Navigating FDA Regulatory Pathways for Nanotechnology Products: A 2025 Guide for Researchers
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the U.S.
Navigating FDA Regulatory Pathways for Nanotechnology Products: A 2025 Guide for Researchers
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the U.S. Food and Drug Administration's (FDA) regulatory framework for nanotechnology products. It covers the foundational principles of the FDA's science-based, product-specific approach, details the methodological considerations for product development and submission, offers strategies for troubleshooting common regulatory challenges, and explains validation through expedited programs and real-world case studies. The content is designed to help innovators efficiently navigate the regulatory process, from early development to market approval, for a wide range of nanotech applications in drugs, biologics, and other regulated products.
Understanding the FDA's Regulatory Framework for Nanotechnology
The FDA's Product-Focused and Science-Based Policy Philosophy
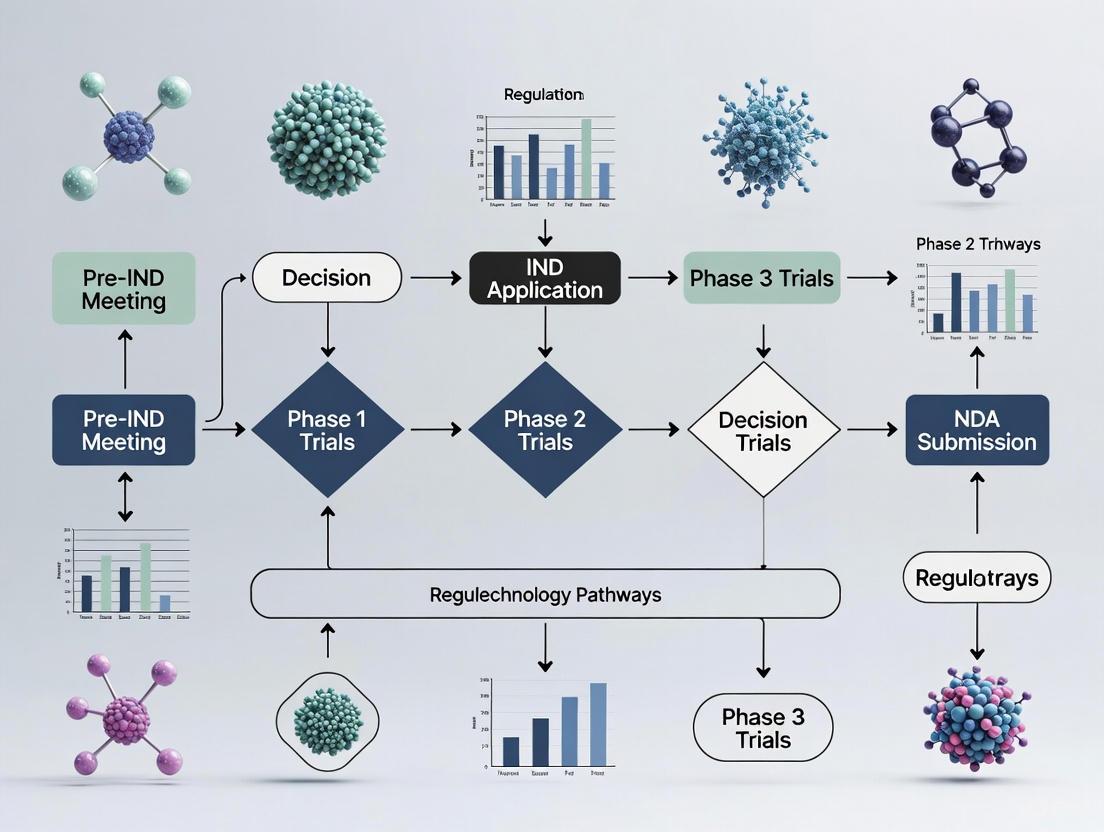
A technical guide for navigating regulatory science for nanotechnology products
The U.S. Food and Drug Administration (FDA) regulates a wide range of products that may utilize nanotechnology or contain nanomaterials, from drugs and devices to foods and cosmetics. The agency's approach is product-focused and science-based, meaning technical assessments consider the effects of nanomaterials in the specific biological and mechanical context of each product and its intended use [1]. This resource provides targeted guidance for researchers and developers working within this regulatory framework.
Frequently Asked Questions: Navigating FDA Nanotechnology Regulation
Q1: How does the FDA define nanotechnology for regulatory purposes? The FDA does not rely on a single, rigid definition. Instead, it focuses on whether a material or product is engineered to have at least one external dimension, or an internal or surface structure, in the nanoscale range (approximately 1–100 nm). More importantly, the agency considers whether the engineered material exhibits properties or phenomena attributable to its dimension(s), including physical or chemical properties or biological effects that differ from those of larger-scale counterparts [2]. The evaluation is based on the product's specific characteristics and intended use.
Q2: Does the FDA have a unique regulatory pathway for nanotechnology products? No. The FDA regulates nanotechnology products under its existing statutory authorities and in accordance with the specific legal standards applicable to each type of product (e.g., drug, device, cosmetic) [1] [2]. The regulatory pathway is determined by the product's classification and its intended use, not solely by the presence of nanotechnology.
Q3: What is the most critical step for developers of an NHP (Nanotechnology-Enabled Health Product) during early development? The FDA strongly encourages early consultation with the agency. Engaging with the FDA early in the product development process facilitates a mutual understanding of the specific scientific and regulatory issues. This allows developers to clarify the methodologies and data needed to meet safety, effectiveness, and other regulatory obligations [1] [2].
Q4: What are the key regulatory science questions the FDA is trying to answer for NHPs? The FDA's nanotechnology regulatory science research focuses on two primary areas [2]:
- Understanding the interactions of nanomaterials with biological systems.
- Assessing the adequacy of testing approaches for evaluating the safety, effectiveness, and quality of products containing nanomaterials.
Q5: How does the FDA's "product-focused" approach impact my regulatory strategy? This approach means that data requirements are not one-size-fits-all. Your regulatory strategy and the data you generate must be tailored to your specific product. A drug delivery nanoparticle will be held to different standards than a nanocoat ed surgical implant, even if they incorporate the same nanomaterial, because the biological context, route of administration, and intended use differ [1].
Regulatory Science Research Priorities
The FDA invests in a robust regulatory science program to enhance its capabilities for assessing nanotechnology products. The table below summarizes key research priority areas that inform the agency's evaluations.
| Research Priority Area | Key Questions for Investigators | Relevant Product Categories |
|---|---|---|
| Physicochemical Characterization | What parameters must be defined to establish a nanomaterial's identity? How do properties change in biological environments? | Drugs, Biologics, Devices, Food Additives |
| Toxicology & Biocompatibility | How do nanomaterials interact with cells and organ systems? What are the appropriate toxicological endpoints? | Drugs, Devices, Cosmetics |
| Safety & Effectiveness Evaluation | Are standard testing models adequate? What new methods are needed to demonstrate clinical benefit? | Drugs, Devices, Biologics |
| Quality & Manufacturing Control | How can manufacturing consistency be ensured? What controls are critical for batch-to-batch reproducibility? | Drugs, Biologics, Devices |
Experimental Protocol: Critical Physicochemical Characterization of Nanomaterials
A foundational step in developing an NHP is a comprehensive characterization of the nanomaterial's physicochemical properties. This data is essential for understanding its behavior, stability, and biological interactions and is a core requirement in regulatory submissions.
Objective
To systematically identify and quantify the key physicochemical parameters of a nanomaterial to establish its critical quality attributes (CQAs) for regulatory evaluation.
Materials and Reagents
| Research Reagent / Material | Function in Characterization |
|---|---|
| Dynamic Light Scattering (DLS) Instrument | Measures hydrodynamic diameter (size) and particle size distribution (polydispersity index) in a liquid suspension. |
| Zeta Potential Analyzer | Determines the surface charge, which predicts colloidal stability and interaction with biological membranes. |
| Electron Microscopy (SEM/TEM) | Provides high-resolution imaging for direct visualization of particle size, morphology, and structure. |
| Surface Area and Porosity Analyzer (BET) | Quantifies specific surface area, a key parameter influencing reactivity, dissolution, and drug loading capacity. |
| X-ray Photoelectron Spectroscopy (XPS) | Analyzes elemental composition and chemical state of the material's surface. |
| High-Performance Liquid Chromatography (HPLC) | Used to quantify drug loading and encapsulation efficiency for nanocarrier systems. |
| Stable Biological Media (e.g., PBS, cell culture media) | Used to assess particle stability and agglomeration behavior in physiologically relevant conditions. |
Step-by-Step Methodology
- Sample Preparation: Prepare a standardized suspension of the nanomaterial in a relevant solvent (e.g., water, buffer) at a defined concentration. Use sonication or other methods to ensure a monodisperse suspension before analysis.
- Size and Distribution Analysis:
- Utilize Dynamic Light Scattering (DLS) to measure the hydrodynamic diameter and polydispersity index (PDI). A PDI value below 0.2 is generally considered monodisperse.
- Validate DLS data with a direct imaging technique like Transmission Electron Microscopy (TEM) to confirm size and assess morphology (e.g., spherical, rod-shaped).
- Surface Charge Measurement: Use a Zeta Potential Analyzer to determine the surface charge. Measurements should be performed in different media (e.g., water, PBS) to predict stability and behavior in biological fluids.
- Surface and Structural Analysis:
- Perform Brunauer-Emmett-Teller (BET) analysis to determine the specific surface area.
- Use X-ray Photoelectron Spectroscopy (XPS) to identify the elemental and chemical composition of the particle surface.
- Drug Loading Assessment (for nanocarriers): For drug-loaded nanoparticles, use a validated HPLC method to separate free drug from the nanocarrier, allowing for calculation of drug loading capacity and encapsulation efficiency.
- Stability in Biological Media: Incubate the nanomaterial in biologically relevant media (e.g., PBS with serum proteins) and monitor changes in size and zeta potential over time (e.g., 0, 1, 4, 24 hours) using DLS to assess agglomeration or degradation.
The workflow for this characterization process is outlined below.
Data Interpretation and Regulatory Significance
Regulatory assessments rely on a clear demonstration of product quality and consistency. A well-characterized nanomaterial, with CQAs that are tightly controlled, is critical for establishing a valid safety profile. This data forms the foundation for all subsequent non-clinical and clinical studies.
The Scientist's Toolkit: Essential Characterization Parameters
For any NHP, regulators will expect a comprehensive dataset detailing the following parameters. This list serves as a checklist for your development work.
| Parameter | Description | Example Technique(s) | Regulatory Significance |
|---|---|---|---|
| Size & Distribution | Hydrodynamic diameter & polydispersity. | DLS, TEM, SEM | Affects biodistribution, clearance, and toxicity [3]. |
| Surface Charge | Zeta potential in relevant media. | Zeta Potential Analyzer | Predicts colloidal stability & interaction with cells [3]. |
| Surface Chemistry | Functional groups & coating composition. | XPS, FTIR | Influences protein corona formation & biological fate [3]. |
| Surface Area | Specific surface area per mass unit. | BET Analysis | Critical for understanding reactivity & dose [3]. |
| Morphology | Particle shape & physical structure. | TEM, SEM | Impacts cellular uptake & biological activity [3]. |
| Drug Release | Release kinetics in physiological conditions. | Dialysis, HPLC | Core to demonstrating controlled release function [3]. |
| Stability | Shelf-life & in-media behavior. | DLS, HPLC | Required to prove product quality & performance during use. |
| Elemental Impurities | Quantification of catalytic residues. | ICP-MS | Required for safety assessment of the manufacturing process. |
| Crystallinity | Physical state of the material (e.g., amorphous, crystalline). | XRPD | Can impact stability, dissolution, and biological performance. |
Troubleshooting Common Nanomaterial Characterization Issues
Problem: Inconsistent Sizing Results Between DLS and TEM
- Cause: DLS measures the hydrodynamic diameter (core + solvation layer) in a liquid state, while TEM provides a dry-state image of the core particle.
- Solution: This discrepancy is expected. Use DLS for stability and behavior in solution, and TEM to confirm core size and morphology. Report both datasets with a clear explanation.
Problem: Rapid Agglomeration in Biological Media
- Cause: Insufficient surface charge or the presence of proteins causing bridging flocculation.
- Solution: Reformulate to increase zeta potential magnitude (e.g., > ±20 mV). Consider modifying the surface with steric stabilizers like polyethylene glycol (PEG).
Problem: Low Drug Loading Capacity in Nanocarrier
- Cause: Poor compatibility between the drug and the carrier matrix, or inefficient encapsulation method.
- Solution: Optimize the drug-to-carrier ratio and the manufacturing process (e.g., solvent displacement, emulsification). Explore different nanocarrier materials.
For further information, the FDA provides a comprehensive search portal for its official guidance documents [4], and encourages direct contact for specific questions via the Office of Policy at 301-796-4830 [1].
Frequently Asked Questions
What is the FDA's regulatory definition of a "nanomaterial"? The FDA has not established a single, rigid regulatory definition for the term "nanomaterial" [5] [6]. Instead, the agency uses a flexible, two-point framework to determine whether an FDA-regulated product involves the application of nanotechnology [6].
If there's no definition, how does the FDA identify nanomaterials? The FDA uses two "Points to Consider" for identification. A product may involve the application of nanotechnology if it meets either of the following criteria [6]:
- It is engineered to have at least one external dimension, or an internal or surface structure, in the nanoscale range (approximately 1 nm to 100 nm).
- It is engineered to exhibit properties or phenomena (e.g., physical, chemical, or biological effects) attributable to its dimension(s), even if these dimensions fall outside the nanoscale range, up to one micrometer (1,000 nm).
Are naturally occurring nanoscale materials (like proteins) considered? The FDA's guidance is primarily intended for engineered nanomaterials. It distinguishes between materials that have been deliberately manipulated to have nanoscale dimensions and those that naturally exist at the nanoscale, such as proteins or other biological materials, which are not explicitly considered nanomaterials per the guidance [5] [6].
What about incidental nanoparticles from manufacturing? The guidance does not pertain to products that contain incidental nanoscale particles generated from conventional manufacturing processes or storage [5] [6]. The focus is on intentionally engineered materials and their properties.
Why is particle size alone not sufficient for identification? Some materials can exhibit dimension-dependent properties or phenomena, such as increased bioavailability or altered chemical reactivity, even at sizes larger than 100 nm. The second "Point to Consider" ensures these materials are also evaluated for potential unique safety and efficacy profiles [6] [7].
Troubleshooting Guide: Common Challenges in Nanomaterial Identification and Characterization
Problem 1: Determining if a material with a size >100 nm falls under FDA nanotechnology considerations.
- Potential Cause: The material exhibits dimension-dependent properties or phenomena, as described in the FDA's second "Point to Consider" [6].
- Solution:
- Investigate Properties: Systematically test whether the material exhibits properties that differ from its larger-scale counterparts. Key properties to investigate include [6]:
- Increased chemical or biological activity
- altered electrical or optical activity
- Increased structural integrity
- Changed magnetic properties
- Link to Dimensions: Confirm that these novel properties are a direct result of the material's engineered dimensions and not just its chemical composition.
- Consult FDA: It is recommended that sponsors consult with the FDA early in the development process if they believe their product may involve the application of nanotechnology [6].
- Investigate Properties: Systematically test whether the material exhibits properties that differ from its larger-scale counterparts. Key properties to investigate include [6]:
Problem 2: A drug product's critical quality attributes (CQAs) change during scale-up.
- Potential Cause: Nanomaterials are often sensitive to process conditions and manufacturing changes, which can affect particle size, size distribution, and other critical attributes [5].
- Solution:
- Early Identification: Identify CQAs early in development. These are physical, chemical, biological, or microbiological properties that should be within an appropriate limit to ensure the desired product quality [5].
- Implement Controls: Develop and implement appropriate in-process controls during manufacturing to ensure consistency.
- Stability Testing: Follow stability testing processes that monitor for nanomaterial-specific changes, such as aggregation, agglomeration, or changes in morphology [5].
Problem 3: Difficulty in characterizing nanomaterial size and properties.
- Potential Cause: Standard analytical techniques, like light microscopy, are often inadequate for resolving materials at the nanoscale due to the diffraction limit of light [5].
- Solution: Employ specialized techniques suited for nanomaterial characterization. The table below summarizes key parameters and common methods as outlined in ISO standards [8].
Table 1: Key Physico-Chemical Characterization Parameters and Methods for Nanomaterials
| Parameter | Description | Relevance / Rationale |
|---|---|---|
| Particle Size & Distribution | The average size and variability of particles in a population. | Affects biodistribution, bioavailability, and biological activity [5] [8]. |
| Aggregation/Agglomeration State | The tendency of particles to clump together. | Influences behavior, dose, and exposure [8]. |
| Shape | The physical form of the particles (e.g., spherical, rod-shaped). | Impacts cellular uptake and toxicity [8]. |
| Surface Area | The total surface area per unit mass. | Increased surface area can enhance reactivity and biological activity [8] [9]. |
| Surface Chemistry | The composition and properties of the material's surface. | Dictates interactions with biological systems (e.g., protein corona formation) [8]. |
| Surface Charge | The electrical charge on the particle's surface. | Affects colloidal stability, aggregation, and interaction with cell membranes [8]. |
| Solubility/Dispersibility | The ability to dissolve or form a stable suspension in a medium. | Critical for understanding fate, persistence, and exposure [8]. |
Problem 4: Designing a biocompatibility testing plan for a medical device containing nanomaterials.
- Potential Cause: Standard biocompatibility tests (ISO 10993 series) may require adaptation for nanomaterials due to their unique kinetic properties and potential for assay interference [8].
- Solution: Follow a two-step process as guided by ISO/TR 10993-22:
- Comprehensive Characterization: Perform a thorough physico-chemical characterization of the nanomaterial using the parameters in Table 1 before any biological testing [8].
- Adapted Biological Testing: Modify standard test protocols to account for nanomaterial behavior. The table below outlines key considerations for common test endpoints.
Table 2: Key Considerations for Biological Testing of Nanomaterial-Containing Medical Devices
| Test Endpoint | Testing Considerations | Justification |
|---|---|---|
| Cytotoxicity | Use several test methods (e.g., with phagocytic and non-phagocytic cell lines). | Nanomaterials are generally taken up by cells; assay interferences are possible; kinetics depend on size and agglomeration [8]. |
| Sensitization | Standard in vivo assays (like GPMT or LLNA) might not be effective. | The skin's barrier function may prevent nano-objects from reaching target immune cells [8]. |
| Hemocompatibility | Must evaluate complement system activation. | Nanomaterials can cause abnormal complement activation, leading to significant inflammatory reactions; high surface area can adsorb serum proteins, distorting results [8]. |
| Systemic Toxicity | Focus on tissues like the liver, spleen, and kidneys. Consider particle number and surface area as dose metrics, not just mass. | Nano-objects can distribute throughout the body, with concern for accumulation and biopersistence in the mononuclear phagocyte system [8]. |
| Genotoxicity | The bacterial reverse mutation test (Ames test) is not appropriate for free nano-objects; use mammalian cell systems instead. | Uncertainty about whether bacteria can uptake nano-objects and thus expose DNA [8]. |
Table 3: Key Research Reagent Solutions and Regulatory Tools
| Item / Resource | Function / Purpose |
|---|---|
| FDA Guidance "Drug Products... Nanomaterials" | Provides specific considerations for the development, manufacturing, and evaluation of human drug products containing nanomaterials [5] [10]. |
| ISO/TR 10993-22 Guidance | Offers detailed protocols for the biological evaluation of medical devices composed of or containing nanomaterials [8]. |
| HEPA-Filtered Local Exhaust Ventilation | An engineering control (e.g., fume hoods, glove boxes) to reduce potential inhalation exposure to aerosolized nanoparticles in the laboratory [9]. |
| Dynamic Light Scattering (DLS) | A common technique used to determine the hydrodynamic size and size distribution of nanoparticles in suspension. |
| Reference Nanomaterials | Standardized materials used to calibrate equipment and validate test methods, though their availability is still a developing area [7]. |
| OECD Test Guidelines for Nanomaterials | Provide internationally agreed-upon methods for testing the safety of nanomaterials, supporting the Mutual Acceptance of Data [7]. |
Experimental Workflow: Applying the FDA's Points to Consider
The following diagram illustrates the logical decision process for identifying if a material falls under the FDA's nanotechnology considerations, integrating characterization and testing steps.
Technical Support Center: Navigating FDA Nanotechnology Regulations
Troubleshooting Guide: Common Regulatory Challenges
Issue 1: Determining When a Product Involves Nanotechnology
- Problem: Researchers are uncertain whether their product meets FDA's criteria for nanotechnology oversight.
- Solution: Apply FDA's two "Points to Consider" [6]:
- Engineered materials with at least one external dimension, internal structure, or surface structure between 1-100 nm
- Materials engineered to exhibit properties or phenomena attributable to their dimension(s), even outside the 1-100 nm range (up to 1000 nm)
- Required Documentation: Comprehensive characterization data including size distribution, surface charge, and stability profiling.
Issue 2: Selecting the Correct Premarket Pathway
- Problem: Confusion about whether a nanotech product requires premarket approval or can use existing regulatory pathways.
- Solution Matrix:
| Product Type | Premarket Review Required? | Key Regulatory Standard | Data Requirements |
|---|---|---|---|
| New Drugs | Yes (NDA) [1] | Safety + Effectiveness [1] | Clinical data, nano-specific toxicology |
| Medical Devices | Varies by class [11] | Risk-based classification [11] | Performance testing, biocompatibility |
| Food Additives | Yes [1] | Reasonable certainty of no harm [1] | Toxicity studies, consumption patterns |
| Cosmetics | No (voluntary consultation) [1] | Safety assurance [1] | Limited safety data, ingredient listing |
| Dietary Supplements | No (except new ingredients) [1] | Safety assurance [1] | History of use, composition data |
Issue 3: Demonstrating Substantial Equivalence for Nanotech Devices
- Problem: Difficulty finding appropriate predicates for 510(k) submissions due to novel nanoscale properties.
- Solution Options:
Experimental Protocols for Regulatory Submissions
Protocol 1: Comprehensive Nanomaterial Characterization
- Objective: Fully characterize physicochemical properties to determine regulatory status
- Methodology:
- Size Distribution: Dynamic light scattering, electron microscopy
- Surface Properties: Zeta potential, surface area analysis
- Stability: Accelerated stability studies under intended storage conditions
- Batch-to-Batch Variability: Minimum of 3 manufacturing lots
- Regulatory Reference: FDA's 2014 nanotechnology guidance [6]
Protocol 2: Nano-Specific Toxicology Assessment
- Objective: Identify unique biological effects of nanoscale materials
- Methodology:
- Biodistribution Studies: Radiolabeling and tissue distribution analysis
- Immune Response Evaluation: Complement activation, cytokine profiling
- Cellular Uptake Assessment: Confocal microscopy, flow cytometry
- Traditional Toxicology: Acute and chronic toxicity per ICH guidelines
- Application: Required for all injectable and systemic delivery nanotechnologies
Table 1: Market Data and Regulatory Maturity by Sector (2024)
| Sector | Global Revenue (USD Billion) | Maturity Level | FDA Regulatory Clarity | Key Challenges |
|---|---|---|---|---|
| Nanomedicine | $12.4 [13] | High [13] | Established pathways for drug delivery [14] | Generic equivalence, long-term safety [14] |
| Semiconductor Manufacturing | $22.1 [13] | High [13] | Device classification framework [11] | Rapid technological evolution |
| Food Ingredients | Not specified | Low [15] | Voluntary GRAS notification [15] | Lack of mandatory oversight [15] |
| Cosmetics | Not specified | Low [1] | Post-market surveillance [1] | No premarket approval required |
Table 2: Medical Device Classification and Pathways
| Device Class | Risk Level | Regulatory Pathway | Typical Timeline | Nano-Specific Considerations |
|---|---|---|---|---|
| Class I | Minimal [11] | General controls, mostly exempt [11] | 1-3 months [11] | May require additional characterization |
| Class II | Moderate [11] | 510(k) substantial equivalence [11] | 6-12 months [11] | Enhanced performance data, special controls |
| Class III | High [11] | Premarket Approval (PMA) [11] | 2-5 years [11] | Clinical data, complete nano-toxicology profile |
| De Novo | Low-Moderate, novel [12] | Risk-based classification [12] | 120-150 days [11] | First-of-its-kind nanotechnology evaluation |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Nanotechnology Characterization
| Reagent/Material | Function | Regulatory Application |
|---|---|---|
| Dynamic Light Scattering Standards | Size distribution calibration | Required for all nanomaterial characterization [6] |
| Zeta Potential Reference Materials | Surface charge validation | Critical for stability assessment and immune response prediction |
| Complement Activation Assay Kits | Immunotoxicity screening | Essential for injectable nanomedicines [14] |
| Tissue Distribution Tracers | Biodistribution studies | Required for all systemic administration products |
| Reference Nanomaterials | Method validation and comparison | Supports substantial equivalence demonstrations |
Frequently Asked Questions
Q1: How does FDA determine if my product requires nano-specific regulation? A: FDA applies a two-point framework considering both size (1-100 nm) and dimension-dependent properties, even for materials up to 1000 nm [6]. The key is whether nanotechnology application changes product safety or effectiveness.
Q2: What are the most common mistakes in nanotech regulatory submissions? A: The most frequent issues include inadequate material characterization, insufficient batch-to-batch reproducibility data, and lack of nano-specific toxicology studies [14]. Early FDA consultation is recommended to avoid these pitfalls.
Q3: How do regulatory pathways differ between nanotech drugs and devices? A: Drugs require safety and effectiveness demonstration regardless of technology, while devices use risk-based classification [1]. Nanotech often pushes devices into higher classes or requires De Novo classification [12].
Q4: Are generic nanotech products eligible for abbreviated pathways? A: Yes, but demonstrating sameness is challenging. FDA issues product-specific guidances addressing complex nanotech generics, requiring extensive characterization and bioequivalence data [16] [14].
Q5: What post-market requirements apply to nanotechnology products? A: All products face ongoing monitoring, but nanotech may require additional surveillance for long-term effects, immunogenicity, and unique toxicity profiles [1] [14].
Workflow Visualization: Regulatory Pathway Decision Matrix
Diagram 1: Decision workflow for nanotechnology product regulatory pathways
Experimental Protocol: Nano-Characterization for Regulatory Compliance
Protocol 3: Standardized Nanomaterial Documentation Package
- Purpose: Create comprehensive documentation meeting multiple regulatory requirements
- Materials:
- Analytical grade reference standards
- Multiple manufacturing batches (minimum 3)
- Stability testing equipment
- Cell-based assay systems for toxicity screening
- Procedure:
- Physicochemical Characterization: Complete profiling of size, shape, surface, and composition
- Manufacturing Controls: Document process parameters and quality controls
- Stability Assessment: Real-time and accelerated conditions
- Biological Performance: Link material properties to biological effects
- Deliverable: Integrated summary bridging material science and biological data
This technical support resource will be updated quarterly as FDA issues new product-specific guidances and nanotechnology regulations evolve. Researchers should consult the most recent FDA guidance documents and engage in early consultations for novel technologies.
The Role of the 2007 Nanotechnology Task Force Report and Subsequent Guidance
In 2006, the U.S. Food and Drug Administration (FDA) formed an internal Nanotechnology Task Force to address the regulatory and scientific questions presented by the emergence of nanotechnology in FDA-regulated products [17]. The Task Force was charged with determining regulatory approaches that would enable the continued development of innovative, safe, and effective products that use nanoscale materials [17]. Its landmark report, issued in July 2007, established the FDA's initial policy foundation for evaluating the safety, effectiveness, and regulatory status of nanotechnology products [17] [2].
This technical support center distills the key outcomes of that report and the subsequent guidance documents into an actionable format for researchers and scientists. The FAQs and guides below are designed to help you navigate the specific regulatory and experimental issues you might encounter during the development of nanotechnology-based drugs, biological products, and devices.
Frequently Asked Questions (FAQs)
Q1: What was the main conclusion of the 2007 Nanotechnology Task Force Report regarding the FDA's regulatory authority?
The Task Force concluded that the FDA's existing authorities are "generally comprehensive" for products subject to premarket authorization (such as drugs, biologics, and devices) [17]. This means the agency has the ability to obtain detailed scientific information needed for review. However, oversight is less comprehensive for products not subject to premarket review, such as dietary supplements and cosmetics. The report therefore recommended issuing additional guidance to improve predictability and ensure public health protection [17].
Q2: Does the FDA have a singular, strict definition of "nanomaterial" for regulatory purposes?
No. The FDA has not established a single rigid regulatory definition [6]. Instead, its guidance provides two flexible "Points to Consider" to help identify if a product involves the application of nanotechnology [6]:
- Whether a material or end product is engineered to have at least one external dimension, or an internal or surface structure, in the nanoscale range (approximately 1 nm to 100 nm).
- Whether a material or end product is engineered to exhibit properties or phenomena (including physical, chemical, or biological effects) that are attributable to its dimension(s), even if these dimensions fall outside the nanoscale range, up to one micrometer (1,000 nm).
Q3: I am developing a drug product that contains a nanomaterial. What is the most critical recent guidance I should consult?
You should consult the April 2022 final guidance: "Drug Products, Including Biological Products, that Contain Nanomaterials - Guidance for Industry" [10]. This product-specific document provides the FDA's current thinking on the development of human drug products where a nanomaterial is present in the finished dosage form, whether as an active or inactive ingredient.
Q4: What is the FDA's overall philosophy for regulating nanotechnology products?
The FDA maintains a product-focused, science-based regulatory policy [1] [2]. The agency does not categorically judge all nanotechnology products as inherently benign or harmful. Instead, technical assessments are product-specific, taking into account the effects of nanomaterials in the particular biological and mechanical context of each product and its intended use [1]. Regulation occurs under existing statutory authorities, in accordance with the specific legal standards for each product type [2].
Q5: What should I do if I am developing a complex product that combines a diagnostic device and a therapeutic nanomaterial?
The 2007 Task Force Report specifically highlighted such combination products as an area needing clarity [17]. It strongly recommended that manufacturers communicate with the FDA early in the development process to facilitate a mutual understanding of the scientific and regulatory issues for these highly integrated products [17] [18].
Troubleshooting Your Regulatory Pathway: A Guide for Researchers
Problem: Uncertainty about when a material is considered a "nanomaterial" under FDA guidance.
Application of the FDA's "Points to Consider"
This protocol will help you determine if your material meets the points to consider for an FDA-defined nanotechnology product, a crucial first step in planning your regulatory strategy [6].
- Objective: To systematically evaluate a material against the FDA's two Points to Consider to determine if it involves the application of nanotechnology.
- Experimental Rationale: Early identification allows for appropriate safety and efficacy testing and informs pre-submission meetings with the FDA.
Step-by-Step Methodology:
Material Characterization:
- Use appropriate techniques (e.g., Dynamic Light Scattering, Electron Microscopy, Atomic Force Microscopy) to determine the physical dimensions of your material. Measure at least one external dimension.
- Decision Point: Is the material engineered to have at least one dimension in the range of approximately 1 nm to 100 nm?
- Result: If YES, the material satisfies Point to Consider 1. Proceed to investigate its biological and toxicological profile.
Property and Phenomenon Analysis:
- Even if the dimensions fall outside the 1-100 nm range (e.g., up to 1000 nm), investigate if the material exhibits dimension-dependent properties or biological effects.
- Compare the properties (e.g., chemical reactivity, magnetic, optical) and biological effects (e.g., altered bioavailability, tissue distribution, catalytic activity, toxicity) of your test material to its larger-scale counterpart with the same chemical composition.
- Decision Point: Are the observed properties or biological effects engineered and attributable to its dimension(s)?
- Result: If YES, the material satisfies Point to Consider 2.
Interpretation and Next Steps:
- An affirmative finding for either Point 1 or Point 2 suggests the product may involve the application of nanotechnology. This indicates a need for particular attention to identify and address potential implications for safety, effectiveness, and regulatory status [6].
- You should consult relevant product-specific FDA guidance documents and consider an early pre-submission meeting with the agency.
The following workflow diagram visualizes this decision-making process:
Problem: Determining the appropriate regulatory data for a drug product containing a nanomaterial.
Systematic Approach for Drug Developers
This methodology outlines the key considerations for planning the non-clinical studies needed to support an application for a drug or biological product containing nanomaterials [1] [10].
- Objective: To identify critical quality attributes and safety profiles of a nanomaterial-based drug product that may differ from conventional counterparts and require additional or modified testing.
- Experimental Rationale: The altered chemical, physical, or biological properties of nanomaterials can impact product quality, safety, and efficacy. A tailored testing strategy is essential [17] [2].
Key Experimental Considerations Table:
| Testing Category | Key Parameters to Investigate | Rationale & Regulatory Basis |
|---|---|---|
| Physicochemical Characterization | Size and size distribution, surface charge (zeta potential), surface chemistry/reactivity, surface area, morphology, solubility, aggregation/agglomeration potential. | These parameters are fundamental as they influence biological interactions, biodistribution, and stability. The 2014 guidance emphasizes understanding dimension-dependent properties [6]. |
| Pharmacokinetics/Toxicokinetics | Absorption, distribution, metabolism, and excretion (ADME) profile; bioaccumulation potential in tissues; plasma protein binding. | Nanomaterials may exhibit altered ADME compared to small molecules or larger particles, affecting safety and efficacy. This is a core element of the regulatory science research plan [1] [2]. |
| Safety Pharmacology & Toxicology | Repeated-dose toxicity; assessment of organs that may accumulate the nanomaterial (e.g., RES organs); immunotoxicity; potential for local tolerance reactions. | The Task Force Report highlighted that properties affecting safety might be amplified at the nanoscale, meriting particular examination [17] [18]. |
| Product Quality & Manufacturing | Control of manufacturing process to ensure consistent attributes; product stability; sterility if applicable. | The 2022 drug product guidance expects rigorous quality control for products containing nanomaterials [10]. |
The Scientist's Toolkit: Key Research Reagents & Materials
When conducting experiments to characterize nanomaterials for regulatory submissions, several key types of reagents and materials are essential. The table below lists critical solutions and their functions in the context of FDA guidance.
Research Reagent Solutions for Nanomaterial Characterization
| Research Reagent / Material | Primary Function in Experimental Protocols |
|---|---|
| Standard Reference Materials | Used for calibration and validation of analytical instruments (e.g., DLS, NTA, SEM) to ensure accurate size and morphology measurements, which are critical for the "Points to Consider" [6]. |
| Cell Culture Models | Relevant in vitro models (e.g., primary cells, cell lines) are used to assess nanomaterial biocompatibility, cytotoxicity, and immunotoxicity as part of the safety profile [18]. |
| Biomolecule Assay Kits | Kits for quantifying proteins, cytokines, or markers of oxidative stress are used to evaluate biological effects and potential immunotoxicity of nanomaterials [1]. |
| Chromatography Columns | Specialized columns (e.g., SEC, HPLC) are used to analyze the stability of the nanomaterial formulation and to detect potential aggregation or release of encapsulated agents [10]. |
| Animal Disease Models | Relevant in vivo models are used to study the pharmacokinetics, biodistribution, and efficacy of the nanomaterial-based drug product, providing data for the benefit-risk assessment [1]. |
Key FDA Guidance Documents for Nanotechnology Products
Frequently Asked Questions (FAQs)
Q1: What is the FDA's general approach to regulating nanotechnology products? The FDA employs a product-focused, science-based regulatory policy for nanotechnology. The agency does not categorically judge all nanotechnology products as inherently benign or harmful. Instead, evaluations are product-specific, considering the unique properties and behaviors of nanomaterials within the particular biological and mechanical context of each product and its intended use. The FDA regulates nanotechnology products under existing statutory authorities, applying the specific legal standards applicable to each product type under its jurisdiction [1] [2].
Q2: Are there specific FDA guidance documents dedicated to nanotechnology? Yes, the FDA has issued several guidance documents specifically addressing nanotechnology. These represent the FDA's current thinking on nanotechnology application in regulated products and are issued as part of the ongoing implementation of recommendations from the FDA's 2007 Nanotechnology Task Force Report [19] [2]. The most significant recent guidance is "Drug Products, Including Biological Products, that Contain Nanomaterials - Guidance for Industry" issued in April 2022 [10].
Q3: What is the recommended particle size range for considering a material a nanomaterial according to FDA guidance? While the FDA has not established a rigid regulatory definition, the guidance considers materials with dimensions up to 1,000 nm (1 micron) to be nanomaterials when they are engineered to exhibit size-dependent properties or phenomena. This is particularly relevant when these properties differ from those observed at larger scales. For reference, a human hair is approximately 80,000-100,000 nanometers wide [5].
Q4: What are the key challenges in characterizing nanomaterials for regulatory submissions? Characterization challenges include:
- Measurement limitations: Standard light microscopes cannot resolve objects smaller than ~250 nm due to the diffraction limit, requiring specialized techniques [5].
- Size distribution: Particle size distribution may significantly affect desired product properties and must be carefully controlled [5].
- Stability issues: Nanomaterials may exhibit changes in size distribution, morphology, solid state, or tendency for aggregation/agglomeration during storage [5].
Q5: Does the FDA require premarket review for all products containing nanomaterials? Premarket review requirements depend on the product category:
- Premarket review required: New drugs, new animal drugs, biologics, food additives, color additives, certain human devices, and certain new dietary ingredients [1].
- Premarket review not required: Dietary supplements (except certain new dietary ingredients), cosmetics (except color additives), and conventional foods (except food or color additives). For these products, the FDA encourages voluntary early consultation before marketing [1].
Q6: What are Critical Quality Attributes (CQAs) for nanomaterial-containing drug products? CQAs are physical, chemical, biological, or microbiological properties that must be within appropriate limits to ensure desired product quality. For nanomaterials, these typically include:
- Particle size and size distribution
- Morphology and solid state
- Surface characteristics
- Tendency for aggregation/agglomeration Early identification of CQAs helps manufacturers develop appropriate in-process controls [5].
Table 1: Key FDA Nanotechnology Guidance Documents
| Document Title | Focus Area | Issue Date | Status | Key Considerations |
|---|---|---|---|---|
| Drug Products, Including Biological Products, that Contain Nanomaterials | Human drug products & biologics | April 2022 | Final | Development considerations for drug products where nanomaterials serve as active/inactive ingredients or carriers [10] |
| Further guidance documents listed on FDA's Nanotechnology Guidance webpage | Various FDA-regulated products | Varies | Final & Draft | Address use of nanotechnology/nanomaterials across product categories [19] |
Table 2: Technical Characterization Parameters for Nanomaterial-Containing Drug Products
| Parameter Category | Specific Attributes | Analytical Challenges | Impact on Product Quality |
|---|---|---|---|
| Physicochemical Properties | Particle size/size distribution, surface charge, surface chemistry, morphology, solid state | Standard microscopy limited to >250 nm; requires specialized techniques | Affects biological behavior, stability, and performance [5] |
| Manufacturing Controls | Process sensitivity, scale-up effects, purification methods | Reproducibility challenges during manufacturing scale-up | Impacts consistency and quality of final product [5] |
| Stability Considerations | Size distribution changes, aggregation/agglomeration, morphological shifts | Requires specialized stability-indicating methods | Affects shelf life, storage conditions, and in vivo performance [5] |
Experimental Protocols for Nanomaterial Characterization
Protocol 1: Comprehensive Physicochemical Characterization
Objective: To fully characterize nanomaterials in drug products to establish Critical Quality Attributes (CQAs) [5].
Methodology:
- Particle Size Analysis:
- Employ dynamic light scattering (DLS) for hydrodynamic diameter
- Use electron microscopy (SEM/TEM) for primary particle size and morphology
- Implement asymmetric flow field-flow fractionation (AF4) for complex mixtures
Surface Characterization:
- Determine zeta potential using electrophoretic light scattering
- Analyze surface chemistry through X-ray photoelectron spectroscopy (XPS)
- Quantify surface functional groups using spectroscopic methods
Structural Analysis:
- Assess crystallinity using X-ray diffraction (XRD)
- Determine molecular weight distribution via gel permeation chromatography (GPC)
- Analyze elemental composition through inductively coupled plasma (ICP) techniques
Data Interpretation: Correlate physicochemical parameters with biological performance and stability profiles. Establish acceptance criteria for each CQA based on clinical relevance.
Protocol 2: Biological Safety Assessment
Objective: To evaluate potential biological interactions and safety concerns specific to nanomaterials [1] [5].
Methodology:
- In Vitro Toxicity Screening:
- Conduct cytotoxicity assays using multiple cell lines relevant to exposure routes
- Perform hemocompatibility testing for intravenous products
- Assess oxidative stress and inflammatory response markers
Biodistribution Studies:
- Use radiolabeling or fluorescent tagging to track nanomaterial distribution
- Quantify accumulation in target and non-target organs over time
- Evaluate clearance pathways and potential for long-term retention
Immunotoxicity Assessment:
- Analyze complement activation potential
- Assess effects on immune cell function and proliferation
- Evaluate potential for hypersensitivity reactions
Data Interpretation: Compare nanomaterial safety profile with conventional formulations. Identify nanomaterial-specific safety concerns that require additional monitoring.
Protocol 3: Manufacturing Control and Validation
Objective: To ensure consistent nanomaterial quality during manufacturing and scale-up [5].
Methodology:
- Process Parameter Optimization:
- Identify critical process parameters (CPPs) through design of experiments (DoE)
- Establish design space for nanomaterial synthesis and purification
- Define in-process controls for each manufacturing step
Scale-up Studies:
- Evaluate impact of scale on nanomaterial characteristics
- Identify potential critical quality attribute shifts during technology transfer
- Establish equivalence criteria between development and commercial scales
Purification and Isolation:
- Optimize purification methods to remove process impurities
- Establish controls for residual solvents and catalysts
- Validate cleaning procedures for equipment dedication
Data Interpretation: Demonstrate manufacturing process robustness and establish validated analytical methods for routine quality control.
Regulatory Pathway Decision Framework
Nanomaterial Characterization Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials for Nanomaterial Research and Development
| Reagent/Material | Function | Application Examples | Critical Considerations |
|---|---|---|---|
| Lipids | Form nanoliposomal structures for drug delivery | Doxil (doxorubicin) formulations | Purity critical for structure/function; must control oxidation [5] |
| Polymers | Create nanoparticle carriers for controlled release | Polymeric nanoparticles for gene delivery | Molecular weight distribution affects drug release kinetics [5] |
| Surface Modifiers | Modify nanomaterial surface properties | PEG coating for stealth properties | Surface density and conformation impact biological behavior [5] |
| Characterization Standards | Validate analytical methods | Size standards, reference materials | Essential for method qualification and comparability studies [5] |
| Stability Indicators | Monitor product degradation | Antioxidants, preservatives | Must not interfere with nanomaterial properties or performance [5] |
Developing and Submitting Your Nanotechnology Product for FDA Review
Premarket Review Requirements for Drugs, Biologics, and Devices
Technical Support Center: FAQs and Troubleshooting
This guide provides answers to frequently asked questions and troubleshooting advice for researchers and scientists navigating the premarket review requirements for drugs, biologics, and devices, with a specific focus on products involving nanotechnology.
Frequently Asked Questions (FAQs)
Q1: What is the foundational regulatory standard for a Quality Management System (QMS) in medical device development? The U.S. Food and Drug Administration (FDA) has updated its medical device current good manufacturing practice (CGMP) requirements by incorporating by reference the international standard ISO 13485:2016. This means that aligning your quality system with ISO 13485 is a central expectation for most premarket submissions for devices [20].
Q2: Does the FDA require special labeling for products using nanotechnology? Based on past assessments, FDA task forces have concluded that products using nanotechnology do not automatically require special labeling. This determination is made on a case-by-case basis, as the current science does not consistently show that nanomaterials pose a greater safety concern than their larger counterparts. However, all products must still meet existing safety substantiation requirements [21].
Q3: How is a "biologic" different from a "drug" in the context of premarket review? The key difference lies in the origin and complexity of the product. Biologics are derived from living organisms and are generally larger and more complex than chemically synthesized drugs. This distinction is critical because the pathway for demonstrating similarity to an existing product differs significantly, as seen with the biosimilar approval process for biologics versus the Abbreviated New Drug Application (ANDA) pathway for generic drugs [22].
Q4: What is a major recent change intended to streamline the biosimilar approval process? In a significant update from October 2025, the FDA issued a draft guidance that may reduce the need for comparative clinical efficacy studies for certain biosimilars. If a developer can provide a highly sensitive comparative analytical assessment demonstrating biosimilarity, along with a pharmacokinetic similarity study and an immunogenicity assessment, it may be sufficient for approval. This can potentially shorten the development timeline by 1-3 years [22].
Q5: Where can I find the FDA's official guidances on premarket submissions? The FDA provides a centralized search page for all guidance documents on its website. You can search by keywords (e.g., "premarket," "nanotechnology") and filter results by product category (e.g., "Medical Devices," "Biologics"), issue date, and document status (draft or final) to find the most current information [4].
Troubleshooting Common Scenarios
Scenario 1: Uncertainty about QMS documentation for a premarket device submission.
- Problem: A sponsor is unsure what quality system information to include in a Premarket Approval (PMA) application for a new device incorporating nanomaterials.
- Solution: Consult the FDA's draft guidance, "Quality Management System Information for Certain Premarket Submission Reviews." This document outlines the expectations for QMS information in submissions once the updated rule aligning 21 CFR Part 820 with ISO 13485 takes effect. Ensure your QMS procedures and submitted documentation are compliant with the principles of ISO 13485:2016 [20].
Scenario 2: A clinical laboratory is unsure about the regulatory status of its Laboratory Developed Tests (LDTs).
- Problem: Following recent litigation, there is confusion over whether LDTs are regulated as medical devices.
- Solution: As of 2025, the status has reverted to the previous framework. A U.S. District Court vacated the FDA's rule that sought to extend its authority over LDTs, classifying them as "professional medical services" outside the scope of medical device regulation. Laboratories should maintain vigilance for any new legislative or regulatory actions from Congress or the FDA [23].
Scenario 3: Designing a clinical trial for a biosimilar product.
- Problem: A sponsor wants to avoid the high cost and long duration of a comparative clinical efficacy study for a biosimilar.
- Solution: Refer to the FDA's new draft guidance on biosimilars. Focus resources on developing a robust comparative analytical assessment that demonstrates the proposed biosimilar is highly similar to the reference product. If the product meets certain criteria (e.g., is well-characterized, and the relationship between its attributes and clinical efficacy is understood), you may be able to submit a justification to waive the comparative efficacy study, relying instead on pharmacokinetic and immunogenicity data [22].
The table below summarizes key quantitative information related to premarket pathways and regulatory actions.
Table 1: Key Regulatory and Development Metrics
| Metric | Data | Context / Source |
|---|---|---|
| Potential Biosimilar Development Time Saved | 1-3 years | Via updated FDA guidance waiving comparative clinical efficacy studies [22]. |
| Average Cost of Clinical Efficacy Study | ~$24 million | For biosimilar development [22]. |
| Approved Biosimilars (as of 2025) | 76 | Referencing a "small fraction of approved biologics" [22]. |
| ISO Standard for Device QMS | ISO 13485:2016 | Incorporated by reference in updated FDA QMSR [20]. |
Experimental Protocols for Regulatory Science
This section outlines generalized methodologies for key experiments often required in premarket submissions, particularly for novel products like those using nanomaterials.
Protocol 1: Comparative Analytical Assessment for a Biosimilar
1. Objective: To demonstrate through extensive structural and functional analysis that a proposed biosimilar product is highly similar to an FDA-licensed reference product, despite minor differences in clinically inactive components.
2. Materials:
- Research Reagent Solutions:
- Reference Product: Multiple lots of the originator biologic product.
- Proposed Biosimilar: Multiple manufacturing lots of the product under development.
- Cell Lines: Clonal cell lines for production (e.g., CHO cells).
- Analytical Instruments: Mass spectrometers, chromatographs (HPLC, UPLC), capillary electrophoresis systems, circular dichroism spectrometers.
- Assay Kits: For evaluating biological activity (e.g., cell-based bioassays, binding ELISAs).
3. Methodology:
- Primary Structure Analysis: Use peptide mapping with LC-MS/MS to confirm amino acid sequence and post-translational modifications (e.g., glycosylation, oxidation).
- Higher-Order Structure Analysis: Employ techniques like Circular Dichroism (CD) and Hydrogen-Deuterium Exchange Mass Spectrometry (HDX-MS) to assess secondary and tertiary structure.
- Functional Assays:
- Conduct in vitro bioassays to measure the biological activity relative to the reference product. This often involves cell-based proliferation or signaling assays.
- Perform binding assays (e.g., Surface Plasmon Resonance) to characterize affinity for target receptors.
- Impurity and Stability Profile: Compare levels of product-related impurities (e.g., aggregates, fragments) and degradation profiles under stressed conditions (e.g., heat, light, pH) to the reference product.
- Data Analysis: Use statistical methods to establish equivalence ranges and demonstrate that any observed differences are within pre-defined, justified limits and are not clinically meaningful.
Protocol 2: Quality Management System (QMS) Audit for a Medical Device
1. Objective: To ensure a manufacturer's QMS complies with FDA regulations, which are harmonized with ISO 13485:2016, and is capable of consistently producing devices that meet specifications and regulatory requirements.
2. Materials:
- Research Reagent Solutions:
- QMS Documentation: Quality manual, documented procedures, standard operating procedures (SOPs).
- Records: Design history file (DHF), device master record (DMR), device history records (DHRs), management review records, internal audit reports.
- Traceability Tools: A system for tracking components, materials, and finished devices.
3. Methodology:
- Documentation Review: Audit the QMS documentation to verify it addresses all required elements of the quality system regulation (21 CFR 820 / ISO 13485), including management responsibility, resource management, product realization, and measurement, analysis, and improvement.
- Process Confirmation: Observe processes like design controls, purchasing controls, production and process controls, and corrective and preventive action (CAPA) to ensure they are implemented as documented.
- Record Sampling: Select a sample of DHRs to verify that devices were manufactured according to the DMR. Review CAPA records to ensure non-conformities are investigated, resolved, and effectiveness checks are performed.
- Management Interview: Interview top management to confirm their commitment to the quality policy and that quality objectives are established and reviewed.
- Reporting: Document all findings (conformities and non-conformities) in an audit report. Non-conformities require a root cause analysis and a corrective action plan.
Regulatory Pathway and Experimental Workflow Visualization
Premarket Review Logic Flow
Biosimilar Analytical Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Regulatory-Focused Experiments
| Item / Solution | Function in Premarket Development |
|---|---|
| ISO 13485:2016 Standard | The foundational framework for establishing a Quality Management System for medical devices, as recognized by the FDA [20]. |
| Reference Product | The licensed originator product (for biologics/drugs) or predicate device; serves as the benchmark for demonstrating comparability, similarity, or substantial equivalence [22]. |
| Clonal Cell Lines | Used in the production of biologics and biosimilars to ensure consistency and purity, a key factor in the updated biosimilar guidance [22]. |
| Mass Spectrometry (MS) | A core analytical technique for characterizing the primary structure (amino acid sequence, post-translational modifications) of protein-based products [22]. |
| Cell-Based Bioassays | Functional assays used to measure the biological activity of a product (e.g., a biologic or biosimilar) and demonstrate it is equivalent to the reference product [22]. |
| Nanomaterial Characterization Tools | Instruments for measuring size, surface charge, and morphology (e.g., DLS, SEM, TEM) are critical for products using nanotechnology to understand their potential impact [24]. |
Frequently Asked Questions (FAQs)
Q1: How does the FDA define "nanomaterial" for regulatory purposes?
The FDA has not established a single rigid regulatory definition. However, the agency considers whether a material or end product is engineered to have at least one external dimension, or an internal or surface structure, in the nanoscale range (approximately 1 nm to 100 nm). Furthermore, the FDA also considers whether a material is engineered to exhibit properties or phenomena attributable to its dimension(s), even if these dimensions fall outside the nanoscale range, up to one micrometer (1,000 nm) [25] [5]. This flexible, case-specific approach allows the FDA to evaluate a diverse range of nanomaterials.
Q2: Are the safety standards for nanomaterials different from those for conventional materials?
No, the same standards of safety, efficacy, and quality apply to products containing nanomaterials as to all other regulated products [5] [2]. However, the pathway to meeting these standards may differ. The unique properties of nanomaterials, such as increased surface area and altered bioavailability, may necessitate additional or modified testing to provide sufficient evidence that the product meets the required safety and effectiveness standards for its intended use [1] [25].
Q3: What is the most critical step in the early development of a product containing nanomaterials?
Early consultation with the FDA is highly encouraged [1] [2]. The agency advises manufacturers to engage in pre-submission meetings to facilitate a mutual understanding of the specific scientific and regulatory issues for their nanotechnology product. This is crucial for clarifying the methodologies and data needed to meet regulatory obligations, especially given the product-specific nature of the FDA's assessment [1].
Q4: For which product types does the FDA require premarket review of nanomaterials?
The requirement for premarket review depends on the product category, not the presence of nanomaterials per se. The following table summarizes the premarket review status for major product categories [1]:
| Product Category | Premarket Review Required? | Governing Statute |
|---|---|---|
| New Drugs & Biologics | Yes (NDA, BLA) | FD&C Act § 505 |
| New Animal Drugs | Yes | FD&C Act |
| Food Additives & Color Additives | Yes | FD&C Act § 409 |
| Certain Medical Devices | Yes (PMA, 510(k)) | FD&C Act |
| Dietary Supplements (with certain new dietary ingredients) | Yes | FD&C Act |
| Cosmetics (except color additives) | No | FD&C Act |
| Most Dietary Supplements | No | FD&C Act |
Q5: If my cosmetic product contains a nanomaterial, what are my responsibilities?
Although cosmetics (except for color additives) are not subject to FDA premarket approval, manufacturers are legally responsible for ensuring their products are safe and properly labeled [25]. The cosmetic must not be adulterated or misbranded. For nanomaterials, this means you must substantiate the safety of the product through adequate testing, which may require special consideration of the nanomaterial's unique properties. The FDA encourages voluntary consultation and submission of safety substantiation data [1] [25].
Troubleshooting Guides
Issue: Inconsistent Results in Particle Size Distribution Analysis
Problem: Measurements of particle size and size distribution, a Critical Quality Attribute (CQA), show high variability between batches or during stability testing.
Solution:
- Validate Characterization Methods: Standard light microscopes cannot resolve objects smaller than ~250 nm [5]. Ensure you are using specialized techniques appropriate for the nanoscale, such as:
- Dynamic Light Scattering (DLS)
- Electron Microscopy (SEM, TEM)
- Atomic Force Microscopy (AFM)
- Control Manufacturing Processes: Nanomaterials can be sensitive to process conditions and scale-up. Identify and tightly control Critical Process Parameters (CPPs) that impact particle size, such as mixing speed, temperature, and solvent addition rates [5].
- Conduct Stability Studies: Monitor for changes in particle size distribution over time as part of your stability protocol. Aggregation or agglomeration can be a sign of formulation instability [5].
Issue: Difficulty in Assessing Nanomaterial Toxicity Using Standard Tests
Problem: Traditional toxicology testing methods may not be fully applicable or may yield misleading results due to the distinctive physicochemical properties of nanomaterials.
Solution:
- Conduct Thorough Material Characterization: Before toxicological assessment, fully characterize the nanomaterial. Key properties include [25]:
- Size, size distribution, and aggregation state
- Morphology and shape
- Surface chemistry, charge, and area
- Chemical composition and purity
- Modify Testing Protocols: Traditional assays may need to be modified to account for nanomaterial-specific behaviors, such as interference with assay reagents or adsorption of biomolecules. Consider using dosimetry metrics relevant to the nanoscale (e.g., surface area) in addition to mass concentration [25].
- Investigate Toxicokinetics: Evaluate the Absorption, Distribution, Metabolism, and Excretion (ADME) profile of the nanomaterial, as its small size may alter its bioavailability and biodistribution compared to its larger-scale counterpart [25].
Experimental Protocols & Data Presentation
Protocol 1: Framework for Safety Assessment of Nanomaterials in Cosmetics
This protocol outlines a general framework for assessing the safety of nanomaterials in cosmetic products, as recommended by the FDA [25].
1. Principle: The safety assessment should be sufficiently robust and flexible to account for the novel or altered properties of nanomaterials. It relies on thorough material characterization and toxicological evaluation, which may require modified or novel testing methods.
2. Methodology:
- Step 1: Physicochemical Characterization
- Determine particle size, size distribution, and dispersion state.
- Analyze morphology (shape, structure) using electron microscopy.
- Measure surface characteristics: zeta potential, surface chemistry, functional groups, and surface area.
- Determine chemical composition, including crystallinity and impurity profile.
- Step 2: Toxicological Assessment
- Uptake and Absorption: Assess dermal penetration and potential for systemic exposure using appropriate in vitro or ex vivo models (e.g., reconstructed human epidermis).
- Toxicity Testing:
- Conduct in vitro assays for cytotoxicity, phototoxicity, and genotoxicity.
- Perform in vivo studies for repeated dose toxicity, sensitization, and irritation as needed.
- Toxicokinetics: Investigate the distribution, metabolism, and excretion of the nanomaterial if systemic exposure is anticipated.
- Step 3: Safety Substantiation
- Integrate all characterization and toxicology data.
- Perform a risk assessment based on the intended use and exposure levels.
- Establish the final safety conclusion for the finished product.
Protocol 2: Identifying Critical Quality Attributes (CQAs) for Nanomaterial Drug Products
This protocol describes the process for identifying CQAs for a nanomaterial-based drug product, which is essential for developing appropriate controls [5].
1. Principle: CQAs are physical, chemical, biological, or microbiological properties that must be within an appropriate limit, range, or distribution to ensure the desired product quality, safety, and efficacy. For nanomaterials, these are often linked to their physical nanostructure.
2. Methodology:
- Step 1: Link Material Properties to Clinical Performance
- Bridge changes in nanomaterial properties (e.g., size, surface charge) to desired clinical outcomes (e.g., targeting, drug release profile, reduced toxicity).
- Step 2: Identify Potential CQAs
- Based on the link to performance, identify properties that are likely critical. For nanomaterials, this often includes:
- Particle size and polydispersity index (PDI)
- Particle surface charge (Zeta Potential)
- Drug loading and encapsulation efficiency
- In vitro drug release profile
- Morphology and structural integrity
- Based on the link to performance, identify properties that are likely critical. For nanomaterials, this often includes:
- Step 3: Develop and Implement Controls
- Develop in-process controls and analytical methods to monitor these CQAs during manufacturing.
- Include these CQAs in stability-testing protocols to monitor changes over the product's shelf life.
Quantitative Data and Standards
The following table summarizes key physicochemical parameters that often require monitoring and typical analytical techniques used, as referenced in FDA guidance documents [25] [5].
| Parameter | Significance / Impact | Recommended Analytical Techniques |
|---|---|---|
| Particle Size & Distribution | Affects biodistribution, targeting, clearance, and toxicity profile. | Dynamic Light Scattering (DLS), Electron Microscopy (SEM/TEM), Analytical Ultracentrifugation |
| Zeta Potential | Indicates colloidal stability; influences cellular uptake and interaction with biological components. | Electrophoretic Light Scattering |
| Surface Area | Increased area can enhance reactivity, dissolution, and biological activity. | Brunauer-Emmett-Teller (BET) Analysis |
| Surface Chemistry | Determines biological identity (protein corona), targeting, and safety. | X-ray Photoelectron Spectroscopy (XPS), Fourier-Transform Infrared Spectroscopy (FTIR) |
| Crystallinity | Can impact chemical stability, dissolution rate, and bioavailability. | X-Ray Diffraction (XRD) |
| Drug Release Kinetics | Critical for efficacy; must be demonstrated in a physiologically relevant medium. | Dialysis, Franz Diffusion Cell, USP Apparatus |
Regulatory Pathway Diagram
Safety Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Application |
|---|---|
| Standard Reference Materials | Certified materials with known properties (e.g., size, surface area) used for calibration and validation of analytical instruments. |
| Cell Culture Models | In vitro systems (e.g., reconstructed human epidermis, Caco-2 cells) used for initial screening of cytotoxicity, absorption, and irritation. |
| Lipids & Polymers | Building blocks for engineered nanomaterials like liposomes and polymeric nanoparticles, used as drug delivery vehicles or functional excipients. |
| Surface Modifiers | PEG, peptides, or other ligands used to functionalize the surface of nanomaterials to improve stability, targeting, or reduce immunogenicity. |
| Stability Testing Buffers | Simulated biological fluids (e.g., simulated gastric fluid, plasma) used to assess the stability and drug release profile of the nanomaterial under physiological conditions. |
| Analytical Standards | High-purity nanomaterials used as benchmarks for comparing properties and performance between batches during development and quality control. |
The Critical Importance of Early FDA Consultation in the Development Process
For researchers and scientists developing nanotechnology-enabled products, engaging with the U.S. Food and Drug Administration (FDA) early in the development process is a critical strategic step. The FDA regulates nanotechnology products under existing statutory authorities, employing a product-focused, science-based regulatory policy that varies according to the specific legal standards applicable to each product type [1]. Nanomaterials can exhibit different chemical, physical, or biological properties compared to their larger-scale counterparts, which may raise important questions about product safety, effectiveness, performance, quality, or public health impact [6] [2]. The FDA does not categorically judge all products containing nanomaterials as intrinsically benign or harmful, but rather evaluates them on a case-by-case basis according to their specific characteristics and intended use [1]. This article provides a technical guide to facilitate effective regulatory navigation for nanotechnology products, emphasizing why early consultation is essential for efficient development.
Determining When Your Product Involves Nanotechnology
FDA's Points to Consider
The FDA has issued guidance outlining two key points to consider when determining whether an FDA-regulated product involves the application of nanotechnology. These points serve as an initial screening tool that researchers should apply during early development phases [6].
| Point to Consider | Description | Technical Scope |
|---|---|---|
| Point 1 | Whether a material or end product is engineered to have at least one external dimension, or an internal or surface structure, in the nanoscale range. | Approximately 1 nm to 100 nm [6] |
| Point 2 | Whether a material or end product is engineered to exhibit properties or phenomena attributable to its dimension(s), even if these dimensions fall outside the nanoscale range. | Up to one micrometer (1,000 nm) [6] |
Key Terminology and Concepts
- Engineered Materials: The FDA specifically focuses on materials that have been "deliberately manipulated" to produce specific properties, distinguishing them from materials that naturally exist at the nanoscale or are incidentally present in conventionally-manufactured products [6].
- Dimension-Dependent Properties: Properties or phenomena (e.g., increased structural integrity, altered chemical or biological activity) that are attributable to a material's dimension(s), even outside the traditional 1-100 nm range [6].
Troubleshooting Common Nanotechnology Development Challenges
Frequently Asked Questions
Q1: Our nanoparticle-based drug delivery system has dimensions between 100-200 nm but exhibits properties not seen in larger particles. Does this require special FDA consideration?
A: Yes. According to FDA guidance, materials engineered to exhibit dimension-dependent properties even outside the traditional 1-100 nm range (up to 1,000 nm) may merit particular examination. You should evaluate whether these new properties affect safety, effectiveness, or public health impact, and consult with the FDA [6].
Q2: We're developing a cosmetic product containing nanomaterials. What are our regulatory obligations?
A: While cosmetics (except color additives) are not subject to mandatory premarket review, you remain responsible for ensuring your product meets all applicable safety standards. The FDA encourages voluntary consultation before marketing and recommends conducting a robust safety assessment that addresses the unique physicochemical properties and potential toxicological implications of nanomaterials [1].
Q3: Our company wants to use a previously approved drug substance in a new nanoformulation. What regulatory pathway applies?
A: A new drug application would typically be required because the nanoformulation may have different safety, effectiveness, or bioavailability profiles compared to the conventionally-manufactured product. You must submit data demonstrating the safety and effectiveness of the new formulation, paying particular attention to how the nanoscale properties may affect its behavior [1].
Q4: What specific technical data should we prepare for an early FDA consultation regarding our nanotechnology product?
A: You should be prepared to discuss:
- Comprehensive physicochemical characterization of the nanomaterial
- Identification and control of critical quality attributes
- Demonstration of manufacturing process control and consistency
- Preliminary safety and toxicology data specific to the nanomaterial properties
- Assessment of potential changes in bioavailability, pharmacokinetics, or biological effects compared to non-nano counterparts [1]
Experimental Protocols for Nanotechnology Product Characterization
Key Methodologies for Regulatory Submissions
Protocol 1: Physicochemical Characterization of Nanomaterials
Purpose: To comprehensively characterize nanomaterials for regulatory submissions, addressing the FDA's emphasis on understanding unique properties that may impact product safety or performance [6].
Materials and Reagents:
- Purified nanomaterial sample
- Appropriate dispersion media (e.g., PBS, cell culture medium)
- Reference standards (when available)
- Grids for electron microscopy (as applicable)
Procedure:
- Size and Size Distribution: Perform dynamic light scattering (DLS) measurements in triplicate using appropriate dispersion media reflective of the product's use conditions.
- Surface Charge: Determine zeta potential using electrophoretic light scattering in relevant physiological buffers.
- Morphology: Characterize particle morphology using transmission or scanning electron microscopy (TEM/SEM).
- Surface Chemistry: Analyze surface functional groups using X-ray photoelectron spectroscopy (XPS) or Fourier-transform infrared spectroscopy (FTIR).
- Crystallinity: Assess crystalline structure using X-ray diffraction (XRD).
- Surface Area: Determine specific surface area using Brunauer-Emmett-Teller (BET) method.
Data Analysis: Document mean particle size, polydispersity index, zeta potential, and other relevant parameters. Compare multiple batches to establish consistency.
Troubleshooting Tip: If aggregation occurs during characterization, optimize dispersion protocols while maintaining physiological relevance.
Protocol 2: Assessment of Nanomaterial Stability
Purpose: To evaluate the stability of nanomaterials under conditions relevant to manufacturing, storage, and use, as stability changes may alter safety or performance profiles [1].
Materials and Reagents:
- Nanomaterial formulation
- Appropriate storage containers
- Analytical instruments for characterization (as above)
Procedure:
- Real-Time Stability: Store nanomaterials under recommended storage conditions and monitor physicochemical parameters at predetermined timepoints (e.g., 0, 1, 3, 6 months).
- Accelerated Stability: Expose nanomaterials to stressed conditions (elevated temperature, humidity, mechanical stress) and monitor for changes.
- In-Use Stability: Evaluate stability under conditions simulating actual use (e.g., in biological fluids, after reconstitution).
- Dissolution/Release Profile: For drug-containing nanomaterials, characterize release kinetics using appropriate methods.
Data Analysis: Establish acceptance criteria for critical quality attributes and monitor for changes exceeding these criteria.
The Scientist's Toolkit: Essential Research Reagents and Materials
Key Research Reagent Solutions for Nanotechnology Development
| Reagent/Material | Function | Technical Considerations |
|---|---|---|
| Dynamic Light Scattering (DLS) Instrument | Measures particle size distribution and zeta potential | Essential for demonstrating consistent nanomaterial size; use multiple dispersion media for comprehensive characterization [6] |
| Electron Microscopy Supplies | Visualizes nanomaterial morphology and structure | Provides critical data on particle shape, surface texture, and potential aggregation [6] |
| Reference Nanomaterials | Serves as controls for method validation | Use well-characterized nanomaterials to validate analytical methods and instrument performance |
| Cell Culture Systems | Assesses biological interactions and potential cytotoxicity | Required for preliminary safety assessment; use multiple cell types relevant to exposure routes [1] |
| Chromatography Materials | Separates and analyzes nanomaterial components | Critical for quantifying drug loading, release kinetics, and potential impurities |
| Animal Models | Evaluates in vivo behavior and toxicology | Necessary for comprehensive safety assessment; select models relevant to intended exposure route [1] |
Regulatory Pathways for Nanotechnology Products
Product-Specific Regulatory Considerations
The FDA's regulatory approach to nanotechnology products varies significantly based on product category and applicable legal standards. Understanding these differences is crucial for selecting the appropriate development strategy [1].
| Product Category | Premarket Review Requirement | Key Regulatory Considerations for Nanotechnology |
|---|---|---|
| Drugs & Biologics | Required (NDA, BLA) | Safety and effectiveness evaluation must consider unique nanomaterial properties; increased focus on pharmacokinetics, biodistribution, and potential immunogenicity [1] |
| Medical Devices | Required for certain devices (PMA, 510(k)) | Evaluation of safety and effectiveness should address nanomaterial characteristics and their impact on device performance and biological responses [1] |
| Cosmetics | Not required (voluntary consultation encouraged) | Manufacturer responsible for safety; FDA recommends specific consideration of nanomaterial penetration, toxicity, and exposure assessment [1] |
| Food & Food Additives | Required for food additives | Safety assessment must address potential changes in bioavailability, absorption, or toxicity due to nanoscale properties [1] |
| Dietary Supplements | Required for new dietary ingredients | Manufacturer must demonstrate safety; nanoformulations may require additional data on absorption and distribution [1] |
Approved Nanomedicines: Case Studies
Reviewing successfully approved nanotechnology products provides valuable insight into regulatory expectations and acceptable development approaches.
| Product Name | Approval Date | Nanotechnology Platform | Indication |
|---|---|---|---|
| Doxil | FDA (1995) | PEGylated liposomal formulation | HIV-associated Kaposi's sarcoma, ovarian cancer [26] |
| Rapamune | FDA (2010) | Nanocrystal formulation | Immunosuppression in kidney transplant patients [26] |
| Onpattro | FDA (2018) | Lipid nanoparticle | Hereditary transthyretin-mediated amyloidosis [26] |
| Abelcet | FDA (1995) | Lipid complex | Antifungal therapy [26] |
Engaging with the FDA early in the development process for nanotechnology products is not merely a regulatory formality but a critical strategic step that can significantly influence development timelines and success rates. The FDA's flexible, science-based approach requires researchers to thoroughly characterize their nanomaterials, understand how nanoscale properties affect product behavior, and generate robust data demonstrating safety and effectiveness under applicable regulatory standards [1]. By utilizing the troubleshooting guides, experimental protocols, and technical resources provided in this article, researchers can more effectively navigate the regulatory pathway for their innovative nanotechnology products, potentially bringing important new treatments to patients while ensuring their safety and efficacy.
Post-Market Surveillance and Ongoing Safety Monitoring Obligations
Regulatory Foundation for Nanotechnology-Enabled Health Products (NHPs)
What is the FDA's regulatory stance on nanotechnology-enabled health products?
The U.S. Food and Drug Administration (FDA) regulates a wide range of products, including foods, cosmetics, drugs, devices, and veterinary products that may utilize nanotechnology or contain nanomaterials [24]. The FDA employs a flexible, product-focused, and science-based approach to regulating these products, recognizing that nanomaterials can have chemical, physical, and biological properties that differ from their larger counterparts [24]. The agency participates in the National Nanotechnology Initiative (NNI) to help coordinate federal research and development efforts in nanoscale science, engineering, and technology [24].
How are Nanotechnology-Enabled Health Products classified?
NHPs are primarily categorized based on their principal mechanism of action, which determines their regulatory pathway [3]. The table below outlines the primary regulatory classifications.
Table: Regulatory Classification of Nanotechnology-Enabled Health Products
| Product Category | Primary Mechanism of Action | Regulatory Focus | Examples |
|---|---|---|---|
| Medicinal Products | Pharmacological, Immunological, or Metabolic (PIM) [3] | Safety, efficacy, and quality verification [3] | Drug-loaded nanoparticles, nanoliposomal formulations [3] |
| Medical Devices | Predominantly physical or mechanical (may include supplemental PIM actions) [3] | Safety and performance; post-market surveillance for AI-enabled devices [3] [27] | AI-enabled diagnostic systems, nano-based sensors [28] |
| In Vitro Diagnostic (IVD) Medical Devices | Analysis of human proximal body fluids [3] | Different technical and safety challenges compared to in-vivo products [3] | Nanomaterials for multi-biomarker analysis [3] |
Post-Market Surveillance Framework
What are the core components of a post-market surveillance system?
A robust post-market surveillance system for NHPs, particularly those incorporating AI, should include two complementary mechanisms as outlined in recent regulatory proposals [29]. The workflow for implementing this surveillance is illustrated below.
What triggers the need for enhanced post-market surveillance for AI-enabled NHPs?
The FDA has highlighted that AI system performance can be influenced by changes in clinical practice, patient demographics, data inputs, and health care infrastructure after deployment [27]. This can lead to data drift, concept drift, or model drift, which may compromise the safety and reliability of AI-enabled devices in real-world settings [27]. The FDA's traditional premarket review system is considered insufficient for AI medical devices whose unpredictability may only emerge after deployment [29].
Troubleshooting Common Post-Market Surveillance Challenges
How can we effectively monitor for and respond to "model drift"?
Problem: AI models in NHPs may degrade in performance over time due to evolving data, a phenomenon known as drift [27].
Solution: Implement a continuous performance monitoring plan with the following steps [28] [27]:
- Define Performance Metrics: Establish clear metrics for safety, effectiveness, and reliability specific to the device's intended use.
- Implement Monitoring Tools: Deploy tools and methodologies to track these metrics in real-world clinical use.
- Identify Reassessment Triggers: Predefine data-driven thresholds that trigger a formal reassessment of the model (e.g., a specific drop in accuracy or change in input data distribution).
- Plan for Mitigation: Have documented procedures for addressing identified performance degradation, which may include model retraining, updating, or other corrective actions.
How can we conduct post-market surveillance without violating patient privacy or intellectual property?
Problem: Traditional monitoring might require sharing sensitive patient data or proprietary model information.
Solution: Utilize a framework that employs periodic revalidation using existing test data [29]. This approach reuses the manufacturer's original premarket test data to revalidate the device periodically. It does not require health systems to access the device's source code, nor does it require manufacturers to access new patient data, thus preserving both intellectual property and patient privacy [29].
What are the key documentation requirements for NHP surveillance?
Documentation Needs: The FDA expects comprehensive documentation for AI-enabled systems, which can be extrapolated to complex NHPs [28]. You must be prepared to provide:
- Design controls and validation strategy.
- Data lineage from raw input to model output.
- Intended use statement and training data documentation.
- Bias mitigation and performance monitoring plans.
- Change control procedures and immutable audit trails.
The Scientist's Toolkit: Key Reagents & Materials for NHP Characterization
Safety assessments for NHPs require specific characterization due to their unique physicochemical properties. The table below details essential reagents and materials for key experimental protocols.
Table: Essential Research Reagents for NHP Characterization and Safety Assessment
| Research Reagent / Material | Function / Application | Key Considerations for NHPs |
|---|---|---|
| Dynamic Light Scattering (DLS) Instrument | Measures particle size distribution and hydrodynamic diameter in suspension. | Critical for confirming nanoscale dimensions (1-100 nm) and monitoring aggregation [30]. |
| Cell-Based Models (e.g., Caco-2, Hepatocytes) | In vitro models for assessing absorption, distribution, metabolism, excretion (ADME), and toxicity. | NHP's high surface area can increase reactivity; use intact and impaired skin models for dermal penetration studies [31]. |
| Animal Models for Toxicological Studies | In vivo assessment of systemic toxicity and organ-specific effects. | Required for repeated dose (21-28 days) and subchronic (90 days) toxicity studies; care needed as reduced particle size can increase uptake and potential toxicity [31]. |
| Genotoxicity/Mutagenicity Assay Kits (e.g., Ames Test, Micronucleus) | Determine if the NHP causes genetic damage. | A basic requirement; unique NPM properties may necessitate modified testing methods [31]. |
| Protein Corona Analysis Tools (e.g., SDS-PAGE, Mass Spectrometry) | Characterize the layer of proteins that adsorb onto nanoparticles in biological fluids. | Protein corona formation can alter the nanoparticle's biological identity, targeting, and clearance [3]. |
Frequently Asked Questions (FAQs)
Do we need to specially label our product if it contains nanotechnology?
Currently, the FDA's position, as reflected in a past task force report, is that products with nanotechnology do not require special labeling because the available science does not support a finding that they pose a greater safety concern than products without it [21]. However, regulatory guidance is evolving, and it is essential to consult the most recent FDA documents.
Our NHP uses an ingredient already considered GRAS (Generally Recognized as Safe). Do we need new safety data?
Yes. If manufacturing process changes, including the use of nanotechnology, significantly alter the properties of a food substance (which includes dietary supplements), the FDA states that the GRAS criteria may no longer apply [31]. Safety assessments should be based on data relevant to the nano-engineered version, as changes in bioavailability can raise new safety issues [31].
What is the role of real-world evidence in post-market surveillance?
The FDA is increasingly interested in how real-world evidence can be used to monitor device performance [27]. They are seeking input on practical methods for ongoing performance evaluation in clinical environments, such as integrating device data with electronic health records [27]. This reflects a shift towards a total product lifecycle approach to regulation.
What are the incentives for manufacturers to implement robust post-market surveillance?
Manufacturers have several strong motivations [29]:
- Avoid Liability: To prevent device failures that could lead to legal and financial liabilities, especially since the "Learned Intermediary Rule" may not protect against injuries from complex, low-explainability AI systems.
- Protect Reputation: To avoid reputational damage from safety-related market withdrawals.
- Enable Innovation: Proactive surveillance provides a pathway for the responsible adoption of innovative but complex technologies, building trust with regulators and healthcare providers.
Special Considerations for Products Not Subject to Premarket Review (e.g., Cosmetics, Dietary Supplements)
For researchers and scientists developing nanotechnology-enabled products, navigating the U.S. Food and Drug Administration (FDA) regulatory landscape is crucial. This guide focuses on the distinct regulatory pathways for products not subject to premarket review, such as cosmetics and dietary supplements, which differ significantly from drugs or medical devices. Understanding these pathways is essential for designing appropriate safety testing protocols and ensuring regulatory compliance from the earliest stages of product development [1] [32].
What is the FDA's general approach to regulating nanotechnology in products like cosmetics and dietary supplements?
The FDA regulates nanotechnology products under its existing statutory authorities, using a product-focused, science-based policy [1]. The agency does not categorically judge all products containing nanomaterials as either intrinsically benign or harmful [1]. For products not subject to premarket review, the FDA encourages manufacturers to consult with the agency before marketing and relies on post-market surveillance activities to provide oversight [1]. The core principle is that industry remains responsible for ensuring that its products meet all applicable legal requirements, including safety standards [1] [2].
Do cosmetics containing nanomaterials require FDA premarket approval?
No. Cosmetic products and ingredients, including those utilizing nanotechnology, do not require FDA premarket approval [32]. The exception is color additives (other than coal-tar hair dyes), which are subject to FDA approval [32]. Despite the lack of premarket approval, cosmetics must be safe for their intended use and properly labeled [32]. Companies are required to substantiate the safety of their products before marketing [21].
Do dietary supplements containing nanomaterials require FDA premarket approval?
No. The FDA is not authorized to approve dietary supplements for safety and effectiveness before they are marketed [32]. However, companies are required to submit a premarket safety notification to the FDA at least 75 days before marketing dietary supplements containing a "new dietary ingredient" (one not marketed in the U.S. before October 15, 1994) [32]. Manufacturers must ensure their products are safe before marketing and comply with labeling and good manufacturing practice requirements [32].
What safety standards must my nanotechnology-based cosmetic or dietary supplement meet?
Regardless of premarket approval requirements, manufacturers are legally required to ensure their products satisfy all applicable safety standards [1]. The FDA advises that evaluations of safety for products containing nanomaterials should consider the unique properties and behaviors that these materials may exhibit [1]. The specific legal standards for safety vary between product categories [1].
Should I consult with the FDA before developing a cosmetic nanomaterial?
Yes, early consultation is strongly encouraged. The FDA recommends that manufacturers consult with the agency early in the product development process to address questions related to safety, effectiveness, or regulatory status [1] [2]. These consultations help facilitate a mutual understanding of the scientific and regulatory issues and can clarify the methodologies and data needed to meet regulatory obligations [1].
Are there special labeling requirements for nanomaterials in cosmetics or supplements?
Currently, the FDA's position, as reflected in a 2006 Task Force report, is that products with nanotechnology do not need to be specially labeled because "the current science does not support a finding that products with nanotechnology pose a greater safety concern than products without it" [21]. All labeling must still be truthful and not misleading.
Troubleshooting Guide: Common Regulatory Scenarios
| Scenario | Regulatory Consideration | Recommended Action |
|---|---|---|
| A new nanomaterial is developed for use in a face cream. | The product is a cosmetic. No premarket approval is required, but the manufacturer is responsible for safety substantiation [32]. | Conduct comprehensive safety testing. Consult FDA guidance. Maintain detailed records of safety substantiation. |
| A new herbal extract, processed using nanotechnology, is intended for use in a capsule for immune support. | The product is a dietary supplement. A premarket notification may be required if it is a "new dietary ingredient" [32]. | Determine if the ingredient is "new". If so, prepare and submit a New Dietary Ingredient (NDI) notification. |
| A nanoparticle is intended for use as a colorant in a shampoo. | The product is a color additive, which requires premarket approval by the FDA, regardless of its use in a cosmetic [32]. | Submit a color additive petition to the FDA for approval before marketing. |
| An existing dietary supplement is reformulated to enhance bioavailability using nanotechnology. | A significant manufacturing change that alters the substance could trigger the need for a new NDI notification [32]. | Evaluate whether the nanoscale processing creates a "new" dietary ingredient requiring notification. |
| A cosmetic product with a nanomaterial receives consumer reports of skin irritation. | The FDA monitors adverse event reports and can take post-market action if a product is found to be unsafe [1] [32]. | Report serious adverse events to the FDA via MedWatch. Investigate the cause and consider a voluntary recall if necessary. |
Experimental Protocols for Regulatory Science
Protocol 1: Assessing the Need for Regulatory Submission
Diagram 1: Regulatory pathway decision tree for nanomaterials.
Objective: To systematically determine the appropriate regulatory pathway for a product containing nanomaterials.
Methodology:
- Product Categorization: Precisely define the product's intended use. This determines the regulatory category (e.g., cosmetic, dietary supplement, drug). Claims such as "treats disease" will classify the product as a drug, triggering premarket approval requirements [32].
- Ingredient Status Assessment:
- Pathway Determination: Based on the categorization and status, follow the appropriate regulatory pathway as outlined in Diagram 1.
Protocol 2: Framework for Safety Substantiation Dossier Development
Diagram 2: Safety substantiation workflow for nanomaterials.
Objective: To compile a robust safety substantiation dossier for a nanomaterial used in a cosmetic or dietary supplement, fulfilling the manufacturer's regulatory responsibility [1] [21].
Methodology:
- Physicochemical Characterization:
- Size and Size Distribution: Use Dynamic Light Scattering (DLS) and Electron Microscopy.
- Surface Charge: Measure zeta potential.
- Surface Chemistry and Reactivity: Use techniques like Fourier-Transform Infrared Spectroscopy (FTIR).
- Agglomeration/Aggregation State: Analyze in relevant solvents and matrices.
- Toxicological Assessment:
- Conduct in vitro assays for cytotoxicity and irritation.
- Perform genotoxicity studies (e.g., Ames test, Micronucleus assay).
- Based on exposure routes, conduct in vivo studies for systemic toxicity.
- Exposure Assessment:
- Determine the route (dermal, oral), frequency, and duration of exposure.
- Estimate the concentration of the nanomaterial that users will be exposed to.
- Risk Assessment and Dossier Assembly:
- Integrate data from characterization, toxicology, and exposure assessments.
- Prepare a comprehensive report that substantiates the safety of the nanomaterial for its intended use.
The Scientist's Toolkit: Research Reagent Solutions
| Research Tool | Function in Nanomaterial Development |
|---|---|
| Dynamic Light Scattering (DLS) Instrument | Measures the hydrodynamic diameter and size distribution of nanoparticles in suspension [2]. |
| Zeta Potential Analyzer | Determines the surface charge of nanoparticles, which predicts colloidal stability and interaction with biological systems [2]. |
| Electron Microscopy (SEM/TEM) | Provides high-resolution imaging of nanomaterial morphology, size, and structure [2]. |
| In Vitro Toxicity Assays (e.g., MTT, Ames test) | Assesses the baseline biological reactivity and potential genotoxicity of nanomaterials before complex in vivo studies. |
| Model Skin/Epithelial Membranes | Used to study dermal penetration and absorption of nanomaterials intended for topical applications. |
| Simulated Biological Fluids (e.g., gastric/intestinal fluids) | Evaluates the stability and behavior of nanomaterials designed for oral administration (e.g., in supplements). |
Overcoming Common Regulatory Hurdles for Nanotech Applications
Addressing Unique Physicochemical Properties and Characterization Challenges
FAQs: Core Concepts and Regulatory Importance
Why do the physicochemical properties of nanomaterials require special attention during characterization? Nanomaterials possess unique, size-dependent properties that differ significantly from their bulk counterparts. These differences arise primarily from two factors: their dramatically increased surface area-to-volume ratio and quantum confinement effects [33] [34]. This means that as particle size decreases, a greater proportion of atoms are located on the surface, increasing reactivity and potentially altering biological interactions [3] [33]. For regulatory purposes, the U.S. FDA emphasizes that these very changes may influence the safety, effectiveness, or other attributes of a product, making thorough characterization essential [1].
Which physicochemical properties are considered Critical Quality Attributes (CQAs) for nanomaterial-based products? For regulatory submissions and to ensure product consistency, several physicochemical parameters are critical. The FDA's science-based, product-specific assessment focuses on properties that influence biological behavior [1] [35]. Key CQAs include:
- Size and Size Distribution: Influences biodistribution, cellular uptake, and clearance [33] [35].
- Surface Characteristics: Includes surface charge (zeta potential), chemistry, and morphology, which affect stability, interaction with biological systems, and targeting capability [33] [35].
- Shape and Aspect Ratio: Impacts cellular internalization, flow properties, and toxicity profiles [33].
- Drug Loading and Release Kinetics: Critical for demonstrating controlled release and therapeutic efficacy [35].
How does nanoparticle shape influence biological activity and safety? Particle shape is a critical determinant of biological activity. Spherical nanoparticles are typically endocytosed more easily and rapidly than rod-shaped or fibrous particles [33]. Conversely, high-aspect-ratio materials (e.g., certain nanotubes or fibers) can present unique toxicological challenges; for instance, long, rigid fibers may resist clearance by macrophages, potentially leading to chronic inflammation, a phenomenon well-documented with asbestos [33]. This has direct implications for the safety profile of a product and must be characterized.
Troubleshooting Guides: Common Experimental Challenges
Challenge 1: Controlling and Characterizing Nanoparticle Size and Dispersion
Problem: A nanoparticle suspension shows significant batch-to-batch variability in size and a tendency to agglomerate, leading to inconsistent experimental results.
Solution:
- Optimize Synthesis and Formulation: Reproducible manufacturing is paramount [35]. Systematically control parameters like solvent addition rate, energy input (e.g., sonication), and stabilizer concentration.
- Implement Robust Characterization: Use Dynamic Light Scattering (DLS) to measure hydrodynamic diameter and polydispersity index (PDI). A PDI below 0.2 is generally considered monodisperse. Confirm results with orthogonal methods like Transmission Electron Microscopy (TEM) to visualize core size and morphology, as DLS can be biased by large agglomerates or dust [34].
- Prevent Agglomeration: Enhance colloidal stability by modulating surface charge (zeta potential). A high zeta potential (typically > |±30| mV) creates strong electrostatic repulsion between particles [34]. Alternatively, use steric stabilizers like polyethylene glycol (PEG) to prevent aggregation.
Challenge 2: Assessing Stability Under Physiological Conditions
Problem: Nanoparticles are stable in pure water but aggregate rapidly in biological media (e.g., cell culture medium, serum), compromising their function.
Solution:
- Pre-characterize in Relevant Media: Do not rely solely on characterization in simple buffers. Perform DLS and zeta potential measurements directly in the biological medium or a relevant simulant to understand behavior in the application environment.
- Understand the "Protein Corona": In serum-containing media, proteins adsorb onto the nanoparticle surface, forming a "corona" that defines the biological identity of the particle [34]. Characterize this corona using techniques like gel electrophoresis or LC-MS to understand how it affects targeting and cellular uptake.
- Design Surface Chemistry Accordingly: Engineer the nanoparticle surface to resist non-specific protein adsorption. PEGylation is a common strategy to create a "stealth" effect, but other hydrophilic polymers are also used [35].
Challenge 3: Differentiating Core, Shell, and Surface Properties
Problem: Difficulty in separately analyzing the core material, shell layer, and surface ligands, which is crucial for complex, multi-component nanomedicines.
Solution:
- Employ a Tiered Analytical Approach:
- Core: Use TEM for core size and morphology. X-ray diffraction (XRD) can determine crystallinity.
- Shell/Coating: Use techniques like Fourier-Transform Infrared Spectroscopy (FTIR) or X-ray Photoelectron Spectroscopy (XPS) to confirm the chemical composition and presence of the shell material.
- Surface Ligands: Use techniques such as Nuclear Magnetic Resonance (NMR) or HPLC to quantify and confirm the integrity of surface-conjugated targeting moieties or drugs [35] [34].
- Monitor Drug Release Kinetics: Use dialysis-based methods or centrifugal filtration with HPLC-UV/FL detection to establish a release profile for the encapsulated drug, which is a key functional attribute linking physicochemical properties to biological performance [35].
Experimental Protocols for Key Characterization Assays
Protocol: Determining Hydrodynamic Size and Zeta Potential
Methodology: Dynamic Light Scattering (DLS) and Laser Doppler Micro-electrophoresis.
Key Steps:
- Sample Preparation: Dilute the nanoparticle sample in an appropriate dispersant (e.g., water, PBS) to achieve an optimal scattering intensity. Filter the dispersant through a 0.1 or 0.2 µm filter to remove dust.
- Equipment Setup: Standardize instrument settings (temperature, equilibration time, measurement angle) across all batches.
- Measurement: Perform DLS measurement in triplicate to obtain the Z-average diameter and PDI. For zeta potential, measure the electrophoretic mobility and apply the Henry equation to calculate the value. Report the mean and standard deviation from multiple runs.
- Data Interpretation: A low PDI indicates a monodisperse sample. A high zeta potential (positive or negative) indicates good electrostatic stability.
Protocol: Visualizing Nanoparticle Morphology and Core Size
Methodology: Transmission Electron Microscopy (TEM).
Key Steps:
- Grid Preparation: Deposit a small volume (5-10 µL) of diluted nanoparticle suspension onto a carbon-coated copper TEM grid.
- Staining (if needed): For organic or soft nanoparticles, negative staining with agents like uranyl acetate or phosphotungstic acid can enhance contrast.
- Imaging and Analysis: Allow the sample to dry completely before imaging under the microscope. Use image analysis software to measure the diameter of at least 200 particles from multiple images to generate a statistically valid size distribution histogram.
Table 1: Correlation Between Physicochemical Properties and Biological/Toxicological Effects
| Physicochemical Property | Biological/Toxicological Implication | Key Evidence | ||
|---|---|---|---|---|
| Size | Determines biodistribution, cellular uptake, and clearance pathways. Particles <50 nm can access most tissues, while 100-200 nm particles are more readily taken up by the reticuloendothelial system (RES) [33]. | Inhaled particles <100 nm deposit in all respiratory regions; particles 10-20 nm deposit in alveoli [33]. | ||
| Surface Charge (Zeta Potential) | Influences protein corona formation, colloidal stability, and cellular interaction. Highly positive or negative surfaces generally increase cellular uptake but may also increase cytotoxicity. | High zeta potential (> | ±30 | mV) improves stability via electrostatic repulsion, preventing aggregation [34]. |
| Aspect Ratio | Affects macrophage clearance and toxicity. High-aspect-ratio materials (e.g., long fibers) can frustrate phagocytosis, leading to prolonged residence and inflammation. | Asbestos fibers >10 µm cause lung carcinoma; fibers >5 µm cause mesothelioma; TiO2 fibers 15 µm are highly toxic vs. 5 µm fibers [33]. | ||
| Surface Area | Increased surface area per unit mass enhances chemical and biological reactivity. A higher surface area can lead to greater catalytic activity and increased generation of reactive oxygen species (ROS). | Smaller nanoparticles with higher surface area cause a dose-dependent increase in oxidative and DNA damage abilities greater than larger particles of the same mass [33]. |
Table 2: Essential Techniques for Nanoparticle Characterization
| Characterization Technique | Property Measured | Typical Output | Considerations for Regulatory Submissions |
|---|---|---|---|
| Dynamic Light Scattering (DLS) | Hydrodynamic diameter, size distribution (PDI) | Z-average, intensity distribution | Report intensity-based distribution; use orthogonal methods (TEM) to confirm. Essential for quality control. |
| Transmission Electron Microscopy (TEM) | Core size, morphology, dispersion state | High-resolution images | Provides "number-based" distribution. Critical for visualizing structure and confirming DLS data. |
| Zeta Potential Measurement | Surface charge, colloidal stability | Zeta potential (mV) | Measure in relevant pH and medium. Indicates batch-to-b consistency and in-vivo stability potential. |
| UV-Vis Spectroscopy | Concentration, optical properties (for some NPs) | Absorption spectrum, concentration | Used for quantifying concentration and monitoring changes in surface plasmon resonance (e.g., for gold NPs). |
| HPLC / Chromatography | Drug loading, encapsulation efficiency, release kinetics | Chromatogram, drug concentration | Crucial for demonstrating controlled release and quantifying the active pharmaceutical ingredient (API). |
Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle Characterization
| Item/Category | Function/Explanation | Example Applications |
|---|---|---|
| Size Standards | Calibrate and validate size measurement instruments (e.g., DLS). | Polystyrene beads of known diameter (e.g., 50 nm, 100 nm). Ensure accurate and reproducible size data. |
| Zeta Potential Transfer Standards | Verify the performance and calibration of zeta potential instruments. | Latex or other standardized particles with a known zeta potential. |
| Sterile Filters | Remove microbial contamination and large aggregates from nanoparticle suspensions prior to biological testing. | 0.22 µm PVDF or PES syringe filters. |
| Dialysis Membranes / Cassettes | Separate free/unencapsulated drug from nanoparticles to determine drug loading and study release kinetics. | Membranes with specific Molecular Weight Cut-offs (MWCO). |
| Stains for Electron Microscopy | Enhance contrast for TEM imaging of organic or soft nanomaterials. | Uranyl acetate, phosphotungstic acid. |
Experimental and Regulatory Workflows
Experimental Characterization Pathway
Protein Corona Impact Pathway
Proactively Managing Potential Safety and Toxicity Uncertainties
For researchers and drug development professionals, navigating the safety assessment of nanotechnology products is paramount. The U.S. Food and Drug Administration (FDA) regulates these products under existing statutory authorities, using a product-focused, science-based policy [1] [2]. The FDA does not categorically judge all nanotechnologies as benign or harmful, but recognizes that the unique properties of nanomaterials merit particular examination to determine their effects on product safety, effectiveness, or performance [1] [6]. This technical support center provides targeted guidance to help you address specific safety and toxicity uncertainties proactively during product development, aligning with the FDA's regulatory expectations.
FAQs: Addressing Critical Safety Questions
1. When does the FDA consider a product to involve the application of nanotechnology? The FDA employs two "Points to Consider". A product may involve nanotechnology if:
- It is engineered to have at least one external dimension, or an internal or surface structure, in the nanoscale range (approximately 1 nm to 100 nm).
- It is engineered to exhibit properties or phenomena (e.g., physical, chemical, or biological effects) that are attributable to its dimension(s), even if these dimensions fall outside the nanoscale range, up to one micrometer (1,000 nm) [6].
2. What is the FDA’s general approach to regulating nanotechnology products? The FDA’s approach is flexible and adaptive. Key principles include:
- Regulating under existing authorities: The Agency uses its current regulatory framework, which is considered sufficiently robust and flexible for nanomaterials [1] [2].
- Product-specific and science-based: Technical assessments consider the effects of nanomaterials in the specific biological and mechanical context of each product and its intended use [1].
- Varied legal standards: Safety and effectiveness evaluations are governed by the specific legal standards for each product class (e.g., drugs vs. cosmetics) [1].
- Encouragement of early consultation: The FDA strongly encourages manufacturers to consult with the agency early in the development process [1].
3. What are the primary mechanisms through which nanoparticles (NPs) may exert toxicity? Understanding the mechanisms of nanotoxicity is crucial for risk assessment. The primary pathways include:
- Oxidative Stress: NPs can generate reactive oxygen species (ROS), leading to oxidative damage of cellular components like lipids, proteins, and DNA [36] [37].
- Mitochondrial Damage: Accumulation of NPs in mitochondria can disrupt the electron transport chain, reducing ATP production and potentially triggering apoptosis [36].
- Inflammatory Response: NPs can activate inflammatory pathways, leading to the release of pro-inflammatory cytokines and causing tissue damage [36].
- DNA Damage and Cell Cycle Disruption: Some NPs can cause genotoxic effects, leading to DNA strand breaks and interference with normal cell cycle progression [36].
- Apoptosis: Cellular uptake of NPs can initiate programmed cell death through intrinsic or extrinsic pathways [36].
The following diagram illustrates the interconnected nature of these key toxicity mechanisms.
4. Our product is a topical cosmetic. Are we subject to premarket review, and how should we handle nanomaterial safety? For products not subject to mandatory premarket review, such as cosmetics (except for color additives), the responsibility for safety rests with the manufacturer [1]. The FDA recommends:
- Proactive Safety Assurance: You are responsible for ensuring your product meets all applicable safety standards [1].
- Voluntary Consultation: The FDA encourages you to consult with the agency before marketing. This allows FDA to advise on safety information and the design of any necessary post-marketing safety oversight [1].
Troubleshooting Guides: From Toxicity Mechanisms to Solutions
Issue: Observing High Cytotoxicity In Vitro
Potential Causes & Investigative Steps:
| Potential Cause | Investigation Method | Reference |
|---|---|---|
| Size-dependent uptake: Smaller NPs (e.g., ~10 nm) are more readily taken up by cells and can cause increased cytotoxicity. | Characterize NP core size, hydrodynamic diameter, and size distribution using Dynamic Light Scattering (DLS) and Transmission Electron Microscopy (TEM). Correlate size data with cell viability assays. | [36] |
| Reactive Oxygen Species (ROS) generation: NP-induced oxidative stress is a primary mechanism of toxicity. | Measure intracellular ROS levels using fluorescent probes (e.g., DCFH-DA). Assess downstream markers like lipid peroxidation (MDA assay) and antioxidant depletion (GSH levels). | [36] [37] |
| Composition and ion release: Metallic NPs (e.g., Ag, ZnО) may release toxic ions in the biological milieu. | Use techniques like inductively coupled plasma mass spectrometry (ICP-MS) to quantify dissolved ions in cell culture media over time. Compare toxicity of particles to ionic controls. | [38] |
Recommended Actions:
- Surface Modification: Coat the NP with inert materials (e.g., PEGylation) to reduce direct cellular interactions and improve biocompatibility [37].
- Adjust Physicochemical Properties: If possible, increase the NP size to a less reactive range or modify the surface charge to be slightly negative to reduce non-specific binding.
Issue: Unpredicted Inflammatory Response in Animal Models
Potential Causes & Investigative Steps:
| Potential Cause | Investigation Method | Reference |
|---|---|---|
| Persistent inflammation due to poor clearance: NPs may be recognized as foreign, triggering a prolonged immune response. | Conduct histopathological analysis of exposed tissues (e.g., lung, liver, spleen). Measure pro-inflammatory cytokines (e.g., IL-1β, TNF-α) in serum or bronchoalveolar lavage fluid (BALF). | [36] [39] |
| Surface charge and opsonization: Positively charged NPs are more likely to be opsonized and cleared by the immune system, provoking inflammation. | Characterize the surface charge (zeta potential) in physiological buffers. Analyze protein corona formation using gel electrophoresis or mass spectrometry. | [38] [37] |
Recommended Actions:
- Surface Functionalization: Employ stealth coatings (e.g., PEG, polysorbates) to minimize opsonization and macrophage uptake.
- Thorough Pre-clinical Characterization: Expand immunotoxicity testing in relevant animal models, including detailed biodistribution and persistence studies.
Experimental Protocols for Safety Assessment
Protocol 1: Assessing Oxidative Stress and Mitochondrial Damage
Objective: To evaluate the potential of engineered NPs to induce oxidative stress and impair mitochondrial function in a relevant cell line (e.g., human hepatic HepG2 cells).
Materials:
- Cell Line: HepG2 cells.
- Test Material: Your engineered NPs, suspended in appropriate vehicle (e.g., saline, PBS with low concentration of dispersant).
- Controls: Vehicle control, positive control for oxidative stress (e.g., tert-Butyl hydroperoxide).
- Reagents:
- DCFH-DA dye: For measuring intracellular ROS.
- JC-1 dye: For measuring mitochondrial membrane potential (ΔΨm).
- ATP Assay Kit: For quantifying cellular ATP levels.
- GSH/GSSG Assay Kit: For assessing glutathione balance.
Methodology:
- Cell Culture and Treatment: Seed HepG2 cells in 96-well or 24-well plates and allow to adhere overnight. Treat cells with a range of NP concentrations for 4-24 hours.
- ROS Measurement: Load cells with DCFH-DA (10 µM) for 30 min. After treatment, wash cells and measure fluorescence (Ex/Em: 485/535 nm).
- Mitochondrial Membrane Potential: Incubate treated cells with JC-1 dye (5 µg/mL) for 20 min. Analyze using fluorescence microscopy or a plate reader. A shift from red (J-aggregates) to green (J-monomers) fluorescence indicates depolarization.
- ATP Quantification: Lyse treated cells and use a luciferase-based ATP assay kit according to the manufacturer's instructions. Measure luminescence.
- GSH/GSSG Ratio: Lyse cells and use a commercial kit to quantify reduced (GSH) and oxidized (GSSG) glutathione. A decreased GSH/GSSG ratio indicates oxidative stress.
The workflow for this comprehensive assessment is outlined below.
Protocol 2: In Vivo Acute Toxicity Screening in Rodents
Objective: To identify potential acute toxic effects and biodistribution of NPs following a single dose in a rodent model.
Materials:
- Animals: Rats or mice (e.g., Sprague-Dawley rats, 8-10 weeks old).
- Test Material: Sterile, endotoxin-free NP suspension.
- Dosing: Single administration via a relevant route (e.g., intravenous, oral gavage, pharyngeal aspiration).
- Equipment: Clinical chemistry analyzer, hematology analyzer, ICP-MS, tissue histopathology materials.
Methodology:
- Study Design: Randomly assign animals to control and treatment groups (e.g., low, mid, high dose). Include a satellite group for biodistribution.
- Dosing and Monitoring: Administer a single dose. Monitor animals closely for 14 days for mortality, clinical signs (aggression, inactivity), and body weight changes [38].
- Terminal Procedures: On day 14, collect blood for hematology (e.g., white blood cell count) and serum biochemistry (e.g., ALT, AST for liver function; creatinine for kidney function) [38].
- Necropsy and Histopathology: Perform gross necropsy. Collect and weigh key organs (liver, spleen, kidneys, lungs, heart). Preserve tissues in formalin for H&E staining and pathological evaluation.
- Biodistribution: Digest organs from the satellite group (sacrificed at an earlier time point, e.g., 24 hours) and analyze NP content using ICP-MS to determine tissue accumulation.
The Scientist's Toolkit: Research Reagent Solutions
| Research Reagent / Material | Primary Function in Nanotoxicity Assessment |
|---|---|
| DCFH-DA Probe | Cell-permeable dye that becomes fluorescent upon oxidation; used to measure intracellular ROS levels. |
| JC-1 Dye | Cationic dye that accumulates in mitochondria; fluorescence shift from red to green indicates loss of mitochondrial membrane potential (ΔΨm). |
| PEG (Polyethylene Glycol) | Polymer used for surface functionalization ("PEGylation") to reduce immune recognition, prolong circulation time, and decrease toxicity. |
| ICP-MS (Inductively Coupled Plasma Mass Spectrometry) | Analytical technique for precise quantification of elemental metal concentrations in tissues and fluids, essential for biodistribution studies of metallic NPs. |
| Dynamic Light Scattering (DLS) Instrument | Used to characterize the hydrodynamic size distribution and aggregation state of NPs in suspension. |
| Zeta Potential Analyzer | Measures the surface charge of NPs, which is critical for predicting colloidal stability and interaction with biological membranes. |
Navigating the GRAS (Generally Recognized as Safe) Pathway for Food Ingredients
This guide provides technical support for researchers and scientists navigating the GRAS pathway, with a focus on the significant regulatory changes anticipated for 2025 and 2026.
The Generally Recognized as Safe (GRAS) pathway is a legal designation for food substances that are considered safe by qualified experts, thus exempting them from the formal food additive approval process [40]. The current regulatory framework provides two pathways for confirming a substance is GRAS [40]:
- GRAS Notification (Voluntary): A entity notifies the FDA of its conclusion that a substance is GRAS. The FDA reviews the submission and issues a response letter.
- Self-Affirmed GRAS (Currently Permitted): An entity independently determines that a substance is GRAS without notifying the FDA, maintaining the determination internally.
Significant regulatory changes are on the horizon. The FDA is moving to eliminate the self-affirmed GRAS pathway [40] [41]. The proposed rule, which was expected in October 2025, would mandate the submission of GRAS notices for all substances claimed to be GRAS [40] [42] [43]. The timeline for implementation is accelerated, with potential finalization by March 2026 [44]. Furthermore, legislative reform was introduced in November 2025 via the "Better FDA Act of 2025" (S. 3122), which would require the FDA to maintain a public list of all GRAS substances [45].
Current and Proposed GRAS Pathways
Frequently Asked Questions (FAQs)
What is the fundamental legal standard for a GRAS determination?
A substance is GRAS if it is generally recognized, among experts qualified by scientific training and experience to evaluate its safety, as having been adequately shown through scientific procedures (or through experience based on common use in food prior to 1958) to be safe under the conditions of its intended use [40] [45].
What are the immediate steps my research team should take given the proposed changes?
- Inventory Substances: Review all ingredients and substances in your development pipeline that rely on self-affirmed GRAS status.
- Prepare Dossiers: Begin compiling comprehensive safety data and expert reports for potential submission.
- Monitor Dockets: Track the Federal Register for the official publication of the proposed rule and prepare to submit comments during the public period [40] [42] [44].
How might the proposed changes impact research and development timelines?
The transition to a mandatory notification system is expected to introduce new pre-market steps. Researchers should anticipate potential delays and build flexibility into project timelines to accommodate the FDA's review process, especially considering the agency's reduced workforce [40]. Early engagement with regulatory affairs professionals is recommended.
What is the status of the GRAS Notice Program in the interim?
Until a final rule is published and effective, the current GRAS framework remains in place. The FDA continues to accept and review voluntary GRAS notifications, as evidenced by the 47 "no questions" letters issued in Q3 2025 [46].
Troubleshooting Common GRAS Pathway Issues
Issue: Incomplete or Inadequate Safety Data
- Root Cause: The scientific evidence and data presented do not establish "reasonable certainty of no harm" under the intended conditions of use.
- Protocol: Conduct a comprehensive safety assessment including:
- Toxicological Studies: Thorough review of existing literature and, if necessary, new studies (e.g., genotoxicity, sub-chronic toxicity).
- Dietary Exposure Assessment: Estimate exposure levels based on proposed use in food categories and consumption data.
- Methodology: Adhere to FDA Redbook 2000 guidelines and OECD test guidelines for laboratory studies. Ensure all studies are conducted under Good Laboratory Practices (GLP).
Issue: Lack of General Recognition Among Qualified Experts
- Root Cause: Insufficient consensus or visibility among the broader scientific community regarding the safety data.
- Protocol: Establish a panel of independent, qualified experts.
- Expert Selection Criteria: Choose experts with relevant scientific training and experience, free from conflicts of interest.
- Documentation: Meticulously document the panel's review process, deliberations, and final conclusion in a detailed report.
Issue: Potential for FDA Rejection or "Cease to Evaluate"
- Root Cause: The GRAS notice does not provide a sufficient basis for a GRAS determination, as seen in two cases in Q3 2025 [46].
- Mitigation Strategy: Conduct a rigorous pre-submission internal review against the criteria in 21 CFR § 170.30 and recent FDA response letters. Consider seeking a pre-submission meeting with the FDA to discuss potential issues.
Recent GRAS Notifications and Agency Review
The table below summarizes the U.S. FDA's GRAS update activities for the third quarter of 2025, illustrating the current workflow and common substance categories [46].
| Submission Status | Number of Substances | Key Substance Categories |
|---|---|---|
| FDA Has No Questions | 47 | Microorganism-related (19), Alternative Sweeteners (4), HMOs (2) |
| Pending Review | 32 | Data not specified in search results |
| Insufficient Basis for GRAS | 2 | Data not specified in search results |
| Evaluation Ceased at Notifier's Request | 1 | Data not specified in search results |
The Scientist's Toolkit: Key Research Reagent Solutions
The table below details essential materials for building a robust GRAS dossier, particularly for novel substances like those derived from nanotechnology.
| Reagent/Material | Function in GRAS Determination |
|---|---|
| In vitro Toxicology Assay Kits | Screening for initial toxicity (e.g., genotoxicity, cytotoxicity) to prioritize further testing. |
| Chemical Identity & Purity Standards | Precisely characterizing the substance, including composition and impurity profiles, which is fundamental to the safety assessment. |
| Food Simulants | Testing potential migration of substances from food contact materials or assessing stability in various food matrices. |
| Reference Materials (e.g., USP, FCC) | Providing validated benchmarks for analytical method development and ensuring accurate quantification. |
| Stable Isotope-Labeled Analogs | Conducting metabolism, pharmacokinetic, and residue studies to understand the substance's fate in biological systems. |
Experimental Workflow for GRAS Determination
Strategies for Handling Changes in Manufacturing Processes
In the highly regulated field of nanotechnology product development, changes to manufacturing processes are inevitable. Whether scaling up from laboratory to commercial production or optimizing existing methods, each modification must be carefully managed to ensure it does not adversely affect the product's Critical Quality Attributes (CQAs). For products falling under the regulatory purview of the U.S. Food and Drug Administration (FDA), such changes must be executed within a robust framework that aligns with regulatory expectations for safety, efficacy, and quality [3] [24]. This technical support guide provides researchers and scientists with a structured approach to managing these changes, complete with troubleshooting advice and essential experimental protocols.
Frequently Asked Questions (FAQs)
1. What constitutes a major versus a minor change in a nanomedicine manufacturing process? A major change is one that has a significant potential to impact the product's CQAs. For nanotechnology-enabled health products (NHPs), this often includes changes to:
- Nanomaterial Source or Synthesis: Altering the method of synthesizing a lipid nanoparticle or changing a key raw material supplier [3] [13].
- Critical Process Parameters: Changing the mixing speed, sonication energy, or purification method in a way that could affect particle size, size distribution, or surface characteristics [3].
- Scale of Manufacturing: Scaling up from lab-scale equipment to commercial-scale bioreactors or reactors, which can alter the physical dynamics of the process [30] [47]. Minor changes are those with a validated, negligible risk to CQAs, such as equipment changes with demonstrated operational parity. Any major change typically requires a regulatory submission to the FDA [24].
2. How can we assess the impact of a manufacturing change without a full, costly new clinical trial? Leverage the FDA's "Quality by Design (QbD)" framework. A scientifically rigorous risk assessment should guide the creation of a comparability protocol. This involves identifying which CQAs are most likely to be affected by the change and conducting a focused battery of in vitro and in vivo studies. The table below outlines a potential strategy for a change in a nanocarrier's formulation.
Table: Experimental Strategy for a Formulation Change Assessment
| Attribute to Assess | Recommended Experiments | Acceptance Criteria for Comparability |
|---|---|---|
| Physical Properties | Particle size (DLS), PDI, zeta potential, morphology (TEM/SEM) | Data should fall within pre-defined ranges equivalent to the original process. |
| Chemical Composition/Purity | HPLC for drug loading/encapsulation efficiency, SDS-PAGE for protein-based NPs, assessment of impurities. | No new impurities; key chemical metrics must be equivalent. |
| In Vitro Performance | Drug release profile under physiologically relevant conditions, cell-based uptake/efficacy assays. | Release profile and cellular activity should be comparable. |
| In Vivo Biodistribution | Pharmacokinetics (PK) study in a relevant animal model (AUC, Cmax, half-life) [3]. | PK parameters should be bioequivalent. |
3. Our nanoparticle aggregation after a process change. What are the systematic troubleshooting steps? Aggregation indicates a potential change in the stability of the nanomaterial. Follow this diagnostic workflow:
4. What is the role of a "Comparability Protocol" in the FDA regulatory pathway? A Comparability Protocol is a detailed, pre-approved plan for how you will study the effect of a anticipated future change on product quality. Submitting this protocol to the FDA for review before implementing the change is a highly strategic tool. If the FDA agrees with your protocol, it can streamline the post-change reporting process, potentially allowing you to implement the change and simply notify the agency, reducing regulatory uncertainty and delay [3] [24].
The Scientist's Toolkit: Essential Research Reagent Solutions
When developing or troubleshooting nanotechnology-based health products, the selection of appropriate materials and analytical techniques is critical. The following table details key reagents and tools used in the field.
Table: Essential Materials and Tools for Nanomedicine Development
| Item / Reagent | Function / Explanation |
|---|---|
| Lipids & Polymers (e.g., PLGA, PEG-lipids) | Serve as the structural backbone for many nanocarriers (liposomes, polymeric NPs), controlling biodegradability, drug release kinetics, and surface properties [3] [30]. |
| Functionalization Ligands (e.g., Antibodies, Peptides) | Attached to the nanoparticle surface to enable active targeting to specific cells or tissues (e.g., cancer cells), enhancing therapeutic efficacy [3]. |
| Dynamic Light Scattering (DLS) Instrument | A core analytical technique for determining nanoparticle hydrodynamic size, size distribution (PDI), and aggregation state in solution [3]. |
| Chromatography Systems (HPLC, FPLC) | Used to quantify drug loading, encapsulation efficiency, and to detect potential impurities or degradation products in the final nanoparticle formulation [3]. |
| Atomic Layer Deposition (ALD) Tools | Used in the manufacture of nanochips and some complex nanodevices, enabling atomic-scale precision in material deposition, which is critical for consistent performance [47] [13]. |
Experimental Protocols for Key Characterization Assays
Protocol 1: Determining Nanoparticle Size and Zeta Potential
1. Principle: Dynamic Light Scattering (DLS) measures particle size by analyzing the Brownian motion of particles in suspension. Laser Doppler Micro-electrophoresis is used to measure zeta potential, which indicates the surface charge and colloidal stability. 2. Reagents: Nanoparticle suspension, appropriate dispersion medium (e.g., purified water, PBS, 1mM NaCl for zeta potential). 3. Procedure: * Sample Preparation: Dilute the nanoparticle sample sufficiently in the chosen medium to avoid signal saturation from multiple scattering. For zeta potential, a clear, low-conductivity medium is often preferred. * Equipment Setup: Equilibrate the instrument to the recommended temperature (e.g., 25°C). Standardize using a reference latex material of known size and zeta potential. * Measurement: Transfer the diluted sample into a disposable sizing cuvette (for size) or a folded capillary cell (for zeta potential). Insert into the instrument. * Data Acquisition: Run the measurement for a minimum of 3-12 runs per sample. For zeta potential, the software will calculate the electrophoretic mobility and apply the Henry equation to derive the zeta potential. 4. Data Analysis: Report the Z-average diameter (mean hydrodynamic size) and the Polydispersity Index (PDI) for size. A PDI < 0.2 is generally considered monodisperse. Report the mean zeta potential and its distribution. A zeta potential more positive than +30 mV or more negative than -30 mV typically indicates good electrostatic stability.
Protocol 2: Assessing Drug Release Kinetics In Vitro
1. Principle: This experiment simulates how the active pharmaceutical ingredient is released from the nanoparticle over time in a physiologically relevant environment, a critical CQA. 2. Reagents: Nanoparticle formulation, release medium (e.g., PBS at pH 7.4, or with added surfactants to simulate sink conditions), dialysis membrane (if using dialysis method). 3. Procedure: * Setup: Place a known volume of nanoparticle suspension into a dialysis bag (MWCO appropriate to retain the nanoparticles but allow free drug diffusion). Alternatively, use a membrane-free method with continuous stirring and centrifugation at time points. * Incubation: Immerse the dialysis bag in a large volume of release medium (sink conditions) and agitate in a shaking water bath or incubator at 37°C. * Sampling: At predetermined time intervals (e.g., 0.5, 1, 2, 4, 8, 24, 48 hours), withdraw a small aliquot from the external release medium. Replace with an equal volume of fresh pre-warmed medium to maintain sink conditions. * Analysis: Quantify the amount of drug released in each sample using a validated analytical method (e.g., HPLC-UV/Vis). 4. Data Analysis: Plot the cumulative percentage of drug released versus time. Fit the data to relevant release kinetic models (e.g., zero-order, first-order, Higuchi) to understand the release mechanism.
Navigating the Regulatory Pathway for a Process Change
The following diagram outlines the logical workflow and decision points for managing a manufacturing process change under FDA regulations, integrating both technical and regulatory steps.
Leveraging FDA and International Collaborations for Regulatory Science Insights
The integration of nanotechnology into healthcare has introduced Nanotechnology-Enabled Health Products (NHPs), which promise revolutionary advancements in medical treatments and diagnostics [3]. These products are engineered materials typically within the range of 1–100 nanometers, a scale where substances exhibit unique physical, chemical, and biological properties that differ significantly from their larger-scale counterparts [3] [30]. The global regulatory landscape for these products is complex, with the U.S. Food and Drug Administration (FDA) and European Union (EU) frameworks serving as influential benchmarks for international standards [3]. For researchers and drug development professionals, navigating this evolving regulatory environment requires a solid understanding of both the scientific and compliance frameworks governing product development.
The FDA regulates a wide range of products—including foods, cosmetics, drugs, devices, veterinary products, and tobacco products—that may utilize nanotechnology or contain nanomaterials [24]. Through its participation in the National Nanotechnology Initiative (NNI), the FDA contributes to a multi-agency effort aimed at realizing the full potential of nanotechnology while supporting its responsible development [24]. The agency has established dedicated research programs, such as the Nanotechnology Core Facility (Nanocore), which focuses on building regulatory science knowledge through material characterization, detection methods, and safety studies [48]. This article provides a technical support framework to help scientific professionals address common experimental challenges and regulatory questions when developing NHPs.
Technical Support Center: FAQs & Troubleshooting Guides
Regulatory Pathway FAQs
What are the primary regulatory categories for Nanotechnology-Enabled Health Products (NHPs)? NHPs are primarily categorized based on their principal mechanism of action. A product is regulated as a medicinal product if it achieves its intended purpose through pharmacological, immunological, or metabolic (PIM) mechanisms. Conversely, products that function predominantly through physical or mechanical means are classified as medical devices, even if they incorporate PIM actions that are secondary to their primary mechanism [3]. A third category, in vitro diagnostic medical devices (IVDs), encompasses products that do not present the same technical and safety challenges as those in direct contact with the human body [3].
How is the FDA's approach to nanotechnology regulation evolving? The FDA employs a flexible, product-focused, science-based approach to regulating products involving nanomaterials [24]. The agency's "significant experience" evaluating data from comparative analytical and clinical studies has led to an evolving scientific approach [22]. For instance, recent draft guidance recognizes that comparative clinical efficacy studies are generally not as sensitive as comparative analytical assessments for demonstrating biosimilarity [22]. When comparative analytical assessment supports a demonstration of biosimilarity, "an appropriately designed human pharmacokinetic similarity study and an assessment of immunogenicity may be sufficient" to evaluate clinically meaningful differences, potentially streamlining development timelines [22].
What are the key regulatory challenges specific to nanotechnology-enabled health products? Despite advancements, nanotech still grapples with several major regulatory obstacles. Safety and Regulation concerns persist, as inhalation of airborne nanoparticles can trigger unforeseen health effects [13]. Scalability remains challenging—while lab-scale synthesis of nanorobotics is impressive, producing millions of functional units remains prohibitively expensive [13]. Additionally, Public Perception influenced by media portrayals of "grey goo" and uncontrolled nanobots requires transparent communication and third-party certifications for market acceptance [13].
Experimental Troubleshooting Guide
Inconsistent results in nanoparticle characterization?
- Problem: Variability in size measurements using Dynamic Light Scattering (DLS).
- Solution: Ensure proper sample preparation including sonication to disrupt aggregates. Use fresh buffers and control temperature consistently during measurements. Validate DLS results with a second technique such as electron microscopy.
- Prevention: Standardize synthesis protocols and implement rigorous quality control of starting materials. Characterize materials in the same biological medium used for experiments to account for protein corona effects.
Unexpected immunogenic responses to nanocarriers?
- Problem: Observed immunotoxicity in preclinical models not predicted by initial characterization.
- Solution: Conduct additional immunotoxicity studies early in development. Modify surface properties (PEGylation) to reduce immune recognition. Perform thorough characterization of protein corona formation using appropriate analytical techniques.
- Prevention: Implement comprehensive immunotoxicity screening as part of initial safety assessment. Refer to FDA Nanocore resources for specialized testing protocols [48].
Difficulty demonstrating biosimilarity for nanotherapeutic proteins?
- Problem: Uncertainty about required clinical studies for biosimilar approval.
- Solution: Consult FDA's updated guidance which states that for well-characterized products, "comparative clinical efficacy studies are generally not as sensitive as comparative analytical assessments" [22]. Focus on comprehensive analytical characterization first.
- Prevention: Early engagement with FDA through pre-IND meetings. Design a stepwise approach that prioritizes sensitive analytical methods over clinical efficacy studies where scientifically justified.
Quantitative Data on Nanotechnology Markets & Applications
Table 1: Global Nanotechnology Market Revenue by Sector (2024 Data) [13]
| Sector | 2024 Global Revenue (USD) | Maturity Level | Key Applications |
|---|---|---|---|
| Semiconductor Manufacturing | $22.1 billion | High | Chip fabrication with atomic layer deposition (ALD) and directed self-assembly (DSA) |
| Nanomedicine | $12.4 billion | High | FDA-approved nanocarriers for drug delivery and diagnostics |
| Energy & Storage | $8.9 billion | Medium-High | Silicon-nanowire anodes for advanced battery technology |
| Advanced Materials | $5.3 billion | Medium | Graphene, carbon nanotubes, and quantum dots |
Table 2: Essential Nanomaterial Research Reagents and Their Functions
| Research Reagent | Function/Application | Key Characteristics |
|---|---|---|
| Carbon Nanotubes (CNTs) | Lightweight composite panels for aerospace; conductive inks [13] | Exceptional tensile strength with high electrical conductivity |
| Graphene | Flexible printed circuits; graphene inks for smart labels and IoT sensors [13] | Single layer of carbon atoms in a hexagonal lattice with extraordinary conductivity |
| Quantum Dots | Display and imaging technologies; enhanced brightness and color gamut [13] | Semiconductor nanocrystals that emit precise wavelengths when excited |
| Liposomal Formulations | Drug delivery vehicles for controlled release [3] | PEG-coated nanoliposomes improve drug stability and reduce systemic toxicity |
| Polymeric Nanoparticles | Carriers for therapeutic genetic material [3] | Engineered to improve bioavailability while minimizing adverse effects |
| Atomic Layer Deposition (ALD) Precursors | Semiconductor manufacturing with sub-nanometer thickness control [13] | Enables precise deposition of high-k dielectric layers for advanced chips |
Experimental Protocols & Methodologies
Protocol: Physicochemical Characterization of Nanomaterials
Objective: Comprehensive characterization of key nanomaterial properties relevant to regulatory submissions.
Materials:
- Purified nanoparticle sample
- Appropriate dispersion buffers (e.g., PBS, cell culture medium)
- Dynamic Light Scattering (DLS) instrument
- Scanning Electron Microscope (SEM) or Transmission Electron Microscope (TEM)
- Zeta potential measurement system
- UV-Vis spectrophotometer
Procedure:
- Size and Size Distribution Analysis
- Prepare nanoparticle suspension at appropriate concentration (typically 0.1-1 mg/mL)
- Sonicate sample for 5-10 minutes to disrupt aggregates
- Measure hydrodynamic diameter by DLS using triple measurements at consistent temperature
- Validate using electron microscopy for primary particle size
Surface Charge Determination
- Dilute nanoparticles in 1mM KCl solution or appropriate low-conductivity buffer
- Measure zeta potential using electrophoretic light scattering
- Perform measurements at pH 7.4 and across relevant physiological range (pH 5-8)
Surface Morphology Assessment
- Prepare samples for SEM/TEM according to standard protocols
- Image multiple fields to ensure representative sampling
- Document morphology, aggregation state, and structural features
Concentration and Purity Analysis
- Use UV-Vis spectroscopy with established extinction coefficients
- Perform purity assessment using appropriate chromatographic methods if applicable
Regulatory Considerations: Document all methodology details thoroughly, including instrument calibration, sample preparation protocols, and validation procedures. FDA guidance emphasizes the importance of robust physicochemical characterization for understanding product consistency and safety [24] [48].
Protocol: In Vitro Cytotoxicity Assessment
Objective: Evaluate nanomaterial cytotoxicity using standardized assays.
Materials:
- Appropriate cell line (relevant to intended exposure route)
- Cell culture media and supplements
- Nanoparticle suspensions at various concentrations
- Cell viability assay kit (e.g., MTT, WST-8, PrestoBlue)
- Multi-well plate reader
Procedure:
- Cell Culture and Seeding
- Culture appropriate cell line under standard conditions
- Seed cells in 96-well plates at optimal density (typically 5,000-10,000 cells/well)
- Allow cells to adhere for 24 hours
Nanoparticle Exposure
- Prepare serial dilutions of nanoparticles in complete cell culture medium
- Remove existing medium from cells and replace with nanoparticle-containing medium
- Include vehicle controls and positive controls for cytotoxicity
- Incubate for 24-72 hours depending on experimental objectives
Viability Assessment
- Perform viability assay according to manufacturer's protocol
- Measure absorbance/fluorescence using plate reader
- Calculate percentage viability relative to untreated controls
Data Analysis
- Determine IC50 values using appropriate curve-fitting software
- Perform statistical analysis with appropriate replicates (minimum n=3)
Troubleshooting Note: Nanoparticles may interfere with some viability assays. Include appropriate controls to detect interference and consider using multiple assay formats to confirm results.
Visualization of Regulatory Pathways and Workflows
NHP Regulatory Pathway
Diagram 1: NHP Regulatory Pathway Overview
Material Characterization Workflow
Diagram 2: Material Characterization Workflow
The regulatory pathway for nanotechnology-enabled health products requires careful navigation of evolving frameworks and standards. By leveraging FDA and international collaborations, researchers can access valuable regulatory science insights to guide product development. The experimental protocols, troubleshooting guides, and characterization workflows provided in this technical support center address common challenges faced during NHP development. As the field continues to advance, maintaining awareness of updated guidance—such as the FDA's recent approach to biosimilarity assessments—will be essential for efficient translation of nanotechnologies from bench to bedside [22]. Through rigorous scientific characterization and early engagement with regulatory bodies, researchers can accelerate the development of safe and effective NHPs while ensuring compliance with global regulatory expectations.
Expedited Pathways and Real-World Success Stories in Nanomedicine
Frequently Asked Questions
What is the key difference between RMAT and Fast Track designations? RMAT designation is specifically for regenerative medicine therapies, including cell therapies, therapeutic tissue engineering products, and human cell and tissue products [49]. Fast Track designation is a broader expedited program for drugs and biologics that address unmet medical needs in serious conditions [50]. The evidence requirements and potential benefits, such as the ability to use accelerated approval, can differ between the pathways.
My regenerative medicine product is for a rare disease. Can I apply for both RMAT and Orphan Drug designations? Yes, and it is common for sponsors to seek multiple designations. A product targeting a rare disease can potentially qualify for Orphan Drug designation, which provides incentives like tax credits and market exclusivity, while also pursuing RMAT designation for expedited development and review if it meets the respective criteria [51]. As of September 2025, the FDA has received almost 370 RMAT designation requests and granted 184 [52].
What level of clinical evidence is required for an RMAT designation request? Preliminary clinical evidence is required to demonstrate the drug's potential to address unmet medical needs for a serious condition [49]. The FDA encourages flexibility in trial design for rare diseases, which can include the use of innovative designs, natural history data as a control (if populations are adequately matched), and patient community input on clinical endpoints [52].
What are the common reasons for an RMAT designation request being denied? A request may be denied if the investigational New Drug (IND) application is on hold during the designation review, or if the Office of Tissues and Advanced Therapies (OTAT) determines the development program does not meet the statutory criteria [49]. The FDA will provide a written rationale for the denial [49].
How does manufacturing impact an expedited designation? For regenerative medicine therapies with expedited development, maintaining chemistry, manufacturing, and controls (CMC) readiness is a unique challenge [52]. If manufacturing changes are made after receiving a designation, the product may no longer qualify if comparability with the pre-change product cannot be established [52]. The FDA recommends conducting a risk assessment for any planned changes.
Comparison of Key Expedited Development Programs
The following table summarizes the core features of three key FDA expedited programs relevant to advanced therapies like nanotechnology-enabled products.
| Feature | RMAT (Regenerative Medicine Advanced Therapy) | Fast Track | Orphan Drug |
|---|---|---|---|
| Governing Law/Origin | Section 3033 of the 21st Century Cures Act [52] | Not specified in search results | Orphan Drug Act of 1983 [51] |
| Scope / Product Type | Regenerative medicine therapies (cell therapies, therapeutic tissue engineering products, human cell and tissue products, certain gene therapies) [49] | Drugs and biologics for serious conditions [50] | Drugs and biologics for rare diseases [51] |
| Key Eligibility Criteria | - Intended for a serious condition- Preliminary clinical evidence shows potential to address unmet medical need [49] | - Intended for a serious condition- Demonstrates potential to address unmet medical need [50] | - Disease affects <200,000 in US (or is not financially viable to develop) [51] |
| Key Incentives & Benefits | Intensive FDA guidance, priority review, accelerated approval potential [52] [53] | More frequent meetings with FDA, rolling review of BLA [50] | 7-year market exclusivity, tax credits, PDUFA fee waiver [51] |
Experimental Protocols for Generating Designation Evidence
Securing an expedited designation requires robust preclinical and clinical data. Below are detailed methodologies for generating the necessary evidence.
Protocol 1: Generating Preliminary Clinical Evidence for RMAT Designation
This protocol outlines a strategy for a pilot clinical study designed to meet the "preliminary clinical evidence" requirement for RMAT designation, particularly for small populations.
- Study Design: Implement a single-arm, open-label study. For very rare diseases, consider a multi-center trial where several sites investigate the same therapy with a common manufacturing protocol, with the intent to share combined data for a future Biologics License Application (BLA) [52].
- Endpoint Selection: Engage with patient communities early to identify and validate clinical endpoints that are most relevant to them [52]. Collaborate with the FDA's Office of Therapeutic Products (OTP) to ensure these endpoints are acceptable.
- Control Strategy: In the absence of a concurrent control group, develop a well-matched historical control using rigorously collected natural history data. Ensure matching for demographics, disease state, concurrent treatments, and other relevant factors [52].
- Safety Monitoring: Establish a comprehensive safety monitoring plan that includes both short-term and long-term safety assessments. Explore the use of digital health technologies to collect real-world safety information efficiently [52].
- Data Analysis: For the primary efficacy analysis, consider a Bayesian statistical approach to quantify the evidence of a treatment effect compared to the historical control. Use the collected real-world evidence (RWE) to support the potential for accelerated approval [52].
Protocol 2: Establishing Pharmacokinetic (PK) Superiority for a Nano-Enabled Drug
This protocol describes experiments to demonstrate the enhanced PK profile of a nanotechnology-enabled drug delivery system, a common rationale for Fast Track designation.
- Formulation: The nano-formulation (e.g., liposomal, polymeric nanoparticle) and its non-nano counterpart (e.g., free drug solution) should be prepared. Key characteristics (size, zeta potential, drug loading) of the nano-formulation must be rigorously defined using techniques like Dynamic Light Scattering (DLS).
- In Vivo PK Study:
- Animal Model: Select a relevant animal model (e.g., Sprague-Dawley rats).
- Dosing & Groups: Animals are randomly divided into two groups (n=6-8/group). Group 1 receives the nano-formulation, and Group 2 receives the non-nano formulation at an equivalent dose via the intended route (e.g., intravenous injection).
- Sample Collection: Serial blood samples are collected at pre-determined time points (e.g., 5 min, 15 min, 30 min, 1, 2, 4, 8, 12, 24 hours) post-dose.
- Bioanalysis: Plasma concentrations of the drug are quantified using a validated analytical method, such as Liquid Chromatography with tandem mass spectrometry (LC-MS/MS).
- Data Analysis: Non-compartmental analysis is performed to calculate key PK parameters: Area Under the Curve (AUC), maximum concentration (Cmax), and elimination half-life [3]. Statistical analysis (e.g., unpaired t-test) is used to confirm significant improvements, such as a higher AUC and lower Cmax, indicating controlled release and improved bioavailability [3].
The Scientist's Toolkit: Research Reagent Solutions
The following table lists key materials and their functions for developing and testing advanced therapies like nano-enabled products or regenerative medicines.
| Research Reagent / Material | Function / Explanation |
|---|---|
| Polyethylene glycol (PEG) | A polymer commonly used to coat nanoliposomes (e.g., in Doxil) to improve stability, reduce immune recognition, and prolong circulation time [3]. |
| Nanoscale Particles (1-100 nm) | The core functional unit; their small size and high surface-area-to-volume ratio enable unique interactions with biological systems, such as crossing biological barriers [3] [30]. |
| AAV (Adeno-Associated Virus) Vectors | A common viral vector system used in gene therapies to deliver therapeutic genetic material to target cells [50]. |
| Mucus Penetrating Particle (MPP) | A nanotechnology platform designed to overcome mucosal barriers, used in products like ophthalmic therapies to improve drug delivery [30]. |
| Real-World Data (RWD) | Data relating to patient health status and/or the delivery of health care collected from diverse sources (e.g., electronic health records, patient registries). Analysis of RWD generates Real-World Evidence (RWE) that can support regulatory decisions [52]. |
Regulatory Pathway Relationship Diagram
The diagram below illustrates the logical relationships between different product attributes, regulatory designations, and potential outcomes.
RMAT Designation Request Workflow
This workflow maps out the specific process for submitting a request for Regenerative Medicine Advanced Therapy (RMAT) designation to the FDA.
Troubleshooting Guides & FAQs for Regulatory Submissions
Q1: What regulatory designations can accelerate the development of a therapy for rare retinal diseases?
A1: The U.S. FDA and European EMA offer several designations to expedite development and review for therapies targeting conditions with high unmet medical need. The table below summarizes the key designations secured by MCO-010.
Table: FDA and EMA Regulatory Designations for MCO-010
| Regulatory Body | Designation Type | Indication/Coverage | Key Benefits |
|---|---|---|---|
| U.S. FDA | Regenerative Medicine Advanced Therapy (RMAT) | Stargardt disease (SD) [54] [55] | Accelerated development and review, flexibility in trial design [54] [56] |
| U.S. FDA | Fast Track | Retinitis Pigmentosa (RP) and Stargardt disease (SD) [54] [57] | Opportunities for accelerated development and review [54] |
| U.S. FDA | Orphan Drug | Retinitis Pigmentosa (RP) and Stargardt disease (SD) [54] [57] | 7 years of market exclusivity upon approval [54] [56] |
| European EMA | Orphan Medicinal Product | Five categories: non-syndromic & syndromic rod- and cone-dominant dystrophies, and macular dystrophies [54] [55] | Protocol assistance, up to 10 years of market exclusivity [54] [56] |
Q2: We are preparing a Biologics License Application (BLA). What submission strategy can facilitate earlier FDA feedback?
A2: The FDA may grant a Rolling Review for a BLA, allowing a company to submit completed sections of the application for review without waiting for all modules to be finished. This can significantly expedite the overall review timeline. Nanoscope initiated a rolling BLA submission for MCO-010 in RP in July 2025, with full submission anticipated in early 2026 [57] [58].
Experimental Protocol: Navigating a Rolling BLA Submission
- Pre-Submission Meeting: Engage with the FDA to discuss the possibility of a rolling review and agree on the submission schedule and content [59].
- Module Submission: Submit completed modules (e.g., non-clinical, clinical, quality) sequentially according to the agreed timeline [57].
- Interactive Review: The FDA reviews submitted modules and provides feedback while the company prepares the remaining sections.
- Final Submission and Review Clock: The FDA's priority review clock (typically 6 months) begins only after the complete application is submitted [57].
Q3: Our therapy is "disease-agnostic." How can we define its regulatory pathway?
A3: A broad, disease-agnostic regulatory path can be established by securing designations that cover a spectrum of related conditions. MCO-010's five EMA Orphan designations, which cover a wide range of retinal dystrophies, provide a precedent for a regulatory strategy that is not tied to a single disease entity [54] [55]. This creates a potential pathway for dozens of retinal conditions involving photoreceptor loss under a single therapy.
The clinical development of MCO-010 is supported by data from multiple trials. The tables below summarize the key efficacy and safety results.
Table: Efficacy Data from Clinical Trials of MCO-010
| Trial Name | Phase | Disease | Key Efficacy Endpoint | Result |
|---|---|---|---|---|
| RESTORE [57] | 2b | Retinitis Pigmentosa (RP) | Improvement in Best Corrected Visual Acuity (BCVA) at 52 weeks | >0.3 LogMAR (equivalent to ≥3 lines on an eye chart) vs. sham-control |
| REMAIN [59] | Long-term Follow-up | Retinitis Pigmentosa (RP) | Durability of BCVA improvement | Vision gains retained for 3 years post-injection |
| STARLIGHT [54] [55] | 2 | Stargardt disease (SD) | Vision improvement | Promising results and measurable vision improvements observed |
Table: Safety Profile of MCO-010 from Clinical Trials
| Trial Name | Phase | Disease | Reported Safety Findings |
|---|---|---|---|
| RESTORE & Long-term Follow-up [57] | 2b & 3-year follow-up | Retinitis Pigmentosa (RP) | No serious adverse events reported in treated eyes |
| STARLIGHT [59] | 2 | Stargardt disease (SD) | No major safety issues reported |
Experimental & Regulatory Pathway Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table: Key Materials and Reagents for Optogenetic Gene Therapy Development
| Reagent / Material | Function in Development & Analysis |
|---|---|
| Adeno-Associated Virus (AAV) Vector | Serves as the delivery vehicle (vector) to transport the therapeutic gene into target cells. MCO-010 uses an AAV2 vector [58]. |
| Multi-Characteristic Opsin (MCO) Gene | The therapeutic transgene that codes for a light-sensitive protein. This is the active component that restores light sensitivity to retinal cells [54] [57]. |
| Cell Lines (e.g., HEK293) | Used for the production and titration of AAV vectors in a laboratory setting. |
| Animal Models of Retinal Degeneration | Essential for preclinical proof-of-concept and safety studies before human trials. |
| Immunoassay Kits (e.g., ELISA) | Critical for assessing the immune response to the vector and transgene product in preclinical and clinical studies. |
| Polymerase Chain Reaction (PCR) Assays | Used to detect and quantify vector DNA, evaluating biodistribution and persistence. |
| Electroretinography (ERG) | A key functional assay to measure electrical responses of various retinal cell types, including light-sensitivity, in animal models and patients. |
Nanotechnology-Enabled Health Products (NHPs) represent a revolutionary advancement in modern medicine, offering new possibilities for diagnosis, treatment, and drug delivery. These products leverage unique properties of nanomaterials, typically ranging from 1-100 nanometers, which exhibit distinct chemical, physical, and biological characteristics compared to their larger-scale counterparts [3]. The global nanotechnology drug delivery market, valued at $97.98 billion in 2024 and projected to reach $231.7 billion by 2035, demonstrates the significant economic and therapeutic potential of these technologies [60].
However, the regulatory landscape for NHPs remains complex and continually evolving. In the United States, the Food and Drug Administration (FDA) oversees NHPs through a product-focused, science-based approach that considers the specific characteristics and applications of nanotechnology across various product categories [24]. In the European Union, the European Medicines Agency (EMA) operates within a framework established by Directive 2001/83/EC, which defines medicinal products and their regulatory requirements [3]. Both regulatory bodies face challenges in assessing the safety, efficacy, and quality of NHPs due to their unique properties and behaviors, leading to ongoing adaptations of regulatory science and guidelines [61].
Comparative Analysis: US FDA vs. EU EMA Regulatory Approaches
Key Similarities and Differences in Regulatory Philosophies
The FDA and EMA share common goals of ensuring patient safety and product efficacy but employ different regulatory strategies and frameworks. The FDA utilizes a flexible, product-focused approach that applies existing statutory authorities to NHPs based on their specific product category (drug, device, biologic, etc.) [24]. The agency participates in the National Nanotechnology Initiative (NNI) to coordinate multi-agency efforts in nanoscale science, engineering, and technology [24]. Conversely, the EMA operates under a more centralized medicines regulation framework with specific directives defining medicinal products and their requirements [3]. Both regulators emphasize science-based assessment and international collaboration, but the EU tends toward more explicit regulatory definitions and requirements for nanomaterials [3].
Regulatory Classification and Definitions
Table 1: Comparison of Regulatory Definitions and Classifications
| Aspect | US FDA Approach | EU EMA Approach |
|---|---|---|
| Core Definition | Flexible, product-focused approach; no universal regulatory definition of nanotechnology [24] | Moving toward a holistic governance approach; generally accepts 1-100 nm size range [62] [3] |
| Legal Basis | Food, Drug, and Cosmetic Act; Authority varies by product category [24] | Directive 2001/83/EC; Definition in Article 1(2) [3] |
| Categorization | Based on primary mode of action; categorized as drugs, devices, biologics, or combinations [24] | Primarily as medicinal products or medical devices based on principal mechanism of action [3] |
| Guidance Documents | Several product-specific guidance documents issued [19] | Framework established through EU regulations and scientific guidelines |
Approval Pathways and Requirements
Table 2: Approval Pathways and Key Requirements
| Parameter | US FDA | EU EMA |
|---|---|---|
| Marketing Authorization | Pathway depends on product classification (e.g., NDA, BLA, PMA) | Centralized, decentralized, or national procedures depending on product |
| Safety Assessment | Requires nanotechnology-specific characterization; case-by-case basis [24] | Comprehensive quality, safety, and efficacy data; may require nano-specific studies [3] |
| Manufacturing Controls | Current Good Manufacturing Practices (cGMP) with nano-specific considerations | Good Manufacturing Practice (GMP) with detailed characterization requirements |
| Pharmacovigilance | Post-market monitoring and reporting requirements | Risk Management Plan and additional monitoring possible for NHPs |
| Technical Documentation | Extensive characterization data including physicochemical properties [19] | Quality, non-clinical, and clinical data per EU requirements; nano-specific details [3] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for NHP Development
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Reference Nanomaterials | Provide benchmark materials for method validation and comparison studies [62] | Limited availability for some material types; critical for assay standardization |
| Lipids (for Liposomes) | Form biocompatible nanocarriers for drug delivery [3] [60] | Quality and purity affect encapsulation efficiency and stability |
| Biodegradable Polymers (e.g., PLGA) | Create sustainable drug delivery systems that degrade into safe byproducts [60] | Molecular weight and composition control release kinetics |
| Surface Modification Agents | Functionalize nanoparticles for targeting, stealth properties, or stability [3] | Impact biological identity, corona formation, and clearance mechanisms |
| Characterization Standards | Enable accurate measurement of size, surface charge, and composition [62] | Essential for regulatory compliance; require validated methods |
Troubleshooting Guides and FAQs: Addressing Common Regulatory Challenges
FAQ 1: How do I determine if my product is considered a "nanomaterial" for regulatory purposes?
Answer: Regulatory definitions vary between regions. The EU employs a more formal definition, generally accepting the 1-100 nanometer size range, though certain legal definitions may require additional properties [62]. The FDA maintains a more flexible, product-specific approach without a universal regulatory definition [24]. Regardless of formal definitions, if your material exhibits properties or phenomena attributable to its nanoscale dimensions, you should characterize it as a nanomaterial and consult relevant guidance documents [19]. Early engagement with regulators is recommended to determine applicable requirements.
FAQ 2: What are the most critical characterization parameters for NHPs?
Answer: Comprehensive physicochemical characterization is fundamental for NHP development. Key parameters include:
- Size and size distribution using dynamic light scattering (DLS) and electron microscopy
- Surface characteristics including charge (zeta potential), area, and functionality
- * morphology and structure* using appropriate imaging techniques
- Composition and purity including elemental analysis and contamination assessment
- Stability under relevant storage conditions and in biological media [62] [3] These parameters significantly influence biological behavior, safety, and efficacy, and are essential for both regulatory submissions and quality control.
FAQ 3: How do I address the challenge of biocompatibility and nanotoxicology assessment?
Answer: Traditional toxicity testing methods may require adaptation for nanomaterials. Key considerations include:
- Dosimetry adjustments to account for particle-specific effects rather than just mass-based concentration
- Characterization in biological media as nanomaterials interact with proteins and form coronas
- Assessment of translocation potential across biological barriers [62]
- Evaluation of unique nano-specific properties that may influence toxicological profiles The OECD's Working Party on Manufactured Nanomaterials (WPMN) has developed nano-specific test guidelines that provide important methodological frameworks [62]. Additionally, alternative test methods are gaining importance as regulatory testing moves away from animal testing, though these methods often require validation for nanomaterials [62].
FAQ 4: What are the key differences in regulatory data requirements between FDA and EMA?
Answer: While both agencies require comprehensive data packages, some notable differences exist:
- The FDA emphasizes a case-by-case approach based on the specific product characteristics and intended use [24]
- The EMA typically requires extensive physicochemical characterization following defined guidelines
- Manufacturing process controls may have different emphasis between the agencies
- Non-clinical testing strategies may vary in specific study requirements Despite these differences, both agencies increasingly recognize the importance of international harmonization and collaborate through forums like the International Council for Harmonisation [4].
Experimental Protocols for Critical Characterization Studies
Protocol 1: Comprehensive Physicochemical Characterization of NHPs
Objective: To systematically characterize key physicochemical parameters of nanotechnology-enabled health products for regulatory submissions.
Materials and Equipment:
- Purified NHP sample
- Dynamic Light Scattering (DLS) instrument
- Zeta potential analyzer
- Electron microscopy (SEM/TEM) with sample preparation supplies
- UV-Vis spectrophotometer
- FTIR spectrometer
- Batch-specific relevant biological media
Methodology:
- Sample Preparation: Prepare NHP suspensions according to intended administration route. Use appropriate buffers and ensure homogeneous dispersion.
- Size and Size Distribution Analysis: Perform DLS measurements in triplicate at relevant concentrations. Confirm results with electron microscopy for morphology assessment.
- Surface Charge Determination: Measure zeta potential in appropriate physiological buffers across a pH range relevant to biological environments.
- Surface Chemistry Analysis: Employ FTIR and XPS to characterize functional groups and surface modifications.
- Stability Assessment: Monitor size, PDI, and zeta potential over time under storage conditions and in biologically relevant media.
- Documentation: Record all methodology details, including instrument settings, sample preparation protocols, and environmental conditions.
Regulatory Application: This characterization protocol provides essential quality data for CTD sections 3.2.S.2.2 (Pharmaceutical Development) and 3.2.S.3.1 (Elucidation of Structure and Characteristics) for EMA submissions, and corresponding sections in FDA applications [3].
Protocol 2: Assessment of NHP Stability in Biological Media
Objective: To evaluate the behavior and stability of NHPs in biologically relevant media, simulating in vivo conditions.
Materials and Equipment:
- NHP sample
- Relevant biological media (plasma, serum, simulated gastric/intestinal fluid)
- Ultracentrifuge with appropriate rotors
- Dialysis membranes (various MWCO)
- DLS and zeta potential instruments
- TEM with negative staining capabilities
- Protein quantification assay kits
Methodology:
- Media Preparation: Source appropriate biological media matching intended exposure route.
- Incubation Studies: Incubate NHPs in media at 37°C with gentle agitation. Collect samples at predetermined time points (e.g., 0, 1, 4, 24 hours).
- Protein Corona Analysis: Separate NHP-protein complexes via centrifugation or size exclusion chromatography. Analyze corona composition using proteomic techniques or SDS-PAGE.
- Colloidal Stability Assessment: Measure size distribution, PDI, and zeta potential changes over time.
- Morphological Evaluation: Examine particles after media exposure using TEM to detect aggregation or structural changes.
- Data Interpretation: Correlate stability findings with potential in vivo behavior and pharmacokinetics.
Regulatory Significance: This protocol addresses FDA guidance recommending understanding of NHP behavior in biological systems [19] and EMA requirements for comprehensive characterization [3].
Visualization of Regulatory Pathways and Experimental Workflows
NHP Regulatory Pathway Decision Algorithm
Essential NHP Characterization Workflow
Technical Support Center: Troubleshooting Guides and FAQs for Regulatory Science
This technical support center provides troubleshooting guides and frequently asked questions (FAQs) to assist researchers, scientists, and drug development professionals in navigating the complex regulatory pathways for nanotechnology-enabled health products (NHPs). The content is framed within the context of a broader thesis on regulatory science, leveraging FDA research and international regulatory frameworks to address specific issues encountered during experiments and product development.
Frequently Asked Questions (FAQs)
FAQ 1: What is the FDA's current position on the regulatory status of nanomaterials in products?
The FDA participates in the National Nanotechnology Initiative (NNI), a U.S. Government R&D program, and employs a flexible, product-focused, and science-based approach for regulating products that contain nanomaterials or use nanotechnology [24]. The agency considers that nanomaterials may have different chemical, physical, or biological properties from their larger-scale counterparts, which must be considered in safety assessments [24] [31].
FAQ 2: How does the FDA define a nanotechnology product?
While the FDA has not adopted a single formal definition, it generally considers two key points for identification:
- Whether an engineered material or end product has at least one dimension in the nanoscale range (approximately 1 nm to 100 nm).
- Whether an engineered material or end product exhibits properties or phenomena (physical, chemical, or biological effects) attributable to its dimension(s), even if these dimensions fall outside the nanoscale range, up to one micrometer [31].
FAQ 3: Where can I find specific FDA guidance documents for my nanomedicine product?
FDA guidance documents are accessible through the agency's online search portal. You can search using keywords (e.g., "nanotechnology," "nanomaterial") and filter results by product area (e.g., drugs, biologics, devices, cosmetics, food), date, and FDA organization [4]. For products that do not fit neatly into existing categories, early engagement with the FDA via pre-submission meetings is highly recommended.
FAQ 4: What are the critical regulatory science challenges for Nanotechnology-Enabled Health Products (NHPs)?
A primary challenge is the complex and sometimes lagging regulatory framework, which can create barriers to clinical application [3]. Key issues include:
- Categorizing products based on their primary mode of action (pharmacological, immunological, metabolic, or physical/mechanical) [3].
- Addressing the unique physicochemical properties of nanomaterials (e.g., increased surface area, surface energy) that influence their safety and performance [3].
- Developing and validating specific testing methods suitable for nanomaterials, as traditional methods may not be adequate [31].
FAQ 5: What are the emerging international trends in regulatory science for NHPs?
Regulatory science is increasingly global. The FDA actively participates in international forums to share perspectives and information on nanotechnology regulation [24]. A major trend is digital transformation, as highlighted by the recent Global Summit on Regulatory Science (GSRS24), which focused on leveraging digital technologies to enhance regulatory applications [63]. Furthermore, the European Union and U.S. frameworks often serve as global benchmarks, making understanding their similarities and differences crucial for international product development [3].
Troubleshooting Guide: Common Experimental Hurdles in NHP Characterization
Issue 1: Inconsistent or Poorly Reproducible Nanoparticle Characterization Data
- Problem: Measurements of size, charge (zeta potential), or dispersion state vary significantly between batches or testing sessions.
- Potential Cause: Inadequate purification, aggregation/agglomeration during storage, or non-optimized characterization parameters.
- Solution:
- Standardize Sample Preparation: Implement strict protocols for buffer exchange, filtration, and sonication.
- Control Environmental Factors: Regulate temperature and pH during measurements, as both critically influence nanoparticle behavior.
- Validate Instrumentation: Use standardized reference materials (e.g., latex beads of known size) to calibrate instruments like Dynamic Light Scattering (DLS) or Nanoparticle Tracking Analysis (NTA).
- Utilize Orthogonal Methods: Confirm results using multiple techniques (e.g., corroborate DLS data with Electron Microscopy).
Issue 2: Unexpected Toxicity or Immunogenic Response in Biological Assays
- Problem: In vitro or in vivo studies show cytotoxicity or immune activation not predicted from the bulk material.
- Potential Cause: The unique physicochemical properties of the nanomaterial, such as high surface reactivity, catalytic activity, or the presence of impurities from synthesis (e.g., residual solvents, metals).
- Solution:
- Thorough Material Characterization: Before biological testing, fully characterize the nanomaterial's size, shape, surface charge, composition, and surface chemistry [3]. This data is essential for understanding structure-activity relationships.
- Implement a Rigorous Toxicology Screen: Follow FDA-recommended testing, which may include assessments for acute toxicity, skin irritation, mutagenicity/genotoxicity, and repeated dose (90-day) toxicity [31].
- Test in Relevant Biological Media: Assess how the nanoparticle interacts with proteins (formation of a "protein corona") in physiologically relevant fluids, as this can alter its biological identity and effects.
Issue 3: Difficulty in Demonstrating Bioavailability or Biodistribution Changes
- Problem: Unable to conclusively show that the nano-formulation alters the pharmacokinetics (e.g., AUC, Cmax) or tissue distribution of an active compound compared to its non-nano counterpart.
- Potential Cause: Insensitive analytical methods, lack of a proper control, or instability of the nano-formulation in vivo.
- Solution:
- Use Radiolabels or Fluorescent Tags: Incorporate traceable labels into the nanoparticle or its payload for sensitive and quantitative tracking.
- Employ Advanced Imaging Techniques: Utilize modalities like PET, SPECT, or fluorescence imaging to visualize real-time distribution.
- Conduct Comparative Pharmacokinetic Studies: Design rigorous studies that directly compare the nano-formulation to the conventional formulation in appropriate animal models, measuring key parameters like half-life, clearance, and volume of distribution [3].
Experimental Protocols and Data Presentation
Protocol 1: Basic Physicochemical Characterization of Nanomaterials for Regulatory Submissions
This protocol outlines a foundational set of experiments to characterize nanomaterials, a critical first step referenced in FDA considerations [31] and regulatory science reviews [3].
- Sample Preparation: Prepare a minimum of three independent batches of the nanomaterial. Disperse in a relevant suspension medium (e.g., water, PBS, cell culture media) using a defined sonication protocol (e.g., power, time).
- Size and Size Distribution (Polydispersity Index, PDI):
- Method: Dynamic Light Scattering (DLS).
- Procedure: Measure the hydrodynamic diameter and PDI at a standard temperature (e.g., 25°C) with a fixed angle. Perform a minimum of 3-5 measurements per batch.
- Surface Charge (Zeta Potential):
- Method: Electrophoretic Light Scattering.
- Procedure: Measure zeta potential in a standardized electrolyte solution (e.g., 1mM KCl) at neutral pH. Conduct a minimum of 3-5 measurements per batch.
- Morphology and Elementary Composition:
- Method: Electron Microscopy (Scanning SEM or Transmission TEM) coupled with Energy Dispersive X-ray Spectroscopy (EDS).
- Procedure: Deposit a diluted sample suspension on a grid, allow to dry, and image. Use EDS for elemental analysis.
- Surface Chemistry and Functional Groups:
- Method: Fourier-Transform Infrared Spectroscopy (FTIR) or X-ray Photoelectron Spectroscopy (XPS).
- Procedure: Prepare a thin film or pellet of the nanomaterial and analyze across a standard wavenumber range (e.g., 4000-400 cm⁻¹ for FTIR).
Summary of Key Characterization Parameters and Methods
| Parameter | Recommended Analytical Technique | Target Data for Regulatory Dossiers |
|---|---|---|
| Hydrodynamic Size | Dynamic Light Scattering (DLS) | Mean diameter, Polydispersity Index (PDI) |
| Particle Morphology | Electron Microscopy (TEM/SEM) | High-resolution images, shape description |
| Surface Charge | Zeta Potential Measurement | Average zeta potential (mV) in relevant media |
| Elemental Composition | Energy Dispersive X-Ray Spectroscopy (EDS) | Elemental mapping and composition percentage |
| Crystallinity | X-Ray Diffraction (XRD) | Crystalline phase identification |
| Surface Chemistry | Fourier-Transform Infrared Spectroscopy (FTIR) | Identification of functional groups |
Protocol 2: In Vitro Cytotoxicity Assessment per Regulatory Expectations
This protocol aligns with the basic test battery recommended by the FDA for a preliminary safety assessment of nanomaterials, particularly for products like cosmetics that may use nanotechnology [31].
- Cell Line Selection: Use at least two relevant mammalian cell lines (e.g., THP-1 monocytes and HepG2 hepatocytes).
- Nanomaterial Dispersion: Prepare a stock dispersion of the nanomaterial in cell culture medium (with serum). Sonicate briefly to minimize aggregation. Serial dilute to create a range of concentrations.
- Exposure and Incubation: Plate cells and allow to adhere overnight. Expose cells to the nanomaterial concentrations for 24 and 48 hours. Include a negative control (medium only) and a positive control (e.g., Triton X-100).
- Viability Endpoint Measurement:
- Assay 1: Metabolic Activity (MTS/MTT Assay): Measure the reduction of MTS tetrazolium compound to formazan by metabolically active cells. Record absorbance at 490nm.
- Assay 2: Membrane Integrity (LDH Assay): Measure the release of lactate dehydrogenase from cells with damaged membranes. Record absorbance at 490nm.
- Data Analysis: Calculate cell viability as a percentage of the negative control. Determine the half-maximal inhibitory concentration (IC₅₀) using non-linear regression analysis.
Visualization of Regulatory Pathways and Workflows
NHP Regulatory Pathway Decision Tree
NHP Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for NHP Characterization and Regulatory Testing
| Research Reagent / Material | Function in NHP Development |
|---|---|
| Standard Reference Nanomaterials (e.g., NIST Gold Nanoparticles) | Used for instrument calibration and as controls in method validation to ensure measurement accuracy and reproducibility. |
| Cell-Based Toxicology Assay Kits (e.g., MTS, LDH, Caspase-Glo) | Provide standardized, reproducible methods for assessing cytotoxicity, cell viability, and apoptosis induction as part of the preliminary safety battery [31]. |
| Dynamic Light Scattering (DLS) Instrument | Measures the hydrodynamic diameter and size distribution (polydispersity) of nanoparticles in suspension, a fundamental physicochemical parameter. |
| Differentiated THP-1 Macrophage Cells | A relevant in vitro model for assessing nanomaterial immune activation, cytokine release, and cellular uptake, which are critical for understanding potential immunogenic effects. |
| Simulated Biological Fluids (e.g., Simulated Gastric Fluid, Plasma) | Used to study the stability, aggregation, and protein corona formation of nanomaterials in physiologically relevant environments, informing bioavailability and safety. |
| HPLC Systems with UV/Vis & MALS Detectors | Essential for analyzing the chemical purity, stability, and drug release kinetics of nanomedicines, providing critical data for chemistry, manufacturing, and controls (CMC) sections of regulatory dossiers. |
FDA's Regulatory Approach to Nanotechnology
The U.S. Food and Drug Administration (FDA) regulates nanotechnology products under its existing statutory authorities, using a product-focused, science-based policy [2] [1]. The agency does not categorically judge nanotechnology as inherently safe or harmful and considers the specific characteristics and effects of nanomaterials in the biological context of each product and its intended use [2] [1].
Key Regulatory Principles
- Adaptive and Flexible Approach: FDA's technical assessments are product-specific, taking into account the effects of nanomaterials in the particular biological and mechanical context of each product and its intended use [1]
- Varied Legal Standards: FDA respects variations in legal standards for different product classes, which may lead to divergent regulatory outcomes for different applications even when objective risk measures are similar [1]
- Premarket Review Integration: Where premarket review authority exists, attention to nanomaterials is being incorporated into standing procedures [1]
- Encouraged Consultations: FDA strongly encourages manufacturers to consult with the agency early in the product development process to address questions related to safety, effectiveness, or regulatory status [2] [1]
Frequently Asked Questions: Regulatory Pathways
Q: What is the foundational policy basis for FDA's approach to nanotechnology? A: FDA's regulatory approach stems from the 2007 Nanotechnology Task Force Report, which provided recommendations to better enable the agency to evaluate safety aspects of FDA-regulated products containing nanoscale materials [2].
Q: Are there specific guidance documents for nanotechnology products? A: Yes, FDA has issued several guidance documents on topics relating to application of nanotechnology in FDA-regulated products. These represent FDA's current thinking on the topic and are available on FDA's website [2] [19].
Q: How does FDA handle products not subject to premarket review? A: For products not subject to mandatory premarket review (such as dietary supplements and cosmetics), FDA encourages consultation before marketing, relies on publicly available or voluntarily submitted information, adverse event reporting, and post-market surveillance activities [1].
Q: What are the key differences between EU and US regulatory frameworks for NHPs? A: Both systems are influential global benchmarks. In the EU, the European Commission provides the foundational legal framework, while in the US, the FDA is the enforcing body for critical health product legislation [3] [64].
Troubleshooting Common Regulatory Challenges
Challenge: Determining When a Product Involves Nanotechnology
Issue: Researchers often struggle to determine whether their product will be considered to involve nanotechnology application.
Solution: FDA outlines points to consider when determining if a product involves nanotechnology application. Key criteria include whether the product has material within the nanoscale range (1nm to 100nm) or whether the product is engineered to exhibit unique properties due to its dimensions [65].
Challenge: Safety Assessment of Nanomaterials
Issue: Standard safety assessment protocols may not adequately address nanomaterial-specific concerns.
Solution: Consult FDA guidance documents specific to product categories and engage in early discussions with the agency. FDA emphasizes that industry remains responsible for ensuring products meet all applicable legal requirements, including safety standards, regardless of the emerging nature of the technology [2] [1].
Experimental Protocols for Regulatory Submission
Physicochemical Characterization Protocol
Comprehensive characterization is fundamental for regulatory submissions of nanotechnology-enabled products. The following parameters should be characterized based on ISO standards and regulatory expectations [65]:
Essential Characterization Parameters:
| Parameter | Method | Significance |
|---|---|---|
| Dimensions and granulometric distribution | Dynamic Light Scattering (DLS), Field Flow Fractionation (FFF) | Determines size distribution and aggregation state |
| Shape | Electron microscopy | Affects cellular uptake and biodistribution |
| Specific surface area | BET analysis | Influences reactivity and dose estimation |
| Surface charge | Zeta potential measurement | Predicts colloidal stability and biological interactions |
| Composition and purity | Mass spectrometry, chromatography | Ensures product quality and batch consistency |
| Crystalline Structure | X-ray diffraction | Affects physicochemical properties and stability |
| Level of crystallinity | Differential scanning calorimetry | Impacts dissolution rate and stability |
| Coatings and surface composition | X-ray photoelectron spectroscopy | Determines surface functionality and behavior |
Regulatory Decision Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Key Characterization Tools and Their Functions
| Tool/Reagent | Function | Application Context |
|---|---|---|
| Dynamic Light Scattering (DLS) | Measures hydrodynamic size distribution | Determining particle size and aggregation state in solution |
| Nanoparticle Tracking Analysis (NTA) | Provides number-based size distribution and concentration | Quantitative analysis of nanoparticles in biological fluids |
| Field Flow Fractionation (FFF) | Separates nanoparticles by size and mass | High-resolution sizing of complex nanomaterial mixtures |
| Resonant Mass Measurement (RMM) | Measures buoyant mass of individual particles | Counting and sizing nanoparticles in complex media |
| Atomic Layer Deposition (ALD) | Deposits precise thin films with atomic-level control | Creating uniform coatings on nanoscale structures |
| Zeta Potential Analyzer | Measures surface charge and stability | Predicting colloidal stability and biological behavior |
| BET Surface Area Analyzer | Determines specific surface area | Calculating surface-area-to-volume ratios for dose metrics |
| Electron Microscopy | Visualizes nanomaterial morphology and structure | Direct observation of size, shape, and surface characteristics |
Common Experimental Issues and Solutions
Problem: Inconsistent Characterization Results
Symptoms: Variable size measurements between batches, conflicting data from different techniques.
Root Cause: Inadequate sample preparation, technique limitations, or material instability.
Solution:
- Use orthogonal characterization methods (e.g., combine DLS with NTA or electron microscopy)
- Standardize sample preparation protocols across batches
- Validate methods with appropriate controls and reference materials
Problem: Regulatory Classification Uncertainty
Symptoms: Difficulty determining whether product qualifies as a drug, device, or combination product.
Root Cause: Complex mode of action involving both pharmacological and physical mechanisms.
Solution:
- Conduct thorough mode of action studies early in development
- Request a classification determination from FDA
- Consider precedent products with similar technological characteristics
Experimental Workflow for Nanotechnology Product Development
The successful development and regulatory approval of nanotechnology products requires careful attention to characterization, safety assessment, and early regulatory engagement. By following established protocols and leveraging lessons from approved products, researchers can navigate the regulatory pathway more effectively and bring innovative nanotechnologies to patients who need them.
Conclusion
Successfully navigating the FDA's regulatory pathways for nanotechnology products requires a deep understanding of its adaptive, product-specific, and science-based framework. Key takeaways include the necessity of early and continuous engagement with the agency, meticulous attention to the unique properties of nanomaterials in safety assessments, and strategic use of expedited programs for high-unmet-need therapies. As demonstrated by real-world successes, robust regulatory science and transparent communication are paramount. Looking ahead, the FDA's continued investment in nanotechnology regulatory science, coupled with growing international regulatory experience, promises a more predictable pathway for innovators. This evolution will further accelerate the translation of groundbreaking nanotechnologies from the laboratory to clinical applications, ultimately advancing patient care and public health.
References
- 1. FDA's Approach to Regulation of Nanotechnology Products [https://www.fda.gov/science-research/nanotechnology-programs-fda/fdas-approach-regulation-nanotechnology-products]
- 2. Nanotechnology Fact Sheet [https://www.fda.gov/science-research/nanotechnology-programs-fda/nanotechnology-fact-sheet]
- 3. Regulatory pathways and guidelines for nanotechnology ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1544393/full]
- 4. Search for FDA Guidance Documents [https://www.fda.gov/regulatory-information/search-fda-guidance-documents]
- 5. Considerations for Drug Products that Contain Nanomaterials [https://www.fda.gov/drugs/cder-small-business-industry-assistance-sbia/considerations-drug-products-contain-nanomaterials]
- 6. Considering Whether an FDA-Regulated Product Involves ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considering-whether-fda-regulated-product-involves-application-nanotechnology]
- 7. 25 years of research and regulation: Is nanotechnology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12286942/]
- 8. Nanomaterials in Medical Devices [https://namsa.com/resources/blog/nanomaterials-medical-devices-biocompatibility-considerations/]
- 9. Nanotechnology Safety Resources [https://www.acs.org/about/governance/committees/chemical-safety/publications-resources/nanotechnology-safety-resources.html]
- 10. Drug Products, Including Biological Products, that Contain ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/drug-products-including-biological-products-contain-nanomaterials-guidance-industry]
- 11. FDA Medical Device Classification: Class I, II, III Explained ... [https://www.complizen.ai/post/fda-medical-device-classification-complete-guide-to-class-i-ii-iii-devices]
- 12. De Novo Classification Request [https://www.fda.gov/medical-devices/premarket-submissions-selecting-and-preparing-correct-submission/de-novo-classification-request]
- 13. Current State of Nanotechnology in 2025 - How Advanced Is It? [https://hsocialcreator.in/current-state-of-nanotechnology-in-2025-how-advanced-is-it]
- 14. Nanomedicine FDA : Regulations and Global Strategies Guidance [https://bla-regulatory.com/fda-nanomedicine-regulations/]
- 15. Safety: Food Should Strengthen Its Oversight of FDA ... | U.S. GAO Food [https://www.gao.gov/products/gao-10-246]
- 16. Product-Specific Guidances for Generic Drug Development [https://www.fda.gov/drugs/guidances-drugs/upcoming-product-specific-guidances-generic-drug-product-development]
- 17. Nanotechnology Task Force Report 2007 [https://www.fda.gov/science-research/nanotechnology-programs-fda/nanotechnology-task-force-report-2007]
- 18. Regulation of nanotechnology: Are we doing enough? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2676667/]
- 19. Nanotechnology Guidance Documents [https://www.fda.gov/science-research/nanotechnology-programs-fda/nanotechnology-guidance-documents]
- 20. QMS Information for Certain PMA Reviews Draft Guidance [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/quality-management-system-information-certain-premarket-submission-reviews]
- 21. Statement By John Bailey, EVP For Science CTFA On FDA ... [https://www.personalcarecouncil.org/newsroom/statement-by-john-bailey-evp-for-science-ctfa-on-fda-nanotechnology-report/]
- 22. New FDA Guidance Aims To Simplify The Biosimilar ... [https://www.mondaq.com/unitedstates/life-sciences-biotechnology-nanotechnology/1707226/new-fda-guidance-aims-to-simplify-the-biosimilar-approval-process]
- 23. FDA Issues Notice Of Intent To Rescind Rule Extending ... [https://www.mondaq.com/unitedstates/life-sciences-biotechnology-nanotechnology/1669832/fda-issues-notice-of-intent-to-rescind-rule-extending-authority-to-laboratory-developed-tests]
- 24. Nanotechnology Programs at FDA [https://www.fda.gov/science-research/science-and-research-special-topics/nanotechnology-programs-fda]
- 25. Guidance for Industry: Safety of Nanomaterials in Cosmetic ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-safety-nanomaterials-cosmetic-products]
- 26. Development of Pharmaceutical Nanomedicines [https://pmc.ncbi.nlm.nih.gov/articles/PMC8777701/]
- 27. FDA seeks public comment on monitoring strategies for AI ... [https://www.hoganlovells.com/en/publications/fda-seeks-public-comment-on-monitoring-strategies]
- 28. FDA AI Guidance 2025: What Life Sciences Must Do Now [https://usdm.com/resources/blogs/fda-ai-guidance-2025-life-sciences-compliance]
- 29. Targeted Postmarket Surveillance: The Way Toward ... [https://paragoninstitute.org/private-health/targeted-postmarket-surveillance-the-way-toward-responsible-ai-innovation-in-health-care/]
- 30. Nanotechnology: The vision of 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4131398/]
- 31. FDA Issues Nanotech Draft Guidances [https://www.supplysidesj.com/supplement-regulations/fda-issues-nanotech-draft-guidances]
- 32. Is It Really 'FDA Approved'? [https://www.fda.gov/consumers/consumer-updates/it-really-fda-approved]
- 33. Physicochemical Properties of Nanomaterials: Implication ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4140132/]
- 34. Nanoparticle classification, physicochemical properties ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01477-8]
- 35. Challenges in Development of Nanoparticle-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326161/]
- 36. Nanoparticles‐induced potential toxicity on human health [https://pmc.ncbi.nlm.nih.gov/articles/PMC10349198/]
- 37. Comprehensive insights into mechanism of nanotoxicity ... [https://link.springer.com/article/10.1186/s11671-024-04118-1]
- 38. A review on toxicity mechanism and risk factors of ... [https://www.sciencedirect.com/science/article/abs/pii/S0300483X24000623]
- 39. Ethical and Scientific Issues of Nanotechnology in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1817662/]
- 40. A Step Closer to the Proposed End of the Self-Affirmed ... [https://www.healthlawadvisor.com/a-step-closer-to-the-proposed-end-of-the-self-affirmed-gras-pathway]
- 41. HHS Secretary Kennedy Directs FDA to Explore ... [https://www.hhs.gov/press-room/revising-gras-pathway.html]
- 42. FDA Plans to Require Mandatory GRAS Notifications [https://www.foodchainid.com/resources/fda-plans-to-require-mandatory-gras-notifications/]
- 43. FDA's 2025 Agenda: GRAS, FOP, and Supplement Rule ... [https://sourcenutra.com/2025/09/fda-2025-unified-agenda-gras-fop-supplement-ingredients/]
- 44. FDA GRAS reform timeline accelerates [https://www.supplysidesj.com/supplement-regulations/gras-reform-proposal-accelerates]
- 45. Senator Marshall Introduces GRAS Reform Bill [https://www.hoganlovells.com/en/publications/senator-marshall-introduces-gras-reform-bill]
- 46. Summary of U.S. FDA GRAS Updates in the Third Quarter ... [https://www.cirs-group.com/en/food/summary-of-us-fda-gras-updates-in-the-third-quarter-of-2025]
- 47. 10 Major Challenges of Nanochip Production (How to ... [https://digitaldefynd.com/IQ/how-to-overcome-challenges-of-nanochip-production/]
- 48. Nanotechnology [https://www.fda.gov/about-fda/nctr-research-focus-areas/nanotechnology]
- 49. Regenerative Medicine Advanced Therapy Designation [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/regenerative-medicine-advanced-therapy-designation]
- 50. FDA Activity Recap: September 2025 Features New Draft ... [https://www.cgtlive.com/view/fda-activity-recap-september-2025-features-draft-guidance-documents-rmat-designation]
- 51. Advanced Regenerative Medicines for Rare Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC11530468/]
- 52. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 53. Expedited Programs for Regenerative Medicine Therapies ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/expedited-programs-regenerative-medicine-therapies-serious-conditions-0]
- 54. Nanoscope Strengthens Global Regulatory Pathways for ... [https://nanostherapeutics.com/2025/09/02/nanoscope-strengthens-global-regulatory-pathways-for-mco-010-with-fda-rmat-and-five-ema-orphan-designations/]
- 55. Nanoscope Strengthens Global Regulatory Pathways for ... [https://www.prnewswire.com/news-releases/nanoscope-strengthens-global-regulatory-pathways-for-mco-010-with-fda-rmat-and-five-ema-orphan-designations-302543344.html]
- 56. EMA grants Orphan designations to MCO-010, FDA ... [https://www.ophthalmologytimes.com/view/ema-grants-orphan-designations-to-mco-010-fda-grants-rmat-in-stargardt-disease]
- 57. Nanoscope Therapeutics Initiates Rolling Submission of ... [https://www.prnewswire.com/news-releases/nanoscope-therapeutics-initiates-rolling-submission-of-biologics-license-application-to-fda-for-mco-010-the-first-gene-agnostic-therapy-to-treat-retinitis-pigmentosa-302503892.html]
- 58. Nanoscope Therapeutics Puts Rolling BLA for Retinitis ... [https://www.cgtlive.com/view/nanoscope-therapeutics-rolling-bla-retinitis-pigmentosa-gene-therapy-mco-010-front-fda]
- 59. MCO-010 Gene Therapy Moves Toward FDA Approval [https://www.usher-syndrome.org/what-is-usher-syndrome/science-news/general-news.html/article/2025/11/04/new-hope-for-vision-nanoscope-therapeutics-mco-010-moves-closer-to-fda-approval]
- 60. Nanotechnology Drug Delivery Market: A Deep-Dive Analysis ... [https://www.pharmiweb.com/press-release/2025-07-17/nanotechnology-drug-delivery-market-a-deep-dive-analysis-2025-2035]
- 61. Regulating nanomedicines: challenges, opportunities, and ... [https://pubmed.ncbi.nlm.nih.gov/40657903/]
- 62. 25 years of research and regulation: Is nanotechnology ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1629813/full]
- 63. Global Summit on Regulatory Science [https://www.fda.gov/about-fda/science-research-nctr/global-summit-regulatory-science]
- 64. Regulatory pathways and guidelines for nanotechnology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11919859/]
- 65. Our Take: FDA Guidance on Nanotechnology [https://www.malvernpanalytical.com/en/learn/knowledge-center/insights/our-take-fda-guidance-on-nanotechnology]