overcome Limitations |
|---|---|---|
| Adeno-associated Viruses (AAVs) | ~4.7 kb [34] | Use smaller Cas protein orthologs (e.g., Cas12a); split cargo into dual/triple AAVs; deliver only sgRNA to Cas-expressing cells. |
| Lipid Nanoparticles (LNPs) | High for mRNA; varies for type [31] | Optimize lipid composition and N:P ratio for different cargo sizes (e.g., saRNA, plasmid DNA). |
| DNA Origami | Up to ~10 kb or more (scaffold) [32] | Use custom-sequence scaffolds; design multimeric "brick" systems for larger genetic circuits [30]. |
| Adenoviral Vectors (AdVs) | Up to ~36 kb [34] | The large capacity generally avoids the need for workarounds for most CRISPR cargos. |
| Lentiviral Vectors (LVs) | No strict size limit [34] | The large capacity generally avoids the need for workarounds for most CRISPR cargos. |
Troubleshooting Guides
Issue 1: Low Transfection or Gene Expression Efficiency
Possible Causes and Solutions:
Cause: Inefficient Endosomal Escape. The nanocarrier is trapped and degraded in the endolysosomal pathway.
- Solution for LNPs: Screen or design novel ionizable lipids with improved endosomolytic activity. Consider incorporating cholesterol analogues like β-sitosterol, which has been shown to enhance transfection by up to 32-fold in some systems by altering intracellular trafficking and promoting escape [29].
- Solution for Polyplexes/DNA Origami: Incorporate endosomolytic peptides or polymers (e.g., polyethylenimine) into the design. Ensure the carrier can destabilize membranes at low pH.
Cause: Poor Cellular Uptake.
Cause: Nanocarrier Does Not Unpack its Payload.
- Solution for DNA Origami: The structure must unfold to express its gene. Avoid over-stabilization through excessive cross-linking. Designs that are stable in circulation but disassemble under intracellular conditions (e.g., in a reductive environment) are ideal [30].
Cause: Low Encapsulation Efficiency.
- Solution for LNPs: Optimize formulation parameters. Use microfluidic mixing for highly reproducible, homogeneous LNPs with >90% encapsulation efficiency, instead of manual methods like thin-film hydration [28]. Adjust the ratio of ionizable lipid to nucleic acid.
Issue 2: High Cytotoxicity or Immunogenicity
Possible Causes and Solutions:
Cause: Cationic Lipid-Induced Toxicity.
- Solution for LNPs: Replace permanently cationic lipids with ionizable lipids, which are neutral at physiological pH (reducing toxicity) but become positively charged in acidic endosomes (facilitating escape) [28].
Cause: Immune Recognition of Viral Vectors.
- Solution for AAVs/AdVs: Utilize different serotypes with lower seroprevalence. Consider using virus-like particles (VLPs), which are empty viral capsids that lack the viral genome, reducing immunogenicity and safety concerns associated with full viral vectors [34].
Cause: Non-Specific Interactions.
Issue 3: Inefficient Co-delivery of Multiple Components
Possible Causes and Solutions:
- Cause: Stoichiometric Imbalance.
- Solution: Use a single nanocarrier system designed for multiplexing. DNA origami "bricks" that self-assemble into higher-order structures, with each brick encoding a different gene, enable stoichiometrically controlled co-delivery and expression, overcoming the limitations of Poisson distribution in co-transfection [30].
- Solution for CRISPR RNP Delivery: Co-encapsulate the Cas protein and guide RNA as a pre-formed ribonucleoprotein (RNP) complex within a single LNP, ensuring they are delivered to the same cell simultaneously [31].
The following tables consolidate key quantitative findings from recent research to aid in experimental design and benchmarking.
Table 1: Impact of Cholesterol Analogues on LNP Transfection Efficiency (Based on [29])
| Cholesterol Analogue | Key Structural Difference | mRNA Encapsulation | Relative Transfection Efficiency (vs. Cholesterol) |
|---|---|---|---|
| Cholesterol (Control) | N/A | ~94% | 1.0x |
| β-Sitosterol | C-24 ethyl group | Comparable to control | Substantially improved (up to 32-fold with some ionizable lipids) |
| Stigmasterol | C-24 ethyl + C-22 double bond | Lower than control | 1.6x |
| Vitamin D2/D3 | Modified ring structure (Body) | High | Poor |
| Group III Analogs | Tail modified into a 5th ring | Limited | Poor |
Table 2: Performance of LNP Formulation Methods (Based on [28])
| Formulation Method | Particle Size Control | Homogeneity (PDI) | Encapsulation Efficiency | Scalability & Notes |
|---|---|---|---|---|
| Microfluidics | High (e.g., 50-200 nm) | High (<0.2) | High (≥90%) | Gold standard for R&D; highly controllable and repeatable. |
| Macrofluidics (T-junction) | Good | Good | High | Suitable for large-scale production (e.g., vaccines); requires larger volumes. |
| Manual Mixing (Pipette) | Low | Low (Highly variable) | Low | Suitable only for basic proof-of-concept; not reproducible. |
| Thin-Film Hydration | Low | Low | Low | Easy to use but poor size control and encapsulation. |
| High-Energy Methods | Low | Low | Low | Risk of damaging delicate nucleic acids. |
Experimental Protocols
Protocol 1: SCP-Nano Pipeline for Whole-Body, Single-Cell Biodistribution Mapping
This protocol enables the sensitive detection and quantification of nanocarrier targeting events across the entire body of a mouse at single-cell resolution [9].
- Nanocarrier Administration: Administer your fluorescence-labeled nanocarrier (e.g., LNP, AAV, liposome) to mice via the desired route (e.g., intravenous, intramuscular) at the relevant dose (validated down to 0.0005 mg kg⁻¹).
- Tissue Clearing (Optimized DISCO):
- Perfuse and fix the mice.
- Key Optimization: Use a refined DISCO clearing protocol that omits urea and sodium azide and reduces dichloromethane (DCM) incubation time to preserve the fluorescence signal of tagged mRNAs or labels throughout the body.
- Whole-Body Imaging: Image the cleared whole mouse bodies using light-sheet fluorescence microscopy at a high resolution (approximately 1–2 µm lateral, 6 µm axial).
- AI-Based Quantification (SCP-Nano Deep Learning Pipeline):
- Data Preparation: Partition the whole-body imaging data into manageable 3D patches.
- Model Application: Process the data using the pre-trained 3D U-Net deep learning model. This model was trained on a diverse dataset of tissues annotated via a virtual reality (VR) system for superior accuracy.
- Analysis: The pipeline identifies each targeted cell/cluster instance, calculating its size and intensity contrast. This allows for organ-level and single-cell-level quantification of nanocarrier delivery.
Protocol 2: Assessing Gene Expression from DNA Origami in Mammalian Cells
This protocol outlines key steps for designing and testing DNA origami for gene delivery and expression [30].
- Design and Production:
- Scaffold Design: Create a custom, circular single-stranded DNA (ssDNA) scaffold that encodes your gene of interest (e.g., EGFP) under a mammalian promoter (e.g., CMV). Incorporate enhancing sequences like Kozak, WPRE, and ITR-like hairpins.
- Staple Design: Design staple strands to fold the scaffold into the desired shape. For enhanced expression, use long, continuous staples with no crossovers in the promoter and polyA regions to create stable double-stranded DNA in these key areas.
- Folding and Purification: Anneal the scaffold and staple strands to form the DNA origami object. Purify the correctly folded structures.
- Cell Transfection:
- Use electroporation (e.g., NeonTM Transfection System) for direct delivery into cells, as traditional cuvette electroporation may cause origami aggregation.
- A control with a non-annealed mixture of scaffold and staples can be used to compare expression from the unstructured components.
- Validation of Unfolding:
- To confirm that unfolding is necessary for expression, create a control group of origami that are topologically locked via UV point welding. Expect to see a near-complete suppression of gene expression in this group compared to the non-crosslinked origami.
- Expression Analysis: Measure transfection efficiency (percentage of fluorescent cells) and gene expression efficiency (mean fluorescence intensity) using flow cytometry or fluorescence microscopy.
Visualization Diagrams
Nanocarrier Intracellular Journey Pathway
SCP-Nano Experimental Workflow
DNA Origami Gene Expression Mechanism
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Ionizable Cationic Lipids (e.g., DLin-MC3-DMA) | Core component of LNPs; encapsulates nucleic acids and enables endosomal escape via charge shift [28] [29]. | pKa is a critical parameter; must be tunable for optimal performance in different applications. |
| PEGylated Lipids (e.g., DMG-PEG2000) | Stabilizes LNPs; controls particle size and reduces aggregation; modulates biodistribution and circulation time [28] [31]. | Molar ratio and PEG chain length are crucial; high percentages can hinder cellular uptake. |
| Cholesterol & Analogues (e.g., β-Sitosterol) | Structural helper lipid in LNPs; enhances stability and membrane fusion. Analogues can drastically improve transfection and trafficking [28] [29]. | The specific structure (head, body, tail) is critical. C-24 alkyl phytosterols show significant promise. |
| Custom ssDNA Scaffolds | The backbone for DNA origami; can be engineered to encode functional genes for expression in mammalian cells [32] [30]. | Requires specialized production (e.g., phagemid). Sequence must include promoter, gene, and enhancing elements (Kozak, WPRE, ITRs). |
| Targeting Ligands (Aptamers, Peptides) | Conjugated to nanocarrier surface for active targeting to specific cell types (e.g., MUC-1 aptamer for breast cancer cells) [33]. | Must consider potential shielding by the protein corona in vivo. Affinity and specificity are key. |
| Microfluidic Mixers | Instrumentation for reproducible, high-quality nanocarrier (LNP) formulation with high encapsulation efficiency and narrow size distribution [28] [31]. | Essential for moving away from variable manual methods. Different systems cater to volumes from µL to liters for R&D through GMP production. |
This technical support center addresses a critical and emerging challenge in nanocarrier research: the unexpected localization of intramuscularly (IM) injected mRNA-loaded Lipid Nanoparticles (LNPs) in heart tissue. Understanding and controlling this tropism is essential for optimizing therapeutic efficacy and safety profiles in next-generation RNA therapeutics. The following guides and FAQs are framed within the broader thesis of achieving precise nanocarrier distribution control at the single-cell level, providing researchers with methodologies to detect, quantify, and modulate this off-target delivery.
Troubleshooting Guides
Guide 1: Detecting Low-Level Cardiac Tropism
Reported Issue: Conventional whole-body imaging techniques fail to detect LNP delivery to the heart after intramuscular injection, especially at low, clinically relevant doses.
Background: Standard methods like bioluminescence imaging lack the sensitivity and resolution to identify low-intensity off-target sites when LNP doses are as low as 0.0005 mg kg⁻¹, which is common for vaccines [9].
Solution: Implement a single-cell resolution biodistribution pipeline.
- Recommended Technique: Single Cell Precision Nanocarrier Identification (SCP-Nano), which integrates whole-body tissue clearing, light-sheet microscopy, and a dedicated deep-learning analysis pipeline [9].
- Workflow Diagram:
- Key Technical Adjustments:
- Tissue Clearing: Modify standard DISCO protocols by eliminating urea and sodium azide and reducing dichloromethane (DCM) incubation time to preserve the fluorescence signal of tagged mRNAs [9].
- Validation: Confirm signal preservation by comparing histological slices before and after the clearing process [9].
Guide 2: Investigating the Impact of Formulation Processes on Tropism
Reported Issue: LNPs with nearly identical biophysical properties (size, PDI, zeta potential) exhibit significant differences in heart tissue tropism.
Background: The microfluidic device used for LNP formulation can influence the in vivo fate of the nanoparticles, independent of their core chemical composition. This effect is potentially mediated by differences in the acquired protein corona [35].
Solution: Systematically compare formulation mixers and characterize the resulting protein corona.
Experimental Protocol:
- Formulate LNPs: Prepare identical LNP compositions (e.g., the LNP++ formulation) using two different microfluidic mixers, such as a chaotic herringbone mixer and a bifurcating mixer (e.g., NxGen) [35].
- Characterize Biophysical Traits: Measure hydrodynamic diameter, polydispersity index (PDI), zeta potential, and encapsulation efficiency. Confirm these are nearly identical between the two batches [35].
- Isolate the Protein Corona: Incubate LNPs with mouse plasma, isolate the hard protein corona via centrifugation through a sucrose cushion, and resuspend the pellet for analysis [35].
- Identify Proteins: Use gel electrophoresis and mass spectrometry to identify differentially adsorbed proteins between the two LNP batches [35].
- Correlate with In Vivo Data: Compare the heart delivery efficiency of the two LNP batches using a sensitive detection method like SCP-Nano.
Expected Outcome: The herringbone-formulated LNP++ showed a 2-fold increase in heart delivery compared to the NxGen-formulated version, despite nearly identical physical properties, highlighting the critical role of the formulation process [35].
Guide 3: Optimizing mRNA Constructs for Cardiac Expression
Reported Issue: Protein expression in the heart is low or transient, limiting therapeutic potential.
Background: mRNA translation efficiency and stability are determined by its structural elements. Optimizing these elements is crucial for enhancing protein expression in challenging environments like ischemic cardiac tissue [36].
Solution: Rationally design the mRNA molecule.
- Key Optimization Strategies Table:
| mRNA Element | Optimization Strategy | Functional Impact |
|---|---|---|
| 5' Cap | Use CleanCap AG analog during IVT. Ensure proper co-transcriptional capping. | Enhances translational initiation and protects from degradation [36] [37]. |
| 5' and 3' UTRs | Incorporate UTRs known to enhance expression in heart tissue, e.g., the 5' UTR of the Ces1d gene. Use combinations from highly expressed genes (e.g., α-globin). | Regulates mRNA stability and translational efficiency; tissue-specific UTRs can double protein output in infarcted heart [36] [37]. |
| Coding Sequence | Perform codon optimization for the host. Place start codon within a Kozak sequence. Remove upstream start codons. | Enhances translational efficiency and reduces secondary structures [36] [35]. |
| Nucleotide Mod. | Incorporate modified nucleotides (e.g., N1-methyl-pseudouridine, m1Ψ). | Reduces innate immune recognition, increases mRNA stability, and prolongs protein expression [36] [38]. |
| Poly(A) Tail | Encode a long poly(A) tail (e.g., ~100 nucleotides) in the DNA template. | Improves mRNA stability and translation by binding to PABP [36] [37]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the biological significance of mRNA-LNP delivery to the heart, and should we be concerned?
The biological consequences are an active area of research. Proteomic analysis of heart tissue following intramuscular injection of LNPs carrying SARS-CoV-2 spike mRNA revealed changes in the expression of proteins related to immune activation and vascular function [9]. This suggests that off-target delivery can induce measurable biological effects. For vaccine applications, this may be a safety concern. For therapeutic applications, it could represent an opportunity for treating cardiac diseases. The significance must be evaluated on a case-by-case basis, underscoring the need for precise biodistribution profiling.
FAQ 2: Our in vitro assays in standard cell lines (e.g., HEK-293) show high transfection, but in vivo heart expression is poor. Why the discrepancy?
This is a common challenge. In vitro models often lack the physiological complexity of in vivo delivery. Key factors not captured in simple cell cultures include:
- ApoE Mediation: The uptake of systemically circulating LNPs in vivo is heavily influenced by apolipoprotein E (ApoE) adsorption and its interaction with specific receptors on target cells [38]. Your cell line may not express these receptors.
- Protein Corona: The protein corona that forms on LNPs in biological fluids dramatically alters their cellular interactions and tropism, a factor absent in standard culture media [9] [38].
- Biological Barriers: LNPs must navigate physical barriers (e.g., endothelial layers) and the immune system to reach the heart after intramuscular injection, which is not modeled in a dish.
Solution: Consider using more complex in vitro models, such as primary cardiomyocytes or heart-on-a-chip systems, and include relevant biological fluids (e.g., plasma) during incubation to allow for a more representative protein corona to form [38].
FAQ 3: How can we reduce unwanted heart tropism of our intramuscularly injected LNP vaccine?
To de-prioritize heart delivery, consider these strategies:
- Modify LNP Composition: Adjust the ionizable lipid, helper lipid, or PEG-lipid ratios. For instance, shifting the pKa of the ionizable lipid away from the optimal range for endosomal escape in cardiomyocytes can reduce expression [39] [40].
- Leverage the Protein Corona: Pre-coat or formulate LNPs to attract a specific protein corona that directs particles away from the heart and towards the desired immune cells in the lymph nodes [9] [35].
- Change Formulation Process: As shown in the troubleshooting guide, the microfluidic mixer type can influence tropism. Screening different formulation parameters may yield a particle with a more favorable biodistribution [35].
The Scientist's Toolkit: Essential Research Reagents & Solutions
This table details key materials and their functions for investigating mRNA-LNP heart tropism.
| Research Reagent / Solution | Function & Application |
|---|---|
| Ionizable Lipids (e.g., cKK-E12, MC3) | Critical for mRNA encapsulation and endosomal escape. The core component defining LNP performance and tropism [35] [40]. |
| Cationic Helper Lipids (e.g., DOTAP) | Can shift LNP tropism towards non-liver tissues, including the heart and lungs. Used in the LNP++ formulation [35] [41]. |
| Modified Nucleotides (e.g., m1Ψ) | Incorporated during IVT to reduce immunogenicity of mRNA and enhance its stability and translational capacity [36] [35]. |
| CleanCap AG Cap Analog | Used in co-transcriptional capping to produce a high-fidelity 5' cap structure, essential for efficient translation initiation [37]. |
| Microfluidic Mixers (Herringbone vs. Bifurcating) | Devices for controlled LNP self-assembly. The mixer type is a Critical Process Parameter (CPP) that can independently influence in vivo tropism [35] [42]. |
| SCP-Nano Deep Learning Pipeline | An AI-based tool for analyzing whole-body, single-cell resolution imaging data to unbiasedly quantify millions of LNP targeting events [9]. |
| Apolipoprotein E (ApoE) | A plasma protein crucial for mediating LNP uptake via ApoE receptors. Used to study or enhance hepatocyte delivery; its absence may indicate alternative uptake pathways in the heart [38]. |
Troubleshooting Off-Target Effects and Optimizing Nanocarrier Design for Precision
Identifying and Mitigating Off-Target Accumulation and Associated Toxicity
Troubleshooting Guide: Frequently Asked Questions
How can I detect nanocarrier accumulation in off-target tissues with high sensitivity?
Conventional whole-body imaging techniques often lack the sensitivity to detect off-target accumulation, especially at the low doses used in vaccines or therapies. The solution is to implement advanced single-cell resolution mapping.
- Recommended Solution: Adopt the Single Cell Precision Nanocarrier Identification (SCP-Nano) pipeline. This integrated method combines optimized tissue clearing, light-sheet microscopy, and a dedicated deep learning model to quantify nanocarrier biodistribution across entire animal models at single-cell resolution, even at doses as low as 0.0005 mg kg⁻¹ [9].
- Experimental Protocol:
- Administer Fluorescently-Labelled Nanocarriers: Inject your nanocarrier (e.g., LNP, liposome, polyplex) tagged with a stable fluorescent dye (e.g., Alexa Fluor) into your model organism [9].
- Optimized Tissue Clearing: Use a refined DISCO clearing protocol that omits urea and sodium azide and reduces dichloromethane incubation time to preserve fluorescence signal throughout the entire body [9].
- High-Resolution Imaging: Image the cleared whole body using light-sheet fluorescence microscopy at approximately 1–2 µm lateral and 6 µm axial resolution [9].
- AI-Powered Analysis: Analyze the large-scale 3D imaging data using the SCP-Nano deep learning pipeline (based on a 3D U-Net architecture) to reliably detect and quantify tens of millions of targeted cells across different organs [9].
What are the primary causes of nanocarrier off-target accumulation?
Off-target accumulation is a multi-factorial problem. The table below summarizes the key contributing factors.
Table: Key Factors Contributing to Off-Target Accumulation of Nanocarriers
| Factor | Description | Consequence |
|---|---|---|
| Physicochemical Properties | Suboptimal size, surface charge (zeta potential), and morphology of the nanocarrier [5]. | Altered biodistribution, rapid clearance by the mononuclear phagocyte system (MPS), and poor tumor penetration [43] [5]. |
| Protein Corona Formation | The spontaneous adsorption of serum proteins onto the nanocarrier surface upon injection [9]. | Can mask targeting ligands, leading to unintended cellular interactions and uptake in non-target organs like the liver and spleen [9]. |
| Heterogeneous EPR Effect | The Enhanced Permeability and Retention (EPR) effect, which facilitates tumor accumulation, is highly variable [44]. | Inconsistent and inefficient tumor targeting, leading to increased nanocarrier presence in healthy tissues [44]. |
| Insufficient Targeting Specificity | Lack of or ineffective active targeting strategies at the tissue, cellular, and subcellular levels [43]. | Poor cellular internalization at the target site and failure to reach the intended subcellular organelle, reducing efficacy and increasing off-target exposure [43]. |
My nanocarrier shows promising in vitro results but fails in vivo due to toxicity. How can I mitigate this?
This common issue often stems from unanticipated nano-bio interactions in a complex biological environment. A multi-pronged strategy focusing on characterization, redesign, and targeting is required.
Solution 1: Comprehensive Physicochemical Characterization Before in vivo studies, rigorously characterize your nanocarrier. Use the following techniques to ensure batch-to-batch consistency and predict in vivo behavior [5]:
- Dynamic Light Scattering (DLS): Determine hydrodynamic particle size and Polydispersity Index (PDI).
- Electrophoretic Light Scattering: Measure zeta potential to assess surface charge and colloidal stability.
- Electron Microscopy (SEM/TEM): Visualize nanocarrier morphology and confirm size.
- Atomic Force Microscopy (AFM): Provide ultra-high-resolution topographic analysis.
Solution 2: Implement Hierarchical Targeting Strategies Move beyond passive targeting by designing nanocarriers that can navigate multiple biological barriers dynamically [44].
- Tissue-Level: Leverage the EPR effect (passive) or target tumor vasculature (active) [44].
- Cellular-Level: Functionalize the surface with targeting moieties (e.g., antibodies, peptides) for specific cell recognition [43] [44].
- Organelle-Level: Incorporate ligands like Nuclear Localization Signals (NLS) to direct the cargo to specific subcellular sites, enhancing efficacy and reducing off-target toxicity within the cell [43].
Solution 3: Employ High-Throughput Single-Cell Screening Use techniques like mass cytometry or imaging flow cytometry to screen nanocarrier-cell interactions at a single-cell level. This helps identify which subpopulations of cells inadvertently take up the nanocarrier, informing a more targeted redesign [11].
How can I visualize the experimental workflow for identifying off-target effects?
The following diagram illustrates the integrated SCP-Nano pipeline for comprehensive, single-cell resolution mapping of nanocarrier biodistribution.
What does the AI analysis pipeline in SCP-Nano involve?
The deep learning component is crucial for accurately processing the vast datasets generated by whole-body imaging. The pipeline involves several key steps to segment and identify nanocarrier-targeted cells.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents and Materials for Investigating Off-Target Effects
| Item | Function in Experiment | Key Considerations |
|---|---|---|
| Fluorescently-Labelled Nanocarriers | Enable visualization and tracking of biodistribution. The tag can be on the cargo (e.g., Alexa Fluor-tagged mRNA) or the carrier structure itself [9]. | Ensure the dye is stable and that labeling does not alter the nanocarrier's intrinsic biodistribution properties [9]. |
| DISCO Tissue Clearing Reagents | Render entire organs or bodies transparent for deep-tissue imaging by matching refractive indices of tissues [9]. | Use optimized protocols that preserve fluorescence; omit urea/sodium azide and limit DCM incubation [9]. |
| Lipid Nanoparticles (LNPs) | A widely used nanocarrier platform for delivering various therapeutic cargoes, such as mRNA [9]. | Ionizable lipid composition (e.g., MC3) is critical for efficiency and tropism. Beware of PEG-induced immune responses [43] [9]. |
| Targeting Ligands (e.g., Peptides) | conjugated to the nanocarrier surface to actively target specific tissues, cells, or subcellular compartments [43] [45]. | Dual peptide-functionalization (e.g., for BBB crossing and microglia targeting) can significantly enhance specificity [45]. |
| Nuclear Localization Signals (NLS) | Short peptide sequences that actively facilitate import into the cell nucleus via the nuclear pore complex [43]. | Crucial for therapeutics whose site of action is the nucleus, helping to overcome a key intracellular barrier and improve efficacy [43]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: What is the primary limitation of conventional covalent conjugation for functionalizing nanocarriers? Conventional covalent methods often require reactive agents or organic solvents that can destabilize nanocarriers, induce cargo leakage, or alter their fundamental properties. Furthermore, these approaches can yield low efficiency, uneven ligand distribution, and compromise structural integrity. [46]
Q2: How does the "PEG dilemma" impact the efficacy of targeted nanocarriers? While PEGylation provides "stealth" properties to prolong circulation, it also creates steric hindrance that can shield targeting ligands and reduce their interaction with cellular receptors. This can diminish cellular uptake and targeting specificity, particularly in protein-rich environments like the bloodstream. [47]
Q3: What advanced technique allows for comprehensive analysis of nanocarrier distribution at the single-cell level across a whole organism? Single Cell Precision Nanocarrier Identification (SCP-Nano) is an integrated pipeline that combines tissue clearing, light-sheet microscopy, and deep learning. It can map and quantify the biodistribution of fluorescently-labeled nanocarriers throughout entire mouse bodies at single-cell resolution, even at very low doses. [9]
Q4: How can researchers validate the successful insertion and spatial distribution of ligands on a PEG corona? A common and effective method is to use Fluorescence Resonance Energy Transfer (FRET). By labeling the ligand (e.g., with pyrene) and the nanocarrier membrane (e.g., with FITC), colocalization and accurate spatial distribution can be confirmed through the characteristic energy transfer upon successful insertion. [46]
Q5: What are some strategies to overcome the limitations of traditional PEGylation? Emerging strategies include using stimuli-responsive (e.g., pH-sensitive) PEG shedding, optimizing PEG chain length and surface density, functionalizing PEG terminal groups, employing branched polymer architectures, and exploring alternative hydrophilic polymer coatings to avoid anti-PEG immunogenicity. [47]
Troubleshooting Common Experimental Issues
Problem: Low Ligand Functionalization Efficiency on PEGylated Nanocarriers
- Potential Cause 1: Inadequate PEG Corona Density or Conformation.
- Solution: Characterize the PEG layer on your nanocarriers using techniques like NMR or FTIR. Ensure the PEG chain length and surface density are sufficient to allow for ligand insertion while maintaining stability. Molecular dynamics simulations suggest PEG can dynamically adjust its conformation to accommodate guest molecules. [46]
- Potential Cause 2: Incorrect Ligand-Pyrene Conjugate Design.
- Solution: Confirm the synthesis and purity of your pyrene-conjugated molecules (Py-Xs). Measure the critical micelle concentration of the Py-Xs to ensure they are in a monomeric state suitable for insertion into the PEG corona, rather than forming their own aggregates. [46]
- Potential Cause 3: Non-optimized Incubation Conditions.
- Solution: Systematically optimize the incubation time, temperature, and ratio of Py-Xs to nanocarriers. The insertion process is rapid (on the scale of nanoseconds) but ensuring equilibrium is reached is crucial for maximum loading. [46]
Problem: Poor Cellular Uptake Despite Successful Ligand Functionalization
- Potential Cause 1: Protein Corona Masking the Targeting Ligands.
- Solution: Pre-incubate nanocarriers with relevant biological media (e.g., serum) and re-isolate them to study the effects of the hard protein corona. Strategies to minimize corona formation, such as using high-density PEG brushes or alternative "stealth" polymers, should be explored. [47]
- Potential Cause 2: Steric Hindrance from the PEG Layer.
- Solution: Implement a stimuli-responsive PEG shedding strategy. For example, use a PEG-lipid conjugate with a pH-labile bond that cleaves in the acidic tumor microenvironment, thereby de-shielding the ligands and promoting receptor interaction. [47]
- Potential Cause 3: Low Receptor Expression on Target Cells.
- Solution: Always validate the expression level of the target receptor on your specific cell line using flow cytometry or Western blot before conducting uptake experiments.
Problem: High Non-Specific Accumulation in Liver and Spleen (MPS Uptake)
- Potential Cause 1: Incomplete or Unstable PEG Coating.
- Solution: Re-optimize the PEGylation protocol. Increase PEG density or use PEG with a higher molecular weight to improve stealth properties and reduce opsonization. Monitor for the Accelerated Blood Clearance (ABC) phenomenon upon repeated injections, which is linked to anti-PEG antibodies. [47]
- Potential Cause 2: Nanoparticle Aggregation in Biological Fluid.
- Solution: Perform dynamic light scattering (DLS) and zeta potential measurements in physiologically relevant buffers (e.g., PBS) to assess colloidal stability before and after functionalization. Aggregation leads to rapid clearance by the Mononuclear Phagocyte System (MPS). [46]
Table 1: Efficiency and Stability of Non-Covalent PEG Corona Functionalization [46]
| Functionalized Ligand | Key Biological Function | Stability (After 3 Wash/Resuspension Cycles) | Key Validation Method |
|---|---|---|---|
| Pyrene-Triphenylphosphine (Py-TPP) | Mitochondrial targeting | >40% functional molecules retained | Confocal Microscopy |
| Pyrene-Folic Acid (Py-FA) | Targeting folate receptor, endocytosis | >40% functional molecules retained | FRET, Confocal Microscopy |
| Pyrene-Hyaluronic Acid (Py-HA) | CD44 targeting, cell migration regulation | >40% functional molecules retained | Confocal Microscopy |
| Pyrene-RGD Peptide (Py-RGD) | Integrin receptor binding, endocytosis | >40% functional molecules retained | Confocal Microscopy |
| Pyrene-GFP (Py-GFP) | Model protein for functionalization | >40% functional molecules retained | Dual-channel Confocal Microscopy |
Table 2: Comparison of Techniques for Analyzing Nano-Bio Interactions at Single-Cell Resolution [9] [11]
| Technique | Key Principle | Sensitivity | Resolution | Key Application in Nanocarrier Research |
|---|---|---|---|---|
| SCP-Nano (Whole-Body) | Tissue clearing + Light-sheet microscopy + AI | Detects doses as low as 0.0005 mg kg⁻¹ | Single-cell (1-2 µm lateral) | 3D whole-body mapping of nanocarrier distribution for any fluorescent label. [9] |
| Imaging Flow Cytometry | High-throughput imaging of cells in flow | High (single nanoparticle detection possible) | Single-cell | Quantification of nanoparticle internalization vs. surface binding; analysis of complex cell populations. [11] |
| Mass Cytometry (CyTOF) | Metal-tagged antibodies + ICP-MS | High (theoretically single nanoparticle) | Single-cell | Deep multiplexing to correlate nanocarrier uptake with dozens of cell surface markers simultaneously. [11] |
| Conventional Flow Cytometry | Light scattering and fluorescence | Moderate | Single-cell | High-throughput quantification of nanoparticle-associated cells; cell sorting (FACS) for downstream -omics. [11] |
Experimental Protocols
Objective: To attach biologically relevant ligands (e.g., TPP, FA, RGD) to the PEG corona of pre-formed nanocarriers using pyrene-based conjugation.
Materials:
- Pre-formed PEGylated nanocarriers (e.g., Polymersomes from PEG--b-PBD).
- Synthesized pyrene-conjugated ligand (Py-X).
- Appropriate aqueous buffer (e.g., PBS, HEPES).
- Purification equipment (e.g., centrifuge, dialysis membrane, size exclusion chromatography columns).
Method:
- Preparation: Dissolve the Py-X conjugate in a suitable solvent (e.g., DMSO) and then dilute significantly in the chosen aqueous buffer to a concentration well below its critical micelle concentration (CMC).
- Incubation: Mix the Py-X solution with the suspension of PEGylated nanocarriers at the desired molar ratio. Vortex gently to ensure homogeneity.
- Reaction: Allow the mixture to incubate at room temperature for a defined period (e.g., 1-2 hours). The pyrene moiety will spontaneously insert into the dense PEG corona via thermodynamically favorable dehydration and van der Waals interactions.
- Purification: Separate the functionalized nanocarriers from unincorporated Py-X molecules using a suitable method such as ultracentrifugation, dialysis, or size exclusion chromatography.
- Validation:
- Use confocal microscopy to visualize ligand attachment if the Py-X is fluorescent.
- Employ FRET, with a donor (pyrene) on the ligand and an acceptor (e.g., FITC) in the nanocarrier membrane, to confirm close proximity and successful insertion.
- Measure zeta potential to detect changes in surface charge upon ligand attachment.
Objective: To quantify the cell-level biodistribution of administered nanocarriers throughout an entire mouse body.
Materials:
- Mice administered with fluorescently-labeled nanocarriers (e.g., LNPs with Alexa Fluor-tagged mRNA).
- Perfusion and fixation solutions (e.g., PBS, 4% PFA).
- DISCO tissue clearing reagents (without urea and sodium azide, reduced DCM incubation time).
- Light-sheet fluorescence microscope.
- SCP-Nano deep learning software pipeline.
Method:
- Administration & Tissue Preparation: Administer the nanocarriers to mice via the chosen route (e.g., IV, IM). After a predetermined time, perfuse the mice transcardially with PBS followed by 4% PFA to fix tissues.
- Tissue Clearing: Process the entire mouse body or dissected organs using the optimized DISCO clearing protocol. The key modifications for fluorescence preservation are the omission of urea and azide and reduced dichloromethane (DCM) incubation.
- Imaging: Image the cleared whole mouse or organs using a light-sheet microscope at a resolution of approximately 1–2 µm (lateral) and approximately 6 µm (axial).
- Data Analysis: Process the large-scale 3D image data using the SCP-Nano deep learning pipeline. The pipeline, based on a 3D U-Net architecture, will segment and identify individual targeted cells across different tissues.
- Quantification: Use the software output to compute organ-level and body-wide statistics on nanocarrier density, number of targeted cells, and signal intensity.
Key Signaling Pathways and Workflows
Non-Covalent Functionalization and Targeting Workflow
SCP-Nano Single-Cell Analysis Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for PEGylation and Functionalization Studies [46] [9] [11]
| Item | Function/Description | Key Application |
|---|---|---|
| Pyrene-Conjugated Ligands | Small molecules, vitamins, peptides, or proteins linked to a pyrene moiety. | Serves as the anchor for non-covalent insertion into the PEG corona for functionalization. [46] |
| PEG--b-PBD Block Copolymer | A specific amphiphilic block copolymer that self-assembles into polymersomes. | A model nanocarrier with a well-defined PEG corona for studying functionalization. [46] |
| Fluorescent Tags (e.g., Alexa Fluor dyes, FITC) | dyes for labeling nanocarriers, ligands, or cargos (e.g., mRNA). | Enables tracking, visualization, and quantification of nanocarriers using microscopy and flow cytometry. [46] [9] |
| FRET Pair (e.g., Pyrene/FITC) | A donor-acceptor fluorescence pair where energy transfer indicates close proximity. | Validates the successful insertion and spatial colocalization of ligands on the nanocarrier surface. [46] |
| Ionizable Lipids (e.g., MC3) | A key component of clinically relevant Lipid Nanoparticles (LNPs). | Used for formulating mRNA-loaded nanocarriers to study biodistribution and delivery efficacy. [9] |
| DISCO Tissue Clearing Reagents | A suite of chemical reagents for making biological tissues transparent. | Essential for whole-body imaging, allowing light penetration for 3D single-cell analysis. [9] |
| Mass Cytometry Tags (e.g., Metal Isotopes) | Stable metal isotopes conjugated to antibodies or nanoparticles. | Allows for highly multiplexed single-cell analysis to correlate nanocarrier uptake with cell phenotype. [11] |
For researchers in drug development, selecting an optimal administration route is a critical determinant of therapeutic success. The choice between intramuscular (IM), intravenous (IV), and intranasal (IN) delivery directly influences nanocarrier biodistribution, cellular uptake, and ultimately, therapeutic efficacy and safety. This guide provides technical support for troubleshooting common challenges and optimizing protocols based on cutting-edge single-cell distribution research.
FAQs: Administration Routes and Nanocarrier Distribution
1. How does the administration route influence nanocarrier biodistribution and off-target effects at the single-cell level?
The administration route fundamentally directs nanocarrier fate, with significant implications for off-target exposure. Advanced imaging techniques like Single Cell Precision Nanocarrier Identification (SCP-Nano) reveal that intramuscularly injected lipid nanoparticles (LNPs) can achieve widespread distribution, with studies detecting LNP accumulation in heart tissue, associated with proteome changes suggestive of immune activation and blood vessel damage [9]. Intravenous administration often leads to significant hepatic sequestration, with typically less than 1% of the administered dose reaching brain targets due to the blood-brain barrier (BBB) and clearance by the phagocyte system [48] [43]. Intranasal delivery offers a direct pathway to bypass the BBB via olfactory and trigeminal nerves, facilitating rapid central nervous system (CNS) access and reducing systemic side effects [48] [49].
2. What are the key methodological considerations for tracking nanocarrier distribution with single-cell resolution?
Conventional whole-body imaging techniques like bioluminescence often lack the sensitivity to detect nanocarriers at the low doses used in vaccines, with signal contrast dropping drastically at typical mRNA vaccine doses (e.g., 0.0005 mg kg⁻¹) [9]. For single-cell resolution, an integrated pipeline is required:
- Tissue Clearing: An optimized DISCO whole mouse clearing method, which eliminates urea and reduces dichloromethane incubation time, is crucial for preserving fluorescence signals throughout the mouse body [9].
- High-Resolution Imaging: Light sheet microscopy enables imaging at resolutions of approximately 1–2 µm (lateral) and 6 µm (axial), allowing visualization of extensive cellular targeting across organs [9].
- Deep Learning Analysis: A robust 3D U-Net deep learning pipeline is essential for the unbiased detection and reliable quantification of tens of millions of targeted cells in different tissues, overcoming the limitations of traditional segmentation software [9].
3. When developing a vaccine for a respiratory virus, how do I choose between intramuscular and intranasal delivery to elicit optimal immunity?
The choice depends on whether the goal is to induce strong systemic immunity, robust mucosal immunity, or both.
- Intramuscular (IM) Immunization primarily induces a systemic humoral and cellular response, characterized by high levels of serum IgG and neutralizing antibodies in systemic immune organs. For instance, an MF59-adjuvanted RSV prefusion F (preF) protein vaccine delivered via IM injection induced potent neutralizing antibodies against RSV strains but failed to stimulate a localized mucosal IgA response [50].
- Intranasal (IN) Immunization is superior for triggering local mucosal immunity in the respiratory tract. The same MF59/preF vaccine administered intranasally demonstrated elevated levels of secretory IgA antibodies and an increased frequency of tissue-resident memory T (TRM) cells locally [50].
- Combined IM and IN Delivery can be synergistic. A hybrid regimen of MF59/preF vaccine has been shown to produce stronger antigen-specific humoral and cellular immune responses at both systemic and mucosal sites compared to either route alone [50].
4. What formulation strategies can enhance intranasal delivery efficiency to the brain?
Overcoming rapid mucociliary clearance and poor epithelial permeability is key for effective nose-to-brain delivery. Promising biomaterial-based strategies include:
- Mucoadhesive and Mucodiffusive Polymers: Using star-shaped poly-L-glutamate (PGA) nanocarriers functionalized with ligands like odorranalectin (OL) improves nasal epithelium permeation through receptor-mediated mechanisms [49].
- Redox-Responsive Crosslinking: Introducing disulfide crosslinking (StPGA-CL-SS) enhances mucosal transport by enabling thiol-mediated anchoring to mucin glycoproteins, prolonging nasal residence time [49].
- Depot-Forming Hydrogels: Incorporating a hyaluronic acid–poly-L-glutamate crosspolymer (HA-CP) vehicle can prolong nasal residence time to approximately 4 hours and increase total brain accumulation [49].
Quantitative Data Comparison
Table 1: Key Parameter Comparison for Lipid Nanoparticles (LNPs) via Different Routes
| Parameter | Intramuscular (IM) | Intravenous (IV) | Intranasal (IN) |
|---|---|---|---|
| Primary Advantage | Robust systemic immunity; quick absorption into bloodstream [51] | Direct, complete bioavailability in circulation [48] | Bypasses BBB; induces mucosal immunity [48] [50] |
| Typical Time to Max Concentration (Tmax) | Slower systemic delivery (e.g., ~50 min for epinephrine) [52] | Almost instantaneous | Rapid CNS access; variable systemic Tmax |
| Ideal For | Non-live attenuated vaccines (e.g., tetanus, COVID-19) [51] | Chemotherapy, systemic drug delivery [43] | Respiratory pathogens, CNS targets [51] [48] |
| Key Limitation | Can miss mucosal immunity; needle phobia [51] [50] | Significant off-target accumulation; first-pass liver metabolism [48] [43] | Rapid mucociliary clearance; variable absorption [49] [53] |
Table 2: Comparison of Advanced Imaging and Analysis Techniques
| Technique | Mechanism | Sensitivity / Resolution | Key Applications | Limitations |
|---|---|---|---|---|
| SCP-Nano (Single Cell Precision Nanocarrier Identification) | DISCO tissue clearing + light sheet microscopy + deep learning (3D U-Net) [9] | Single-cell resolution across entire mouse body; detects doses as low as 0.0005 mg kg⁻¹ [9] | Comprehensive 3D mapping of nanocarrier distribution; quantification of off-target effects [9] | Complex integrated pipeline; computationally intensive [9] |
| Conventional Bioluminescence Imaging | Detection of light from luciferase-expressing cells | Lacks sensitivity and resolution for low-dose, single-cell analysis [9] | Whole-organ level tracking at high injection doses [9] | Poor signal contrast at low, clinically relevant doses [9] |
| Traditional Histology | 2D thin tissue sections analyzed by microscopy | Subcellular resolution and high sensitivity [9] | Detailed analysis of pre-selected tissue regions [9] | Not suitable for whole-body analysis; limited field of view [9] |
Experimental Protocols
Protocol 1: Evaluating Nanocarrier Biodistribution at Single-Cell Resolution Using the SCP-Nano Pipeline
This protocol is adapted from studies mapping LNP distribution throughout mouse bodies [9].
1. Nanocarrier Preparation:
- Fluorescent Labeling: Tag your nanocarrier (e.g., LNP, liposome, polyplex, AAV) or its payload (e.g., mRNA) with a stable fluorescent dye (e.g., Alexa Fluor 647). Validate that the dye conjugation does not alter the nanocarrier's biodistribution or function [9].
2. Animal Administration and Tissue Preparation:
- Dosing: Administer the nanocarrier at a clinically relevant dose (e.g., 0.0005 mg kg⁻¹ for mRNA vaccines) via the routes under investigation (IM, IV, IN) [9].
- Perfusion and Fixation: At the designated time point, perfuse mice transcardially with a fixative (e.g., 4% paraformaldehyde) to preserve tissue architecture and nanocarrier location.
- Optimized Tissue Clearing: Process the entire mouse body or specific organs using the refined DISCO clearing protocol. Critical steps include eliminating urea and sodium azide and reducing dichloromethane (DCM) incubation time to preserve the fluorescence signal of tagged mRNAs [9].
3. Data Acquisition and Analysis:
- High-Resolution 3D Imaging: Image the cleared tissues using light sheet fluorescence microscopy at a resolution of approximately 1–2 µm (lateral) and 6 µm (axial) [9].
- AI-Based Cell-Level Quantification: Process the large-scale imaging data using the SCP-Nano deep learning pipeline. The recommended model is a 3D U-Net architecture with six encoding and five decoding layers. This pipeline partitions the whole-body data into discrete units for analysis, reliably segmenting and quantifying targeted cells based on factors like particle shape and brightness relative to the neighborhood, not just single-value thresholding [9].
Troubleshooting:
- Poor Fluorescence Signal After Clearing: Ensure the DISCO protocol modifications (no urea, shortened DCM) are strictly followed. Validate the signal preservation by comparing histology slices before and after clearing [9].
- Suboptimal Cell Segmentation: If the deep learning model performance (F1 score) is low on your validation set, use virtual reality (VR)-based annotation to create a high-quality, diverse training dataset from various tissues (head, heart, lungs, kidneys, liver, etc.) [9].
Protocol 2: Comparing Immune Responses for IM vs. IN Vaccination
This protocol is based on research with an MF59-adjuvanted RSV preF protein vaccine [50].
1. Vaccine Formulation:
- Prepare the subunit vaccine antigen (e.g., RSV preF protein) combined with an adjuvant such as an MF59-like oil-in-water emulsion [50].
2. Immunization Schedule:
- Use a prime-boost regimen in appropriate animal models (e.g., BALB/c mice). Administer the vaccine via IM injection (e.g., in the quadricep or deltoid muscle) or IN instillation (e.g., as a nasal drop). For a combined regimen, administer the prime via IM and a boost via IN [50].
- Example Schedule: Prime on Day 0, first boost on Day 21, and second boost on Day 42. Collect samples for analysis 14 days after each immunization [50].
3. Immune Response Analysis:
- Systemic Humoral Immunity: Collect serum and measure antigen-specific IgG levels using ELISA. Perform live virus neutralization assays to quantify neutralizing antibody titers against relevant pathogen strains [50].
- Mucosal Immunity: Collect bronchoalveolar lavage fluid (BALF) and measure levels of antigen-specific secretory IgA using ELISA [50].
- Cellular Immunity: Isolate cells from lymphoid and mucosal tissues. Analyze the frequency of antigen-specific T cells, particularly tissue-resident memory T (TRM) cells, via flow cytometry [50].
Visualization of Workflows and Pathways
SCP-Nano Single-Cell Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Advanced Nanocarrier Distribution Studies
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| SCP-Nano Pipeline [9] | Comprehensive 3D mapping of nanocarrier distribution at single-cell resolution. | Integrates optimized DISCO clearing, light sheet microscopy, and a 3D U-Net deep learning model. |
| MF59-like Adjuvant [50] | Oil-in-water emulsion used to boost immune responses to subunit vaccines. | Enhances humoral and cellular immunity; suitable for both IM and IN administration. |
| Star-shaped Poly-L-glutamate (StPGA) [49] | A rationally designed polypeptide nanocarrier core for intranasal delivery. | Tunable architecture; allows for functionalization with mucoadhesive ligands. |
| Odorranalectin (OL) [49] | A small, cyclic lectin-like peptide ligand conjugated to nanocarriers. | Binds to L-fucose on olfactory epithelium, promoting brain targeting after IN delivery. |
| Hyaluronic Acid–Poly-L-glutamate Crosspolymer (HA-CP) [49] | A depot-forming hydrogel vehicle for intranasal delivery. | Prolongs nasal residence time (up to ~4 hours) and increases brain accumulation. |
| DISCO Tissue Clearing Reagents [9] | A set of chemicals for making whole tissues transparent for 3D imaging. | The refined protocol (without urea, reduced DCM) is critical for fluorescence signal preservation. |
| Lipid Nanoparticles (LNPs) [9] [54] | Versatile nanocarriers for delivering a wide range of therapeutics, including mRNA. | Composed of ionizable lipids, phospholipids, cholesterol, and PEG-lipids; protect payload and facilitate cellular uptake. |
Leveraging AI for Predictive Modeling of Nanocarrier-Cell Interactions
Frequently Asked Questions (FAQs)
FAQ 1: What are the main advantages of using AI to study nanocarrier-cell interactions? AI, particularly deep learning models, enables the analysis of complex, high-dimensional datasets generated from single-cell experiments. It can identify non-linear relationships between nanocarrier properties and their biological behavior, predict biodistribution patterns, and optimize design parameters far more efficiently than traditional trial-and-error approaches. This data-driven strategy accelerates the development of precise and safe nanocarrier-based therapeutics [55].
FAQ 2: My model performs well on training data but poorly on new experimental data. What could be wrong? This is often a sign of overfitting or a dataset that lacks diversity. Ensure your training data encompasses the full range of nanocarrier properties (size, surface charge, composition) and biological conditions (cell types, serum concentrations) you intend to model. Employing cross-validation during training and using techniques like data augmentation can improve model generalizability. The iterative AI workflow emphasizes continuous model refinement with new experimental data to enhance predictive accuracy [55].
FAQ 3: What experimental methods are essential for validating AI predictions on single-cell nanocarrier distribution? Advanced imaging techniques that provide high-resolution, whole-body data are crucial for validation. The SCP-Nano pipeline, which combines optimized tissue clearing, light-sheet microscopy, and deep learning, can comprehensively quantify nanocarrier targeting throughout an entire organism at single-cell resolution. This provides the high-quality, volumetric data needed to confirm AI-generated hypotheses about off-target accumulation and tissue tropism [9]. Other methods like imaging flow cytometry also offer high-throughput, single-cell data suitable for validation [11].
FAQ 4: Why does my targeted nanocarrier still show significant accumulation in the liver and spleen? This is a common challenge due to the body's natural clearance mechanisms, specifically the Mononuclear Phagocyte System (MPS). Even with targeting ligands, a substantial portion of intravenously administered nanocarriers is often sequestered by the liver and spleen. The use of "stealth" coatings like polyethylene glycol (PEG) can help mitigate this, but shifting the entire biodistribution profile remains difficult. AI models can help predict how different surface modifications influence this off-target accumulation [56] [57].
Troubleshooting Guides
Guide 1: Addressing Low Contrast in Single-Cell Imaging Data
Poor contrast between nanocarrier signals and cellular background can severely limit the accuracy of AI-based quantification.
- Problem: Weak or blurred fluorescent signal from nanocarriers.
- Solution:
- Verify Labeling: Confirm the fluorescent tag is stable and does not detach from the nanocarrier. Use dyes like Alexa Fluor that are known for brightness and photostability [9].
- Optimize Clearing: If using tissue clearing techniques, ensure the protocol preserves fluorescence. For DISCO-based methods, this may involve eliminating urea and reducing dichloromethane incubation times [9].
- Validate Specificity: Perform control experiments to ensure the signal originates from internalized nanocarriers and not from free dye or non-specific binding.
Guide 2: Improving AI Model Performance for Biodistribution Prediction
- Problem: Model predictions do not match in vivo results.
- Solution:
- Curate Better Features: Instead of using only basic nanocarrier properties (e.g., size, charge), incorporate features derived from 'omics data or advanced characterization of the protein corona.
- Increase Data Diversity: Train your model on a wider variety of nanocarrier types (LNPs, liposomes, polyplexes, AAVs) and administration routes to improve its robustness [9] [55].
- Adopt a Robust Pipeline: Implement an integrated pipeline like SCP-Nano, which uses a dedicated 3D U-Net model trained on diverse tissue patches. This approach has been shown to achieve high instance F1 scores (over 0.73) for segmenting targeted cells across entire organs [9].
Experimental Protocols
Protocol: SCP-Nano for Whole-Body, Single-Cell Quantification of Nanocarriers
This protocol outlines the method for mapping nanocarrier biodistribution with single-cell resolution, as detailed in the search results [9].
1. Sample Preparation and Administration
- Nanocarrier Formulation: Prepare fluorescence-labeled nanocarriers (e.g., LNPs, liposomes, AAVs). For mRNA-loaded LNPs, tag the mRNA with a stable fluorescent dye (e.g., Alexa Fluor 647).
- Animal Administration: Administer nanocarriers to mice via the desired route (e.g., intravenous, intramuscular) at a clinically relevant dose (as low as 0.0005 mg kg⁻¹).
2. Tissue Processing and Clearing
- Perfusion and Fixation: Perfuse mice with fixative to preserve tissue architecture and nanocarrier location.
- Optimized DISCO Clearing: Clear the entire mouse body using a modified DISCO protocol. Critical steps include:
- Omitting urea and sodium azide from clearing solutions.
- Reducing the incubation time in dichloromethane (DCM).
- Validate that clearing preserves the fluorescence signal and nanocarrier integrity by comparing histology before and after clearing.
3. Light-Sheet Microscopy and Data Acquisition
- Image Acquisition: Image the entire cleared mouse body using light-sheet fluorescence microscopy at a resolution of approximately 1–2 µm (lateral) and 6 µm (axial).
- Data Management: The output will be a large-scale 3D image dataset of the entire mouse, revealing nanocarrier fluorescence at the single-cell level across all tissues.
4. AI-Based Analysis with 3D U-Net
- Data Partitioning: Partition the whole-body image data into smaller, manageable 3D patches for analysis.
- Model Training: Train a 3D U-Net deep learning model using a VR-annotated dataset. The training data should include 3D patches randomly selected from diverse tissues (e.g., liver, spleen, heart, lungs).
- Segmentation and Quantification: Use the trained model to detect and segment individual nanocarrier-targeted cells. The
cc3dlibrary can then be used to identify each segmented instance and calculate metrics like size and signal intensity contrast relative to the background. - Data Output: The pipeline generates organ-level and whole-body statistics, including the density and location of nanocarrier-targeted cells.
Key Quantitative Data from SCP-Nano Analysis
Table 1: Performance Metrics of the SCP-Nano AI Pipeline [9]
| Metric | Value | Context |
|---|---|---|
| Average Instance F1 Score | 0.7329 | Independent test dataset |
| Organ-Specific F1 Scores | 0.6857 - 0.7967 | Range across different organs |
| Detection Dose Limit | 0.0005 mg kg⁻¹ | Far below conventional imaging limits |
| Spatial Resolution | ~1-2 µm (lateral), ~6 µm (axial) | Enables single-cell resolution |
Table 2: Comparison of Single-Cell Analysis Techniques [11]
| Technique | Throughput | Key Strength | Key Limitation |
|---|---|---|---|
| SCP-Nano (Light-sheet + AI) | Medium-High | Whole-body, 3D single-cell mapping | Requires tissue clearing |
| Imaging Flow Cytometry | High | High-speed single-cell images | Lack of volumetric tissue context |
| Mass Cytometry (CyTOF) | High | Multiplexed metal tagging | No visual information on sub-cellular location |
| Conventional Flow Cytometry | Very High | Rapid phenotyping and sorting | Limited detail on spatial distribution |
Workflow Diagrams
AI-Nanocarrier Development Workflow
SCP-Nano Experimental Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AI-Driven Nanocarrier Research
| Reagent / Material | Function in Research | Example Use Case |
|---|---|---|
| Lipid Nanoparticles (LNPs) | A primary nanocarrier type for delivering therapeutic nucleic acids (e.g., mRNA). | Used in SCP-Nano to study dose-dependent biodistribution after different injection routes [9]. |
| Adeno-Associated Viruses (AAVs) | Viral vector for efficient gene delivery; various serotypes have different tissue tropisms. | SCP-Nano revealed an AAV2 variant transduces adipocytes throughout the body [9]. |
| Alexa Fluor Dyes | Bright, photostable fluorescent tags for labeling nanocarriers or their payloads. | Conjugated to mRNA inside LNPs to enable sensitive detection after tissue clearing [9]. |
| DISCO Clearing Reagents | Chemical cocktails for making biological tissues transparent for 3D microscopy. | An optimized DISCO protocol is central to the SCP-Nano pipeline for whole-body imaging [9]. |
| 3D U-Net Model | A deep learning architecture for volumetric image segmentation. | The core AI model in SCP-Nano for detecting nanocarrier-targeted cells in large 3D image datasets [9]. |
Addressing Protein Corona Formation and Its Impact on Targeting Specificity
Frequently Asked Questions (FAQs)
FAQ 1: What is the protein corona and why does it fundamentally alter the behavior of my nanocarriers?
When nanocarriers enter a physiological environment (e.g., blood plasma), proteins and other biomolecules rapidly adsorb onto their surface, forming a layer known as the "protein corona" [58] [59]. This corona provides the nanocarriers with a new biological identity, which is different from their synthetic identity created in the lab [60]. This new identity is what cells and tissues actually "see" and interact with, ultimately determining critical behaviors like cellular uptake, biodistribution, toxicity, and targeting efficacy [58] [60]. The corona can mask surface-bound targeting ligands (like antibodies or peptides), leading to a loss of targeting specificity and unintended off-target effects [58].
FAQ 2: My nanocarriers are losing their targeting ability in biological media. How can I mitigate the corona's masking effect?
The loss of targeting is a common consequence of protein corona formation. Strategies to mitigate this include:
- Surface Engineering: Pre-coating nanocarriers with specific "stealth" proteins, such as clusterin or apolipoprotein A1 (ApoA1), can create a pre-defined corona that helps evade immune recognition and may reduce the nonspecific adsorption of other proteins [61].
- Polymer Modification: Modifying the surface with hydrophilic polymers can minimize protein adsorption. Glycosylated polyhydroxy polymers with a balanced ratio of amino and hydroxyl groups have been shown to effectively suppress immunoglobulin adsorption, leading to prolonged circulation and a more favorable corona composition in target tissues like tumors [62].
- Rational Design: The physicochemical properties of the nanocarrier—including size, surface charge, and hydrophobicity—directly influence corona composition. Tuning these parameters can help steer the corona toward a more desirable profile [5] [59].
FAQ 3: Are in vitro protein corona studies reliable for predicting in vivo behavior?
There are significant differences between in vitro and in vivo protein coronas, not only in the quantity of adsorbed proteins but also in their composition and structure [59]. The complex and dynamic nature of in vivo environments is difficult to fully replicate in a lab dish. Therefore, while in vitro studies provide valuable initial insights, their predictive power for in vivo outcomes is limited. Characterizing the corona after in vivo administration provides a more accurate picture [59].
FAQ 4: How do washing protocols during corona isolation affect my results?
The choice of washing media (e.g., PBS, water, Tris buffer) has a major impact on the final composition of the isolated "hard corona" [60]. Different washing solutions can remove loosely-bound proteins to varying degrees, directly influencing which proteins are identified in subsequent analyses like SDS-PAGE or LC-MS. This, in turn, can affect the interpretation of which proteins are responsible for observed cellular uptake. It is critical to standardize and report washing protocols to ensure meaningful and comparable data [60].
Troubleshooting Guides
Problem: Inconsistent or Irreproducible Cellular Uptake and Targeting Results
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Variable Corona Formation | Characterize the protein corona formed in different biological media (e.g., plasma from different species, different serum lots) using SDS-PAGE and LC-MS/MS [60] [59]. | Standardize the protein source and incubation conditions. Consider pre-coating nanocarriers with a defined protein layer to create a more consistent biological identity [61]. |
| Improper Washing Protocol | Review and document the exact washing media and steps used to isolate the corona. Test how different washing buffers affect the final corona composition and subsequent cell uptake [60]. | Adopt a consistent, physiologically-relevant washing buffer (e.g., a buffer with a defined pH and ionic strength) and clearly document it in your methods [60]. |
| Uncontrolled Nanocarrier Properties | Use DLS to monitor batch-to-batch consistency in size and PDI. Use ELS to measure zeta potential [5]. | Rigorously control synthesis parameters to ensure consistent nanocarrier size, surface charge, and morphology, as these properties dictate corona formation [5] [59]. |
Problem: Rapid Clearance of Nanocarriers from Bloodstream by the Immune System
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Adsorption of Opsonins | Perform proteomic analysis of the in vivo corona to identify the presence of opsonin proteins (e.g., immunoglobulins, complement factors) [59]. | Engineer a "stealth" corona by pre-adsorbing dysopsonins like clusterin or ApoA1 [61]. Modify the surface with polymers like glycosylated polyhydroxy polymers to minimize opsonin binding [62]. |
| Aggregation in Biological Fluid | Use DLS and TEM to check for size increase and aggregation after incubation with plasma [61] [5]. | Optimize surface chemistry and polymer coating to improve colloidal stability in high-ionic-strength environments. Note that carboxyl-functionalized particles may be prone to aggregation in mouse plasma [61]. |
Experimental Protocols for Characterizing the Protein Corona
Protocol 1: In Vitro Protein Corona Formation and Isolation for SDS-PAGE Analysis
This protocol is used to qualitatively analyze the protein profile adsorbed onto nanocarriers.
- Incubation: Incubate a standardized concentration of your nanocarriers (e.g., 1 mg/mL) with the selected biological fluid (e.g., human citrate plasma or serum) at a physiologically relevant temperature (37°C) for a desired time (e.g., 1 hour) with gentle agitation [60].
- Isolation: Separate the protein-coated nanocarriers from unbound proteins using an appropriate method:
- Ultracentrifugation: Centrifuge at high speed (e.g., 100,000 × g for 1 hour) to pellet the nanocarrier-corona complexes [60] [59].
- Size-Exclusion Chromatography (SEC): Use a column to separate larger nanocarrier-corona complexes from smaller, unbound proteins [59].
- Magnetic Separation: If using magnetic nanocarriers, use a magnet to isolate the complexes [59].
- Washing: Resuspend the pellet in a controlled washing buffer (see FAQ 4). Repeat the isolation step 2-3 times to remove loosely associated proteins [60].
- Elution and Denaturation: Resuspend the final pellet in an SDS-PAGE sample buffer and heat at 95°C for 5-10 minutes to denature and elute the proteins from the nanocarrier surface.
- Analysis: Load the supernatant onto an SDS-PAGE gel to separate the proteins by molecular weight and visualize them with a stain like Coomassie Blue [60] [62].
Protocol 2: Proteomic Analysis of the Corona via Liquid Chromatography-Mass Spectrometry (LC-MS/MS)
This protocol identifies and quantifies the specific proteins in the corona.
- Steps 1-3: Follow the incubation, isolation, and washing steps from Protocol 1.
- Protein Digestion: Instead of SDS-PAGE buffer, digest the hard corona proteins directly on the nanocarrier surface using a protease like trypsin.
- Peptide Analysis: Analyze the resulting peptides using nano-liquid chromatography coupled to tandem mass spectrometry (nano-LC-MS/MS) [61] [59].
- Data Processing: Use database search engines (e.g., MaxQuant) to identify proteins from the mass spectra. Label-free quantification methods can be used to compare the relative abundance of different proteins in the corona [61] [60].
Data Presentation
Table 1: Common Characterization Techniques for Protein Corona and Nanocarriers
| Technique | Measures | Key Insights | Limitations |
|---|---|---|---|
| Dynamic Light Scattering (DLS) [5] | Hydrodynamic size, Polydispersity Index (PDI) | Indicates changes in size due to corona formation and aggregation. | Less reliable in polydisperse samples or biological media. |
| Electrophoretic Light Scattering [5] | Zeta Potential | Measures surface charge change after protein adsorption. | Requires sample dilution; sensitive to ionic strength and pH. |
| SDS-PAGE [60] [62] | Protein molecular weight profile | Qualitative overview of the protein corona composition. | Does not identify specific proteins; less sensitive. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) [61] [59] | Protein identity and abundance | Provides a detailed, quantitative profile of the corona proteome. | Complex, expensive, requires expertise; may lose weakly bound proteins during isolation. |
| Transmission Electron Microscopy (TEM) [61] [5] | Morphology, size, and aggregation | Visualizes the nanocarrier and can sometimes visualize a dense corona layer. | Sample preparation (drying, staining) may alter the native state of the corona. |
| Single Cell Precision Nanocarrier Identification (SCP-Nano) [9] | Single-cell biodistribution of nanocarriers in whole organisms | Directly quantifies targeting efficiency and off-target effects in vivo, revealing the functional outcome of corona formation. | Complex integrated pipeline of tissue clearing, light-sheet microscopy, and deep learning. |
Table 2: Example Protein Corona Compositions on Different Nanocarrier Types
| Nanocarrier Type & Surface Properties | Key Proteins Identified in Corona (Top Hits) | Observed Biological Impact |
|---|---|---|
| Lipid Nanoparticles (LNPs) [9] | Not specified in results, but method allows for single-cell resolution biodistribution analysis. | Biodistribution patterns are route-dependent; intramuscular injection led to heart tissue accumulation with proteome changes suggesting immune activation. |
| Polystyrene NPs (Plain, Amino-, Carboxyl-) [61] | Clusterin, Apolipoprotein A1 (when pre-coated); composition varies with plasma source (human vs. murine). | Pre-coating with clusterin/ApoA1 can enhance stealth properties. Significant discrepancies observed between human and murine systems. |
| Glycosylated Polyhydroxy Nanovesicles (CP1-LVs) [62] | Suppressed immunoglobulins in blood; enriched CD44 and Osteopontin in tumor interstitial fluid. | Prolonged circulation and mediated selective tumor cell internalization due to environmentally-dependent corona transformation. |
| Gold Nanoparticles (AuNPs) [59] | Serum albumin, alpha-2-macroglobulin, Hemoglobin subunits. | Protein composition and abundance depend heavily on the core material, size, and surface chemistry of the nanocarrier. |
Workflow and Pathway Visualizations
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Protein Corona and Targeting Studies
| Item | Function/Benefit | Example Application in Research |
|---|---|---|
| Lipid Nanoparticles (LNPs) [9] | Versatile, clinically approved platform for nucleic acid and drug delivery. | Used in SCP-Nano pipeline to study single-cell biodistribution after different injection routes [9]. |
| Pre-coated 'Stealth' Proteins (Clusterin, ApoA1) [61] | Forms a pre-defined corona to evade macrophage uptake and improve blood circulation time. | Engineered onto nanoparticle surfaces to study stability and stealth effects in interspecies plasma [61]. |
| Glycosylated Polyhydroxy Polymers [62] | Surface modification that regulates protein corona formation by presenting amino/hydroxyl groups, reducing immune protein adsorption. | Modified onto nanovesicles (CP-LVs) to achieve prolonged circulation and tumor-specific protein adsorption [62]. |
| Asymmetrical Flow Field-Flow Fractionation (AF4) [5] | Separates nanocarriers by size before characterization, improving accuracy for polydisperse samples. | Coupled with DLS or MS to analyze nanocarrier size and corona composition without aggregation artifacts [5]. |
| SCP-Nano Pipeline [9] | Integrated method (clearing, imaging, AI) to map nanocarrier biodistribution at single-cell resolution across entire organisms. | Quantifies targeting efficiency and reveals off-target accumulation for various nanocarriers (LNPs, liposomes, AAVs, DNA origami) [9]. |
| 3D U-Net Deep Learning Model [9] | AI tool for reliably detecting and quantifying millions of nanocarrier-targeted cells in large 3D image datasets. | Used within SCP-Nano for unbiased, high-throughput quantification of whole-body biodistribution data [9]. |
Validation Frameworks and Comparative Analysis of Nanocarrier Platforms
Benchmarking SCP-Nano Against Conventional Imaging and Analysis Methods
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What is the core technological advantage of SCP-Nano over conventional imaging like SPECT or bioluminescence? SCP-Nano provides single-cell resolution across entire organisms, a capability conventional methods lack. While traditional whole-body imaging (e.g., SPECT, CT, MRI, bioluminescence) offers organ-level visibility, SCP-Nano combines optical tissue clearing, light-sheet microscopy, and a specialized deep-learning pipeline to detect and quantify nanocarriers at the single-cell level throughout a whole mouse body. Furthermore, its sensitivity is vastly superior, detecting nanocarrier doses as low as 0.0005 mg kg−1, which is 100–1,000 times below the detection limit of conventional techniques [9] [13].
Q2: Our lab is familiar with Imaris for image analysis. Why does SCP-Nano require a custom deep-learning model? Existing software solutions, including filter-based Imaris and other deep-learning tools like DeepMACT, delivered suboptimal performance (F1 scores < 0.50) when tasked with reliably detecting and quantifying the tens of millions of targeted cells in the large, diverse datasets generated by SCP-Nano. The custom 3D U-Net model was developed specifically to handle this scale and complexity, achieving a high average instance F1 score of 0.7329 on test data, enabling unbiased and reliable organ-level and cell-level quantification [9].
Q3: We observed signal loss during tissue clearing in our pilot study. How does SCP-Nano address this? The SCP-Nano protocol uses an optimized DISCO tissue-clearing method. Key modifications to the standard protocol include the elimination of urea and sodium azide and a reduction in dichloromethane (DCM) incubation time. These steps were found to be crucial for preserving the fluorescence signal of Alexa Fluor–tagged mRNAs and nanocarriers throughout the entire mouse body. Validation via histology confirmed that both signal contrast and the number of positive structures were well preserved after this optimized clearing process [9].
Q4: For nanocarrier development, what specific off-target effects has SCP-Nano been able to identify? A key finding enabled by SCP-Nano was that intramuscularly injected Lipid Nanoparticles (LNPs) carrying SARS-CoV-2 spike mRNA can reach heart tissue. Subsequent proteomic analysis of this off-target site revealed changes in the expression of proteins related to immune activation and blood vessel damage, providing a mechanistic insight into potential side effects. This level of precise, whole-body off-target detection is not feasible with conventional methods [9] [13] [63].
Q5: Is SCP-Nano applicable only to Lipid Nanoparticles (LNPs)? No, the SCP-Nano platform is highly generalizable. It has been successfully applied to profile a wide range of nanocarriers, including:
- Liposomes (e.g., based on the Doxil formulation)
- Polyplexes (e.g., based on branched polyethyleneimine)
- DNA origami structures
- Adeno-associated viruses (AAVs) [9] [13]
Troubleshooting Guides
Issue: Low Signal-to-Noise Ratio in Whole-Body Images
- Potential Cause: Inefficient tissue clearing or fluorophore quenching.
- Solution:
- Preventive Measure: Conduct a pilot test to confirm that your chosen fluorescent label (e.g., Alexa Fluor tags) is compatible with the entire SCP-Nano pipeline, from administration to clearing and imaging [9].
Issue: Inaccurate Cell Segmentation by the AI Pipeline
- Potential Cause: The deep learning model may not generalize well to your specific nanocarrier or tissue type.
- Solution:
- Verify Input Data Quality: Ensure your 3D image data has sufficient resolution (approximately 1–2 µm lateral, approximately 6 µm axial) and contrast [9].
- Leverage the VR Annotation Method: For highly specialized applications, consider using the virtual reality (VR)-based annotation method described in the original study to generate high-quality, customized training data to fine-tune the model for your specific needs [9].
- Preventive Measure: When starting with a new nanocarrier type, initially compare the AI's segmentation results with manual annotations on a small tissue volume to assess baseline performance.
Issue: Difficulty Reproducing Biodistribution Quantification
- Potential Cause: Inconsistent injection doses or routes, or variability in data analysis parameters.
- Solution:
- Standardize Administration: Precisely control the injection route (intravenous, intramuscular, intranasal) and use doses within the validated range (down to 0.0005 mg kg−1) [9].
- Use the Provided Analysis Pipeline: Adhere to the published SCP-Nano computational workflow, which partitions whole-body data into discrete units for analysis and uses the
cc3dlibrary to identify individual segmented cell instances and calculate organ-level statistics [9].
Comparative Performance Data
The table below summarizes a quantitative benchmark of SCP-Nano against conventional imaging methods.
| Feature | SCP-Nano | Conventional SPECT/CT | Bioluminescence Imaging |
|---|---|---|---|
| Spatial Resolution | Single-cell (1-2 µm lateral) [9] | Organ level (millimeter to centimeter) [9] [64] | Organ level (millimeter to centimeter) [9] |
| Detection Sensitivity | ~0.0005 mg kg⁻¹ [9] [13] | Requires much higher doses [9] | Loses contrast at low doses (e.g., 0.0005 mg kg⁻¹) [9] |
| Quantitative Output | Single-cell counts & spatial mapping via AI (F1 score: 0.73) [9] | Voxel-level activity concentration [64] | Relative luminescence units (organ-level) |
| Whole-Body 3D Mapping | Yes, with single-cell detail [9] | Yes, but at organ-level resolution [64] | Limited, poor depth penetration [9] |
| Key Technology | Tissue clearing + Light-sheet microscopy + AI [9] [13] | Gamma camera detection + CT [64] | Photon detection from luciferase reaction |
Experimental Protocols
Protocol 1: Validating SCP-Nano Against a Conventional Method (Bioluminescence)
Objective: To compare the biodistribution of LNPs at a clinically relevant low dose using both bioluminescence imaging and the SCP-Nano pipeline.
Materials:
- Mice (e.g., C57BL/6)
- LNPs carrying EGFP mRNA tagged with a fluorescent dye (e.g., Alexa Fluor 647)
- In vivo imaging system (IVIS) or equivalent for bioluminescence
- Reagents for optimized DISCO tissue clearing [9]
- Light-sheet fluorescence microscope
Methodology:
- Administration: Inject mice intramuscularly or intravenously with LNPs at a low dose (e.g., 0.0005 mg kg−1) [9].
- Bioluminescence Imaging:
- At a predetermined time post-injection (e.g., 6-24 hours), image live animals using the bioluminescence system.
- Document the signal distribution and contrast, which is expected to be low at this dose [9].
- SCP-Nano Processing:
- Data Analysis:
- Process the 3D image data through the SCP-Nano deep learning pipeline (3D U-Net model) to segment and quantify targeted cells in each organ [9].
- Compare the detailed, single-cell distribution map from SCP-Nano with the organ-level, low-contrast image from bioluminescence.
Protocol 2: Profiling Off-Target Effects of mRNA-LNPs
Objective: To identify and validate off-target accumulation of LNPs and associated physiological effects.
Materials:
- As in Protocol 1, plus reagents for proteomic analysis (e.g., mass spectrometry).
Methodology:
- Administration & Imaging: Follow Steps 1-4 from Protocol 1 to obtain the whole-body, single-cell distribution of LNPs.
- Off-Target Identification: Use the SCP-Nano quantification data to identify organs or tissues with unexpected LNP accumulation (e.g., heart tissue) [9] [13].
- Spatial Proteomics:
- Dissect the identified off-target tissue (e.g., heart) and a control tissue (e.g., muscle).
- Perform proteomic analysis (e.g., using liquid chromatography-mass spectrometry) on these tissues [9].
- Data Integration:
- Correlate the spatial location of LNP accumulation with changes in the proteome.
- As demonstrated, look for upregulated proteins involved in immune response and vascular integrity to hypothesize mechanisms for potential side effects [9].
Signaling Pathways and Experimental Workflows
SCP-Nano Experimental Workflow
AI Segmentation Pipeline Logic
Research Reagent Solutions
The following table lists key materials and reagents essential for implementing the SCP-Nano methodology.
| Reagent / Material | Function / Description | Example / Note |
|---|---|---|
| Fluorescently-Labeled Nanocarriers | The subject of the study; must be tagged for detection. | LNPs with Alexa Fluor-tagged mRNA; Liposomes (Doxil-based); DNA origami [9]. |
| DISCO Clearing Reagents | Renders whole mouse bodies transparent for light-sheet microscopy. | Critical: Use urea-free, sodium azide-free formulation with reduced DCM time [9]. |
| Light-Sheet Fluorescence Microscope | Generates high-resolution 3D images of cleared tissues. | Provides ~1-2 µm lateral and ~6 µm axial resolution for single-cell detection [9]. |
| 3D U-Net Deep Learning Model | Core AI for segmenting targeted cells from large 3D image datasets. | Trained on VR-annotated data; achieves an F1 score of ~0.73 [9]. |
| Virtual Reality (VR) Annotation Tool | Creates high-quality training data for the AI model. | Used for manual, 3D annotation of image patches to train the segmentation model [9]. |
Comparative Biodistribution of Lipid, Polymeric, and Viral Nanocarriers
Troubleshooting Guides & FAQs
FAQ 1: What are the key factors causing off-target nanocarrier accumulation and how can they be mitigated?
Answer: Off-target accumulation is primarily influenced by nanocarrier physicochemical properties and injection route. It can lead to reduced therapeutic efficacy and increased side effects.
- Root Cause 1: Physicochemical Properties. The size, surface charge, and composition of the nanocarrier fundamentally determine its biodistribution. For example, large particles (>100 nm) or those with a positive surface charge are more readily cleared by the liver and spleen [5].
- Solution: Carefully characterize and control the nanocarrier's properties. Use Dynamic Light Scattering (DLS) for size and surface charge (zeta potential), and Atomic Force Microscopy (AFM) or electron microscopy for morphology [5]. Aim for a size range of 10-100 nm and a near-neutral or slightly negative surface charge to prolong circulation.
- Root Cause 2: Injection Route. The administration pathway (e.g., intravenous, intramuscular, intranasal) directly defines the initial biological barriers the nanocarrier encounters and its subsequent distribution profile [9].
- Solution: Select the injection route based on the target tissue. For example, intramuscular injection, common for vaccines, can lead to widespread distribution, including to the heart, as detected by sensitive imaging techniques [9] [18]. Consider local administration for localized targets.
- Root Cause 3: Protein Corona. Upon entering a biological fluid, nanocarriers are rapidly coated with proteins, forming a "corona" that can mask targeting ligands and alter their cellular interactions [9].
- Solution: Use surface functionalization with polymers like polyethylene glycol (PEG) to reduce protein adsorption. However, be aware that repeated dosing with PEGylated nanocarriers can induce immune responses [43].
FAQ 2: Why is my nanocarrier not reaching the intended subcellular compartment, such as the nucleus?
Answer: Reaching a specific subcellular organelle like the nucleus requires overcoming multiple intracellular barriers after cellular uptake.
- Root Cause: Endo/Lysosomal Trapping. Most nanocarriers are internalized via endocytosis and become trapped in endosomes and lysosomes, where the acidic environment and enzymes can degrade the cargo before it reaches the cytoplasm or nucleus [43].
- Solution: Employ active subcellular targeting strategies. Incorporate Nuclear Localization Signals (NLS), which are short peptide sequences that hijack the cell's nuclear import machinery, facilitating transport through nuclear pores [43]. This is crucial for gene therapies where the target is genomic DNA.
FAQ 3: What are the best methods to quantify biodistribution at the single-cell level, especially for low-dose studies?
Answer: Conventional whole-body imaging techniques often lack the sensitivity and resolution for low-dose, single-cell analysis.
- Challenge: Techniques like bioluminescence imaging lose signal contrast at very low doses (e.g., 0.0005 mg kg⁻¹, common in vaccines), making off-target detection difficult [9].
- Recommended Solution: Single Cell Precision Nanocarrier Identification (SCP-Nano). This integrated pipeline combines tissue clearing, light-sheet microscopy, and deep learning to map nanocarrier distribution across the entire mouse body with single-cell resolution [9] [18].
- Workflow:
- Tissue Clearing: Use an optimized DISCO method (e.g., omitting urea and reducing dichloromethane time) to make the whole mouse body transparent while preserving fluorescence.
- Imaging: Image the entire cleared body with light-sheet fluorescence microscopy at high resolution (~1-2 µm laterally).
- Analysis: Analyze the massive 3D image data with a dedicated deep learning model (e.g., a 3D U-Net) to automatically identify and quantify every targeted cell in every organ [9].
- Workflow:
- Alternative Methods: For high-throughput analysis of cell suspensions, imaging flow cytometry can provide single-cell data and visual confirmation of nanoparticle internalization [11].
Quantitative Biodistribution Data
The following tables summarize key quantitative findings from comparative biodistribution studies.
Table 1: Key Biodistribution Findings from Comparative Studies
| Nanocarrier Type | Cargo / Label | Key Biodistribution Finding | Experimental Model | Reference |
|---|---|---|---|---|
| Polymeric (PEBCA) | Cabazitaxel (Cbz) | >50x higher concentration ratio in all organs vs. blood compared to IR780-oleyl in NLCs | Healthy Rats | [65] |
| Polymeric (PEBCA) | Cabazitaxel (Cbz) | Notable and prolonged accumulation in lung tissue; higher brain accumulation with increasing dose | Healthy Rats | [65] |
| Lipid (LNP - MC3) | EGFP mRNA (Alexa-tagged) | Widespread cellular targeting in liver and spleen at ultra-low doses (0.0005 mg kg⁻¹) | Mouse | [9] |
| Lipid (LNP) | SARS-CoV-2 spike mRNA | Detection in heart tissue after intramuscular injection, associated with proteome changes | Mouse | [9] [18] |
Table 2: Dose-Linearity and Organ Accumulation Trends
| Parameter | Polymeric Nanoparticle (Cbz) | Nanostructured Lipid Carrier (IR780-oleyl) |
|---|---|---|
| Normalized Dose Linearity | Showed a clear trend with increasing injected dose | Opposite trend to polymeric nanoparticles after injection |
| Organ-to-Blood Ratio | Consistently high across all organs | More than 50-fold lower than polymeric nanoparticles |
| Specific Organ Accumulation | Pronounced accumulation in lungs; brain accumulation at higher doses | Not specified in the provided results |
Experimental Protocols
Protocol 1: Whole-Body Single-Cell Biodistribution Analysis (SCP-Nano)
This protocol is adapted from the SCP-Nano pipeline for mapping nanocarrier distribution at single-cell resolution across an entire mouse body [9].
1. Sample Preparation and Injection
- Nanocarrier: Use fluorescently labeled nanocarriers (e.g., LNPs with Alexa Fluor-tagged mRNA or dyes conjugated to the lipid component).
- Animal Model: Administer the nanocarrier to mice via the desired route (e.g., intravenous, intramuscular) at a clinically relevant dose (as low as 0.0005 mg kg⁻¹).
2. Tissue Clearing (Optimized DISCO Protocol)
- Perfusion and Fixation: Perfuse the mouse transcardially with phosphate-buffered saline (PBS) followed by 4% paraformaldehyde (PFA). Fix the entire body in 4% PFA for 24-48 hours at 4°C.
- Dehydration: Gradually dehydrate the sample by immersing it in a series of tetrahydrofuran (THF) solutions in water (50%, 70%, 80%, 100%, 100%) for 24 hours each.
- Delipidation and Clearing:
- Incubate the sample in 100% dichloromethane (DCM) for 1-2 hours. Note: Reducing DCM incubation time is crucial for fluorescence preservation.
- Transfer the sample to dibenzyl ether (DBE) until it becomes transparent. Note: This optimized protocol omits urea and sodium azide to protect the fluorescence signal.
3. Light-Sheet Microscopy Imaging
- Mount the cleared mouse body specimen in a custom-made imaging chamber filled with DBE.
- Image the entire body using a light-sheet fluorescence microscope with a resolution of approximately 1-2 µm (lateral) and 6 µm (axial).
- Use appropriate laser wavelengths and filters to detect the fluorescent signal from the nanocarrier.
4. Deep Learning-Based Quantification (SCP-Nano Pipeline)
- Data Partitioning: Partition the whole-body imaging data into smaller 3D patches (e.g., 200x200x200 voxels) for processing.
- Model Application: Analyze the data using a pre-trained 3D U-Net deep learning model. This model was trained on manually annotated datasets from various tissues and achieves a high instance F1 score (~0.73) for identifying targeted cells [9].
- Data Analysis: Use the model output to quantify the number, size, and signal intensity of nanocarrier-positive cells in every organ and tissue. The
cc3dlibrary can be used to identify individual cell instances.
Protocol 2: Analyzing Nano-Bio Interactions via Imaging Flow Cytometry
This protocol provides a high-throughput method for analyzing nanocarrier uptake and interaction with single cells in suspension [11].
1. Cell and Nanocarrier Preparation
- Culture the relevant cell line(s) (e.g., A549 pulmonary cancer cells, HeLa cells) under standard conditions.
- Incubate the cells with fluorescently labeled nanocarriers for a predetermined time.
2. Cell Harvesting and Preparation
- Gently wash the cells with PBS to remove non-internalized nanocarriers.
- Trypsinize adherent cells and resuspend them in a suitable buffer (e.g., PBS with 1% bovine serum albumin) to create a single-cell suspension.
- Pass the cell suspension through a cell strainer to remove aggregates.
3. Data Acquisition on Imaging Flow Cytometer
- Use an imaging flow cytometer (e.g., Annis ImageStream).
- Set up the instrument: use a 488 nm laser for side scatter (SSC) and forward scatter (FSC), and the appropriate lasers and channels to detect the nanocarrier fluorescence.
- Collect data from at least 10,000 cells per sample.
4. Data Analysis
- Use the instrument's software (e.g., IDEAS) for analysis.
- Gating Strategy:
- Gate on single cells using the FSC and SSC area vs. aspect ratio.
- Create a fluorescence intensity histogram for the nanocarrier channel.
- Apply a threshold to distinguish between nanocarrier-positive and negative cells.
- For internalization analysis, use the "internalization feature" which calculates the ratio of fluorescence inside the cell to the fluorescence on the cell membrane.
Visualization Diagrams
SCP-Nano Whole-Body Biodistribution Workflow
Nuclear-Targeted Delivery Strategy
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Advanced Nanocarrier Biodistribution Studies
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| IR780-oleyl dye | A near-infrared (NIR) fluorescent dye tailored for efficient encapsulation in lipid nanocarriers. Used for in vivo imaging and tracking [65]. | Loading into Nanostructured Lipid Carriers (NLCs) for comparative biodistribution studies against polymeric NPs [65]. |
| Poly(2-ethylbutyl cyanoacrylate) (PEBCA) | A biodegradable polymer used to form polymeric nanoparticles with high drug loading and limited burst release [65]. | Nanoformulating cabazitaxel (Cbz) to reduce off-target toxicity and study its accumulation in tissues like lungs and brain [65]. |
| Ionizable Lipid (MC3) | A clinically approved ionizable lipid used to formulate Lipid Nanoparticles (LNPs) for nucleic acid delivery [9]. | Formulating LNPs to encapsulate and deliver mRNA (e.g., EGFP, SARS-CoV-2 spike) in biodistribution and efficacy studies [9]. |
| Nuclear Localization Signal (NLS) Peptide | A short amino acid sequence that binds to importin proteins, facilitating active transport through the nuclear pore complex [43]. | Conjugating to nanocarriers (e.g., gold NPs, polymeric NPs) to achieve subcellular targeting to the nucleus for gene therapy or chemotherapy [43]. |
| Dibenzyl Ether (DBE) | A refractive index matching medium used as the final immersion solvent in DISCO-based tissue clearing protocols [9]. | Rendering the entire mouse body transparent after dehydration and delipidation for deep-tissue light-sheet microscopy [9]. |
Linking Cellular-Level Distribution to Therapeutic Efficacy and Proteomic Changes
Frequently Asked Questions (FAQs)
FAQ 1: What methods enable the tracking of nanocarrier distribution at single-cell resolution across a whole organism?
Current conventional whole-body imaging techniques (e.g., bioluminescence, PET, CT) lack the resolution to identify individual cells targeted by nanocarriers and have limited sensitivity at low doses [9]. To address this, researchers have developed Single Cell Precision Nanocarrier Identification (SCP-Nano), an integrated pipeline that combines advanced tissue clearing, light-sheet microscopy, and deep learning [9] [13].
- Experimental Protocol: SCP-Nano Workflow
- Administer Fluorescence-Labelled Nanocarriers: Nanocarriers (e.g., LNPs, AAVs, liposomes) are fluorescently labeled on the payload (e.g., mRNA) or the carrier structure itself [9].
- Tissue Clearing: Use an optimized DISCO clearing protocol for whole mouse bodies. Key modifications include eliminating urea and sodium azide and reducing dichloromethane incubation time to preserve fluorescence signal [9].
- 3D Imaging: Image the entire cleared mouse body using light-sheet fluorescence microscopy at high resolution (approximately 1–2 µm lateral, 6 µm axial) [9].
- AI-Based Analysis: Process the large-scale imaging data with a dedicated deep learning model (a 3D U-Net architecture) to detect, segment, and quantify nanocarrier-positive cells across all tissues with an average instance F1 score of 0.73 [9].
FAQ 2: How can I investigate proteomic changes resulting from nanocarrier delivery to off-target tissues?
Liquid chromatography-mass spectrometry (LC-MS/MS)-based proteomics is a powerful and high-throughput method for identifying and quantifying protein abundance changes in response to stimuli, such as off-target nanocarrier delivery [66] [67] [68].
- Experimental Protocol: LC-MS/MS Proteomic Analysis
- Sample Preparation:
- Digestion and Preparation: Digest proteins into peptides using trypsin. This can be facilitated by methods like FASP (Filter-Aided Sample Preparation) or SP3 (Single-Pot, Solid-Phase-enhanced Sample Preparation) on magnetic beads [69] [66].
- LC-MS/MS Analysis:
- Data Analysis: Use specialized software (e.g., Skyline, Proteome Discoverer) to identify peptides and proteins. Analyze differential expression and pathway enrichment using bioinformatics tools [67].
FAQ 3: What are the critical nanocarrier properties that influence their cellular-level distribution?
The physicochemical properties of nanocarriers are key determinants of their in vivo journey and final cellular destination [5] [70].
- Particle Size and Polydispersity Index (PDI): Size affects circulation half-life, cellular uptake, and biodistribution. PDI indicates the heterogeneity of the particle population, which should ideally be low for consistent behavior. Characterization is typically done via Dynamic Light Scattering (DLS) [5].
- Surface Charge (Zeta Potential): The surface charge influences stability, aggregation tendencies, and interactions with cell membranes. It is measured by electrophoretic light scattering [5].
- Surface Hydrophobicity: This property impacts protein corona formation and uptake by the mononuclear phagocyte system (MPS), critically affecting biodistribution. It can be assessed via hydrophobic interaction chromatography or biphasic partitioning [5] [70].
Troubleshooting Guides
Problem: Low signal-to-noise ratio when imaging nanocarriers at low doses.
- Potential Cause 1: Signal loss during the tissue clearing process.
- Solution: Optimize the clearing protocol by removing urea and sodium azide and shortening the incubation time in dichloromethane, as these factors can quench fluorescence [9].
- Potential Cause 2: Insufficient sensitivity of the detection method.
Problem: Inaccurate or inefficient quantification of targeted cells from large 3D image datasets.
- Potential Cause: Existing software solutions (e.g., Imaris, DeepMACT) deliver suboptimal performance (F1 scores < 0.50) for this specific task [9].
- Solution: Implement the AI-based analysis pipeline from SCP-Nano. Use a 3D U-Net deep learning model trained on VR-annotated 3D patches from diverse tissues. This approach achieves a high average instance F1 score of 0.73 for segmenting nanocarrier-positive cells [9].
Problem: Inconsistent drug efficacy results in in vitro cell models.
- Potential Cause: Variations in cell density (confluence) at the time of drug treatment, which alters the cellular proteome and can bias drug response [69].
- Solution: Standardize cell seeding numbers and ensure drug treatments are initiated at a consistent, documented cell confluence. Proteomic studies show that key pathways, like the cell cycle, are significantly altered by confluence, directly impacting the efficacy of targeted drugs [69].
Data Presentation Tables
Table 1: Performance Comparison of Nanocarrier Imaging and Analysis Techniques
| Technique | Resolution | Sensitivity (Typical Dose) | Quantification Capability | Key Limitation |
|---|---|---|---|---|
| Bioluminescence/ Optical Imaging | Organ-level | Low (requires ~0.5 mg kg⁻¹) [9] | Low, based on signal intensity | Lacks cellular resolution; poor contrast at low doses [9] |
| PET/CT/MRI | Organ-level | Moderate | Low, based on signal intensity | Cannot resolve single cells [9] |
| Traditional Histology | Single-cell | High | Manual, limited to 2D sections | Not suitable for whole-organism analysis [9] |
| SCP-Nano Pipeline | Single-cell (1-2 µm lateral) [9] | Very High (0.0005 mg kg⁻¹) [9] | AI-based, automated for millions of cells in 3D [9] | Complex integrated workflow requiring specialized expertise |
Table 2: Proteomic Profiling Platforms for Biomarker Discovery
| Platform | Principle | Throughput | Key Advantage | Key Consideration |
|---|---|---|---|---|
| LC-MS/MS (Label-Free) [69] [66] | Mass spectrometry-based protein identification and quantification | High | Unbiased detection; can discover novel proteins [66] | Complex data analysis; high-abundance proteins can mask low-abundance ones |
| Olink [66] | Proximity Extension Assay (antibody-based) | High | High sensitivity and specificity; validated assays | Targeted approach; limited to pre-defined protein panels |
| SomaScan [66] | Slow Off-rate Modified Aptamer (SOMAmer)-based binding | High | Very high multiplexing capacity (up to 11,000 proteins) | Targeted approach; aptamer kinetics may differ from immunoassays |
| Proteograph (Seer) [66] | Nanoparticle-based protein enrichment followed by MS | High | Dramatically expands depth of plasma proteome coverage | High initial cost and reagent expense; requires larger plasma volumes |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Single-Cell Nanocarrier Distribution Studies
| Item | Function/Description | Example from Research |
|---|---|---|
| Fluorescently Labeled Nanocarriers | Enable visualization via microscopy. Can be labeled on the payload (e.g., Alexa Fluor-tagged mRNA) or the carrier lipid [9]. | Alexa Fluor 647 or 750 tagged mRNA encapsulated in MC3-LNPs [9]. |
| DISCO Tissue Clearing Reagents | Render whole biological tissues transparent for deep imaging. | Optimized DISCO protocol without urea/sodium azide [9]. |
| Light-Sheet Fluorescence Microscope | Instrument for rapid, high-resolution 3D imaging of large cleared samples with minimal photobleaching [9] [13]. | Used for imaging entire cleared mouse bodies [9]. |
| Magnetic Beads for Proteomics | Simplify protein/peptide purification and preparation for MS analysis (e.g., SP3 method) [66]. | Used in platforms like Seer's Proteograph for deep plasma proteome profiling [66]. |
| LC-MS/MS System | The core instrumental setup for high-throughput identification and quantification of proteins in a sample [69] [67]. | Thermo Orbitrap Fusion Lumos mass spectrometer with Easy-NLC 1200 system [69]. |
Experimental Protocols
Protocol 1: AI-Powered Single-Cell Quantification of Nanocarriers
Objective: To reliably detect and quantify tens of millions of nanocarrier-targeted cells in whole-body 3D imaging data [9].
- Data Partitioning: Partition the whole-body imaging data into manageable 3D patches (e.g., 200x200x200 to 300x300x300 voxels) to fit computational memory constraints [9].
- Training Dataset Creation: Create a ground-truth dataset by annotating nanocarrier-positive cells in 3D patches using a virtual reality (VR)-based annotation tool. Patches should be randomly selected from diverse tissues (head, heart, lungs, kidneys, liver, etc.) [9].
- Model Training: Train a 3D U-Net deep learning model with six encoding and five decoding layers, using a leaky ReLU activation function. Employ a five-fold cross-validation strategy to optimize performance [9].
- Prediction and Instance Segmentation: Apply the trained model to new whole-body data. Use the
cc3dlibrary to identify individual segmented cell/cluster instances and compute metrics like size and intensity contrast relative to the background [9]. - Data Aggregation and Visualization: Compute organ-level statistics and generate 3D maps of nanocarrier density for visual analysis and interpretation [9].
Protocol 2: Assessing Off-Target Proteomic Effects in Cell Lines
Objective: To comprehensively evaluate changes in the abundance of safety-relevant off-target proteins in human cell lines after treatment with gene silencing or protein-degrading therapeutics [68].
- Define the Selected Off-Target Proteome (SOTP): Systematically select ~2,800 proteins based on human genetics and pharmacological evidence linked to adverse drug reactions in key organ systems [68].
- Select Cell Lines: Use a greedy algorithm to analyze transcriptome data from hundreds of cell lines (e.g., from the Cancer Cell Line Encyclopedia) to select a minimal set (e.g., 4) that collectively expresses ~80% of the SOTP [68].
- Cell Treatment and Sample Prep: Treat selected cell lines with the therapeutic modality. Prepare samples from both cytosolic and secreted protein fractions to cover intracellular and extracellular targets [68].
- LC-MS/MS Analysis and Quantification: Perform label-free quantitative proteomics to measure protein abundance changes. Use intensity-based absolute quantification (iBAQ) [68].
- Bioinformatic Analysis: Identify proteins with statistically significant abundance changes. Cross-reference these with the pre-defined SOTP to prioritize off-targets with potential safety implications [68].
Signaling Pathways and Workflow Diagrams
Toxicity and Biocompatibility Profiles of Leading Nanocarrier Platforms
The development of safe and effective nanocarriers is a critical step in advancing nanomedicine for drug delivery and other biomedical applications. Biocompatibility—the ability of a material to perform its desired function without eliciting any undesirable local or systemic effects in the host—is paramount for clinical translation. Similarly, understanding nanocarrier toxicity is essential for risk assessment and regulatory approval. Different nanocarrier platforms exhibit distinct toxicity profiles based on their physicochemical properties, including composition, size, surface charge, and stability. This technical support guide provides researchers with a comprehensive framework for evaluating these profiles, with particular emphasis on methodologies relevant to single-cell distribution studies.
The table below summarizes the documented toxicity concerns and biocompatibility performance of major nanocarrier platforms based on current literature:
Table 1: Toxicity and Biocompatibility Profiles of Leading Nanocarrier Platforms
| Nanocarrier Platform | Common Materials | Documented Toxicity Concerns | Biocompatibility Advantages | Clinical Status |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Ionizable lipids (e.g., MC3), phospholipids, PEG-lipids | Activation of immune response; proteome changes in heart tissue after intramuscular injection [9] | High biodegradability; FDA-approved formulations; suitable for nucleic acid delivery [9] [71] | Multiple FDA approvals (e.g., COVID-19 mRNA vaccines) |
| Liposomes | Phospholipids, cholesterol | Interaction with blood opsonins; activation of the mononuclear phagocyte system (MPS) [71] | PEGylation reduces opsonization and extends circulation half-life [71] | Multiple FDA approvals (e.g., Doxil, Onivyde) |
| Metal-Organic Frameworks (MOFs) | Zr-based (UiO-66, PCN-222, NU-901), Zn-based (ZIF-8) | Framework-dependent immunotoxicity; specific pro-inflammatory cytokine induction (IL-6); selective cytotoxicity to CD14+ monocytes [72] | Favorable biocompatibility of Zr-, Fe-, and Zr-based frameworks; high porosity for drug loading [72] | Preclinical research stage |
| Polymeric Nanoparticles | Poly(lactic-co-glycolic acid) (PLGA), Polyethyleneimine (PEI) | Potential for hepatotoxicity and nephrotoxicity; charged surfaces can cause non-specific interactions [71] [73] | Biodegradable and biocompatible (e.g., PLGA); tunable surface chemistry [73] | Several in clinical trials (e.g., BIND-014) |
| Inorganic/Metal Nanoparticles | Superparamagnetic Iron Oxide (SPIONs), Gold, Silver | Oxidative stress via ROS generation; DNA damage; inflammation; complement system activation [71] | FDA approval for specific applications (e.g., Ferumoxytol for anemia); useful for imaging and hyperthermia [71] | Some FDA-approved, others discontinued due to toxicity (e.g., Feridex) |
| Carbon-Based Nanotubes | Single-walled (SWCNT), Multi-walled (MWCNT) | Neurotoxicity, pulmonary toxicity, embryotoxicity; induction of anxiety/depression effects in models; ROS promotion [71] | Effective for tumor suppression in animal models; high drug-loading capacity [71] | Preclinical research stage |
Essential Characterization for Toxicity Assessment
A thorough physicochemical characterization is the foundation of any reliable toxicity or biocompatibility assessment. The properties you measure will directly predict the biological behavior of your nanocarriers.
Table 2: Key Physicochemical Properties and Characterization Methods
| Property | Impact on Toxicity/Biocompatibility | Recommended Characterization Techniques |
|---|---|---|
| Particle Size & PDI | Determines cellular uptake, biodistribution, circulation half-life, and clearance [5]. | Dynamic Light Scattering (DLS), Static Light Scattering, Centrifugal Liquid Sedimentation (CLS) [5]. |
| Surface Charge (Zeta Potential) | Indicates colloidal stability and aggregation tendency; influences protein corona formation and cellular interactions [5]. | Electrophoretic Light Scattering (Laser Doppler Velocimetry) [5]. |
| Surface Chemistry & Hydrophobicity | Affulates stability, bioavailability, and cellular uptake; can lead to unintended biomolecular interactions [5] [71]. | X-ray Photon Correlation Spectroscopy, Contact Angle Measurements, Adsorption Probe Methods [5]. |
| Morphology & Shape | Impacts half-life, targeting efficiency, and toxicity (e.g., fiber-like shapes can cause asbestos-like toxicity) [5]. | Atomic Force Microscopy (AFM), Scanning Electron Microscopy (SEM), Transmission Electron Microscopy (TEM) [5]. |
| Aggregation/Agglomeration State | Alters effective particle size and can lead to capillary blockage and altered pharmacokinetics [74]. | DLS, TEM, Asymmetrical Flow Field-Flow Fractionation (AF4) [5]. |
Experimental Protocol: Basic Physicochemical Characterization
Method: Dynamic Light Scattering (DLS) and Zeta Potential Measurement.
- Sample Preparation: Dilute the nanocarrier suspension in the same buffer that will be used for biological studies (e.g., PBS) to a concentration that avoids signal saturation (often between 0.1-1 mg/mL). Filter the buffer through a 0.1 or 0.22 µm filter to remove dust.
- Measurement: Equilibrate the sample in the instrument at 25°C for 2 minutes. For DLS, perform a minimum of 3 measurements per sample to obtain the hydrodynamic diameter and Polydispersity Index (PDI). For Zeta Potential, the sample is placed in a dedicated folded capillary cell, and an electric field is applied. The measurement is based on the electrophoretic mobility of the particles.
- Data Analysis: Report the Z-average diameter and PDI for DLS. A PDI < 0.2 is generally considered monodisperse. For Zeta Potential, report the average value and standard deviation from multiple runs. Highly positive or negative values (> ±30 mV) typically indicate good colloidal stability.
Figure 1: Workflow for Basic Physicochemical Characterization of Nanocarriers
Advanced Immunotoxicity and Single-Cell Biodistribution Profiling
For research focused on optimizing distribution at the single-cell level, advanced models that go beyond basic characterization are required. These methods bridge the gap between in vitro assays and in vivo outcomes.
Experimental Protocol: Hierarchical 'Safety-by-Design' Immunotoxicity Pipeline
This multi-stage workflow, as demonstrated for Metal-Organic Frameworks (MOFs), efficiently de-risks nanocarrier development [72].
Stage 1: In Silico Machine Learning Screening
- Objective: To computationally predict toxicity of nanocarrier components (e.g., metal clusters and organic linkers) before synthesis.
- Methodology: Use trained ML models that classify linker molecules as "fatal," "toxic," or "safe" based on median lethal dose (LD50) thresholds from databases. This allows for high-throughput screening of virtual nanocarrier libraries to prioritize biocompatible candidates [72].
Stage 2: Ex Vivo Human Blood Assays
- Objective: To validate in silico predictions in a human-relevant immune model.
- Methodology:
- Isolate Peripheral Blood Mononuclear Cells (PBMCs) from healthy donors.
- Expose PBMCs to a range of nanocarrier concentrations for 24-48 hours.
- Viability/Apoptosis: Use flow cytometry to assess viability and apoptosis in specific immune cell populations (e.g., CD14+ monocytes, CD3+ T lymphocytes).
- Cytokine Profiling: Quantify a panel of inflammatory cytokines (e.g., IL-6, IL-1β, TNF-α) in the supernatant using a multiplex immunoassay. This identifies framework-dependent "immune fingerprints" [72].
- Cellular Uptake: Use imaging flow cytometry to visualize nanocarrier interactions with different immune cells.
Stage 3: Targeted In Vivo Models
- Objective: To evaluate systemic immunotoxicity and biodistribution in a whole organism.
- Methodology: Advance candidates predicted to be safe (e.g., UiO-66, PCN-222) to animal models (e.g., mice). Administer nanocarriers via the clinically relevant route (e.g., intravenous) and monitor for signs of systemic immune activation, such as transient cytokine release or immune cell infiltration in organs. This stage validates the ex vivo and in silico findings [72].
Experimental Protocol: SCP-Nano for Single-Cell Biodistribution
The Single Cell Precision Nanocarrier Identification (SCP-Nano) pipeline is a breakthrough for quantifying nanocarrier targeting across entire organisms at single-cell resolution, which is crucial for understanding off-target effects and optimizing delivery [9] [18].
Nanocarrier Administration and Tissue Preparation:
- Administer fluorescence-labeled nanocarriers to mice at the desired dose and route (e.g., intravenous, intramuscular).
- Perfuse and fix the whole mouse body. Use an optimized DISCO tissue clearing protocol (modified to preserve fluorescence by eliminating urea and sodium azide and reducing dichloromethane incubation time) to render the entire body transparent [9].
Imaging and Data Processing:
- Image the cleared whole mouse body using light sheet fluorescence microscopy at high resolution (≈1–2 µm lateral, ≈6 µm axial).
- The massive 3D imaging dataset is partitioned into discrete units for analysis.
AI-Based Quantification:
- A deep learning model (a 3D U-Net architecture) is used to detect and quantify nanocarrier-positive cells with high accuracy (F1 score > 0.73) [9].
- The pipeline generates organ-level and whole-body statistics on nanocarrier density, identifying even low-intensity off-target sites (e.g., LNP accumulation in heart tissue) that are missed by conventional imaging [9].
Figure 2: SCP-Nano Single-Cell Biodistribution Workflow
FAQs and Troubleshooting Guide
Q1: My nanocarriers are aggregating in biological media, leading to high toxicity in cell culture. What should I do?
- Problem: Aggregation changes the effective size and surface properties, leading to physical cell damage and erroneous toxicity readings.
- Solution:
- Check Zeta Potential: Ensure your nanocarriers have a strong surface charge (> ±30 mV) for electrostatic stabilization.
- Modify Surface Chemistry: Introduce steric stabilizers like polyethylene glycol (PEG) or other polymers (e.g., polysorbates) to create a protective layer that prevents aggregation.
- Use Different Dispersion Media: Try dispersing the nanocarriers in a different buffer or adding low concentrations of serum albumin to the media to pre-form a protein corona that improves stability.
Q2: In vivo, my nanocarriers are being cleared too quickly by the liver and spleen, reducing therapeutic efficacy. How can I improve their circulation time?
- Problem: Rapid clearance by the Mononuclear Phagocyte System (MPS) is a common hurdle.
- Solution:
- PEGylation: Covalently attach PEG chains to the surface. This creates a "stealth" effect, reducing opsonization and recognition by phagocytic cells [71].
- Optimize Size and Charge: Aim for a small size (< 100 nm) and a neutral or slightly negative surface charge, as highly positive particles are more readily opsonized.
- Biomimetic Coatings: Explore coating with cell membranes (e.g., from red blood cells) to create a "self" camouflage.
Q3: I am concerned about the potential for nanocarriers to cause neurotoxicity or cross the blood-brain barrier (BBB) unintentionally. How can I assess this risk?
- Problem: Some nanocarriers can cross the BBB, potentially causing neurotoxic effects through oxidative stress, DNA damage, and neuroinflammation [75].
- Solution:
- Use Specialized In Vitro Models: Employ validated in vitro models of the BBB, such as transwell co-cultures of brain endothelial cells, astrocytes, and pericytes.
- Conduct Targeted In Vivo Studies: After systemic administration, carefully dissect and analyze brain tissue using techniques like the SCP-Nano pipeline, TEM, or inductively coupled plasma mass spectrometry (ICP-MS) for inorganic carriers to detect and quantify nanocarrier accumulation [9] [75].
- Behavioral and Histopathological Analysis: Include behavioral tests and detailed histopathological examination of brain sections in your in vivo studies to look for signs of neuroinflammation or neuronal damage.
Q4: My in vitro cytotoxicity assays (e.g., MTT) show the nanocarrier is safe, but in vivo I see significant immunotoxicity. Why is there a discrepancy?
- Problem: Simple 2D cell cultures cannot recapitulate the complexity of the immune system and organ-level interactions.
- Solution:
- Adopt More Complex Models: Move beyond basic cell lines. Use primary immune cells, 3D organoids, or ex vivo human PBMC assays to better predict immune responses [72].
- Implement a Tiered Testing Pipeline: Follow a hierarchical approach like the 'Safety-by-Design' pipeline, which integrates in silico predictions with ex vivo human immune cell assays before moving to in vivo models. This helps catch immunotoxicity risks earlier [72].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Nanocarrier Toxicity and Biodistribution Studies
| Item/Category | Specific Examples | Function/Application |
|---|---|---|
| Characterization Instruments | DLS/Zeta Potential Analyzer, AFM, TEM/SEM | Determining core physicochemical properties (size, charge, morphology) [5]. |
| Fluorescent Labels | Alexa Fluor dyes (647, 750), Atto dyes | Tagging nanocarriers or their cargo (e.g., mRNA) for sensitive detection in biodistribution and cellular uptake studies [9]. |
| Tissue Clearing Reagents | DISCO kit reagents (optimized without urea/azide) | Rendering whole organs or bodies transparent for 3D light sheet microscopy and single-cell resolution imaging [9]. |
| Cell Culture Models for Toxicity | Primary Human PBMCs, Phagocytic & Non-Phagocytic Cell Lines (e.g., THP-1, HepG2) | Assessing cell-type-specific toxicity, immunotoxicity, and cellular uptake [72] [74]. |
| In Vivo Models | Mice (e.g., C57BL/6, Balb/c) | Evaluating systemic toxicity, biodistribution, immunotoxicity, and organ-level effects in a whole organism [72] [9]. |
| AI/Image Analysis Software | Custom 3D U-Net models, cc3d library | Quantifying millions of targeted cell instances from large-scale 3D imaging data [9]. |
| Cytotoxicity & Viability Assays | Flow Cytometry (with Annexin V/PI), LDH Assay, Metabolic Assays (Alamar Blue) | Quantifying cell death, apoptosis, and metabolic impairment. |
| Immunotoxicity Assays | Multiplex Cytokine Arrays (e.g., for IL-6, IL-1β, TNF-α) | Profiling the inflammatory "immune fingerprint" of nanocarriers [72]. |
Technical Support & Troubleshooting Hub
This section addresses frequently encountered experimental challenges in nanocarrier research at the single-cell level, providing targeted troubleshooting guidance.
FAQ 1: How can I improve the detection sensitivity for nanocarriers at clinically relevant low doses?
- Problem: Conventional imaging techniques like bioluminescence lack the sensitivity to detect nanocarriers at low doses typical for vaccines or therapies, leading to incomplete biodistribution data.
- Solution: Implement advanced tissue-clearing and light-sheet microscopy. An optimized DISCO clearing method, which removes urea and reduces dichloromethane incubation time, can preserve fluorescent signals from tagged nanocarriers. This approach allows for single-cell resolution imaging of nanocarrier distribution throughout the entire mouse body at doses as low as 0.0005 mg kg−1, which is 100–1,000 times lower than the detection limit of conventional whole-body imaging [9].
- Troubleshooting Steps:
- Perfusion and Fixation: Ensure proper perfusion of the animal model to remove blood and preserve tissue integrity.
- Tissue Clearing: Use the optimized DISCO protocol. Avoid standard clearing agents that quench fluorescence.
- Validation: Correlate findings with histological slices from the same tissue sample before and after clearing to confirm signal preservation.
FAQ 2: What is the best method to quantitatively analyze cell-level nanocarrier targeting across entire organs?
- Problem: Manually counting nanocarrier-targeted cells from large 3D imaging datasets is time-consuming and prone to bias.
- Solution: Employ a deep learning-based analysis pipeline. Standard software often delivers suboptimal results (F1 scores < 0.50). A robust solution involves using a 3D U-Net architecture, which can achieve an average instance F1 score of 0.73 for segmenting targeted cells across diverse tissues [9].
- Troubleshooting Steps:
- Data Preparation: Partition whole-body imaging data into manageable 3D patches.
- Model Training: Train the model using a high-quality, VR-annotated dataset from various organs.
- Quantification: Use libraries like
cc3dto identify individual segmented cells and calculate organ-level statistics, such as nanocarrier density and intensity.
FAQ 3: How can I overcome the low transport efficiency of large human cells in single-cell ICP-MS analysis?
- Problem: Transport Efficiency (TE) for large human cells (e.g., A549 lung carcinoma cells, ~20 µm) can be as low as 0.2–5% in standard SC-ICP-MS systems, causing extended analysis times and unreliable data [76].
- Solution: Implement a heated spray chamber. Operating the spray chamber at an elevated temperature of 150°C can increase the TE for A549 cells by 81-fold. This technique reduces cell loss in the introduction system and enhances signal stability [76].
- Troubleshooting Steps:
- System Setup: Couple the heated introduction system to an ICP-TOF-MS for quasi-simultaneous monitoring of multiple elements.
- Cell Preparation: Use chemical fixation to enhance cell robustness, but note that heating is the primary factor for TE improvement.
- Validation: Monitor endogenous elements (e.g., P, Zn) and a DNA intercalator (e.g., Ir) to differentiate between cell events and free nanoparticles reliably.
FAQ 4: What are the key regulatory considerations for preclinical biodistribution studies of a novel RNA nanocarrier?
- Problem: The regulatory path for novel RNA therapeutics and their delivery systems can be unclear, potentially delaying clinical translation.
- Solution: Engage with regulatory bodies early and design comprehensive studies. For a new lipid nanoparticle (LNP), biodistribution data may be required for the RNA molecule, the individual lipid components, and the final formulated product [77].
- Troubleshooting Guidelines:
- Study Scope: Biodistribution studies should characterize the presence, persistence, and clearance in both target and non-target tissues.
- Animal Model: Use a relevant species and include both sexes (e.g., at least 5 rodents per sex per time point, as advised by FDA and ICH) [77].
- Product Consistency: The administered formulation must reflect the intended clinical product in quality, dose, and route of administration.
The tables below consolidate key quantitative data from recent studies to inform the design of your experiments.
Table 1: Comparison of Single-Cell Analysis Techniques for Nanocarrier-Cell Interactions
| Technique | Key Metric | Performance / Value | Key Advantage | Reference |
|---|---|---|---|---|
| SCP-Nano (AI + Light Sheet) | Instance F1 Score | 0.73 (avg., range 0.69-0.80 across organs) | High-accuracy, single-cell quantification across whole bodies | [9] |
| SC-ICP-TOF-MS | Transport Efficiency (A549 cells) | ~0.2-5% (standard); up to 81-fold increase with heating | High-throughput, quantitative metal detection per cell | [76] |
| Flow Cytometry | Parameters | Multiplexed surface and intracellular markers | High-throughput phenotypic analysis | [11] [78] |
| Mass Cytometry (CyTOF) | Parameters | >40 simultaneous markers | Extreme multiplexing for deep immunophenotyping | [78] |
Table 2: Key Physicochemical Properties of Nanocarriers and Their Biological Impact
| Property | Measurement Technique | Biological Influence | Reference |
|---|---|---|---|
| Particle Size & PDI | Dynamic Light Scattering (DLS), AF4, CLS | Biodistribution, cellular uptake, clearance, circulation half-life | [5] |
| Surface Charge (Zeta Potential) | Electrophoretic Light Scattering | Colloidal stability, aggregation, interaction with cell membranes | [5] |
| Morphology | SEM, TEM, Atomic Force Microscopy (AFM) | Targeting efficiency, toxicity, cellular internalization mechanisms | [5] |
| Hydrophobicity | X-ray Photon Correlation Spectroscopy, Contact Angle | Protein corona formation, bioavailability, stability | [5] |
Detailed Experimental Protocols
Protocol 1: Whole-Body Single-Cell Nanocarrier Mapping via SCP-Nano
This protocol enables comprehensive 3D mapping of nanocarrier distribution at single-cell resolution [9].
- Nanocarrier Administration: Inject fluorescence-labeled nanocarriers (e.g., LNPs, liposomes, AAVs) into animal models (e.g., mouse) via the route of interest (e.g., intravenous, intramuscular).
- Tissue Clearing (Optimized DISCO Method):
- Perfuse and fix the animal with 4% paraformaldehyde (PFA).
- Critical Step: Eliminate urea and sodium azide from the clearing reagents. Reduce dichloromethane (DCM) incubation time to preserve fluorescence.
- Dehydrate and clear the entire mouse body using the refined DISCO reagents.
- Light-Sheet Microscopy:
- Image the cleared whole mouse body at a resolution of approximately 1–2 µm (lateral) and 6 µm (axial).
- AI-Based Data Analysis:
- Data Partitioning: Split the whole-body imaging data into discrete 3D patches (e.g., 200x200x200 voxels).
- Model Application: Process patches with a pre-trained 3D U-Net deep learning model for targeted cell segmentation.
- Quantification: Use the
cc3dlibrary to identify individual cell instances and calculate organ-level statistics (size, intensity, density).
Protocol 2: High-Throughput Quantification of Nanoparticle Uptake via SC-ICP-TOF-MS
This protocol quantifies the number of metal-containing nanocarriers associated with individual cells [76].
- Cell Preparation and Labelling:
- Harvest and wash cells (e.g., A549) after exposure to metal-nanocarriers (e.g., AuNPs).
- Fix cells with PFA to enhance robustness.
- Optional: Stain cells with a metal-tagged DNA intercalator (e.g., Ir) or surface marker (e.g., Ru) to improve cell event detection.
- Sample Introduction System Optimization:
- Critical Step: Heat the spray chamber to 150°C to dramatically improve transport efficiency for large cells.
- Use a total sample consumption introduction system.
- Dilute the cell suspension to a concentration of 10^5 - 10^6 cells/mL.
- ICP-TOF-MS Data Acquisition:
- Operate the ICP-TOF-MS in time-resolved analysis mode.
- Quasi-simultaneously monitor signals for:
- Nanocarrier Element: e.g., Au
- Cellular Elements: e.g., P, S, Zn
- DNA Tag: e.g., Ir
- Data Analysis:
- Identify transient signals corresponding to single-cell events.
- Differentiate between cells with nanoparticles, cells without nanoparticles, and free nanoparticles based on the co-detection of elemental tags.
- Quantify the number of nanoparticles per cell based on the intensity of the nanocarrier element signal.
Workflow and Pathway Visualizations
SCP-Nano Whole-Body Analysis Workflow
The following diagram illustrates the integrated experimental and computational pipeline for single-cell precision nanocarrier identification.
Regulatory Pathway for Novel Nanocarriers
This diagram outlines the key stages and considerations for translating a novel nanocarrier from preclinical development to regulatory approval.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Single-Cell Nanocarrier Research
| Item | Function / Application | Key Consideration |
|---|---|---|
| DNA Nanoball (DNB) Arrays (Stereo-cell) | Spatial barcoding for multimodal single-cell analysis (transcriptomics, proteomics, morphology). | Enables near-subcellular resolution and detection of rare cell populations (~0.05%) [79]. |
| Lipid Nanoparticles (LNPs) | Delivery vehicle for RNA therapeutics (mRNA, siRNA) and vaccines. | Composition (ionizable lipid, PEG-lipid) dictates tropism and protein corona formation [77] [9]. |
| Metal-Tagged Antibodies & DNA Intercalators | Cell phenotyping and identification in mass cytometry and SC-ICP-MS. | Allows for multiplexed analysis (>40 parameters). Iridium (Ir) intercalator labels DNA for cell event detection [11] [76]. |
| Tissue Clearing Reagents (DISCO) | Renders whole organs or bodies transparent for 3D microscopy. | Formula must be optimized to preserve fluorescence of tagged nanocarriers and mRNAs [9]. |
| Polyethylene Glycol (PEG) | Surface coating to improve nanocarrier stability, biocompatibility, and circulation time. | Can reduce interactions with endothelial cells and minimize rapid clearance [5] [80]. |
Conclusion
Achieving optimized nanocarrier distribution at the single-cell level is no longer an aspirational goal but an attainable reality, thanks to integrated technological pipelines like SCP-Nano. This approach, combining advanced tissue clearing, high-resolution microscopy, and robust deep learning, provides an unprecedented view of nanocarrier biodistribution, revealing both intended targeting and critical off-target effects. The key takeaways are that design parameters must be meticulously controlled, administration routes strategically selected, and AI-driven analysis embraced to move beyond organ-level to true single-cell precision. Future directions will involve refining these AI models for predictive design, developing next-generation smart nanocarriers with enhanced targeting specificity, and translating these precise delivery systems into clinical therapies for cancer, genetic disorders, and beyond, ultimately ushering in a new era of personalized nanomedicine.
References
- 1. Understanding the synergistic effect of physicochemical properties of nanoparticles and their cellular entry pathways - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7192949/]
- 2. Understanding the synergistic effect of physicochemical ... [https://www.nature.com/articles/s42003-020-0917-1]
- 3. Nanocarriers’ entry into the cell: relevance to drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11115599/]
- 4. Effect of physicochemical and surface properties on in vivo ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X1930002X]
- 5. Nanocarrier Drug Delivery Systems: Characterization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9026217/]
- 6. Physicochemical characterization of drug nanocarriers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5516877/]
- 7. Optimization and characterization of nanomaterials for drug ... [https://www.malvernpanalytical.com/en/learn/knowledge-center/insights/qa-optimization-and-characterization-of-nanomaterials-for-drug-delivery]
- 8. Lipid nanoparticle (LNP) manufacturing: Challenges & ... [https://www.susupport.com/blogs/knowledge/lipid-nanoparticle-lnp-manufacturing-challenges-solutions]
- 9. Nanocarrier imaging at single-cell resolution across entire ... [https://www.nature.com/articles/s41587-024-02528-1]
- 10. Injectable nanomaterials for drug delivery: Carriers, ... [https://www.sciencedirect.com/science/article/abs/pii/S0939641112004262]
- 11. High-Throughput Single-Cell Analysis of Nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10373476/]
- 12. Transpathology: molecular imaging-based pathology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8241651/]
- 13. New Technology to Visualize Nanocarriers in Cells and ... [https://www.helmholtz-munich.de/en/ehc/ehc-news/news-detail/scp-nano-a-new-technology-to-visualize-nanocarriers-in-cells-and-tissues]
- 14. WildDISCO: Visualizing Whole Bodies in Unprecedented ... [https://www.helmholtz-munich.de/en/newsroom/news-all/artikel/wilddisco-visualizing-whole-bodies-in-unprecedented-detail]
- 15. High-precision cell-type mapping and annotation of single-cell ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03773-6]
- 16. High-resolution mapping of single cells in spatial context [https://www.nature.com/articles/s41467-025-61667-4]
- 17. Overcoming barriers to single-cell RNA sequencing adoption ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11499908/]
- 18. Nanocarrier imaging at single-cell resolution across entire ... [https://pubmed.ncbi.nlm.nih.gov/39809933/]
- 19. PXD056871 - ProteomeCentral Datasets - ProteomeXchange [https://proteomecentral.proteomexchange.org/dataset/PXD056871]
- 20. A beginner's guide to tissue clearing - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5336404/]
- 21. Light-Sheet Microscopy FAQ [https://www.bruker.com/en/products-and-solutions/fluorescence-microscopy/light-sheet-microscopes/faq.html]
- 22. Facing an issue while training UNet for Image Segmentation [https://stackoverflow.com/questions/78344194/facing-an-issue-while-training-unet-for-image-segmentation]
- 23. Universal consensus 3D segmentation of cells from 2D ... [https://www.nature.com/articles/s41592-025-02887-w]
- 24. CellSNAP: a fast, accurate algorithm for 3D cell segmentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11025678/]
- 25. Revisiting model scaling with a U-net benchmark for 3D ... [https://www.nature.com/articles/s41598-025-15617-1]
- 26. Medical Image Segmentation Using Automatic Optimized U ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10533074/]
- 27. Can't fit data to 3d convolutional U-net Keras [https://stackoverflow.com/questions/44921058/cant-fit-data-to-3d-convolutional-u-net-keras]
- 28. A complete guide to understanding Lipid nanoparticles (LNP) [https://insidetx.com/resources/reviews/complete-guide-to-understanding-lipid-nanoparticles-lnp/]
- 29. Naturally-occurring cholesterol analogues in lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7033178/]
- 30. Gene-encoding DNA origami for mammalian cell expression [https://www.nature.com/articles/s41467-023-36601-1]
- 31. Lipid Nanoparticle LNP overview and resources [https://www.precigenome.com/lipid-nanoparticles-lnp?srsltid=AfmBOooP4_AenLaDy2CK7g0fmGhpjGqCLUP1UrMM5gP8AATm23yBoU-W]
- 32. Emerging Research on Gene Delivery to the Nucleus via DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458035/]
- 33. Construction of a smart dual-responsive targeted drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0045206825001646]
- 34. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 35. Microfluidic Device Type Improves Heart mRNA Delivery In Vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529952/]
- 36. Harnessing mRNA for heart health - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12316028/]
- 37. Protocol for the development of mRNA lipid nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11144802/]
- 38. Challenges in Measuring In Vitro Activity of LNP-mRNA ... [https://www.mdpi.com/1422-0067/26/17/8152]
- 39. Optimization of Lipid-Nanoparticle Delivery Systems [https://www.bioprocessintl.com/vaccines/bottlenecks-in-rna-delivery-optimization-of-lipid-nanoparticle-delivery-systems]
- 40. Lipid nanoparticles for mRNA delivery [https://www.nature.com/articles/s41578-021-00358-0]
- 41. Optimization of Lipid Nanoformulations for Effective mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9259059/]
- 42. A guide to RNA-LNP formulation screening [https://insidetx.com/resources/reviews/a-guide-to-rna-lnp-formulation-screening/]
- 43. Nanocarrier‐Based Systems for Targeted Delivery: Current Challenges and Future Directions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371215/]
- 44. Nanomedicine in cancer therapy | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-023-01536-y]
- 45. Nanocarriers Offer Hope for Improving Parkinson's Treatment [https://www.apdaparkinson.org/article/nanocarrier-breakthrough-offers-hope-for-pd-treatment/]
- 46. Activating PEG host to enable spatially controlled surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629181/]
- 47. Beyond PEGylation: nanoparticle surface modulation for ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00014-4]
- 48. Brain-targeted intranasal delivery of biologics - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00148j]
- 49. A Rationally Designed Polypeptide-based Hybrid Platform ... [https://www.sciencedirect.com/science/article/pii/S0142961225007872]
- 50. Combining Intramuscular and Intranasal Immunization With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264085/]
- 51. All About Different Vaccine Delivery Methods [https://www.sabin.org/resources/all-about-different-vaccine-delivery-methods/]
- 52. Pharmacokinetics and pharmacodynamics of AQST-109 [https://pubmed.ncbi.nlm.nih.gov/41297629/]
- 53. Nanotechnology-driven advances in intranasal vaccine ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1573037/full]
- 54. Advances in Nanotechnology-Based Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389492/]
- 55. Artificial Intelligence‐Driven Nanoarchitectonics for Smart ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548523/]
- 56. Critical questions in development of targeted nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4817320/]
- 57. Q&A Translational Cancer Nanomedicine [https://www.nature.com/articles/s41467-025-63488-x]
- 58. Impact of protein coronas on nanoparticle interactions with ... [https://pubmed.ncbi.nlm.nih.gov/38103519/]
- 59. In vivo Protein Corona Formation: Characterizations ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.646708/full]
- 60. Preparation of the protein corona: How washing shapes ... [https://www.sciencedirect.com/science/article/abs/pii/S174270612030427X]
- 61. Engineered protein corona sustains stealth functionality of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261846/]
- 62. Regulating protein corona on nanovesicles by glycosylated ... [https://www.nature.com/articles/s41467-024-45254-7]
- 63. Introducing SCP - Nano : Groundbreaking Technology for Imaging ... [https://scienmag.com/introducing-scp-nano-groundbreaking-technology-for-imaging-nanocarriers-within-cells-and-tissues/]
- 64. Quantitative validation of Monte Carlo SPECT simulation: application to... [https://ejnmmiphys.springeropen.com/articles/10.1186/s40658-023-00581-4]
- 65. A comparative biodistribution study of polymeric and lipid- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9012159/]
- 66. Blood proteomics for quantitative biomarkers of cellular ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00837-4]
- 67. LC-MS-based proteomics: insights into natural product- ... [https://www.sciencedirect.com/science/article/pii/S1359644625002478]
- 68. A proteomic platform to identify off-target proteins ... [https://www.nature.com/articles/s41598-021-95354-3]
- 69. Proteomics reveals that cell density could affect the efficacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9763681/]
- 70. Strategies for improving drug delivery: Nanocarriers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5584706/]
- 71. Toxicology of Nanoparticles in Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8611175/]
- 72. Multiscale Profiling of Nanoscale Metal‐Organic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616609/]
- 73. Recent advances in the development of biocompatible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9420852/]
- 74. Nanomaterials in Medical Devices [https://namsa.com/resources/blog/nanomaterials-medical-devices-biocompatibility-considerations/]
- 75. Navigating Neurotoxicity and Safety Assessment of ... [https://www.sciencedirect.com/science/article/pii/S1742706124005439]
- 76. Improving transport efficiency for large human cells ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025011877]
- 77. Regulatory guidelines and preclinical tools to study the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8957368/]
- 78. Using single cell analysis for translational studies in ... [https://www.sciencedirect.com/science/article/abs/pii/S0161589018308228]
- 79. Advancing spatial single‐cell biology towards clinical translation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455014/]
- 80. for targeted drug delivery in the vascular system: focus... Nanocarriers [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02892-9]