Nanobiosensors vs. Traditional Diagnostics: A New Paradigm in Accuracy for Biomedical Research
This article provides a comprehensive analysis for researchers and drug development professionals on the transformative role of nanobiosensors in diagnostic accuracy.
Nanobiosensors vs. Traditional Diagnostics: A New Paradigm in Accuracy for Biomedical Research
Abstract
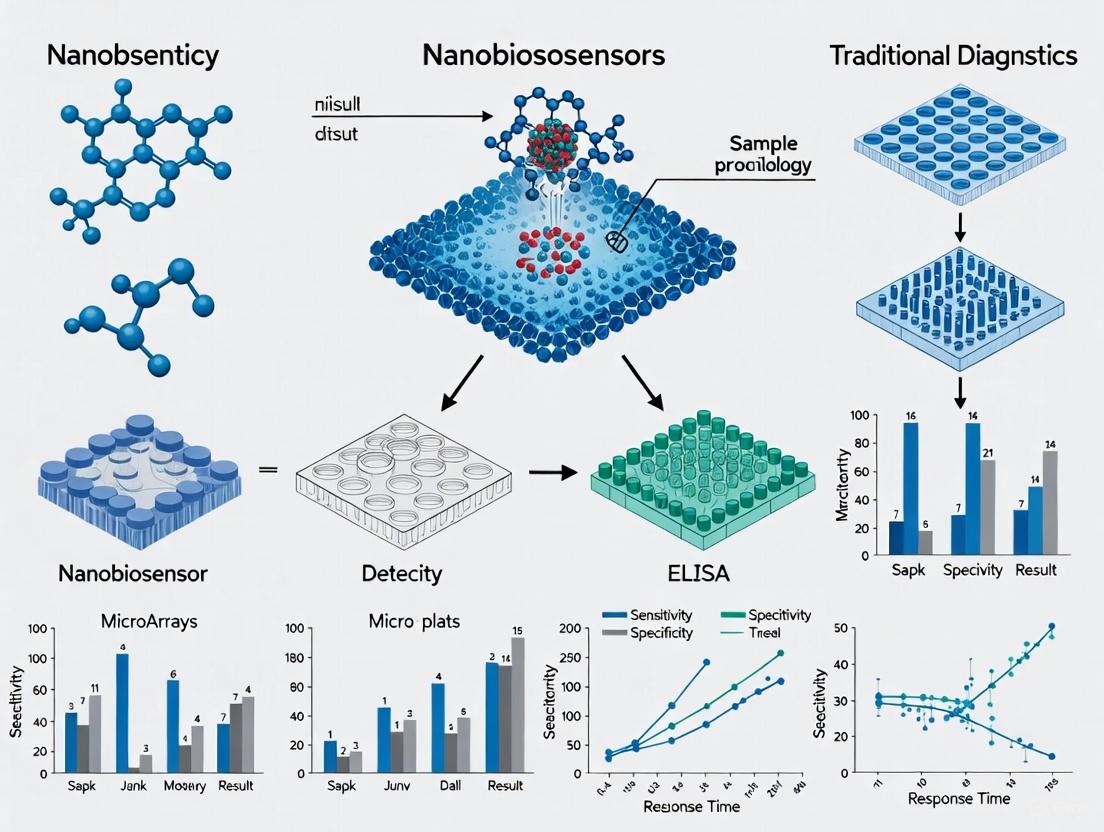
This article provides a comprehensive analysis for researchers and drug development professionals on the transformative role of nanobiosensors in diagnostic accuracy. It explores the foundational principles of nanobiosensors, detailing their operation and the nanomaterials that enhance their function. The review covers diverse methodological applications across oncology, neurodegenerative diseases, and infectious diseases, highlighting their integration into point-of-care systems. It critically addresses current challenges in fabrication and standardization while presenting a rigorous comparative validation against traditional techniques like ELISA and PCR. The synthesis concludes that nanobiosensors offer a significant leap in sensitivity, specificity, and speed, paving the way for personalized medicine and advanced clinical diagnostics.
The Foundation of Nanobiosensors: Principles and Core Components
Nanobiosensors represent a transformative class of analytical devices that synergistically integrate biological recognition elements with nanotechnology-enabled transducers. According to the International Union of Pure and Applied Chemistry (IUPAC), a biosensor is a device that uses specific biochemical reactions mediated by isolated enzymes, immune systems, tissues, or organelles to detect chemical compounds through optical, thermal, or electrical signals [1]. The evolution into nanobiosensors involves the application of nanomaterials and nanoscale engineering principles to create systems with significantly enhanced sensitivity, specificity, and operational characteristics. These devices are fundamentally characterized by their ability to detect biological markers (BioMKs) linked with various disease states with exceptional precision, addressing critical limitations of traditional diagnostic methods such as truncated sensitivity, stunted specificity, and cumbersome operational procedures [2].
The architectural foundation of a nanobiosensor consists of two primary components: a biological recognition element and a nanotechnology-based transducer. The biological element, which can include enzymes, antibodies, DNA/RNA probes, or whole cells, provides the mechanism for specific target interaction. The transducer, enhanced with nanomaterials such as nanoparticles, carbon nanotubes (CNTs), quantum dots (QDs), or nanowires, converts this biological interaction into a quantifiable electronic, optical, or acoustic signal [2] [1]. This integration has propelled innovations across medical diagnostics, with applications ranging from continuous intravascular monitoring of physiological parameters to early-stage detection of cancers and infectious diseases [3]. The burgeoning market interest is reflected in the estimated biosensor market size of USD 30.25 billion in 2024, with a projected compound annual growth rate (CAGR) of 8.7% from 2025 to 2034, underscoring the significant impact of these technologies [3].
Comparative Analysis: Nanobiosensors vs. Traditional Diagnostics
The diagnostic performance of nanobiosensors substantially surpasses that of traditional methods across multiple parameters, including sensitivity, specificity, response time, and potential for miniaturization. The defining advantage stems from the nanoscale interface, which offers a dramatically increased surface-to-volume ratio, enhancing the density of biorecognition events and improving signal transduction efficiency [2] [1].
Table 1: Performance Comparison of Diagnostic Modalities
| Performance Parameter | Traditional Diagnostics | Nanobiosensors | Experimental Evidence |
|---|---|---|---|
| Sensitivity | Truncated sensitivity (e.g., microscopic procedures) [2] | Exceptionally high; capable of detecting single biomolecules [1] | Detection of cellular miRNA in colorectal cancer; identification of single biomarkers [2] |
| Specificity | Susceptible to interference; stunted specificity [2] | High specificity via precise biorecognition (e.g., antibody-antigen, DNA hybridization) [1] | Functionalized nanoparticles for specific pathogen detection [2] |
| Response Time | Often lengthy (e.g., culture tests taking weeks) [4] | Rapid, real-time monitoring (minutes vs. weeks) [4] [3] | Intravascular glucose sensors providing real-time data [3]; molecular PCR diagnostics cutting wait time by up to four weeks versus culture [4] |
| Multiplexing Capability | Generally limited to single-analyte detection | High potential for simultaneous detection of multiple analytes [2] | Use of multiplex PCR assays for identifying multiple resistance mutations [4] |
| Miniaturization & Portability | Cumbersome equipment; mostly confined to laboratories [2] | High degree of miniaturization; enables point-of-care testing (POCT) [4] [3] | Implantable intravascular biosensors for continuous monitoring [3]; expansion of POCT in remote areas [4] |
A critical application demonstrating this performance leap is in glucose monitoring for diabetes management. While traditional methods require frequent, invasive blood sampling with delayed results, electrochemical implantable biosensors, including subcutaneous or intravascular variants, provide real-time glucose level data, enabling precise therapy adjustments [3]. A study utilizing the GluCath System—an intravascular continuous glucose monitoring system based on a chemical fluorescence quenching mechanism—demonstrated acceptable accuracy during 48-hour placement in critically ill patients, a scenario where both hyperglycemia and hypoglycemia can lead to adverse outcomes [3].
Furthermore, the emergence of non-invasive liquid biopsies for early cancer detection represents another area where nanobiosensors outperform traditional tissue biopsies. These nanobiosensor-based liquid biopsies analyze blood samples to detect cancers earlier than traditional methods, offering a safer, less invasive alternative to surgical procedures [4].
Experimental Protocols and Methodologies
Protocol 1: Fabrication of an Electrochemical Nanobiosensor for Glucose Detection
This protocol details the development of an implantable electrochemical glucose sensor, a technology that has been validated in clinical studies for continuous monitoring [3].
1. Reagent Preparation:
- Glucose Oxidase and Catalase: Immobilize these enzymes within a specialized polymer membrane. Glucose oxidase catalyzes the oxidation of glucose, while catalase is often co-immobilized to break down the resulting hydrogen peroxide, mitigating its interfering effects and improving sensor longevity [3].
- Nanomaterial-functionalized Electrode: Prepare a working electrode by functionalizing its surface with nanomaterials such as carbon nanotubes or gold nanoparticles. This step increases the electroactive surface area, enhances electron transfer rates, and improves the stability of the immobilized enzymes [2] [1].
2. Sensor Assembly and Transduction Mechanism:
- Integrate the enzyme-immobilized membrane with the nanomaterial-functionalized oxygen electrode. The operational principle is based on the electrochemical detection of oxygen consumption. As glucose diffuses into the membrane and is oxidized by glucose oxidase, local oxygen is consumed. The oxygen electrode transduces this change in oxygen concentration into a quantifiable amperometric signal (current) that is proportional to the glucose concentration [3].
- Assemble the sensor with a reference electrode and a counter electrode to form a complete three-electrode electrochemical cell. The entire assembly is then integrated with a miniaturized telemetry system for wireless data transmission from the implant site [3].
3. Calibration and Validation:
- Calibrate the sensor response in vitro using standard glucose solutions across a physiologically relevant range (e.g., 50-400 mg/dL).
- Validate sensor performance in vivo by comparing the sensor's telemetry signal with reference blood glucose values measured using standard laboratory techniques. A mathematical model is often applied to describe the dynamic relationship between blood glucose and the sensor signal in the tissue [3].
Protocol 2: Development of an Optical Nanobiosensor for Liquid Biopsy
This protocol outlines the creation of a nanobiosensor for detecting cancer biomarkers in blood serum, a key application in the trend toward liquid biopsies [4].
1. Surface Functionalization:
- Functionalization with Antibodies: A optical fiber or waveguide is coated with a nanomaterial (e.g., gold nanoparticles or graphene) to enhance its evanescent field and surface plasmon resonance properties. The surface is then functionalized with specific monoclonal antibodies that act as capture probes for a target cancer biomarker (e.g., prostate-specific antigen or circulating tumor DNA) [2] [1].
2. Sample Incubation and Binding:
- A serum sample from a patient is introduced to the functionalized sensor surface and allowed to incubate. Target biomarkers present in the sample will bind specifically to the immobilized antibodies.
3. Signal Generation and Detection:
- Label-based Detection: A secondary antibody, conjugated with a fluorescent nanomaterial (e.g., quantum dots), is introduced. This antibody binds to the captured biomarker, forming a "sandwich" complex. The excitation of the quantum dots results in a fluorescence signal whose intensity is proportional to the biomarker concentration [1].
- Label-free Detection: The binding of the biomarker to the sensor surface directly alters the local refractive index. This change is detected as a shift in the resonance angle of a surface plasmon resonance (SPR) setup or a wavelength shift in a fiber Bragg grating, providing a quantitative measure of the biomarker without the need for secondary labels [2] [1].
Signaling Pathways and Experimental Workflows
The core functionality of a nanobiosensor can be visualized as a sequential process involving molecular recognition and signal transduction. The following diagram illustrates this generalized workflow, which is common to many nanobiosensor designs.
Diagram 1: Generalized workflow of a nanobiosensor.
For electrochemical biosensors, which are widely used for continuous monitoring of metabolites like glucose, the process involves a specific biochemical reaction that generates an electrical current.
Diagram 2: Electrochemical glucose nanobiosensor mechanism.
The Scientist's Toolkit: Key Research Reagent Solutions
The development and operation of high-performance nanobiosensors rely on a suite of specialized reagents and materials. The table below details several key components and their critical functions in experimental setups.
Table 2: Essential Research Reagents and Materials for Nanobiosensor Development
| Reagent/Material | Function in Nanobiosensors | Specific Examples & Applications |
|---|---|---|
| Nanoparticles (NPs) | Signal amplification; carrier for biorecognition elements; enhance conductivity and catalytic activity. | Au NPs for colorimetric sensors; magnetic NPs for separation and detection [2]. |
| Carbon Nanotubes (CNTs) | Transducer element; provide high electrical conductivity and large surface area for biomolecule immobilization. | Used in electrochemical sensors to enhance electron transfer and sensitivity [1]. |
| Quantum Dots (QDs) | Fluorescent labels; provide high photostability and tunable emission wavelengths for multiplexed optical detection. | QD-antibody conjugates for fluorescent immunoassays and bioimaging [1] [3]. |
| Enzymes | Biological recognition element; catalyze specific reactions with the target analyte to generate a detectable product. | Glucose oxidase for glucose sensors; horseradish peroxidase used in enzyme-linked assays [2] [3]. |
| Antibodies/Aptamers | Biological recognition element; provide high specificity and affinity for binding to target antigens or molecules. | Monoclonal antibodies for immunoassays; DNA/RNA aptamers as synthetic recognition elements [2] [1]. |
| Functionalized Surfaces | Platform for immobilizing biorecognition elements; ensure stability and proper orientation of biomolecules. | SAMs (Self-Assembled Monolayers) on gold surfaces; polymer membranes for enzyme encapsulation [2] [3]. |
The integration of nanotechnology with biological recognition principles has unequivocally given rise to a new generation of diagnostic tools. As the comparative data and experimental protocols in this guide demonstrate, nanobiosensors objectively surpass traditional diagnostic methods in critical performance metrics such as sensitivity, speed, and miniaturization potential. These devices are poised to fundamentally reshape diagnostic paradigms, enabling a shift from centralized, delayed testing to decentralized, real-time, and personalized health monitoring. The ongoing research and development, particularly in areas like intravascular biosensors, liquid biopsies, and point-of-care devices, underscore a clear trajectory toward more integrated, intelligent, and accessible healthcare solutions. For researchers and drug development professionals, mastering the materials, methods, and principles behind nanobiosensors is not merely an academic exercise but a necessary step toward actively participating in and driving the future of medical diagnostics.
At the heart of every biosensor lies a fundamental principle: the specific interaction between a biological recognition element (bioreceptor) and a target analyte, which is subsequently transformed into a quantifiable signal [3] [1]. This process bridges the biological and digital worlds, enabling the detection and measurement of substances ranging from simple ions to complex proteins and whole cells. Biosensors are defined as analytical instruments that measure variations in biological activity and transform them into quantifiable electronic signals [3]. The evolution of this technology, particularly with the integration of nanotechnology, has revolutionized diagnostics by enhancing sensitivity, specificity, and miniaturization far beyond the capabilities of traditional methods [1] [5].
The core architecture of a biosensor universally comprises two essential components: a bioreceptor that facilitates specific interaction with the target analyte, and a transducer that converts this biological event into a measurable electrical, optical, or other physical signal [1]. This review provides a systematic comparison of the working principles, performance metrics, and experimental methodologies of various biosensor classes, with a specific focus on the transformative impact of nanotechnology in enhancing diagnostic accuracy.
Core Components and Working Principles
The Bioreceptor-Target Interaction
The initial and most critical step in biosensing is the specific molecular recognition between the bioreceptor and the target analyte. This interaction confers the sensor's selectivity. Common bioreceptors and their binding mechanisms include:
- Enzymes: Catalyze specific biochemical reactions, with the reaction rate proportional to the analyte concentration [1].
- Antibodies: Bind to specific antigens (e.g., proteins, pathogens) with high affinity through immunocomplex formation [5].
- Nucleic Acids (DNA/RNA): Hybridize with complementary sequences, enabling the detection of genetic markers, mutations, or pathogens [1] [5].
- Whole Cells and Tissues: Utilize inherent metabolic pathways or receptor functions for detection [1].
The following diagram illustrates the generalized workflow of a biosensor, from analyte binding to signal output.
Diagram 1: The core signal transduction pathway in a biosensor.
Transduction Mechanisms: Converting Biology to Signal
Following the biorecognition event, a physicochemical change (e.g., electron transfer, mass change, photon emission) occurs. The transducer detects this change and converts it into an analyzable signal. The principal transduction mechanisms are compared below:
- Electrochemical: Measures electrical properties (current, potential, impedance) resulting from the biological interaction. These are highly sensitive and compatible with miniaturization [3] [1].
- Optical: Detects changes in light properties (wavelength, intensity, polarization) using techniques like fluorescence, surface plasmon resonance (SPR), or Raman scattering (e.g., SERS) [3] [5].
- Acoustic: Utilizes sound waves; the binding of mass to the sensor surface alters the frequency of acoustic wave devices (e.g., Quartz Crystal Microbalance - QCM) [3].
- Thermal: Measures the heat absorbed or released during a biochemical reaction using thermistors [3].
Performance Benchmarking: Nanobiosensors vs. Traditional Diagnostics
The integration of nanomaterials such as nanoparticles, nanotubes, quantum dots, and nanowires has profoundly enhanced the performance characteristics of biosensors [1] [6]. The table below provides a quantitative and qualitative comparison of key diagnostic approaches.
Table 1: Performance comparison of diagnostic sensor technologies
| Parameter | Traditional Diagnostics (e.g., ELISA, Standard Electrodes) | Modern Nanobiosensors | Experimental Basis & Context |
|---|---|---|---|
| Sensitivity | Low to moderate (μM-mM range) | Very High (pM-fM range) | Nanomaterials provide a large surface area, enhancing response to low-abundance biomarkers [1] [5]. |
| Specificity | Moderate; susceptible to cross-reactivity | Very High | High specificity of bioreceptors combined with nanomaterial-enhanced signal-to-noise ratio reduces false positives [5]. |
| Response Time | Minutes to hours (e.g., 1-4 hours for ELISA) | Seconds to minutes | Nanostructures facilitate faster mass transfer and catalytic activity, enabling real-time monitoring [1]. |
| Miniaturization Potential | Low | Very High | Nanoscale components enable implantable and wearable form factors (e.g., intravascular biosensors) [3] [1]. |
| Multiplexing Capability | Low (typically single analyte) | High | Nanostructured arrays (e.g., Au@SiO₂) allow simultaneous detection of multiple analytes on a single platform [5]. |
| Accuracy (Example: IL-6 Detection) | Standard ELISA: Reference value | AuNP/THI Immunosensor: Excellent correlation with ELISA results [5] | A novel label-free electrochemical immunosensor using gold nanoparticles (AuNPs) demonstrated successful detection of Interleukin-6 (IL-6) in patient blood samples, showing high agreement with the standard ELISA method [5]. |
Experimental Protocols for Key Nanobiosensor Types
Protocol: SERS-based Biosensor for Telomerase Activity
This protocol details the construction of a surface-enhanced Raman scattering (SERS) biosensor for ultra-sensitive analysis of telomerase activity, used for early cancer diagnosis [5].
1. Sensor Fabrication:
- Substrate Preparation: A single-layer SiO₂ colloidal crystal film is self-assembled by vertical evaporation. Gold nanoparticles (AuNPs) are then adsorbed onto this film via electrostatic adsorption to create an ordered Au@SiO₂ array substrate.
- Probe Immobilization: The Au@SiO₂ array is functionalized with hairpin DNA2 (hpDNA2) to serve as the capture substrate. Separately, SERS probes are prepared by labeling Au-Ag nanocages (Au-AgNCs) with a Raman reporter molecule and hairpin DNA1 (hpDNA1).
2. Assay Procedure:
- Telomerase Extension: The sample containing telomerase and deoxyribonucleoside triphosphates (dNTPs) is applied. Telomerase primers elongate to form long-strand DNA containing repetitive sequences (TTAGGG).
- Dual DNA Amplification: The elongated product triggers a Strand Displacement Amplification (SDA) reaction. The SDA product then initiates a Catalytic Hairpin Assembly (CHA) reaction, bringing the SERS probes (Au-AgNCs) into close proximity with the capture substrate (Au@SiO₂ array).
- Signal Generation & Readout: The assembly of metallic nanostructures creates "hot spots" that dramatically enhance the local electromagnetic field, leading to a significantly amplified SERS signal. The intensity of this signal is quantitatively correlated with telomerase activity.
The following diagram outlines this complex experimental workflow.
Diagram 2: Workflow for a SERS-based telomerase activity assay.
Protocol: Electrochemical Immunosensor for Interleukin-6 (IL-6)
This protocol describes the development of a label-free electrochemical immunosensor for the rapid and sensitive detection of IL-6, a key inflammatory biomarker [5].
1. Sensor Fabrication:
- Electrode Modification: A platinum carbon electrode is modified with gold nanostructures (e.g., Au nanospheres, AuNPs/THI) to create a high-surface-area platform that enhances electron transfer and provides sites for antibody immobilization.
- Bioreceptor Immobilization: IL-6 antibodies are fixed onto the nano-structured electrode surface. In one approach, 4-mercaptobenzoic acid is used as a linker to anchor antibodies to the gold nanoparticles [5].
2. Assay Procedure:
- Incubation: The functionalized electrode is incubated with the sample (e.g., patient serum). IL-6 antigens specifically bind to the immobilized antibodies.
- Label-Free Detection: The binding event directly alters the interfacial properties of the electrode (e.g., charge transfer resistance or capacitance), which is measured without the need for a secondary enzyme label.
- Electrochemical Measurement: Techniques such as electrochemical impedance spectroscopy (EIS) or voltammetry are employed to quantify the change in the electrical signal, which is proportional to the IL-6 concentration in the sample. This sensor has been successfully validated against the standard ELISA method using patient blood samples [5].
The Scientist's Toolkit: Essential Research Reagents and Materials
The fabrication and operation of high-performance nanobiosensors rely on a suite of specialized materials and reagents. The following table details key components and their functions in typical experiments.
Table 2: Essential research reagents and materials for nanobiosensor development
| Material/Reagent | Function in Biosensing | Example Application |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Signal amplification; biocompatible platform for bioreceptor immobilization; enhances electron transfer in electrochemical sensors [6] [5]. | Used in SERS substrates and electrochemical immunosensors for IL-6 detection [5]. |
| Quantum Dots (QDs) | Fluorescent labels with high brightness and photostability; size-tunable emission wavelengths [3] [1]. | Multiplexed detection of biomarkers via distinct fluorescent colors. |
| Carbon Nanotubes (CNTs) | Enhance electrical conductivity in electrochemical sensors; high surface area for analyte loading [1]. | Used for creating highly sensitive enzyme-based or DNA-based electrochemical sensors. |
| Specific Bioreceptors (Antibodies, DNA) | Molecular recognition element that provides high specificity for the target analyte [1]. | Antibodies for protein detection (e.g., IL-6); DNA probes for genetic marker detection [5]. |
| Enzymes (e.g., Glucose Oxidase) | Biological catalyst that generates a measurable product (e.g., H₂O₂) upon interaction with the analyte [3] [1]. | Core recognition element in continuous glucose monitoring systems [3]. |
The fundamental working principle of a biosensor—from specific bioreceptor interaction to signal transduction—provides a versatile framework for analytical science. The integration of nanotechnology has decisively shifted the performance benchmarks, enabling nanobiosensors to achieve superior sensitivity, speed, and multiplexing capabilities compared to traditional diagnostic methods. Experimental data from advanced platforms, such as SERS-based sensors for telomerase and electrochemical immunosensors for IL-6, consistently demonstrate this enhanced accuracy and their growing potential for clinical translation. While challenges such as biocompatibility, long-term stability, and standardized manufacturing remain active areas of research, the continued development of novel nanomaterials and sophisticated bioreceptor engineering promises to further solidify the role of nanobiosensors in the future of precise molecular diagnosis and personalized medicine.
The evolution of biosensor technologies is revolutionizing modern healthcare, shifting the paradigm from traditional diagnostic methods towards real-time, continuous monitoring and personalized medicine [3]. Central to this transformation are nanomaterials—gold nanoparticles (AuNPs), quantum dots (QDs), carbon nanotubes (CNTs), and graphene. Their integration into biosensing platforms addresses critical limitations of conventional diagnostics, such as poor sensitivity for low-concentration biomarkers, inability for real-time monitoring, and lengthy processing times. For instance, traditional techniques like Enzyme-Linked Immunosorbent Assay (ELISA) for biomarker detection are specialized and time-intensive, limiting real-time disease progression monitoring [7]. Nanomaterials, with their high surface-to-volume ratio, exceptional electrical properties, and tunable surface chemistry, enable the development of biosensors with unprecedented sensitivity, specificity, and form factor, paving the way for devices capable of detecting targets from glucose to female hormones, which are present in concentrations millions of times lower [8]. This guide provides a comparative analysis of these key nanomaterials, focusing on their performance in biosensing applications within the broader research context of nanobiosensors versus traditional diagnostic accuracy.
Comparative Performance Analysis of Nanomaterials
The table below summarizes the core characteristics and performance metrics of the four key nanomaterials in biosensing applications, based on recent experimental findings.
Table 1: Comparative Performance of Key Nanomaterials in Biosensing
| Nanomaterial | Key Biosensing Properties | Reported Performance & Experimental Data | Common Functionalization Strategies |
|---|---|---|---|
| Gold Nanoparticles (AuNPs) | High biocompatibility, strong Surface Plasmon Resonance (SPR), easy functionalization, size/shape-dependent optical properties [9]. | - AI-integrated AuNP biosensors reduce false positives by 40% [10].- Enable optical imaging resolution down to 10 nm [10].- Provide rapid, non-invasive pathogen detection with 95% accuracy within 30 minutes [10]. | Conjugation with antibodies, aptamers, and DNA; formation of core-shell structures with polymers [9]. |
| Quantum Dots (QDs) | Carbon QDs (CQDs): Low toxicity, tunable photoluminescence, excellent biocompatibility, eco-friendly [11] [12].Graphene QDs (GQDs): Higher surface area, superior carrier mobility, smaller bandgaps than CQDs [13]. | - CQDs function as effective photoelectrodes, absorbing visible and near-infrared light [13].- GQD-based nanohybrids demonstrate better hydrogen evolution rates and catalytic efficiency than CQD-based materials [13].- GQDs as co-catalysts improved photocurrent densities by up to 8.8 times compared to CQD co-catalysts [13]. | Doping (e.g., nitrogen), surface passivation with PEG or PEI, combination with other nanomaterials in hybrids [13] [11]. |
| Carbon Nanotubes (CNTs) | High carrier mobility, ballistic electron transport, large surface-to-volume ratio, nanoscale dimensions [14]. | - Single-Walled CNT (SWCNT) sensors enable real-time monitoring of Nitric Oxide (NO), a key inflammatory biomarker for Osteoarthritis [7].- SWCNTs functionalized with (AT)15-ssDNA show specific fluorescence quenching in response to NO concentration [7].- Chirality-pure (6,5) CNTs show higher dopamine adsorption efficiency than (6,6) CNTs, crucial for low-concentration sensing [8]. | Non-covalent wrapping with ssDNA, functionalization with specific polymers, antibody conjugation [14] [7]. |
| Graphene | Exceptional electrical conductivity, high mechanical strength, atomic thickness, large surface area, tunable surface chemistry [15]. | - Graphene Field-Effect Transistors (GFETs) enable real-time, label-free detection of DNA, proteins, and gases [15].- Enhances Surface Plasmon Resonance (SPR) and Surface-Enhanced Raman Scattering (SERS) sensitivity due to strong light-matter interaction [15].- Graphene-based electrodes in electrochemical sensors support rapid electron transfer and fast response times [15]. | π–π stacking, covalent bonding with bioreceptors (antibodies, aptamers), use of derivatives like GO and rGO [15]. |
Experimental Protocols for Nanomaterial-Based Detection
Protocol 1: Real-Time Monitoring of Nitric Oxide with SWCNT Biosensors
This protocol details the methodology for using ssDNA-functionalized Single-Walled Carbon Nanotubes (SWCNTs) to detect nitric oxide (NO), a key inflammatory biomarker, as described in recent research [7].
- Primary Objective: To enable real-time, wireless optical monitoring of NO concentrations in biological environments for early diagnosis and management of inflammatory conditions like osteoarthritis.
- Materials & Reagents:
- SWCNTs: Serve as the fluorescent transducer element.
- (AT)15 Single-Stranded DNA (ssDNA): Used to suspend and functionalize SWCNTs, providing selectivity for NO.
- Gelatin Methacryloyl (GelMA) Hydrogel: Acts as a biocompatible matrix to immobilize the sensor.
- Poly-(Methyl Methacrylate) (PMMA): Used as the substrate for the implantable sensor tag.
- Custom Optical Reader: A device with 657 nm and 726 nm LEDs for excitation and a sensitive SWIR camera for detecting the fluorescence emission of SWCNTs (~900-1400 nm).
- Methodology:
- Sensor Preparation: SWCNTs are suspended and non-covalently functionalized with (AT)15 ssDNA nucleotide sequences. This coating confers selectivity for NO.
- Immobilization: The ssDNA-SWCNT complex is uniformly embedded within a GelMA hydrogel to create a stable, biocompatible sensing layer.
- Tag Integration: The ssDNA-SWCNT:GelMA sensor is integrated into a tiny, implantable PMMA tag.
- Optical Sensing: The implanted tag is excited by the external optical reader. Upon binding of NO, the SWIR fluorescence of the SWCNTs is selectively quenched.
- Quantification: The degree of fluorescence quenching is measured and correlated with the concentration of NO in the surrounding environment.
- Key Experimental Workflow:
Protocol 2: Enhanced Photoelectrochemical Sensing with Graphene Quantum Dots
This protocol outlines the use of Graphene Quantum Dots (GQDs) to significantly enhance the performance of photoelectrochemical (PEC) systems, such as those used for water splitting and biomarker detection [13].
- Primary Objective: To leverage the superior properties of GQDs over CQDs to improve light absorption, charge separation, and catalytic activity in PEC biosensing platforms.
- Materials & Reagents:
- Graphene Quantum Dots (GQDs): Act as a co-catalyst and sensitizer.
- Semiconductor Photoelectrode (e.g., TiO₂): Serves as the primary photoactive material.
- Nitrogen Dopant Precursor: Used to introduce nitrogen atoms into the GQD structure to enhance electrocatalytic activity.
- PEC Cell: A standard electrochemical cell equipped with a light source and electrodes.
- Methodology:
- Synthesis & Doping: GQDs are synthesized via a bottom-up approach (e.g., from citric acid) or top-down method. They are subsequently doped with nitrogen to create more active sites.
- Nanohybrid Formation: The N-doped GQDs are composited with the semiconductor photoelectrode (e.g., TiO₂) to form a nanohybrid material.
- PEC Testing: The GQD-semiconductor photoelectrode is assembled in a PEC cell. Upon illumination, the GQDs enhance light absorption, particularly in the visible spectrum.
- Performance Measurement: The photocurrent density generated is measured. GQDs act as electron reservoirs, reducing the recombination of photogenerated electron-hole pairs and leading to a significantly higher photocurrent.
- Key Experimental Workflow:
Signaling Pathways and Sensing Mechanisms
The superior performance of nanobiosensors is rooted in the distinct physical mechanisms through which they transduce a biological binding event into a quantifiable signal. The following diagram illustrates the primary signaling pathways for the featured nanomaterials.
Table 2: Core Sensing Mechanisms in Nanobiosensors
| Nanomaterial | Primary Sensing Mechanism | Description |
|---|---|---|
| Gold Nanoparticles | Localized Surface Plasmon Resonance (LSPR) | Oscillation of conduction electrons at the nanoparticle surface upon light excitation, which shifts upon analyte binding [9]. |
| Quantum Dots | Photoluminescence Modulation | Changes in fluorescence intensity or wavelength due to energy/electron transfer processes or direct binding to the QD surface [13] [11]. |
| Carbon Nanotubes | Fluorescence Quenching / Electrochemical Gating | In optical sensors, fluorescence quenching by charge transfer (e.g., NO detection). In FETs, analyte binding alters the local electrostatic potential, modulating conductivity [14] [7]. |
| Graphene | Field-Effect Modulation / Electrochemical Transfer | In GFETs, analyte binding directly dopes the graphene channel, changing its electrical resistance and enabling label-free detection [15]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers developing nanobiosensors, the following reagents and materials are fundamental for fabricating and functionalizing these advanced sensing platforms.
Table 3: Essential Research Reagents for Nanobiosensor Development
| Item Name | Function / Application in Research |
|---|---|
| Single-Walled Carbon Nanotubes (SWCNTs) | The core transducer material for optical and electrochemical sensors; requires separation/purification by chirality for optimal performance [14] [8]. |
| Specific ssDNA Sequences (e.g., (AT)15) | Used to non-covalently functionalize and suspend SWCNTs, providing selectivity for target analytes like nitric oxide [7]. |
| Graphene Oxide & Reduced Graphene Oxide | Graphene derivatives with abundant oxygen groups for easy functionalization with bioreceptors, widely used in composite sensors and electrodes [15]. |
| Gold Nanospheres, Nanorods, & Nanostars | Spherical particles are common, but shapes with high surface area (nanorods, nanostars) offer superior sensitivity and are preferred for sensor modification [9]. |
| Polyethyleneimine & PEG | Polymers used for surface passivation of Quantum Dots and CNTs to improve solubility, stability, and biocompatibility [14] [11]. |
| PBASE Linker | A common chemical linker (1-pyrenebutyric acid N-hydroxysuccinimide ester) used for the stable attachment of biomolecules onto the surface of CNTs and graphene via π–π stacking [14]. |
| GelMA Hydrogel | A biocompatible hydrogel used to encapsulate and immobilize nanosensors (e.g., ssDNA-SWCNTs) for in vivo implantation and cellular studies [7]. |
| Nitrogen Dopant Precursors | Chemicals used to introduce nitrogen atoms into the lattice of Carbon and Graphene QDs, enhancing their electrocatalytic activity and creating more active sites [13]. |
The evolution of diagnostic technologies has marked a significant transition from conventional laboratory-based assays to advanced biosensing platforms, with transduction mechanisms forming the core of this innovation. Biosensors are analytical devices that integrate a biological recognition element with a transducer to detect and quantify a specific analyte [16]. The transducer's role is to convert the biological interaction into a measurable electrical, optical, or physical signal [17]. The accuracy and efficacy of modern diagnostics, particularly the emerging field of nanobiosensors, are fundamentally governed by the performance of these transduction systems. Within this context, electrochemical, optical, and piezoelectric transduction mechanisms have emerged as the three principal pillars, each with distinct operating principles, advantages, and limitations. This guide provides a structured comparison of these three core transduction mechanisms, framing their performance within the broader thesis of nanobiosensors versus traditional diagnostics accuracy research. It is tailored for researchers, scientists, and drug development professionals by summarizing quantitative performance data and detailing essential experimental protocols.
Comparative Performance Analysis of Transduction Mechanisms
The selection of a transduction mechanism is critical for biosensor design, as it directly influences key analytical parameters such as sensitivity, detection limit, and response time. Table 1 provides a comparative summary of the core performance characteristics of electrochemical, optical, and piezoelectric biosensors, highlighting their suitability for different diagnostic applications.
Table 1: Performance Comparison of Biosensor Transduction Mechanisms
| Performance Parameter | Electrochemical | Optical | Piezoelectric |
|---|---|---|---|
| Fundamental Principle | Measures changes in electrical properties (current, potential, impedance) due to bio-recognition events [16] [18]. | Measures changes in light properties (wavelength, intensity, phase) upon analyte interaction [18] [17]. | Measures change in resonance frequency due to mass change on the sensor surface [19] [20]. |
| Typical Limit of Detection (LOD) | Very high sensitivity (e.g., attomolar (aM) for microRNA [21]). | Very high sensitivity (e.g., 84 aM for microRNA using nanobiosensors [21]). | Nanogram (ng) range per cm² (e.g., ~4.4 ng/cm² for a 10 MHz crystal) [20]. |
| Key Advantage(s) | High sensitivity, simplicity, low cost, portability, suitability for miniaturization and point-of-care (POC) devices [16] [18] [1]. | High sensitivity, capacity for multiplexing (detecting multiple analytes simultaneously), and ability for label-free detection [21] [18]. | Label-free detection, real-time monitoring of binding events, and simplicity of the measurement principle [19] [20]. |
| Primary Limitation(s) | Signal can be susceptible to interference from non-target molecules in complex matrices [18] [1]. | Instrumentation can be complex and costly; some formats may be susceptible to ambient light interference [1]. | Lack of sensitivity and specificity in liquid environments; performance is compromised in viscous solutions [19] [20]. |
| Representative Applications | Glucose monitoring, cardiac biomarker detection, environmental pollutants, foodborne pathogens [16] [18] [17]. | Infectious disease diagnostics (e.g., SARS-CoV-2), cancer biomarker detection, environmental monitoring [21] [17]. | Detection of viruses, bacteria, monitoring of cellular interactions, and enzyme activity studies [20] [18]. |
Experimental Protocols for Key Transduction Mechanisms
A critical understanding for researchers is the methodology behind generating the data that informs performance tables like the one above. This section outlines generalized experimental protocols for each transduction mechanism.
Electrochemical Biosensor Protocol for Glucose Detection
This protocol is based on the classic amperometric glucose biosensor, which detects the current generated from the enzymatic production of hydrogen peroxide [16].
- Electrode Preparation: A three-electrode system (working, counter, and reference) is used. The working electrode (often gold or carbon) is cleaned and polished.
- Enzyme Immobilization: Glucose oxidase (GOx) is immobilized onto the working electrode surface. This can be achieved via methods like cross-linking with glutaraldehyde, entrapment within a polymer matrix (e.g., Nafion), or covalent bonding to a self-assembled monolayer.
- Sensor Assembly and Calibration: The electrode system is integrated into a electrochemical cell. A buffer solution is added, and a constant potential (e.g., +0.7 V vs. Ag/AgCl) is applied. Standard glucose solutions of known concentration are introduced.
- Measurement and Transduction: As GOx catalyzes the oxidation of glucose, it produces hydrogen peroxide (H₂O₂). H₂O₂ is oxidized at the working electrode, generating an electrical current that is directly proportional to the glucose concentration [16].
- Data Analysis: The measured current is plotted against glucose concentration to create a calibration curve, which is used to determine the concentration of unknown samples.
Optical Biosensor Protocol for Antigen Detection using Surface Plasmon Resonance (SPR)
This protocol details a label-free method for detecting antigens, such as a viral protein, using SPR [21].
- Sensor Chip Functionalization: A gold-coated SPR sensor chip is placed in the instrument. The surface is modified with a self-assembled monolayer to create a reactive interface.
- Ligand Immobilization: A specific antibody (ligand) is covalently immobilized onto the sensor chip surface using standard amine-coupling chemistry.
- Baseline Establishment: A running buffer is flowed over the sensor surface to establish a stable optical baseline, measured as a resonance angle.
- Association Phase: The sample containing the target antigen is injected and flowed over the chip. Binding of the antigen to the antibody causes a change in the refractive index at the surface, leading to a shift in the resonance angle, which is monitored in real-time.
- Dissociation Phase: The sample flow is replaced with buffer. The dissociation of the antigen-antibody complex is observed as a return of the signal towards the baseline.
- Regeneration: A mild acidic or basic solution is injected to break the antigen-antibody bonds, regenerating the surface for the next analysis cycle.
- Data Analysis: The sensorgram (a plot of resonance shift vs. time) is analyzed to determine the association and dissociation rate constants, from which the equilibrium dissociation constant (KD) and analyte concentration are calculated.
Piezoelectric Biosensor Protocol for Bacterial Detection
This protocol utilizes a Quartz Crystal Microbalance (QCM) to detect whole bacteria based on mass change [19] [20].
- Crystal Preparation: A quartz crystal with gold electrodes (e.g., AT-cut, 10 MHz) is cleaned. The gold surface is often modified with a chemical layer to facilitate bioreceptor attachment.
- Bioreceptor Immobilization: A specific antibody for the target bacteria is immobilized onto the crystal's electrode surface, typically through physical adsorption or covalent chemistry.
- Baseline Frequency Measurement: The crystal is incorporated into an oscillator circuit and its fundamental resonant frequency (f₀) is measured in air or a clean buffer solution to establish a stable baseline.
- Sample Exposure and Mass Transduction: The sample solution containing the target bacteria is introduced. Binding of the bacteria to the immobilized antibodies increases the mass on the crystal surface. According to the Sauerbrey equation, this mass increase (Δm) causes a proportional decrease in the resonant frequency (Δf) [20].
- Data Analysis: The frequency shift (Δf) is recorded. Using the Sauerbrey equation (Δm = -C · Δf, where C is a constant for the specific crystal), the mass of bound bacteria is quantified. A calibration curve with known bacterial concentrations is used for quantification.
System Workflow and Signaling Pathways
The following diagrams illustrate the logical workflow and core signaling principles for each transduction mechanism, from analyte interaction to signal output.
Electrochemical Biosensor Workflow
Electrochemical Biosensor Signal Generation Pathway
Optical Biosensor Workflow
Optical Biosensor Signal Generation Pathway
Piezoelectric Biosensor Workflow
Piezoelectric Biosensor Signal Generation Pathway
Essential Research Reagent Solutions
The successful development and implementation of biosensors rely on a suite of specialized reagents and materials. Table 2 details key components used across different transduction mechanisms, with their primary functions.
Table 2: Key Research Reagents and Materials for Biosensor Development
| Reagent/Material | Core Function | Transduction System |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Signal amplification; enhance electron transfer in electrochemical sensors; plasmonic core in optical sensors [21] [16]. | Electrochemical, Optical |
| Glucose Oxidase (GOx) | Model enzyme bioreceptor; catalyzes glucose oxidation to produce electroactive H₂O₂ [16]. | Electrochemical |
| Specific Antibodies | High-affinity biorecognition element for antigens, viruses, or bacteria [20] [16]. | Optical, Piezoelectric, Electrochemical |
| Quartz Crystal Microbalance (QCM) Chip | Piezoelectric transducer; resonant frequency shifts with mass loading [19] [20]. | Piezoelectric |
| Carbon Nanotubes (CNTs) | Enhance electrode surface area and conductivity; improve sensitivity in electrochemical detection [16] [1]. | Electrochemical |
| SPR Sensor Chip (Gold Film) | Transducer surface for optical biosensors; supports plasmon wave generation sensitive to refractive index changes [21]. | Optical |
| Aptamers | Synthetic nucleic acid-based biorecognition elements; offer high stability and selectivity for targets [20] [16]. | Optical, Electrochemical |
| Fluorescent Dyes / Quantum Dots | Labels for generating optical signal in fluorescence-based biosensing assays [21] [1]. | Optical |
Electrochemical, optical, and piezoelectric transduction mechanisms each offer a unique set of capabilities that determine their suitability for specific diagnostic applications. Electrochemical systems excel in providing low-cost, portable, and highly sensitive platforms ideal for point-of-care testing, such as glucose monitoring. Optical biosensors offer superior capabilities for multiplexing and real-time, label-free kinetic analysis of biomolecular interactions, making them powerful tools for fundamental research and advanced clinical diagnostics. Piezoelectric biosensors provide a direct method for mass-sensitive detection, useful for monitoring cellular processes and pathogenic microbes. The ongoing integration of nanotechnology, through the use of nanomaterials like gold nanoparticles and carbon nanotubes, is consistently pushing the limits of all three transduction mechanisms, enabling the development of nanobiosensors with dramatically enhanced sensitivity and specificity. This progress is steadily bridging the performance gap between traditional diagnostic methods and modern biosensing platforms, paving the way for more accurate, rapid, and accessible diagnostics in research, clinical, and point-of-care settings.
The Evolution from Traditional Biosensors to Nano-Enhanced Platforms
The field of biosensing has undergone a revolutionary transformation, evolving from first-generation enzyme electrodes to sophisticated platforms enhanced by nanotechnology. This evolution has been driven by the persistent challenge of detecting disease biomarkers at ultra-low concentrations in complex biological fluids, a task where traditional methods often fall short. The integration of nanomaterials has fundamentally improved biosensor performance by leveraging unique properties such as high surface-to-volume ratios, quantum effects, and enhanced reactivity. This guide objectively compares the performance characteristics of traditional biosensors against nano-enhanced platforms, providing researchers and drug development professionals with experimental data and methodologies central to ongoing research on diagnostic accuracy.
Performance Comparison: Traditional vs. Nano-Enhanced Biosensors
The transition to nanotechnology has led to orders-of-magnitude improvements in key analytical metrics. The table below summarizes a direct performance comparison across critical parameters.
Table 1: Performance Comparison Between Traditional and Nano-Enhanced Biosensors
| Performance Parameter | Traditional Biosensors | Nano-Enhanced Biosensors | Experimental Support |
|---|---|---|---|
| Detection Limit | ~10–100 ng/mL (e.g., conventional ELISA) [22] | Femtogram to attomolar levels (e.g., 16.73 ng/mL for AFP; 0.64 fM for biomarkers) [23] [22] | SERS-based α-fetoprotein immunoassay; Aptamer-based SPR sensor [23] [22] |
| Sensitivity | Lower current/optical signal change per unit concentration | High sensitivity (e.g., 95.12 ± 2.54 µA mM⁻¹ cm⁻² for glucose) [23] | Nanostructured composite glucose electrode [23] |
| Selectivity | Good with specific bioreceptors | Enhanced specificity via functionalized nanomaterials (antibodies, aptamers on NPs) [22] [24] | Au-Ag nanostars for biomarker detection; Functionalized NPs for complex fluids [23] [24] |
| Response Time | Minutes to hours for steady-state signal | Rapid, real-time monitoring; Minutes faster using transient signal [25] [26] | Dynamic signal analysis with cantilever biosensors [26] |
| Multiplexing Capability | Limited, often single-analyte | High, simultaneous detection of multiple targets [22] | Nanobiosensor panels for biomarker profiling [22] |
Experimental Protocols and Methodologies
Protocol 1: SERS-Based Immunoassay for Protein Biomarkers
This protocol details a methodology for detecting α-fetoprotein (AFP) using a surface-enhanced Raman scattering (SERS) platform with Au-Ag nanostars, demonstrating the practical application of nanomaterials for ultra-sensitive detection [23].
Key Research Reagent Solutions:
- Au-Ag Nanostars: Plasmonic nanoparticles with sharp-tipped morphology for intense signal enhancement.
- Mercaptopropionic Acid (MPA): A self-assembled monolayer for functionalizing the gold surface.
- EDC/NHS Crosslinkers: Activate carboxyl groups for covalent antibody immobilization.
- Monoclonal Anti-α-fetoprotein Antibodies (AFP-Ab): Biorecognition element for specific antigen capture.
Workflow:
- Nanostar Synthesis & Concentration: Synthesize Au-Ag nanostars and concentrate them via centrifugation (10-60 mins) [23].
- Substrate Functionalization: Incubate the nanostar platform with MPA to form a self-assembled monolayer. Then, activate the carboxyl groups using EDC and NHS chemistry [23].
- Antibody Immobilization: Covalently attach the monoclonal AFP-Ab to the activated platform [23].
- Sample Incubation & Washing: Expose the functionalized sensor to the sample solution containing the AFP antigen. Unbound molecules are removed by washing [23].
- Signal Acquisition & Analysis: Record the intrinsic SERS spectrum of the captured AFP. The limit of detection (LOD) is calculated to be 16.73 ng/mL [23].
The following diagram illustrates the experimental workflow and the signal enhancement principle of the SERS-based nanostar platform.
Protocol 2: AI-Enhanced Dynamic Signal Analysis for microRNA
This protocol leverages machine learning to analyze the dynamic response of cantilever biosensors, significantly improving speed and accuracy while reducing false responses [25] [26].
Key Research Reagent Solutions:
- DNA-Functionalized Cantilever Biosensor: Piezoelectric sensor with a thiolated-DNA probe immobilized on a gold pad.
- microRNA let-7a Target: The analyte of interest (5′ UGAGGUAGUAGGUUGUAUAGUU 3′).
- Theory-Guided Feature Engineering: Extracts features from the binding kinetics (e.g., initial rate of signal change) as inputs for machine learning models [26].
Workflow:
- Data Acquisition: Monitor the resonant frequency (Δf) vs. time (t) as the miRNA binds to the cantilever in a continuous-flow format [26].
- Data Preprocessing: Normalize the dynamic signal to account for sensor-to-sensor variance [26].
- Data Augmentation: Address data sparsity and class imbalance using techniques like jittering and time warping [25] [26].
- Feature Engineering: Generate theory-based features informed by the kinetics of surface-based affinity biosensors [26].
- Model Training & Classification: Train a classifier (e.g., Support Vector Machine) to categorize the biosensor response into target concentration bins, enabling quantification of false-positive and false-negative probabilities [26].
The logical workflow for this AI-enhanced methodology is outlined below.
The Scientist's Toolkit: Essential Research Reagents
The development and operation of high-performance nanobiosensors rely on a specific set of materials and tools. This table details key research reagent solutions and their functions.
Table 2: Essential Research Reagents for Nanobiosensor Development
| Reagent/Material | Function | Example Application |
|---|---|---|
| Gold Nanoparticles (AuNPs) & Nanostars | Plasmonic enhancement, high surface area for bioreceptor immobilization, improved conductivity [23] [22] [27] | SERS-based immunoassays; Electrode modification [23] |
| Carbon Nanotubes (CNTs) | Enhance electron transfer, increase effective surface area, act as transducer element [22] [24] [27] | Electrochemical sensor electrodes for neurotransmitters [22] |
| Quantum Dots (QDs) | Fluorescent probes with size-tunable emission and high photostability [3] [27] | Optical biosensing and multiplexed detection [27] |
| Aptamers | Synthetic nucleic acid bioreceptors with high specificity and stability [22] | Target recognition for electrochemical and optical sensors [22] |
| EDC/NHS Chemistry | Crosslinking system for covalent immobilization of biomolecules on sensor surfaces [23] | Antibody attachment to functionalized nanomaterials [23] |
| Microfluidic Chips | Provide lab-on-a-chip platform for precise fluid manipulation, high throughput, and minimal reagent use [28] | Isolation and analysis of extracellular vesicles (EVs) [28] |
The evolution from traditional to nano-enhanced biosensors represents a quantitative and qualitative leap in diagnostic capability. Experimental data confirms that nanomaterials directly enhance performance by improving sensitivity, lowering detection limits, and enabling faster, multiplexed analyses. Furthermore, the integration of artificial intelligence with dynamic signal analysis introduces a powerful new dimension for improving accuracy and reducing time delay. For researchers and drug development professionals, these advanced platforms offer powerful tools for fundamental research and the development of next-generation clinical diagnostics, particularly for early disease detection where biomarker concentrations are minimal. The continued convergence of nanotechnology, advanced materials, and data science promises to further redefine the limits of biosensing.
Methodologies and Cutting-Edge Applications in Disease Detection
Liquid biopsy has emerged as a compelling minimally invasive alternative to traditional tissue biopsy for cancer diagnosis and monitoring. This approach involves screening for disease-related markers from blood or other biofluids, promising early diagnosis, timely prognostication, and effective treatment monitoring [29]. Unlike traditional tissue biopsies, which provide information from a specific lesion location and can be risky and painful, liquid biopsy captures biomarkers shed into the bloodstream, offering a more comprehensive view of tumor heterogeneity [29]. The primary biomarkers detected through liquid biopsy include circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), and tumor-derived exosomes containing microRNAs (miRNAs) [29]. However, these biomarkers present significant detection challenges due to their extraordinarily low abundance amidst normal cellular components in biofluids, necessitating ultra-sensitive and accurate detection methods [29]. This review comprehensively compares these three biomarker classes within the context of nanobiosensors versus traditional diagnostic approaches, providing experimental data and methodological insights for research professionals.
Biomarker Characteristics and Clinical Significance
Table 1: Comparative Analysis of Key Cancer Biomarkers
| Biomarker | Origin & Composition | Concentration in Cancer | Primary Clinical Applications | Key Challenges |
|---|---|---|---|---|
| CTCs | Intact cancer cells shed from primary or metastatic tumors | Extremely rare (few cells among billions of blood cells) [30] | Assessing tumor heterogeneity, guiding immunotherapy, monitoring minimal residual disease [30] | Specialized isolation methods needed; extreme rarity [29] [30] |
| ctDNA | Fragmented tumor-derived DNA (∼150-350 bp) released into circulation [31] | Short fragments (median: 175 bp in pancreatic cancer) [31] | Early cancer detection, therapy monitoring, tracking resistance mutations [31] | Low fractional abundance; requires ultra-sensitive detection [29] |
| miRNAs | Small non-coding RNAs (~22 nucleotides) packaged in exosomes or protein complexes [32] | Varies by specific miRNA; often dysregulated in cancer [33] | Diagnostic/prognostic biomarkers, therapeutic targets [32] [33] | Panel approach needed for sufficient accuracy [33] |
Traditional Detection Methods Versus Nanobiosensor Approaches
Established Conventional Techniques
Traditional methods for biomarker detection have formed the foundation of liquid biopsy but present significant limitations for clinical implementation:
CTC Detection: Traditional approaches include immunomagnetic separation (CellSearch system) and size-based filtration methods, often followed by immunohistochemical analysis or fluorescence in situ hybridization (FISH) [30]. These methods face challenges in processing large blood volumes sufficient for rare cell capture and often lack standardization for single-cell molecular analyses [30].
ctDNA Analysis: Next-generation sequencing (NGS) platforms serve as the cornerstone for ctDNA mutation profiling, with digital PCR (dPCR) providing ultra-sensitive quantification of specific mutations [31]. These methods exploit fragmentomic patterns, with pancreatic cancer patients showing significantly shorter cfDNA fragments (median: 175 bp) compared to controls (182-186 bp) [31]. While established, these technologies can be costly and require sophisticated bioinformatics infrastructure.
miRNA Profiling: Conventional methods include next-generation sequencing, microarray analysis, Northern blotting, and reverse transcription-quantitative PCR (RT-qPCR) [32]. These techniques have been essential for miRNA biomarker discovery but often lack the sensitivity for direct clinical application without pre-amplification steps and struggle with multiplexing capabilities [32].
Nanobiosensor Platforms and Performance Metrics
Nanobiosensors represent a transformative approach to biomarker detection, leveraging the unique properties of nanomaterials to overcome limitations of conventional methods:
Enhanced Sensitivity and Specificity: Nanobiosensors incorporate engineered nanomaterials such as gold nanoparticles (AuNPs), quantum dots (QDs), carbon nanotubes, and graphene as functional components to improve signal generation and amplification [21]. These materials provide substantially increased surface-area-to-volume ratios, enhancing biorecognition element density and improving detection limits [29] [21].
CTC Capture Technologies: Emerging rare cell capture technologies employing nanostructured substrates functionalized with capture antibodies can process larger blood volumes and enable advanced single-cell analyses [30]. These platforms demonstrate superior capture efficiency and purity compared to conventional methods, with the additional capability of releasing captured cells alive for downstream molecular characterization [30].
ctDNA Detection Innovations: Nanoplasmonic sensors and electrochemical nanosensors have demonstrated capability in detecting cancer-specific fragmentation patterns and methylation signatures in ctDNA [29]. These platforms can distinguish pancreatic cancer patients from healthy controls with high accuracy based on fragmentomic profiles without requiring sequencing [31].
miRNA Sensing Platforms: Nanomaterial-based fluorimetric and electrochemical techniques enable highly sensitive, efficient, and selective detection of miRNAs, addressing the limitations of Northern blotting and RT-qPCR [32]. For colorectal cancer detection, multi-miRNA panels in plasma samples demonstrate pooled sensitivity of 0.85 and specificity of 0.84, with an area under the curve (AUC) of 0.90 across 29 studies [33].
Table 2: Performance Comparison of Detection Platforms
| Detection Platform | Limit of Detection | Analysis Time | Multiplexing Capacity | Key Advantages |
|---|---|---|---|---|
| Traditional CTC Capture | 1-10 CTCs/mL [30] | 3-6 hours | Low | FDA-approved systems available |
| Nano-enhanced CTC Capture | Improved rare cell detection [30] | 1-3 hours | Moderate | Viable cell retrieval; integrated analysis |
| NGS ctDNA Profiling | VAF: 0.1-1% [31] | 2-5 days | High | Comprehensive mutation profiling |
| Nanobiosensor ctDNA | Comparable to NGS [29] | Minutes-hours | Moderate | Point-of-care potential; lower cost |
| RT-qPCR miRNA | ~pM concentrations [32] | 2-4 hours | Low-medium | Gold standard; quantitative |
| Nanosensor miRNA | aM-fM concentrations [21] | <1 hour | High | Superior sensitivity; minimal sample prep |
Experimental Protocols and Workflows
CTC Enrichment and Molecular Characterization Protocol
Advanced CTC analysis workflows integrate nanomaterial-based capture with single-cell omics technologies:
Blood Collection and Processing: Collect 5-10 mL peripheral blood in EDTA or CellSave tubes. Process within 4-24 hours of collection [30].
Nanomaterial-Based CTC Enrichment:
- Incubate blood samples with immunomagnetic nanoparticles conjugated to epithelial (EpCAM) or cancer-specific antibodies
- Apply to microfluidic devices with nanostructured surfaces for enhanced contact and capture efficiency
- Use negative depletion to remove hematopoietic cells using CD45-conjugated nanoparticles
Downstream Molecular Analysis:
- Isolate single CTCs using micromanipulation or microfluidic sorting
- Perform whole genome amplification for copy number alteration analysis
- Conduct RNA sequencing for transcriptional profiling
- Implement protein biomarker characterization using immunocytochemistry
This integrated approach enables the assessment of tumor heterogeneity and identification of heterogeneous drug resistance mechanisms [30].
cfDNA-Based Multi-Feature Analysis for Pancreatic Cancer Detection
A comprehensive cfDNA analysis protocol leveraging multiple molecular features demonstrates superior diagnostic performance:
Sample Preparation and Sequencing:
- Collect plasma from 5 mL blood following double centrifugation protocol
- Extract cfDNA using silica-membrane or magnetic bead-based kits
- Prepare sequencing libraries with 50-100 ng cfDNA input
- Perform low-pass whole-genome sequencing (∼0.5-1× coverage) on DNBSEQ or similar platforms [31]
Multi-Dimensional Feature Extraction:
- Fragmentomics Analysis: Calculate fragment size distribution, end motif preferences, and nucleosome footprinting patterns [31]
- Copy Number Alteration (CNA) Profiling: Identify chromosomal gains and losses using circular binary segmentation algorithm
- Nucleosome Footprint (NF) Analysis: Map protected regions indicative of nucleosome positioning
Predictive Model Construction:
- Apply Least Absolute Shrinkage and Selection Operator (LASSO) regression to select most predictive features
- Construct a weighted diagnostic model (PCM score) integrating fragment, motif, NF, and CNA signatures
- Validate model performance in independent cohorts (AUC: 0.979-0.992 across validation sets) [31]
This multi-feature approach significantly outperforms single-analyte models, distinguishing early-stage pancreatic cancer from healthy controls with AUC of 0.994 [31].
Multi-miRNA Panel Validation for Colorectal Cancer Detection
A systematic framework for developing and validating miRNA panels as diagnostic tools:
miRNA Extraction and Quality Control:
- Isolate miRNAs from 200-500 μL plasma/serum using phenol-chloroform or column-based methods
- Include synthetic spike-in controls (e.g., cel-miR-39) for normalization
- Assess RNA quality using Agilent Bioanalyzer small RNA assay
Profiling and Panel Selection:
- Perform initial discovery phase using miRNA microarrays or NGS on training cohort
- Identify differentially expressed miRNAs with statistical significance (p<0.05, FDR correction)
- Construct multi-miRNA panels using combinatorial optimization or machine learning approaches
- Three-miRNA panels typically demonstrate optimal diagnostic trade-offs [33]
Analytical Validation:
- Validate selected panels using RT-qPCR with stem-loop primers in independent cohorts
- Calculate diagnostic metrics (sensitivity, specificity, AUC) using receiver operating characteristic analysis
- Perform mechanistic validation by mapping recurrent miRNAs to canonical cancer pathways (e.g., PI3K/AKT, Wnt/β-catenin) [33]
This systematic approach has established that multi-miRNA panels achieve pooled sensitivity of 0.85 and specificity of 0.84 for colorectal cancer detection across 29 studies comprising 5,497 participants [33].
Visualization of Experimental Workflows
Diagram 1: Integrated Workflow for Multi-Biomarker Liquid Biopsy Analysis
Diagram 2: miRNA Biomarkers in Oncogenic Pathways and Detection Platforms
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Liquid Biopsy Applications
| Reagent/Material | Function | Example Applications | Performance Notes |
|---|---|---|---|
| Immunomagnetic Nanoparticles | CTC enrichment via epitope-specific capture (e.g., EpCAM, HER2) | Isolation of rare CTCs from whole blood [30] | Enable viable cell release for downstream culture/analysis |
| Silica-coated Magnetic Beads | Nucleic acid binding and purification | cfDNA and miRNA extraction from plasma/serum [31] | Higher recovery rates vs. traditional phenol-chloroform |
| Locked Nucleic Acid (LNA) Probes | Enhanced hybridization affinity for miRNA detection | Northern blotting, in situ hybridization [32] | Increased melting temperature and specificity |
| Quantum Dots (QDs) | Fluorescent labeling with narrow emission spectra | Multiplexed biomarker detection, cellular imaging [29] [21] | Superior photostability vs. organic dyes |
| Gold Nanoparticles (AuNPs) | Signal amplification in colorimetric/electrochemical sensors | Lateral flow assays, SERS-based detection [21] [34] | Tunable optical properties based on size/shape |
| Plasmonic Nanostructures | Enhanced electromagnetic fields for single-molecule detection | SERS-based biomarker quantification [21] | Enable detection at attomolar concentrations |
| DNA Nanoballs (DNB) | High-density sequencing templates | Low-pass whole genome sequencing of cfDNA [31] [35] | Reduce sequencing errors and costs |
The integration of nanobiosensors in liquid biopsy applications represents a paradigm shift in cancer diagnostics, offering unprecedented sensitivity and specificity for detecting CTCs, ctDNA, and miRNAs. While traditional methods like NGS and RT-qPCR remain essential for biomarker discovery and validation, nanomaterial-based platforms demonstrate clear advantages in point-of-care potential, cost-effectiveness, and processing time. The future of cancer diagnostics lies in multi-analyte approaches that combine the strengths of different biomarker classes, such as integrating cfDNA fragmentomics with miRNA panels and CTC protein markers. Emerging technologies including microfluidic-nanobiosensor integration, artificial intelligence-assisted analysis, and single-molecule detection platforms will further enhance diagnostic precision [21]. For research and drug development professionals, understanding the complementary nature of these biomarkers and their optimal detection platforms is crucial for advancing precision oncology and developing novel therapeutic strategies. As standardization improves and large-scale validation studies accumulate, these technologies are poised to transform cancer screening, monitoring, and personalized treatment selection.
The management of neurodegenerative diseases, particularly synucleinopathies like Parkinson’s disease (PD), is undergoing a fundamental transformation, moving from reliance on clinical symptoms to objective biological measures. This shift is centered on the detection of pathological biomarkers, with alpha-synuclein (α-syn) taking a primary role. The aggregation of α-synuclein protein in neurons is a defining pathological hallmark of a spectrum of disorders, including Parkinson's disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA) [36]. Currently, the gold-standard for diagnosis remains a detailed clinical evaluation, which can be prone to error, especially in early disease stages or atypical presentations [36]. The development of tools for direct in vivo detection of α-synuclein pathology represents a critical unmet need in both research and clinical care [36].
This article provides a comparative analysis of emerging diagnostic technologies, framing them within the broader thesis of nanobiosensors versus traditional diagnostics accuracy research. We objectively compare the performance of innovative sensing platforms against established methods, providing supporting experimental data and detailed protocols to illustrate the rapid advancements in this field. The ability to accurately detect and measure α-synuclein and related biomarkers is crucial not only for early and accurate diagnosis but also for monitoring disease progression, stratifying patients for clinical trials, and evaluating the efficacy of novel disease-modifying therapies [36] [37].
Performance Comparison: Traditional Assays vs. Next-Generation Platforms
The evolution of α-synuclein detection technologies has significantly enhanced sensitivity, allowing for earlier disease identification and the use of more accessible biofluids like blood plasma. The table below summarizes the key performance metrics of various diagnostic platforms.
Table 1: Performance Comparison of α-Synuclein Detection Platforms
| Technology / Platform | Detection Mechanism | Sample Type | Detection Limit | Key Advantages |
|---|---|---|---|---|
| Traditional ELISA [22] [38] | Enzyme-linked colorimetric assay | CSF, Plasma | ~10-100 ng/mL (general for proteins) | Well-established, standardized |
| Seed Amplification Assays (SAA) [36] [39] | Amplification of misfolded protein seeds | CSF, Skin biopsy | Qualitative (Presence/Absence) | High correlation with clinical diagnosis, detects pathological forms |
| SIMOA [38] | Digital immunoassay (fluorescence) | CSF, Plasma | Femtomolar range | Ultra-high sensitivity, quantifies low concentrations in blood |
| Electrochemical Nanobiosensor [40] | Impedance spectroscopy (Electrochemical) | Plasma | 0.08 pg/mL | Extreme sensitivity, low-cost, point-of-care potential |
| PET Tracers [37] | Molecular imaging | In vivo (Brain) | N/A (Spatial distribution) | Direct in vivo visualization, regional distribution |
The data reveals a clear trend: nanobiosensor technology achieves detection limits that are orders of magnitude lower than traditional methods like ELISA. For instance, a specific electrochemical nanobiosensor demonstrated a limit of detection of 0.08 pg/mL in human plasma, a sensitivity level that reliably allows for discrimination between healthy individuals and PD patients [40]. This is crucial because α-synuclein concentrations in blood plasma are typically very low, reported as 0.157 ± 0.285 pg·mL⁻¹ for healthy controls [40]. Furthermore, while Seed Amplification Assays are groundbreaking for detecting the pathological form of α-synuclein, they are primarily qualitative [39]. In contrast, nanobiosensors and SIMOA provide quantitative data, which is more valuable for tracking changes in biomarker levels over time.
Experimental Protocols for Key Technologies
Protocol: α-Synuclein Electrochemical Nanobiosensor
This protocol details the fabrication and operation of a highly sensitive hierarchical nanowire-based electrode for detecting α-synuclein in plasma, as presented in the search results [40].
- 1. Electrode Fabrication: Begin with a cleaned PET-ITO substrate. Synthesize ZnO nanowires arranged as nanostars (NS) using a chemical bath deposition (CBD) method. Decorate the ZnO NSs with gold nanoparticles (Au NPs) via electrodeposition from a HAuCl₄ solution. Grow a layer of poly-glutamic acid through electro-polymerization onto the Au NP/ZnO NS structure.
- 2. Biorecognition Immobilization: Functionalize the sensor surface by covalently attaching anti-α-synuclein antibodies to the poly-glutamic acid layer. This is typically achieved using carbodiimide crosslinker chemistry (e.g., EDC/NHS). Block non-specific binding sites with Bovine Serum Albumin (BSA).
- 3. Sample Incubation & Measurement: Incubate the functionalized biosensor with a prepared sample of human plasma. After a washing step to remove unbound material, the electrochemical measurement is performed using a solution of Fe(II)(CN)₆⁴⁻/Fe(III)(CN)₆³⁻ as a redox probe. The binding of α-synuclein to the immobilized antibody increases the electrical impedance at the electrode surface.
- 4. Data Analysis: The change in charge transfer resistance (Rₑₜ) is measured via Electrochemical Impedance Spectroscopy (EIS). This change is correlated with the concentration of α-synuclein in the sample using a pre-established calibration curve, which is linear in the range of 0.5 to 10 pg·mL⁻¹ [40].
Protocol: Seed Amplification Assay (SAA) for Misfolded α-Synuclein
This protocol outlines the general principles for detecting pathological α-synuclein aggregates, a method highlighted in recent research updates [36] [39].
- 1. Sample Preparation: Cerebrospinal fluid (CSF) is collected via lumbar puncture and prepared with a buffer to maintain protein stability.
- 2. Seeding Reaction: The CSF sample is mixed with a solution containing recombinant α-synuclein monomer substrate and an energy source (e.g., buffer salts). The mixture is subjected to cycles of agitation and incubation in a thermostated plate reader. If pathological α-synuclein "seeds" are present in the CSF sample, they will template the conversion and aggregation of the monomeric substrate into amyloid fibrils.
- 3. Signal Detection: The formation of aggregates is monitored in real-time using a fluorescent dye, such as Thioflavin T (ThT), which intercalates into amyloid fibrils and exhibits enhanced fluorescence. Samples are classified as positive or negative based on the fluorescence reaching a predetermined threshold within the assay time.
- 4. Data Interpretation: The kinetic parameters of the aggregation (e.g., lag time, maximum fluorescence) can provide information on the concentration and seeding activity of the pathological α-synuclein in the original sample. It is noted that while SAA strongly correlates with symptoms, it does not reliably predict disease progression on its own [39].
Diagnostic Pathways and Technology Integration
The following diagram visualizes the integrated diagnostic and research workflow for synucleinopathies, incorporating both established and emerging technologies.
Diagnostic and Research Workflow for Synucleinopathies
The Scientist's Toolkit: Key Research Reagent Solutions
Successful research and development in this field rely on a suite of specialized reagents and materials. The following table catalogues essential components for building advanced diagnostic platforms for α-synuclein detection.
Table 2: Essential Research Reagents for α-Synuclein Biomarker Development
| Reagent / Material | Function / Application | Specific Examples from Literature |
|---|---|---|
| Anti-α-Synuclein Antibodies | Biorecognition element for immunoassays; binds specifically to α-synuclein protein. | Clone 1D22 Rabbit Monoclonal antibody used in electrochemical biosensor functionalization [40]. |
| Functional Nanomaterials | Enhance sensor signal, increase surface area, and improve electron transfer. | Gold nanoparticles (Au NPs), Zinc Oxide Nanostars (ZnO NSs), exfoliated graphene oxide (EGO), carbon nanotubes (CNTs) [22] [40] [41]. |
| CRISPR-Cas Systems | Ultra-sensitive nucleic acid detection; can be adapted for protein biomarkers via aptamer sequences. | Cas proteins with guide RNA (gRNA) used in fluorescence-based biosensors for attomolar-level sensitivity [38]. |
| Recombinant α-Synuclein | Essential substrate for Seed Amplification Assays (SAA); used as a standard for calibration curves. | Used in SAA protocols to amplify pathological seeds from patient CSF [36]. |
| PET Tracer Candidates | Allow for direct in vivo imaging of α-synuclein aggregates in the brain. | Novel tracers from Merck and MGH presented at AD/PD 2025, showing proof-of-concept in humans [37]. |
The comparative data and protocols presented herein strongly support the thesis that nanobiosensors represent a significant leap forward in the accurate detection of neurodegenerative disease biomarkers. The demonstrated ability of electrochemical nanobiosensors to detect α-synuclein at 0.08 pg/mL in plasma underscores a performance advantage over traditional assays, offering a path toward accessible, cost-effective, and ultrasensitive point-of-care diagnostics [40]. However, the diagnostic future is not a winner-takes-all scenario. The research community is moving toward a multimodal approach, where the strengths of different technologies are combined. For example, a 2025 study showed that integrating CSF α-synuclein data with radiomic analysis of T1-weighted images created a model with an AUROC of 0.939 for predicting PD progression, far exceeding the performance of either method alone [42]. The ongoing development of α-synuclein PET tracers [37] and the validation of Seed Amplification Assays [39] will further enrich this diagnostic ecosystem. The convergence of these technologies is paving the way for a biological definition of Parkinson's disease, enabling earlier intervention, precise patient stratification for clinical trials, and ultimately, more effective management of neurodegenerative diseases.
The diagnosis of parasitic infections, particularly those caused by Plasmodium (malaria) and Leishmania (leishmaniasis), is undergoing a revolutionary transformation driven by nanotechnology. Traditional diagnostic methods, while established, face significant limitations in sensitivity, specificity, speed, and applicability in resource-limited settings where these diseases are most prevalent [43] [44]. Globally, leishmaniasis affects 12-15 million people, causing approximately 70,000 deaths annually, while malaria remains a persistent public health threat [44]. The urgent need for more accurate, rapid, and accessible diagnostic tools has catalyzed the development of nanobiosensors—analytical devices that integrate biological recognition elements with nanomaterials to detect pathogens at the molecular level [43]. This guide provides a comprehensive comparison between emerging nanobiosensor technology and conventional diagnostic platforms, focusing specifically on Plasmodium and Leishmania detection. We objectively evaluate their performance based on published experimental data, detail standardized methodological protocols, and provide essential resource information to facilitate research and development in this critical area of infectious disease diagnostics.
Comparative Analysis: Nanobiosensors vs. Traditional Diagnostics
The following tables provide a direct performance comparison between conventional diagnostic methods and emerging nanobiosensor technologies for detecting Plasmodium and Leishmania infections.
Table 1: Overall Performance Comparison of Diagnostic Platforms for Parasitic Infections
| Parameter | Microscopy | ELISA | PCR | Nanobiosensors |
|---|---|---|---|---|
| Sensitivity | Low to Moderate [43] | Moderate to High [43] | Very High [43] | Extremely High (e.g., femtomolar levels) [43] |
| Specificity | Moderate [43] | High (antibody-dependent) [43] | Very High [43] | Extremely High (target-specific probes) [43] |
| Time-to-Result | Minutes to Hours [43] | Several Hours (4-6h) [43] | Hours to Days [43] | Minutes to Hours (real-time potential) [43] |
| Cost | Very Low [43] | Low to Moderate [43] | High [43] | High (nanomaterial synthesis) [43] |
| Throughput | Low (manual process) [43] | Moderate (batch processing) [43] | Low to Moderate [43] | High (multiplexing capability) [43] |
| Ease of Use | Requires expert technician [43] | Standardized protocols [43] | Requires special equipment and skills [43] | Requires technical expertise for operation [43] |
| Point-of-Care Suitability | Limited | Limited | Limited | High (with lab-on-a-chip integration) [43] |
Table 2: Performance of Specific Nanobiosensors for Plasmodium and Leishmania
| Parasite | Nanomaterial Used | Target Biomarker | Reported Sensitivity / LOD | Detection Mechanism |
|---|---|---|---|---|
| Plasmodium | Gold Nanoparticles (AuNPs) [43] | PfHRP2 antigen [43] | Extremely High (for PfHRP2) [43] | Electrochemical / Optical [43] |
| Leishmania | Quantum Dots (QDs) [43] | kDNA probes [43] | Extremely High (for kDNA) [43] | Fluorescence [43] |
| Leishmania | Various Nanomaterials [44] | Antigens, Antibodies, DNA [44] | High (potential for improved accuracy) [44] | Optical / Electrochemical [44] |
Experimental Protocols for Key Methodologies
To ensure reproducibility and provide a clear framework for evaluation, this section outlines the core experimental protocols for both traditional and nanobiosensor-based diagnostic methods.
Traditional Diagnostic Protocol: Microscopy (Gold Standard)
Principle: Direct morphological identification of parasites in stained blood (malaria) or tissue (leishmaniasis) smears using a light microscope [43] [44].
- Sample Preparation:
- Plasmodium: Prepare thin and thick blood smears on a glass slide. The thick smear is used for sensitive detection, while the thin smear allows for species identification. Air-dry the smears [45].
- Leishmania: Prepare tissue aspirates from spleen, bone marrow, lymph nodes, or skin lesions. Smear the aspirate on a glass slide and air-dry [44] [45].
- Staining:
- Fix thin smears (and tissue smears) with methanol. Thick smears are not fixed.
- Stain slides using Giemsa, Wright's, or Leishman stains. Giemsa staining is most common. Incubate the slides with diluted Giemsa stain (e.g., 3-10%) for 15-30 minutes [45].
- Examination:
- Rinse the slides gently with water and air-dry.
- Examine under a light oil-immersion objective (1000x magnification).
- For malaria, identify intraerythrocytic parasites. For leishmaniasis, identify amastigotes within macrophages [44].
- Analysis: The result is based on the visual confirmation of parasite morphology by a skilled technician. Sensitivity is highly dependent on parasite load and technician expertise [43] [44].
Nanobiosensor Protocol: Quantum Dot-Based Fluorescent DNA Sensor
Principle: Fluorescence detection of specific parasite DNA sequences using quantum dots (QDs) as fluorescent probes. For example, QDs can be labeled with DNA probes complementary to Leishmania kinetoplast DNA (kDNA) [43].
- Probe Functionalization:
- Activate the carboxyl groups on the surface of water-soluble QDs (e.g., CdSe/ZnS core-shell) using EDC/NHS chemistry.
- Incubate the activated QDs with amine-modified DNA probes specific to the target parasite sequence (e.g., Leishmania kDNA). Purify the QD-DNA conjugates via centrifugation or chromatography [46].
- Sample DNA Extraction and Preparation:
- Extract DNA from patient whole blood or tissue samples using a commercial kit.
- The extracted DNA may be amplified via PCR or isothermal amplification (e.g., LAMP) for low-parasite-load samples to enhance sensitivity, though direct detection is the ultimate goal [44].
- Hybridization and Detection:
- Incubate the sample DNA with the QD-DNA probe conjugates under optimal hybridization conditions (specific buffer, temperature, and time).
- If the target DNA sequence is present, it hybridizes with the probe on the QD surface.
- Wash the mixture to remove unbound DNA and probes.
- Signal Measurement:
- Excite the QDs at a specific wavelength using a spectrophotometer or a microplate reader. A single wavelength can excite different QDs [46].
- Measure the fluorescence emission intensity. The signal intensity is proportional to the amount of target DNA captured.
- The narrow, symmetrical emission spectrum of QDs allows for multiplexing by using different colored QDs targeting different DNA sequences simultaneously [46].
Nanobiosensor Protocol: Gold Nanoparticle (AuNP)-Based Electrochemical Immunosensor
Principle: Electrochemical detection of a specific parasite antigen, such as Plasmodium falciparum histidine-rich protein 2 (PfHRP2), using AuNPs to enhance the electrode surface and signal [43].
- Immunosensor Fabrication:
- A working electrode (e.g., glassy carbon or gold electrode) is polished and cleaned.
- The electrode is modified with a nanocomposite material, such as AuNPs, to increase its surface area and electrical conductivity [43] [47].
- A capture antibody (e.g., anti-PfHRP2) is immobilized onto the AuNP-modified electrode surface. The surface is then blocked with bovine serum albumin (BSA) to prevent non-specific binding [43].
- Sample Incubation and Antigen Capture:
- A liquid patient sample (e.g., blood, serum) is applied to the functionalized electrode.
- The target antigen (e.g., PfHRP2) in the sample binds to the capture antibody on the electrode surface.
- The electrode is washed with a buffer to remove unbound materials.
- Signal Generation and Measurement:
- A detection antibody, which is also specific to the target antigen and conjugated with an enzyme label (e.g., horseradish peroxidase - HRP), is added. This forms an antibody-antigen-antibody "sandwich" complex on the electrode.
- An electrochemical substrate (e.g., TMB/H₂O₂ for HRP) is added.
- The enzymatic reaction produces an electroactive product. The AuNPs enhance the electron transfer in this reaction [47].
- An electrochemical technique, such as amperometry or electrochemical impedance spectroscopy (EIS), is used to measure the resulting current or impedance change [43] [47]. The signal is correlated with the antigen concentration in the sample.
Visualizing Diagnostic Pathways
The following diagrams illustrate the logical workflows and core principles of the diagnostic methods discussed, highlighting the key differences between traditional and nanotechnology-enhanced approaches.
Workflow for Parasite Detection Methods
Core Principle of a Nanobiosensor
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Nanobiosensor Development
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Gold Nanoparticles (AuNPs) [43] | Signal amplification in electrochemical and optical (e.g., SPR, colorimetric) sensors; platform for bioreceptor immobilization. [43] [47] | Excellent conductivity, biocompatibility, tunable optical properties, easy functionalization. [47] |
| Quantum Dots (QDs) [43] [46] | Fluorescent labels in optical biosensors for DNA (genosensors) and antigen detection. Enable multiplexing. [43] [46] | High quantum yield, narrow emission bands, size-tunable emission, resistance to photobleaching. [46] |
| Carbon Nanotubes (CNTs) [43] | Electrode modification to enhance surface area and electron transfer in electrochemical sensors. [43] [47] | High electrical conductivity, large surface-to-volume ratio, mechanical strength. [43] |
| Graphene Oxide (GO) [43] | Platform in optical and electrochemical biosensors; quencher in fluorescence-based assays. [43] [47] | Large surface area, excellent water dispersibility, rich functional groups for bioconjugation. [47] |
| Specific Bioreceptors | Provide selectivity by binding the target analyte (antigen, DNA, antibody). [43] | High affinity and specificity are critical. Includes monoclonal/polyclonal antibodies and DNA/aptamer probes. |
| EDC/NHS Chemistry | Standard crosslinking method for covalently immobilizing bioreceptors (e.g., antibodies) onto nanomaterial surfaces. [46] | Activates carboxyl groups for conjugation with primary amines; fundamental for biosensor fabrication. |
Point-of-Care and Lab-on-a-Chip Integration for Rapid Field Deployment
The field of medical diagnostics is undergoing a transformative shift from centralized laboratory testing toward decentralized, rapid analysis at the point-of-care (POC). This evolution is largely driven by the integration of Lab-on-a-Chip (LoC) technologies, which miniaturize and integrate complex laboratory functions onto a single, portable device [48] [49]. For researchers and drug development professionals, the critical question is how these emerging systems perform against established diagnostic methods, particularly within the context of a broader thesis comparing nanobiosensors and traditional diagnostics. The driving vision, termed QUICK-PCR (Quick, Ubiquitous, Integrated, Cost-efficient molecular diagnostic kit), aims to deliver diagnostic systems embodying six key principles: simplicity, speed, small size, sustainability, sensitivity, and specificity [50]. This guide provides an objective comparison of the performance, experimental protocols, and core components of these integrated systems to inform research and development directions.
Performance Comparison: Traditional Diagnostics vs. POC-LoC Integration
The following tables provide a quantitative and qualitative comparison of diagnostic technologies, highlighting the performance of integrated POC-LoC systems against traditional methods and emerging nanobiosensors.
Table 1: Overall Technology Platform Comparison
| Parameter | Centralized Laboratory (qPCR) | Integrated POC-LoC (QUICK-PCR Goal) | Isothermal Amplification (LAMP/RPA) | Nanobiosensors |
|---|---|---|---|---|
| Assay Time | 1-4 hours (includes transport) [50] | Target: < 30 minutes [50] | 15-60 minutes [50] | Minutes [22] |
| Sensitivity | High (aM-zM) | High (targeting lab-equivalent) [50] | High, but prone to false positives [50] | Ultra-high (fM-aM) [22] |
| Specificity | High | High (PCR gold standard) [50] | Moderate (challenges with primer-dimer) [50] | High (highly specific biorecognition) [22] |
| Multiplexing Capability | High | Developing (microfluidics enable) [51] | Low (LAMP requires 6 primers) [50] | High (multiple biomarker panels) [22] |
| Sample Volume | mL-scale | µL-scale [52] | µL-scale | µL to nL-scale [22] |
| Equipment Cost | High (>$10k) | Target: Low (cost-efficient) [50] | Moderate | Varies (nanomaterial costs) [22] |
| User Skill Level | Skilled technician | Minimal training [50] | Minimal training | Minimal training |
Table 2: Analytical Performance of Nanobiosensors vs. Traditional Techniques Data adapted from research on neurodegenerative disease biomarkers [22]
| Detection Method | Target Biomarker | Detection Limit | Traditional Method (for comparison) | Traditional Method Detection Limit |
|---|---|---|---|---|
| Electrochemical Aptamer Sensor [22] | miRNA-195 (Parkinson's) | 10 pM | RT-qPCR | ~pM range |
| Antibody-based Voltammetric Sensor [22] | Tau protein (Alzheimer's) | 10 aM (attomolar) | ELISA | 10-100 ng/mL (≈ pM-nM range) |
| Surface Plasmon Resonance Aptamer Sensor [22] | α-synuclein (Parkinson's) | 0.64 fM (femtomolar) | Immunoassay | Low nM range |
| Colorimetric Aptamer Sensor [22] | General biomarker | 1 nM | Visual Lateral Flow | nM-µM range |
Experimental Protocols for Key POC-LoC Technologies
To validate the performance of integrated systems, rigorous experimental protocols are employed. The following methodologies are commonly cited in the literature for benchmarking new diagnostic technologies.
Protocol 1: Microfluidic Chip-based Digital PCR (cdPCR) for Absolute Quantification
This protocol is used to achieve a high sensitivity and absolute quantification of nucleic acids without a standard curve, making it suitable for low-abundance targets [50].
- Chip Fabrication: Fabricate a microfluidic chip containing thousands of microwells using soft lithography with Polydimethylsiloxane (PDMS) or injection molding with Cyclic Olefin Copolymer (COC).
- Sample Partitioning: Dilute the purified nucleic acid sample in a master mix containing DNA polymerase, dNTPs, primers, and a fluorescent DNA-binding dye (e.g., EVAGreen). Use a microfluidic pump or capillary forces to load the sample mixture into the microwells, ensuring a statistical distribution of 0 or 1 target molecule per well.
- Thermal Cycling: Place the chip on a miniaturized, integrated thermal cycler. Run the following PCR protocol for 40 cycles:
- Denaturation: 95°C for 10 seconds.
- Annealing/Extension: 60°C for 30 seconds.
- Endpoint Fluorescence Imaging: After thermal cycling, use a compact fluorescent reader or a smartphone-based imaging system to capture an image of the entire chip. Wells containing amplified target DNA (positive) will fluoresce.
- Data Analysis: Use software to count the number of fluorescent (positive) and non-fluorescent (negative) wells. Apply Poisson statistics to the ratio of positive to total wells to calculate the absolute concentration of the target nucleic acid in the original sample.
Protocol 2: Electrochemical Nanobiosensor Detection of miRNA
This protocol details the use of functionalized electrodes for detecting specific miRNA biomarkers, demonstrating the potential for ultra-high sensitivity in POC settings [22].
- Electrode Functionalization:
- Start with a screen-printed carbon electrode.
- Modify the electrode surface by drop-coating with a nanocomposite of gold nanowires (GNWs) and exfoliated graphene oxide (EGO) to enhance surface area and electrochemical conductivity.
- Immobilize a thiolated, single-stranded DNA probe sequence that is complementary to the target miRNA (e.g., miR-195 for Parkinson's) onto the GNWs via gold-thiol bonding.
- Hybridization and Incubation:
- Incubate the functionalized electrode with a sample solution (e.g., diluted serum or cerebrospinal fluid) for 15-20 minutes to allow the target miRNA to hybridize with its complementary probe.
- Wash the electrode thoroughly to remove unbound molecules.
- Electrochemical Signal Generation:
- Immerse the electrode in a solution containing doxorubicin, which acts as an electrochemical indicator. Doxorubicin intercalates specifically into the double-stranded DNA-RNA hybrid.
- Use Differential Pulse Voltammetry (DPV) to measure the electrochemical signal from the intercalated doxorubicin. The peak current is proportional to the amount of hybridized target miRNA.
- Quantification:
- Generate a calibration curve by plotting the DPV peak current against the logarithm of the concentration of a synthetic miRNA standard.
- Use this curve to determine the concentration of the target miRNA in unknown samples.
Signaling Pathways and Experimental Workflows
The integration of POC and LoC devices involves a defined sequence of steps, from sample introduction to result delivery. The following diagram visualizes this integrated workflow and the data analysis pipeline incorporating Artificial Intelligence (AI).
Figure 1: Integrated POC-LoC and AI workflow. The main horizontal flow shows the sample-to-answer process on the microfluidic device. The raw signal from the biosensor detector is fed into an AI/ML algorithm for enhanced analysis, which supports clinical decision-making [52] [51].
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and operation of POC-LoC systems rely on a suite of specialized reagents and materials. The following table details key components and their functions in experimental setups.
Table 3: Essential Research Reagents and Materials for POC-LoC Development
| Item Name | Function/Description | Application Example |
|---|---|---|
| Functionalized Nanomaterials | Enhance signal transduction and provide a high surface area for biorecognition element immobilization. | Gold nanoparticles, quantum dots, and carbon nanotubes are used in electrochemical and optical nanobiosensors to improve sensitivity [52] [22]. |
| Biorecognition Elements | Provide high specificity by binding to the target analyte. | Antibodies, aptamers, and enzymes are immobilized on sensor surfaces or microfluidic channels to capture specific biomarkers or pathogens [22]. |
| Microfluidic Chips/Cartridges | The disposable core that integrates fluidic channels, chambers, and sensors to automate the assay. | Made from polymers (e.g., PDMS, COC) via soft lithography or injection molding; pre-loaded with reagents for sample preparation, amplification, and detection [50] [53]. |
| Lyophilized Reagent Pellets | Stable, room-temperature storage of assay reagents. | PCR or isothermal amplification master mixes (polymerases, dNTPs, primers) are pre-deposited in reaction chambers to simplify the user workflow and enhance shelf-life [50]. |
| Signal Generation Reagents | Produce a measurable signal (optical, electrochemical) upon target detection. | Fluorescent dyes (SYBR Green), intercalating agents (doxorubicin), and enzyme substrates (TMB) generate a quantifiable signal proportional to the target concentration [50] [22]. |
The integration of Point-of-Care and Lab-on-a-Chip technologies represents a significant leap forward for rapid field deployment of diagnostic capabilities. The experimental data and performance comparisons presented in this guide demonstrate that while traditional laboratory methods like qPCR remain the gold standard for sensitivity and specificity, integrated POC-LoC systems are rapidly closing this performance gap. Furthermore, the incorporation of nanobiosensors offers a pathway to potentially surpass traditional methods in sensitivity for specific applications, such as detecting ultra-low abundance biomarkers [22]. The ongoing integration of Artificial Intelligence (AI) and machine learning for data analysis, pattern recognition, and predictive analytics further enhances the value proposition of these systems, transforming them from simple diagnostic tools into sophisticated clinical support systems [52] [51]. For researchers and drug development professionals, the future lies in addressing the remaining challenges of manufacturing scalability, reagent stability, and regulatory compliance to fully realize the potential of these transformative technologies.
The Rise of Multiplexed Sensors for Simultaneous Multi-Analyte Detection
The landscape of diagnostic testing is undergoing a transformative shift from single-analyte detection to sophisticated multiplexed sensing platforms capable of simultaneously measuring multiple biomarkers. This evolution is particularly evident in the direct comparison between emerging nanobiosensors and traditional diagnostic methods, where key differentiators include dramatically improved sensitivity, enhanced specificity, and significantly reduced analysis time. Multiplexed photoelectrochemical (M-PEC) sensors exemplify this advancement, overcoming limitations of traditional single-signal sensors that often struggle with interference and selectivity in complex samples like blood, serum, or environmental samples [54]. The fundamental superiority of these platforms lies in their ability to perform parallel analysis, providing a comprehensive diagnostic profile from minimal sample volume—a crucial advantage for early disease detection, therapeutic monitoring, and point-of-care testing (POCT) in resource-limited settings [55] [56].
The drive toward multiplexing is fueled by clinical reality: most diseases cannot be accurately diagnosed by monitoring a single biomarker. For instance, cancer biomarker miR-21 exhibits abnormal expression levels in multiple cancers, including pancreatic, breast, lung, and prostate cancer [56]. Similarly, carcinoembryonic antigen (CEA), a common biomarker for colorectal cancer, shows elevated levels in numerous other cancers [56]. Simultaneous detection of multiple biomarkers reduces false positives and false negatives, thereby improving diagnostic accuracy while minimizing sample volume requirements, analysis time, and overall cost [56]. This review objectively compares the performance of multiplexed nanobiosensors against traditional diagnostics, supported by experimental data and detailed methodologies, to provide researchers and drug development professionals with a comprehensive analysis of this rapidly advancing field.
Performance Comparison: Multiplexed Nanobiosensors vs. Traditional Diagnostics
Analytical Performance Metrics
The following tables summarize key performance differences between multiplexed nanobiosensors and traditional diagnostic methods across critical parameters, based on published experimental findings.
Table 1: Overall Performance Comparison of Diagnostic Platforms
| Performance Parameter | Traditional Diagnostics | Multiplexed Nanobiosensors | Experimental Evidence |
|---|---|---|---|
| Detection Sensitivity | Moderate to High (e.g., PCR: ~copies/μL) | Very High (fM to aM levels) | SERS-based DNA sensor: 50 fM LOD [56] |
| Multiplexing Capacity | Limited (typically 1-3 analytes) | High (up to 500 analytes with xMAP) | xMAP technology: 500-plex capability [55] |
| Sample Volume Required | High (mL range for some assays) | Low (μL to nL range) | Microfluidic chips: nanoliter volumes [55] |
| Analysis Time | Hours to days | Minutes to hours | Colorimetric nanoarray: <10 minutes [57] |
| Portability/POCT Suitability | Mostly lab-based systems | High with miniaturized platforms | Lateral Flow Assays: fully portable [55] [58] |
Table 2: Specific Experimental Performance Data for Multiplexed Sensors
| Sensor Technology | Target Analytes | Detection Limit | Multiplexing Level | Reference |
|---|---|---|---|---|
| Colorimetric Nanoarray | S. aureus, E. coli | 10 CFU/mL | 2 pathogens | [57] |
| Fluorescence Microarray (AgNPs) | Hepatitis B virus DNA | 50 fM | Single-plex (extendable) | [56] |
| Electrochemical Implantable | Glucose | Clinical range (3-20 mM) | Single-plex (continuous) | [3] |
| Lateral Flow (Triage) | Cardiac markers, Drugs | nM range | Up to 3 analytes | [55] |
| M-PEC Sensors | Biomolecules, Metal ions | Unspecified trace-level | Wavelength/spatial-resolved | [54] |
Diagnostic Accuracy in Clinical Applications
The superior accuracy of multiplexed nanobiosensors is particularly evident in applications where traditional methods face limitations:
Infectious Disease Diagnostics: Traditional pathogen detection methods like culture techniques (2-3 days for results), immunoassays (false-positive rate >15%), and PCR (requires skilled operators) are being superseded by optical biosensors that offer rapid, sensitive, multiplexed identification. For instance, a slidable paper-embedded plastic optical biosensor utilizing colorimetric detection and loop-mediated isothermal amplification (LAMP) technology successfully detected Salmonella, Staphylococcus aureus, and Escherichia coli O157:H7 simultaneously, demonstrating specificity and rapid results crucial for food safety and clinical diagnostics [57].
Parasitic Infection Detection: Traditional methods for diagnosing parasitic infections (microscopy, ELISA, PCR) suffer from limitations in sensitivity, specificity, and accessibility. Nanobiosensors utilizing various nanomaterials (gold nanoparticles, carbon nanotubes, quantum dots) have demonstrated efficient and vulnerable detection of helminth antigens or genetic material, significantly improving diagnostic reliability. For example, nanobiosensors functionalized with anti-EgAgB antibodies showed enhanced detection capabilities for Echinococcus antigens compared to conventional ELISA [59].
Cancer Diagnostics: The ability to detect multiple cancer biomarkers simultaneously addresses a critical limitation of single-analyte tests. While individual cancer biomarkers may exhibit cross-reactivity across multiple cancer types, measuring panels of biomarkers simultaneously significantly improves diagnostic specificity. Optical nanosensors employing fluorescence, SERS, and colorimetric detection have been developed for simultaneous detection of multiple cancer biomarkers, though clinical validation studies are ongoing [56].
Experimental Protocols: Methodologies for Multiplexed Detection
Protocol 1: Multiplexed Pathogen Detection Using Colorimetric Nanoparticles
This protocol adapts the experimental approach described by Wen et al. for simultaneous detection of multiple pathogens using magnetically separated plasmon nanoparticles [57].
Principle: Different colored plasmonic nanoparticles (red gold nanoparticles for SARS-CoV-2, yellow silver nanoparticles for S. aureus, blue silver triangle nanoparticles for Salmonella) are conjugated with specific antibodies. When target pathogens are present, sandwich complexes form with magnetic particles and are separated magnetically, producing supernatant color changes indicative of specific infections.
Materials Required:
- Gold Nanoparticles (AuNPs): 20 nm diameter, for conjugation with anti-SARS-CoV-2 antibodies
- Silver Nanoparticles (AgNPs): Spherical (20 nm) and triangular (50 nm edge length) for conjugation with anti-S. aureus and anti-Salmonella antibodies respectively
- Magnetic Beads: Carboxylated superparamagnetic beads (1-2 μm) conjugated with capture antibodies
- Phosphate Buffered Saline (PBS): 10 mM, pH 7.4, for washing and dilution
- Blocking Buffer: PBS with 1% BSA for minimizing non-specific binding
Procedure:
- Nanoparticle Functionalization:
- Prepare three separate batches of nanoparticles (red AuNPs, yellow spherical AgNPs, blue triangular AgNPs)
- Conjugate each nanoparticle type with specific detection antibodies via EDC-NHS chemistry
- Purify conjugated nanoparticles using centrifugation (14,000 × g, 20 minutes) and resuspend in storage buffer
Magnetic Bead Preparation:
- Conjugate magnetic beads with capture antibodies specific to each target pathogen
- Block remaining active sites with blocking buffer for 1 hour at room temperature
- Wash three times with PBS and resuspend in assay buffer
Assay Procedure:
- Mix 100 μL sample with 50 μL of mixed magnetic beads and incubate for 15 minutes with shaking
- Add 50 μL of mixed color reporter nanoparticles and incubate for additional 15 minutes
- Apply magnetic separation for 5 minutes to pull down sandwich complexes
- Transfer supernatant to clean microplate well
- Image color changes using standard scanner or smartphone camera
- Analyze color patterns using RGB analysis software
Validation: The method demonstrated effective discrimination between individual and mixed infections of SARS-CoV-2, S. aureus, and Salmonella with distinct color signatures for each combination.
Protocol 2: Fluorescence-Based Multiplexed DNA Detection Using Metal-Enhanced Fluorescence
This protocol is based on the enzyme-free fluorescence microarray employing silver nanoparticle aggregates for hepatitis B virus DNA detection [56], with adaptability to other nucleic acid targets.
Principle: Silver nanoparticle (AgNP) aggregates create plasmonic hotspots that significantly enhance fluorescence signals via metal-enhanced fluorescence (MEF), enabling detection limits down to 50 fM with over 1500-fold signal amplification compared to unenhanced fluorescence.
Materials Required:
- Silver Nanoparticles (AgNPs): 40-60 nm diameter, citrate-stabilized
- Fluorescent Probes: DNA oligonucleotides labeled with Cy5 or similar fluorophores
- Microarray Substrate: Functionalized glass slides with amine or epoxy groups
- Hybridization Buffer: 5× SSC with 0.1% SDS
- Wash Buffers: 2× SSC/0.1% SDS and 0.1× SSC
Procedure:
- AgNP Aggregate Formation:
- Mix AgNPs with NaCl solution (final concentration 50 mM) to induce controlled aggregation
- Monitor aggregation by UV-Vis spectroscopy until broad plasmon band appears at 600-800 nm
- Stabilize aggregates with thiolated polyethylene glycol (SH-PEG)
Microarray Fabrication:
- Spot capture DNA probes onto functionalized glass slides using microarray spotter
- Include appropriate controls (positive, negative, calibration spots)
- Immobilize probes by UV crosslinking or baking according to slide manufacturer's protocol
- Block slides with BSA solution to minimize non-specific binding
Detection Procedure:
- Apply sample (50 μL) containing target DNA to microarray chamber
- Hybridize for 60 minutes at appropriate temperature (based on probe Tm)
- Wash sequentially with: 2× SSC/0.1% SDS (5 minutes), 0.1× SSC (2 minutes × 2)
- Apply AgNP aggregates in hybridization buffer and incubate for 30 minutes
- Wash gently with 0.1× SSC to remove unbound aggregates
- Scan slides using fluorescence microarray scanner with appropriate laser/excitation filters
- Quantify fluorescence intensity using image analysis software
Optimization Notes: The distance between fluorophore and metallic surface must be carefully controlled (optimal separation ~7-8 nm) as closer proximity can induce quenching through non-radiative energy transfer rather than enhancement [56].
Technology Workflows: From Sample to Result
Multiplexed Optical Biosensing Workflow
Multiplexed Biosensing Workflow
Nanomaterial Enhancement Mechanisms
Nanomaterial Enhancement Mechanisms
Research Reagent Solutions: Essential Materials for Multiplexed Sensing
Table 3: Key Research Reagents for Developing Multiplexed Nanobiosensors
| Reagent Category | Specific Examples | Function in Multiplexed Detection | Commercial Sources/Alternatives |
|---|---|---|---|
| Plasmonic Nanoparticles | Gold nanorods, Silver nanotriangles, Core-shell nanoparticles | Generate distinct LSPR signals for wavelength-resolved multiplexing; enhance fluorescence via MEF | Sigma-Aldrich, NanoComposix |
| Fluorescent Nanomaterials | Quantum dots (CdSe/ZnS), Carbon dots, Upconversion nanoparticles | Provide narrow, tunable emission peaks for multiple analyte tracking | Thermo Fisher, NN-Labs |
| Magnetic Beads | Carboxylated superparamagnetic beads, Streptavidin-coated beads | Enable sample preparation, concentration, and separation of multiple targets | Thermo Fisher, Millipore Sigma |
| Capture Molecules | Antibodies, Aptamers, Molecularly imprinted polymers (MIPs) | Provide specific recognition for multiple targets in parallel | Custom synthesis, Abcam, Integrated DNA Technologies |
| Signal Amplification Reagents | Enzyme-polymer conjugates, Catalytic nanomaterials, DNA amplification reagents | Enhance detection sensitivity for low-abundance targets in multiplexed panels | Abcam, New England Biolabs |
| Microfluidic Chip Materials | PDMS, PMMA, Paper substrates | Enable spatial separation and fluidic control for multiplexed assays | Microfluidic chip foundries |
Multiplexed sensors for simultaneous multi-analyte detection represent a significant advancement over traditional diagnostic methods, offering superior sensitivity, specificity, and comprehensive profiling capabilities. The integration of nanomaterials with advanced transduction mechanisms and multiplexing strategies has enabled detection platforms that were not possible with conventional technologies. Future developments will likely focus on increasing multiplexing capacity while simplifying platform design, improving quantitative capabilities, and enhancing connectivity for real-time data analysis [54] [60]. The convergence of AI-assisted design, novel nanomaterials, and microfluidics will further propel this field toward clinical translation, ultimately enabling personalized health monitoring and precision medicine applications that surpass the capabilities of traditional diagnostic approaches.
Navigating Challenges and Optimization Strategies for Clinical Translation
Addressing High Production Costs and Complex Nanofabrication Processes
The transition of nanobiosensors from sophisticated research prototypes to commercially viable and clinically adopted diagnostic tools is critically dependent on overcoming two interconnected challenges: high production costs and complex nanofabrication processes. Within the broader research on nanobiosensors versus traditional diagnostics accuracy, these economic and manufacturing barriers are not merely logistical concerns but fundamental factors that influence the scalability, reproducibility, and ultimate practicality of these advanced diagnostic platforms. While the superior sensitivity and specificity of nanobiosensors, often enabling single-molecule detection, are well-documented in controlled laboratory settings [28], their widespread adoption is constrained by the financial and technical overhead of their manufacture. This analysis objectively compares the cost structures and fabrication methodologies of nanobiosensors against traditional diagnostics, providing a data-driven perspective for researchers and drug development professionals aiming to navigate this evolving landscape.
Comparative Analysis: Fabrication Methods and Associated Costs
The fabrication of nanobiosensors relies on a suite of advanced nanofabrication techniques, which can be broadly categorized into top-down and bottom-up approaches. The choice of method significantly impacts not only the final device performance but also the production cost, scalability, and suitability for specific applications.
Table 1: Comparison of Primary Nanofabrication Approaches
| Fabrication Approach | Key Methods | Relative Cost | Scalability | Technical Challenges | Best Suited For |
|---|---|---|---|---|---|
| Top-Down | Mechanical milling [61], Plasma etching [61], Electron-beam lithography | High | Moderate to High | Lack of control over shape/structure, defect introduction, waste generation [61] | Creating nanostructures from bulk materials, large-area electronics [61] |
| Bottom-Up | Chemical vapor deposition [28], Hydrothermal processing [28], Sol-gel [28] | Moderate | Low to Moderate | Reproducibility at industrial scale, process control during self-assembly [61] | High-quality nanomaterials with controlled properties [61] |
| Hybrid & Emerging | Nano-OPS printing [62], Flame-sprayed nanoparticles [63] | Varies (Potentially Lower) | High (Potential) | Process optimization, integration with existing workflows | High-throughput, inexpensive manufacturing for IoT and sensing [62] |
The high costs associated with these "hi-tech nano sensors" are a significant market restraint [63]. These costs are driven by the complexity of the manufacturing process, which requires intricate fabrication techniques, specialized equipment, and skilled labor [63]. Furthermore, fluctuations in the price and availability of raw nanomaterials add to cost variability, making it difficult to maintain competitive and consistent pricing [63].
Experimental Protocols for Cost and Performance Analysis
To objectively compare the performance of nanobiosensors against traditional diagnostic methods, controlled experiments are essential. The following protocols outline methodologies for evaluating key parameters, including sensitivity, limit of detection (LOD), and production throughput.
Protocol 1: Evaluating Limit of Detection (LOD) for a Glucose Biosensor
This protocol is designed to compare the performance of an intravascular nanobiosensor against a traditional blood glucose monitor.
- Objective: To determine and compare the LOD and dynamic range of a novel intravascular nanobiosensor (e.g., the GlySure Ltd. system [3]) versus a standard finger-prick glucometer.
- Materials:
- Nanobiosensor: Intravascular continuous glucose monitoring (CGM) system with a diboronic acid-based receptor [3].
- Traditional Sensor: Commercial electrochemical strip-based glucometer.
- Analytes: Serial dilutions of D-glucose in human plasma, spanning hypoglycemic to hyperglycemic concentrations (2.0-30.0 mmol/L).
- Reference Instrument: Clinical-grade blood gas analyzer or laboratory glucose oxidase reference method.
- Methodology:
- Calibration: Calibrate both the intravascular CGM and the traditional glucometer according to manufacturer specifications.
- Sample Measurement: For each glucose concentration in the series, simultaneously measure the glucose level using the CGM (via a central venous catheter [3]), the traditional glucometer (via a single drop of the plasma solution), and the reference instrument.
- Data Collection: Record triplicate measurements for each device at each concentration.
- Data Analysis: Plot the measured signal (e.g., fluorescence intensity for CGM [3], electrical current for the strip) against the reference glucose concentration. The LOD is calculated as 3σ/s, where σ is the standard deviation of the blank signal and s is the slope of the calibration curve.
- Expected Outcome: The intravascular nanobiosensor is expected to demonstrate a lower LOD and a wider dynamic range, providing more reliable data in critically ill patients, as suggested by studies [3]. The traditional glucometer may show higher variance at extremely low and high concentrations.
Protocol 2: Throughput Analysis of a High-Rate Nano-Manufacturing Process
This protocol assesses the scalability and cost-efficiency of an emerging fabrication tool.
- Objective: To quantify the throughput and cost-per-device of the Nano-OPS Printer, a high-rate nano-manufacturing tool [62], versus conventional lithography for producing simple nanosensor elements.
- Materials:
- Equipment: Nano-OPS Printer research tool [62], standard electron-beam lithography system.
- Substrates: Flexible electronic backplanes or silicon wafers.
- Materials: Conductive nanoparticle inks, standard photoresists.
- Methodology:
- Process Setup: Design a simple electrode pattern. Optimize the printing process for the Nano-OPS tool and the lithography recipe for the e-beam system.
- Production Run: Fabricate the pattern on 1000 substrates using each method, tracking the total time required.
- Cost Calculation: Factor in equipment depreciation, material consumption, labor, and energy costs for both runs to determine a cost-per-device.
- Quality Control: Use microscopy (e.g., SEM) to analyze the feature geometry and repeatability of the fabricated devices from both methods.
- Expected Outcome: The Nano-OPS Printer is designed to achieve an "order of magnitude reduction in costs over conventional fabrication processes" [62] and is expected to show significantly higher throughput and lower cost-per-device, though potentially with a trade-off in minimal feature size compared to e-beam lithography.
Quantitative Data: Market Trends and Economic Drivers
The economic landscape for nanosensors reveals both the growth potential and the financial challenges of the field. The global nanosensors market, valued at USD 832.28 million in 2024, is projected to grow at a CAGR of 8.25% to reach approximately USD 1,838.11 million by 2034 [63]. This growth is propelled by the healthcare industry's demand for miniaturized, sensitive, and rapid diagnostic tools [63]. The pressing need to reduce the average time for detection and diagnosis is an indirect driver favoring the adoption of faster nanosensor technologies [63].
Table 2: Nanosensors Market Data and Application Segmentation
| Parameter | 2024 Data | Projected Growth & Trends | Source |
|---|---|---|---|
| Global Market Size | USD 832.28 Million | USD 1,838.11 Million by 2034 (CAGR 8.25%) | [63] |
| Leading Product Type | Electrochemical Sensors (45.50% share) | Electromagnetic segment (CAGR 8.93%) growing rapidly | [63] |
| Dominant Application | Healthcare (30% share) | Defense & Military segment (CAGR 9.43%) is fastest-growing | [63] |
| Key Regional Market | North America (33% share) | Asia-Pacific to expand at fastest CAGR (9.32%) | [63] |
| Nanofabrication Market | --- | Projected CAGR of 10.1% (2026-2033) | [64] |
Strategies for Cost Mitigation and Process Optimization
The industry and research community are developing multiple strategies to address the inherent cost and complexity challenges.
- High-Throughput Tools: Investing in equipment like the Nano-OPS Printer, which is explicitly designed for "inexpensive, high throughput" nano-fabrication to overcome the "significant bottleneck" of scale-up [62].
- Sustainable & Biological Synthesis: Utilizing eco-friendly biological agents (plants, bacteria, fungi) for nanomaterial synthesis can yield biocompatible, low-toxicity nanostructures, potentially reducing reliance on expensive and harsh chemical processes [28].
- Material Science Advancements: Continuous development of new nanomaterials, such as graphene, carbon nanotubes, and quantum dots, alongside improved functionalization strategies, enhances sensor sensitivity and can lead to more robust and less costly designs [63].
- Regulatory Adaptation: Navigating the "stringent regulatory approvals" from agencies like the FDA and ECHA is a major hurdle [65] [64]. Proactive adaptation to these frameworks, though initially costly, is essential for market entry and can streamline long-term development.
Visualizing the Fabrication Workflow and Challenges
The following diagram illustrates the key decision points and challenges in selecting a nanofabrication pathway, integrating both technical and economic considerations.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Nanobiosensor Fabrication
| Material / Reagent | Function in Fabrication / Experimentation | Example Use Case |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Provide excellent biocompatibility and tunable optical properties for signal transduction [28]. | Functionalized with antibodies for colorimetric detection of target biomarkers. |
| Graphene & Carbon Nanotubes | Offer superior electrical conductivity for electrochemical sensors; high surface area for immobilization [28]. | Used as the sensing electrode in a glucose or cholesterol biosensor [3]. |
| Quantum Dots | Serve as highly photostable fluorescent probes for optical imaging and detection [28]. | Tagging antibodies for single-molecule detection and super-resolution microscopy [28]. |
| Diboronic Acid Receptors | Act as a highly specific recognition element for glucose molecules [3]. | The core sensing chemistry in an intravascular continuous glucose monitor (CGM) [3]. |
| Flame-Sprayed Silver Nanoparticles | Amplify chemical signals (e.g., in SERS) to enhance detection sensitivity and accuracy [63]. | Used on a sensor surface for detecting trace-level pesticides on fruit [63]. |
| Conductive Nanoparticle Inks | Enable printed electronics through high-throughput tools like the Nano-OPS Printer [62]. | Creating electrode patterns for flexible and disposable sensor strips. |
The journey toward making nanobiosensors as economically accessible as they are technologically advanced hinges on a concerted effort to simplify fabrication and reduce costs. While traditional diagnostic methods currently hold an economic advantage, the data shows that the unparalleled sensitivity and potential for miniaturization of nanobiosensors justify the intensive research into overcoming their production challenges. The convergence of high-throughput manufacturing tools like the Nano-OPS Printer [62], innovative biological synthesis methods [28], and advances in material science presents a viable roadmap forward. For researchers and drug developers, the focus must remain on not only achieving diagnostic breakthroughs but also on designing devices and processes that are inherently scalable and cost-effective, ensuring that these powerful tools can transition from the laboratory to global clinical impact.
Overcoming Biological Matrix Interference and Ensuring Signal Stability
The pursuit of diagnostic accuracy is fundamentally a battle against interference and instability. For biosensors, particularly the emerging class of nanobiosensors, the complex mixture of biological components—the biological matrix—in samples like blood, serum, and urine presents a formidable barrier to obtaining reliable, reproducible signals. This biological matrix interference can suppress signals, generate false positives, and irreproducibly alter analyte recovery, ultimately compromising diagnostic accuracy [66] [67]. The broader thesis of comparing nanobiosensors against traditional diagnostics hinges on how these technologies manage this universal challenge. While traditional methods often rely on extensive sample preparation to mitigate matrix effects, nanotechnology offers innovative strategies to enhance signal stability and specificity at the point of detection [3] [68]. This guide objectively compares the performance of different technological approaches to overcoming matrix interference, providing a structured analysis of experimental data and methodologies relevant to researchers and drug development professionals.
Understanding the Challenge: Biological Matrix Effects
Biological matrix interference arises from the competition between target analytes and endogenous matrix components—such as phospholipids, proteins, and electrolytes—during the detection process. In blood plasma or serum, phospholipids are a predominant interferent, notorious for fouling instrumentation and causing matrix-induced ionization suppression in techniques like mass spectrometry due to charge competition in the electrospray source [66]. One study demonstrated that phospholipids can cause up to a 75% reduction in analyte response (e.g., for propranolol), severely impacting sensitivity and reproducibility [66].
The problem is not confined to plasma. Urine presents a highly variable matrix where organic compounds, pH, and electrolytes can significantly interfere with immunoassays. Recovery of proteins spiked into different urine samples can be wildly inconsistent, with documented recovery rates for a single analyte (MIP1α) ranging from 0.3% to 195% across different samples [67]. This variability makes accurate quantification of low-abundance biomarkers exceptionally challenging without effective countermeasures.
Comparative Analysis of Solutions and Performance
Approaches to overcoming matrix effects can be broadly categorized into sample preparation-based methods and sensor-level engineering solutions. The following sections and tables provide a detailed comparison of their performance and applications.
Sample Preparation-Based Methods
These traditional methods focus on purifying or preparing the sample before analysis to remove interfering matrix components.
- Protein Precipitation: A common but relatively crude initial step for protein removal from biological fluids. It often co-precipitates the analyte and fails to remove phospholipids, which continue to cause interference [66].
- Solid-Phase Extraction (SPE): A traditional workhorse for purifying and concentrating analytes. It involves passing the sample through a cartridge to bind analytes, washing away impurities, and then eluting the purified analytes [66].
- Targeted Phospholipid Depletion: This approach uses specialized sorbents, such as hybrid zirconia-silica particles, to selectively isolate phospholipids from plasma or serum via Lewis acid/base interactions. This method specifically targets a key source of interference [66].
- Solid-Phase Microextraction (SPME): An equilibrium-based technique that uses a coated fiber to extract analytes from a sample. Biocompatible SPME (bioSPME) phases can concentrate analytes while shielding the fiber from larger biomolecules, thereby performing simultaneous cleanup and concentration without co-extracting most of the sample matrix [66].
- Sample Dilution: A simple and effective technique for reducing the concentration of matrix components. Its effectiveness depends on the endogenous analyte concentration being high enough to remain above the assay's limit of detection after dilution [67].
Table 1: Comparison of Sample Preparation Methods for Overcoming Matrix Interference
| Method | Principle | Key Performance Data | Advantages | Limitations |
|---|---|---|---|---|
| Targeted Phospholipid Depletion (e.g., HybridSPE) [66] | Selective isolation of phospholipids from plasma/serum. | - Increased analyte response by 4x vs. protein precipitation.- Reduced error bars, improving precision. | - Highly specific to phospholipids.- Effective cleanup without major analyte loss. | - Primarily targets phospholipids; other interferents may remain. |
| Biocompatible SPME (bioSPME) [66] | Equilibrium-based analyte extraction with biocompatible phases. | - 2x higher analyte signal.- 90% lower phospholipid response compared to protein precipitation. | - Simultaneous cleanup and concentration.- Non-exhaustive; multiple extractions from same sample. | - Equilibrium process can be time-consuming.- Requires method optimization. |
| Sample Dilution [67] | Reduces concentration of matrix interferents. | - IL-8 concentration 2-55x higher in diluted (1:10) vs. undiluted urine samples.- Most effective when analytes are well above LoQ. | - Extremely simple and low-cost.- No specialized equipment needed. | - Ineffective for low-abundance analytes (diluted below LoQ).- Can dilute analyte of interest. |
| Standard Addition [67] | Analyte is spiked at different concentrations into the sample matrix. | - Considered a "gold standard" for inhibitory matrices.- Accurate quantification at low concentrations. | - Directly accounts for matrix-specific effects.- High accuracy. | - Time-consuming and labor-intensive.- Requires larger sample volume. |
Sensor-Level and Nanotechnology-Enabled Solutions
Nanobiosensors integrate micro- and nanotechnology to enhance performance directly at the sensing interface, offering a path to reduced sample preparation.
- Functionalized Nanosurfaces: Surfaces can be engineered with molecular receptors (e.g., thiols, boronic acids) that selectively capture target analytes. The use of multiple receptors generates a composite "SERS superprofile," which amplifies subtle spectral differences between chemical analogs, enhancing specificity amidst interference [3] [69].
- Nanomaterial-Enhanced Transducers: The integration of nanomaterials like quantum dots, Ag nanocubes, and carbon nanotubes can dramatically improve sensitivity and signal-to-noise ratios. This allows the transducer to detect smaller changes upon target recognition, making the sensor more robust to matrix effects [3] [69] [68].
- Data-Driven Receptor Selection: Moving beyond trial-and-error, machine learning frameworks can now algorithmically recommend optimal molecular receptors for distinguishing specific analytes. One study achieved over 95% classification accuracy for structurally similar haloanisoles using an XGBoost-powered recommender system [69].
Table 2: Comparison of Sensor-Level Engineering Solutions
| Technology | Principle | Key Performance Data | Advantages | Limitations |
|---|---|---|---|---|
| Multi-Receptor SERS Superprofiles [69] | Combined signals from multiple receptors create a unique fingerprint for each analyte. | - >95% classification accuracy for haloanisole analogs.- Overcomes the "curse of dimensionality" in ML analysis. | - Amplifies minor spectral differences.- High specificity for complex mixtures. | - Requires development of a receptor database.- Complex data analysis. |
| Electrochemical Biosensors [3] | Measure electronic signals from biological reactions (e.g., enzyme-analyte interaction). | - High sensitivity for glucose monitoring.- Enables real-time, continuous monitoring. | - High sensitivity and broad applicability.- Amenable to miniaturization. | - Can be sensitive to chemical interferences. |
| AI/ML-Powered Signal Processing [69] [70] | Uses machine learning to identify patterns and filter out interference from complex signals. | - Generative AI diagnostic accuracy is ~52.1%, performing on par with non-expert physicians [71]. | - Can learn and adapt to complex matrix patterns.- Improves over time with more data. | - Requires large, high-quality datasets for training.- "Black box" decision-making can be a barrier. |
Experimental Protocols for Key Studies
This protocol outlines the method for quantifying and correcting matrix interference in urine using dilution and standard addition.
- Sample Collection: Collect urine samples and characterize baseline matrix components (e.g., Na+, K+, pH, osmolality).
- Spike-and-Recovery Test: Spike known concentrations of target protein standards (e.g., IL-6, IL-8, TNF-α) into the urine matrix.
- Dilution Series: Create a series of dilutions (e.g., neat, 1:2, 1:5, 1:10, 1:20) of both spiked and unspiked urine samples using a standard diluent (e.g., PBS with 0.5% BSA).
- Multiplex Bead Assay: Analyze all samples and standards in quadruplicate using a fluorescence-based multiplex bead array system (e.g., Bio-Rad Bioplex with Luminex technology).
- Data Analysis:
- Recovery Calculation: Calculate percent recovery as: (Interpolated concentration in urine / Interpolated concentration in buffer) × 100.
- Standard Addition: For each sample, spike six known concentrations of the analyte. Plot spike concentration vs. fluorescence intensity. The negative x-intercept of the fitted line gives the endogenous analyte concentration.
- Comparison: Compare the concentrations obtained by the simple dilution method (e.g., at 1:10) against those derived from the standard addition method to validate the dilution approach.
This protocol describes the use of surface-enhanced Raman scattering with multiple receptors to achieve high-specificity detection.
- Substrate Preparation: Functionalize Ag nanocube-based SERS substrates with nine different molecular receptors (e.g., CHO, NH2, OH, Br, COOH, PY, B(OH)2, CH3, NT) using thiol chemistry.
- Control Measurement: Acquire SERS spectra for each receptor-functionalized substrate before analyte exposure to establish a baseline ("control").
- Analyte Interaction: Expose each type of functionalized substrate to the target analytes (e.g., haloanisoles) individually.
- SERS Profiling: Acquire a large number of SERS spectra (e.g., 1620 total) after receptor-analyte interaction.
- Data Processing: Combine the SERS spectra from all nine receptors serially to create a single "SERS superprofile" for each analyte.
- Machine Learning Analysis: Input the superprofiles into a three-stage XGBoost recommender system to:
- Identify SERS vibrational modes related to receptor-analyte interactions.
- Rank the importance of these feature groups for differentiating analytes.
- Recommend the best-performing receptor combinations for maximum classification accuracy.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Matrix Interference Research
| Item | Function/Application | Example from Literature |
|---|---|---|
| HybridSPE-Phospholipid Plates/Cartridges [66] | Selective depletion of phospholipids from plasma or serum samples prior to LC/MS analysis. | Zirconia-silica based sorbent for selective phospholipid removal via Lewis acid/base interaction. |
| Biocompatible SPME (bioSPME) Fibers [66] | Equilibrium-based extraction and clean-up of small molecule analytes from complex biological fluids. | C18-modified silica particles in a biocompatible binder for direct extraction from plasma. |
| Ag Nanocubes [69] | High-performance SERS substrate building blocks that provide significant signal enhancement. | Nanocubes (~115 nm edge) used as building blocks for functionalized SERS substrates. |
| Molecular Receptors (Thiol-based) [69] | Functionalize metal surfaces to selectively capture target analytes and induce specific SERS signal changes. | 4-aminothiophenol (NH2), 4-mercaptobenzoic acid (COOH), 2-naphthalenethiol (NT), etc. |
| Multiplex Bead Array Kits [67] | Simultaneous quantification of multiple low-abundance proteins (cytokines, chemokines) in complex matrices. | Commercial human cytokine panels (e.g., Bio-Rad) for use with Luminex/Bioplex systems. |
| XGBoost Algorithm [69] | A machine learning framework for building "recommender systems" to identify optimal sensing receptors. | Used in a three-stage 'identify, rank, and recommend' system for SERS receptor selection. |
Overcoming biological matrix interference is not a one-size-fits-all endeavor but a critical determinant of diagnostic accuracy. Traditional sample preparation methods like targeted phospholipid depletion and bioSPME provide powerful, specific cleanup, but often add steps and time. In contrast, sensor-level solutions, particularly nanobiosensors leveraging multi-receptor SERS profiles and machine learning, represent a paradigm shift towards integrated, intelligent sensing that minimizes pre-processing. The experimental data shows that while simple dilution remains effective for abundant analytes, advanced nanotechnologies are achieving classification accuracies exceeding 95% for challenging structural analogs. The future of accurate diagnostics lies in the synergistic combination of robust sample preparation where necessary and the strategic deployment of nanotechnology and AI to ensure signal stability and specificity at the point of detection.
Strategies for Improving Reproducibility and Batch-to-Batch Consistency
For researchers and drug development professionals, the translation of diagnostic technologies from promising research to clinically validated tools hinges on two critical factors: reproducibility and batch-to-batch consistency. Within the rapidly advancing field of nanobiosensors, these factors present both a significant challenge and a key differentiator against traditional diagnostic methods. While conventional techniques like enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR) are well-established, their nanobiosensor counterparts offer the potential for superior sensitivity and point-of-care application but must overcome hurdles in manufacturing stability to achieve widespread adoption [72] [59]. This guide objectively compares the strategies and performance of nanobiosensors against traditional diagnostics, providing a framework for evaluating and selecting the most consistent technologies for critical research and development projects.
The Critical Role of Reproducibility in Diagnostics
Reproducibility is the cornerstone of credible research and reliable diagnostic tools. It ensures that results can be consistently replicated, allowing conclusions to be drawn and scientific advancements to be built upon a solid foundation [73]. For affinity reagents—the core of many biosensors—batch-to-batch consistency is a primary determinant of reproducibility. Variations in production can alter reagent performance, leading to different results with different batches and jeopardizing the longevity and validity of research projects [73].
The consequences of irreproducible data are severe, costing millions in research and development and potentially terminating projects mid-stream. Reports of irreproducible antibody studies due to batch consistency issues are a well-known challenge in the field [73]. This underscores the necessity of starting research projects with the most consistent affinity ligands available to avoid extensive re-standardization procedures and ensure data credibility.
Comparative Analysis: Nanobiosensors vs. Traditional Diagnostics
Performance and Consistency Metrics
The following table compares the key performance and consistency characteristics of nanobiosensors against traditional diagnostic methods.
Table 1: Performance Comparison of Diagnostic Platforms
| Feature | Traditional Diagnostics (e.g., ELISA, PCR) | Nanobiosensors |
|---|---|---|
| Typical Sensitivity | Lower sensitivity (e.g., ELISA for IL-6 barely reaches nanomolar level) [46] | High to ultra-high sensitivity; capable of single-molecule detection [74] [75] |
| Batch Consistency Challenge | Significant for biological reagents (e.g., monoclonal antibodies from hybridomas prone to genetic drift) [73] | Varies by material and design; can be superior with chemically-defined components [73] |
| Key Consistency Factor | Biological production systems susceptible to variation in culture conditions [73] | Chemical synthesis and defined nanomaterials can ensure high reproducibility [73] |
| Multiplexing Capability | Challenging; typically requires separate tests run in parallel [46] | A core strength; multiple biomarkers can be detected in a single sample using nanoparticles with distinct optical properties [46] |
| Primary Readout | Colorimetric (e.g., ELISA) or fluorescence [46] | Diverse: Photoluminescence (QDs), SPR/LSPR, Electrochemical, SERS [74] [46] |
Batch-to-Batch Consistency of Affinity Reagents
The choice of affinity reagent is a major determinant of batch-to-batch consistency. The table below compares the core production and consistency profiles of antibodies and aptamers.
Table 2: Affinity Reagent Consistency Comparison
| Characteristic | Monoclonal Antibodies (Hybridoma) | Recombinant Antibodies | Aptamers |
|---|---|---|---|
| Production Method | Biological production in hybridoma cell lines [73] | Biological expression in host cells [73] | Chemical synthesis based on a defined DNA sequence [73] |
| Defining Characteristic | Not fully sequence-characterized; subject to genetic drift over time [73] | Characterized by sequence [73] | Defined by a known and stable sequence [73] |
| Primary Consistency Risk | Genetic drift in cell lines alters antibody binding, leading to batch failure or increased cross-reactivity [73] | Numerous complex culture parameters (temperature, pH, metabolites) can cause significant product variation [73] | Minimal risk; synthesis follows a precise template, ensuring identical sequence and composition in every batch [73] |
| Inherent Batch Consistency | Low to Moderate | Moderate | High |
Experimental data from biolayer interferometry (BLI) and ELISA-like assays demonstrate this consistency. For example, two separate batches of a COVID-19 S1 aptamer showed minimal variation in binding to the SARS-CoV-2 S protein trimer. Similarly, three separate batches of aptamers targeting folate metabolites and the stress hormone cortisol showed highly reproducible performance across the quantifiable range of their respective assays [73].
Strategies for Enhancing Nanobiosensor Reproducibility
Material and Design Selection
The foundation of a reproducible nanobiosensor is laid during the design and material selection phase.
- Leveraging Chemically-Defined Reagents: Opting for affinity ligands that are chemically synthesized, such as aptamers, rather than biologically produced, eliminates a major source of batch-to-batch variability. Their production is based on a solid-phase synthesis process following a defined sequence, ensuring identical composition in every batch [73].
- Rational Nanomaterial Selection: The transformative potential of nanobiosensors depends on careful nanomaterial selection and device design. The unjustified or excessive use of nanomaterials can lead to unnecessarily complex systems that are difficult to reproduce. Selecting materials with stable and well-characterized optical or electronic properties, such as gold nanoparticles (AuNPs), quantum dots (QDs), or graphene, is crucial [75].
- Incorporating Advanced Statistical Process Control: For complex botanical drug products, a combination of chromatographic fingerprinting and multivariate statistical analysis has been successfully used to evaluate batch-to-batch quality consistency. This approach can be adapted for nanobiosensor manufacturing. Characteristic peaks in a fingerprint are weighted by their variability among production batches. A principal component analysis (PCA) model is then established, and multivariate control charts (Hotelling T2 and DModX) are used to monitor and evaluate quality consistency statistically [76].
Standardization and Characterization Protocols
Robust and standardized experimental protocols are essential for generating reliable and comparable data.
- Standardized Characterization Techniques: The reliability and properties of nanomaterials used in biosensors should be evaluated using standardized techniques. These include:
- Zeta Potential (ZP) Measurements: To assess the stability and surface charge of nanoparticles [59].
- Electron Microscopy (SEM/TEM): To characterize the size, morphology, and structure of nanomaterials [59].
- Electrochemical Impedance Spectroscopy (EIS): To evaluate the sensitivity and specificity of electrochemical nanobiosensors [59].
- Detailed Experimental Protocol: Quartz Crystal Microbalance (QCM) Biosensor Assay
- Objective: To quantitatively measure the binding affinity and kinetics between an immobilized aptamer and its target protein.
- 1. Sensor Chip Functionalization: A gold-coated QCM sensor chip is placed in the instrument. The chip surface is cleaned via UV-ozone treatment for 15 minutes. It is then incubated with a 2 mM solution of 11-mercaptoundecanoic acid (11-MUA) in ethanol for 24 hours to form a self-assembled monolayer (SAM). The chip is rinsed thoroughly with ethanol and dried under a stream of nitrogen.
- 2. Aptamer Immobilization: The functionalized chip is mounted in the QCM flow cell. A mixture of 0.4 M EDC (1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide) and 0.1 M NHS (N-hydroxysuccinimide) in deionized water is flowed over the surface for 10 minutes at a rate of 50 μL/min to activate the carboxyl groups. A solution of the 5'-amino-modified aptamer (1 μM in 10 mM PBS, pH 7.4) is then injected and recirculated for 40 minutes, allowing for covalent immobilization. The surface is subsequently rinsed with PBS to remove non-specifically bound aptamers.
- 3. Binding Kinetics Measurement: The target protein, serially diluted in PBS (e.g., 0 nM, 5 nM, 10 nM, 25 nM, 50 nM), is injected into the flow cell at a constant rate of 30 μL/min. The frequency shift (ΔF) is monitored in real-time for 15 minutes during the association phase, followed by a 15-minute dissociation phase with a pure PBS buffer. The data is fitted to a 1:1 Langmuir binding model using the instrument's software to calculate the association (kₐ) and dissociation (kḍ) rate constants, from which the equilibrium dissociation constant (K_D = kḍ/kₐ) is derived.
- Utilizing Multiplexed Control Systems: For applications requiring the detection of multiple biomarkers, multiplexed nanobiosensors that use nanoparticles with distinct signals, such as quantum dots with different emission wavelengths, can provide internal controls and more data points from a single sample, reducing errors associated with running multiple separate tests [46].
QCM Biosensor Experimental Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the right materials is critical for developing and executing reproducible experiments with nanobiosensors. The following table details essential reagents and their functions.
Table 3: Essential Research Reagents for Nanobiosensor Development
| Reagent / Material | Function / Explanation |
|---|---|
| Aptamers | Chemically-synthesized affinity ligands (DNA or RNA) that bind specific targets; offer superior batch-to-batch consistency compared to antibodies [73]. |
| Gold Nanoparticles (AuNPs) | Versatile plasmonic nanomaterials; used as signal probes in colorimetric assays or as a substrate for Surface-Enhanced Raman Spectroscopy (SERS) and SPR due to their strong optical properties [74] [77]. |
| Quantum Dots (QDs) | Semiconductor nanocrystals with size-tunable, narrow emission peaks; ideal for multiplexed detection as different colored QDs can be excited by a single light source [46]. |
| EDC/NHS Crosslinker Kit | Standard chemistry for covalent immobilization of biomolecules (e.g., aptamers, antibodies) onto sensor surfaces containing carboxyl or amine groups [59]. |
| Characterized Antibodies | For comparisons; recombinant antibodies are preferred over hybridoma-derived for better sequence definition and consistency, though risks remain from biological production [73]. |
The journey toward robust and clinically accepted nanobiosensors is inextricably linked to solving the challenges of reproducibility and batch-to-batch consistency. As the data indicates, the strategic selection of chemically-defined components like aptamers, over biologically-produced antibodies, provides a direct and effective path to superior batch consistency. Furthermore, the implementation of standardized characterization protocols and advanced statistical modeling for process control is essential for quality assurance. For the research and drug development community, prioritizing these strategies during the technology selection and development phases is not merely a technical consideration but a fundamental requirement for generating reliable data, ensuring the successful translation of diagnostic innovations, and ultimately, improving patient care through accurate and accessible diagnostics.
The Path to Standardization and Regulatory Approval
The integration of nanotechnology into diagnostic biosensors has ushered in a new era of potential for ultrasensitive and rapid disease detection. Nanobiosensors, which incorporate nanomaterials such as quantum dots, gold nanoparticles, and carbon nanotubes, leverage unique physicochemical properties to achieve significantly enhanced sensitivity and specificity compared to traditional diagnostic methods [21] [59]. However, their path to widespread clinical adoption is contingent upon overcoming significant challenges in standardization and regulatory approval. Establishing robust, universally accepted evaluation protocols is critical for objectively comparing the performance of these emerging technologies against established benchmarks and for providing the reliable data required by regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the World Health Organization (WHO) [68] [78]. This guide provides a structured framework for the experimental comparison of nanobiosensors against traditional diagnostics, focusing on the key analytical and clinical parameters that underpin standardization and regulatory success.
Comparative Performance Metrics: Nanobiosensors vs. Traditional Diagnostics
Objective comparison requires quantifying performance against a set of universally recognized metrics. The table below summarizes key performance data from empirical studies, highlighting the relative advantages of nanobiosensor technologies.
Table 1: Performance Comparison of Diagnostic Platforms
| Diagnostic Platform | Limit of Detection (LOD) | Sensitivity / Specificity | Assay Time | Key Applications & Findings |
|---|---|---|---|---|
| Nanobiosensors | ||||
| ― Microfluidic miRNA sensor [21] | 84 aM [21] | 95% (for salivary miRNAs) [79] | 10-15 minutes [79] | Breast cancer diagnostics via EV-associated microRNA [21]. |
| ― Electrochemical IL-8 sensor [79] | 2.4 ng/mL cutoff [79] | 89% sensitivity (for early OSCC) [79] | - | Salivary detection of oral squamous cell carcinoma [79]. |
| ― Plasmodium PfHRP2 sensor [59] | - | High sensitivity for histidine-rich protein 2 [59] | - | Malaria detection using gold nanoparticles (AuNPs) [59]. |
| Traditional Diagnostics | ||||
| ― Microscopy [59] | - | Low; requires expert operator [59] | - | Constrained by low sensitivity and specificity [59]. |
| ― ELISA [59] | - | Often hindered by cross-reactions or low sensitivity [59] | - | Serological assay for parasitic antigens/antibodies [59]. |
| ― PCR [21] | Varies | High, but can fail for low-abundance biomarkers in blood [21] | Hours | Requires special equipment and sample pretreatment [21] [59]. |
Standardized Experimental Protocols for Diagnostic Comparison
To generate the comparable data required for regulatory submission, researchers must adhere to rigorous and standardized experimental designs. The following protocols outline key methodologies for evaluating diagnostic performance.
Protocol for Analytical Sensitivity and Specificity
This protocol is designed to determine the Limit of Detection (LOD) and assess cross-reactivity.
- Sample Preparation: Prepare a dilution series of the purified target analyte (e.g., recombinant protein, synthetic nucleic acid) in a relevant biological matrix (e.g., artificial saliva, spiked serum, pooled human plasma). The matrix should mimic the intended clinical sample to account for potential interference [59].
- LOD Determination: Analyze each dilution in the series with the nanobiosensor and the traditional method (e.g., ELISA, PCR) across multiple replicates (n ≥ 5). The LOD is empirically defined as the lowest analyte concentration that yields a signal statistically distinguishable from the negative control (blank matrix) with 95% confidence [21].
- Specificity Testing: To evaluate cross-reactivity, test the biosensor against a panel of structurally similar analytes and other common biomarkers found in the sample matrix. For a nanobiosensor targeting a specific parasite antigen, this would include testing against antigens from other, similar parasites [59].
- Data Analysis: Calculate the mean signal and standard deviation for each concentration. Plot a dose-response curve to visualize the dynamic range. The LOD is typically calculated as the mean signal of the blank plus 3 standard deviations.
Protocol for Clinical Validation
This protocol assesses performance in real-world clinical scenarios, measuring clinical sensitivity and specificity.
- Cohort Selection: Obtain well-characterized clinical samples (e.g., blood, saliva, urine) from a cohort that includes confirmed positive patients and confirmed negative controls. The cohort size should be sufficient for statistical power and reflect the intended-use population [78] [79].
- Blinded Testing: Analyze all samples using both the novel nanobiosensor and the recognized gold-standard diagnostic method (e.g., histopathology, PCR with sequencing confirmation) in a blinded manner. Personnel operating the devices should be blinded to the reference results.
- Data Comparison: Construct a 2x2 contingency table to compare the results from the nanobiosensor against the gold standard.
- Statistical Analysis: Calculate clinical sensitivity (ability to correctly identify positives), specificity (ability to correctly identify negatives), and overall accuracy. A meta-analysis of diagnostic technologies has shown that overall accuracy for advanced models can be around 52.1%, but direct comparison to expert physicians may still show a performance gap [71].
Workflow Diagram: Diagnostic Evaluation Pathway
The following diagram illustrates the logical workflow for the standardized evaluation of a novel nanobiosensor, from initial analytical characterization to final regulatory submission.
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and validation of nanobiosensors rely on a specific set of materials and reagents. The table below details key components and their functions in a typical experimental setup.
Table 2: Key Reagent Solutions for Nanobiosensor Research
| Reagent / Material | Function / Explanation | Example Applications in Diagnostics |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Signal amplification due to strong plasmonic resonance; easy functionalization with biomolecules [21] [59]. | Functionalized with antibodies for colorimetric detection of Plasmodium PfHRP2 (malaria) [59]. |
| Quantum Dots (QDs) | Fluorescent nanoparticles with high brightness and photostability; used as optical labels [3] [21]. | Labeled with DNA probes for sensitive detection of Leishmania kinetoplast DNA (kDNA) [59]. |
| Carbon Nanotubes (CNTs) | Excellent electrical conductivity; serve as high-performance transducers in electrochemical sensors [21] [59]. | Functionalized with anti-EgAgB antibodies for detection of Echinococcus [59]. |
| Specific Bioreceptors | Molecular recognition elements that provide high specificity by binding to the target analyte [68] [21]. | Antibodies, aptamers, or DNA probes are immobilized on the sensor to capture specific biomarkers like IL-8 in saliva for oral cancer detection [79]. |
| Microfluidic Chips | Lab-on-a-chip platforms for precise fluid manipulation; enable minimal reagent use and automated, high-throughput analysis [21]. | Integrated with nanosensors for isolating extracellular vesicles (EVs) and detecting microRNA biomarkers for breast cancer [21]. |
Navigating the Regulatory Pathway
The regulatory approval pathway demands a rigorous demonstration of safety and efficacy, guided by established principles.
Adherence to International Standards and Criteria
A foundational step in regulatory strategy is alignment with international standards. The WHO ASSURED criteria provide a benchmark for ideal diagnostics, defining them as Affordable, Sensitive, Specific, User-friendly, Robust and rapid, Equipment-free, and Deliverable to end-users [68]. Furthermore, the ISO 20186 series and ISO 20914 provide specific standards for validating measurement procedures and estimating analytical performance characteristics in clinical laboratories, which are directly applicable to the analytical validation of nanobiosensors.
Key Regulatory Considerations for Nanomaterials
The unique properties of nanomaterials introduce additional considerations for regulatory bodies.
- Biosafety and Biocompatibility: A primary hurdle is the potential toxicity of nanomaterials. Regulatory submissions must include comprehensive data on the biocompatibility and biosafety of all components. This involves assessing cellular toxicity, potential for inflammatory responses, and long-term stability within the body, especially for implantable devices [3] [5]. Strategies to mitigate these concerns include surface modification of nanomaterials to improve biocompatibility and the exploration of biodegradable nanomaterials [5].
- Analytical and Clinical Performance: As detailed in the experimental protocols, regulators require exhaustive data on analytical sensitivity (LOD), clinical sensitivity/specificity, precision, and accuracy. This data must be generated from studies that closely mimic the intended clinical use, including testing in diverse and relevant clinical populations [78].
- Manufacturing Quality and Reproducibility: A significant challenge in the translation of nanobiosensors is ensuring batch-to-batch reproducibility and quality control during mass production. Regulatory approval is contingent on demonstrating a manufacturing process that is scalable, consistent, and adheres to Good Manufacturing Practice (GMP) [59] [5]. The complexity of fabricating nanomaterial-based sensors can pose a barrier to this standardization.
Diagram: From Development to Regulatory Approval
The journey from a laboratory prototype to an approved diagnostic tool involves a multi-stage process with iterative feedback, as shown in the following pathway.
The path to standardization and regulatory approval for nanobiosensors is complex but navigable. It requires a meticulous, data-driven approach centered on objective performance comparison with established diagnostics through standardized experimental protocols. By systematically addressing the key challenges of analytical validation, clinical evaluation, biosafety, and manufacturing reproducibility, researchers can generate the robust evidence needed to satisfy regulatory requirements. Success in this endeavor will accelerate the translation of these promising technologies from the research laboratory to the clinic, ultimately fulfilling their potential to revolutionize disease diagnosis and enable more personalized and effective patient care.
Optimization via Microfluidics and Artificial Intelligence
The pursuit of higher diagnostic accuracy is a central theme in modern medical research, driving the comparison between emerging nanobiosensors and traditional diagnostic methods. Within this context, the integration of microfluidics and artificial intelligence (AI) represents a transformative optimization frontier. Microfluidics, the science of manipulating fluids at a sub-millimeter scale, brings the advantages of miniaturization, automation, and reduced reagent consumption to diagnostic platforms [47] [80]. When combined with the data processing, pattern recognition, and predictive power of AI, these systems evolve from simple analytical tools into intelligent, adaptive, and highly efficient diagnostic solutions [81] [82]. This guide objectively compares the performance of diagnostics enhanced by these technologies against conventional alternatives, providing a detailed analysis of experimental data and methodologies relevant to researchers and drug development professionals.
Performance Comparison: AI-Enhanced Microfluidic Nanobiosensors vs. Traditional Methods
The convergence of AI and microfluidics with nanobiosensors addresses critical limitations of traditional diagnostics, namely sensitivity, speed, and the need for centralized laboratory infrastructure. The table below summarizes a quantitative comparison based on published experimental data.
Table 1: Performance Comparison of Diagnostic Modalities
| Diagnostic Parameter | Traditional Methods (e.g., PCR, ELISA) | AI-Augmented Microfluidic Nanobiosensors | Experimental Basis & Key Findings |
|---|---|---|---|
| Limit of Detection (LOD) | ELISA: ~ pM to nM range [68]PCR: ~ few copies/μL (but requires lab setup) [81] | H1N1 Virus: 9 TCID50/mL [81]Salivary Nucleic Acids: 50 IU/mL [81] | Microfluidic pre-concentration and AI-enhanced signal interpretation enable detection of low-abundance targets in complex samples like saliva. |
| Assay Time | PCR: Several hours (including sample prep) [81]Culture: Days to weeks [81] | Integrated Nucleic Acid Extraction: ~10 minutes [81]Full pathogen detection (H1N1, SARS-CoV-2): ~2 hours [81] | Microfluidic automation integrates lysis, extraction, and detection into a single "sample-in, answer-out" workflow, drastically reducing manual steps and time. |
| Sample Volume | mL volumes typically required | Saliva processing: 50-500 μL [81] | Microscale fluidic handling significantly reduces sample and reagent consumption, enabling analysis from minimal samples. |
| Multiplexing Capability | Limited; often requires separate assays | High; enabled by droplet microfluidics and spatially encoded microbeads [81] | AI algorithms are crucial for deconvoluting complex, high-dimensional data from multiplexed assays, allowing simultaneous detection of multiple pathogens. |
| Signal-to-Noise Ratio | Susceptible to non-specific binding and background interference | Greatly enhanced via AI-driven signal prediction and interpretation [81] [82] | Machine learning models are trained to distinguish specific signals from complex background noise in electrochemical and optical readouts. |
Experimental Protocols and Methodologies
To validate the performance claims in comparative studies, researchers employ rigorous experimental protocols. The following section details the methodologies cited for key advancements.
Protocol for AI-Optimized Microfluidic Saliva Processing
This protocol is adapted from integrated systems used for respiratory pathogen detection [81].
- 1. Sample Introduction: 500 μL of raw saliva sample is injected into a dedicated inlet on a microfluidic cartridge.
- 2. On-Chip Lysis & Binding: A lysis buffer is mixed with the sample. Magnetic nanoparticles (MNPs) or magnetic beads coated with specific aptamers are added. Using electromagnetic actuation or a vibrating magnetic rod, the beads are mixed vigorously with the sample to facilitate binding to the target (e.g., virus or nucleic acids).
- 3. Washing: An external magnetic field is applied to immobilize the bead-target complexes. The fluidic waste is flushed away. A wash buffer is then introduced to remove non-specifically bound contaminants while the beads remain held in place.
- 4. Elution: The purified targets are released from the beads into a small volume (e.g., 20-50 μL) of an elution buffer (e.g., pH 10.4). The resulting purified concentrate is then ready for downstream detection.
Protocol for AI-Enhanced Biosensing and Signal Analysis
This workflow is common in optical and electrochemical nanobiosensors [81] [82].
- 1. Recognition Event: The purified analyte interacts with the biological recognition element (e.g., antibody, aptamer) immobilized on a nanomaterial-based transducer (e.g., graphene, gold nanoparticles).
- 2. Signal Transduction: The binding event generates a raw physical signal (e.g., change in refractive index for SPR, current change for electrochemical sensors, fluorescence emission).
- 3. Data Acquisition: A sensor (e.g., CMOS camera, potentiostat) collects the raw signal data, which may be noisy or complex, especially in a multiplexed setting.
- 4. AI-Based Analysis: The raw data is fed into a pre-trained machine learning model (e.g., a convolutional neural network for image-based signals, or a random forest model for electrochemical data). The AI model's role is to classify the signal, quantify the analyte concentration, and distinguish specific binding from background noise.
- 5. Result Output: The AI system provides a diagnostic readout (e.g., pathogen identified, biomarker concentration) with a calculated confidence interval.
Visualizing the Integrated Diagnostic Workflow
The following diagram illustrates the logical flow and interaction between microfluidics, nanosensors, and AI in an optimized diagnostic system.
Diagram 1: Integrated AI-Microfluidic Diagnostic Workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
The development and operation of these advanced diagnostic platforms rely on a specific set of materials and reagents.
Table 2: Essential Research Reagents and Materials
| Item | Function in Experiment | Specific Examples |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Transducer material; enhance electron transfer and catalytic activity in electrochemical sensors; used in LSPR and SERS-based optical sensors [47]. | Gold nanorods (GNRs), nanoporous gold, gold nanoflowers. |
| Magnetic Nanoparticles (MNPs) | Enable automated on-chip separation, purification, and enrichment of targets from complex biological samples [81]. | Aptamer-coated magnetic beads; beads for nucleic acid binding. |
| Graphene & Derivatives | Carbon-based transducer with high surface area and excellent electrical conductivity for electrochemical sensing [47]. | Graphene oxide (GO), reduced graphene oxide (rGO), Graphene Quantum Dots (GQDs). |
| Molecularly Imprinted Polymers (MIPs) | Synthetic, stable recognition elements for specific target capture, often used in microfluidic pre-treatment [81] [82]. | Virus Imprinted Polymers (VIP) for H1N1 enrichment [81]. |
| Bio-Recognition Elements | Provide specificity by binding to the target analyte. AI is increasingly used to discover and optimize these elements [82]. | Antibodies, aptamers (from ML-powered SELEX), peptides. |
| Microfluidic Chip Substrates | Fabricate the miniaturized channels and chambers that fluidically process the sample. | Polydimethylsiloxane (PDMS), thermoplastics (e.g., PMMA), glass. |
The AI Optimization Engine: From Data to Design
Artificial intelligence contributes to optimization at multiple levels, from hardware design to data analysis. The diagram below outlines this multi-faceted role.
Diagram 2: The Multifaceted Role of AI in Optimization.
In conclusion, the integration of microfluidics and artificial intelligence presents a paradigm shift for diagnostic accuracy, directly addressing the core thesis of nanobiosensors versus traditional methods. The experimental data and protocols detailed herein provide robust evidence that this synergy offers superior performance in sensitivity, speed, and operational efficiency. For researchers and drug developers, mastering these tools and methodologies is pivotal for advancing the next generation of precise, point-of-care, and personalized diagnostic solutions.
Validation and Comparative Analysis: Nanobiosensors vs. Traditional Diagnostics
In the field of diagnostic testing, particularly in the advancing domain of nanobiosensors, the terms "sensitivity" and "Limit of Detection (LOD)" are frequently used. While often mistakenly interchanged, they represent two distinct and fundamental performance characteristics of an analytical procedure. A precise understanding of their differences is crucial for researchers and scientists developing and evaluating new diagnostic platforms, as it directly impacts the assessment of a method's capability and limitations [83] [84].
Sensitivity is formally defined as the slope of the analytical calibration curve, which is obtained when the results of the measurements are plotted against the amounts (or concentrations) of the analyte being determined [83] [84]. In practical terms, it indicates how much the analytical signal changes for a unit change in analyte concentration. A steeper slope signifies a higher sensitivity, meaning the method can distinguish small differences in concentration more effectively.
The Limit of Detection (LOD), on the other hand, is the lowest concentration of an analyte that can be reliably distinguished from the absence of that analyte (a blank sample) with a specified degree of statistical confidence [83] [85] [86]. It answers the question: "What is the smallest amount I can detect?" The LOD is not solely dependent on sensitivity but is profoundly influenced by the noise and random errors inherent in the measurement system [87]. As one source aptly states, "Detection limit is about how large part of the measured signal is useful, not how large the total signal is" [87].
Experimental Protocols for Determining Sensitivity and LOD
Protocol for Determining Analytical Sensitivity
The protocol for establishing sensitivity involves constructing a calibration curve, a foundational step in any analytical method development.
- Preparation of Standard Solutions: Prepare a series of standard solutions with known analyte concentrations spanning the expected range of the assay. The matrix of these standards should closely match that of the real samples (e.g., serum, buffer) to account for matrix effects.
- Measurement of Analytical Signal: Analyze each standard solution in replicate (typically n ≥ 3) using the developed method (e.g., nanobiosensor, traditional ELISA). Record the analytical signal (e.g., absorbance, fluorescence, frequency shift, electrical current) for each measurement.
- Calibration Curve Plotting: Plot the mean analytical signal (y-axis) against the known concentration of each standard (x-axis).
- Regression Analysis: Perform a linear regression analysis on the data points. The sensitivity of the method is given by the slope of the resulting calibration curve (y = mx + c) [83]. A higher slope value indicates greater sensitivity.
Standard Protocol for Estimating the Limit of Detection (LOD)
The estimation of LOD is a statistical exercise based on the characteristics of the blank (analyte-free) sample and a low-concentration sample. The method endorsed by the Clinical and Laboratory Standards Institute (CLSI) EP17 guideline is widely accepted [85].
- Analysis of Blank Sample: Measure a blank sample (containing no analyte) repeatedly (recommended n = 20 for verification; n = 60 for establishment by manufacturers) to estimate the mean blank signal and its standard deviation (SD~blank~).
- Calculation of Limit of Blank (LoB): The LoB is the highest apparent analyte concentration expected to be found when replicates of a blank sample are tested. It is calculated as: LoB = mean~blank~ + 1.645(SD~blank~) [85]. This establishes a threshold where only 5% of blank measurements would produce a false positive (assuming a Gaussian distribution).
- Analysis of Low-Concentration Sample: Measure a sample with a low concentration of analyte (near the expected LOD) repeatedly (again, n = 20 or 60).
- Calculation of LOD: The LOD is the lowest analyte concentration likely to be reliably distinguished from the LoB. It is calculated using the standard deviation of the low-concentration sample (SD~low conc~): LOD = LoB + 1.645(SD~low conc~) [85]. This ensures that 95% of measurements from a sample at the LOD will exceed the LoB, minimizing false negatives.
It is critical to note that another common, though less rigorous, approach defines LOD directly from the blank: LOD = mean~blank~ + 3(SD~blank~) [84] [86]. However, the CLSI EP17 protocol is considered more robust as it incorporates the variability of a low-level sample.
Quantitative Data Comparison: Sensitivity vs. LOD
The following tables summarize the core definitions and the direct comparative data for sensitivity and LOD, highlighting their distinct roles.
Table 1: Core Definitions and Calculations of Key Analytical Parameters
| Parameter | Definition | Typical Calculation | Primary Function |
|---|---|---|---|
| Sensitivity | Slope of the analytical calibration curve [83] [84]. | ( S = \frac{dy}{dx} ) (from y = Sx + c) | Measures ability to distinguish small concentration differences. |
| Limit of Detection (LOD) | Lowest analyte concentration reliably distinguished from a blank [85] [86]. | LOD = LoB + 1.645(SD~low conc~) [85] OR LOD = mean~blank~ + 3(SD~blank~) [86]. | Defines the minimum detectable level. |
| Limit of Quantification (LOQ) | Lowest concentration that can be measured with acceptable precision and accuracy [85] [86]. | LOQ = mean~blank~ + 10(SD~blank~) [84]. | Defines the minimum quantifiable level. |
Table 2: Head-to-Head Comparison of Sensitivity and Limit of Detection
| Aspect | Sensitivity | Limit of Detection (LOD) |
|---|---|---|
| Definition | Slope of the calibration curve [83]. | Lowest concentration distinguishable from blank with confidence [85]. |
| What it Measures | Change in signal per unit change in concentration. | Minimum detectable concentration. |
| Governed By | Analytical technique, transducer efficiency, signal amplification. | Noise level, background interference, imprecision of the method [87]. |
| Role in Method Selection | High sensitivity is desired for quantifying small concentration changes. | Low LOD is critical for detecting trace-level analytes. |
| Interdependence | A high sensitivity does not guarantee a low LOD. | A low LOD requires an acceptable sensitivity and, more importantly, a low noise level. |
Impact on Nanobiosensors vs. Traditional Diagnostics
The emergence of nanobiosensors has dramatically influenced the landscape of diagnostic accuracy, primarily by improving both the sensitivity and LOD of assays compared to traditional methods like ELISA. Nanomaterials, such as carbon nanotubes, graphene, and quantum dots, possess unique properties including a high surface-to-volume ratio and quantum effects, which make them excellent transducer materials [88]. This directly enhances the sensitivity of the device, as a given mass change of the analyte produces a larger analytical signal [88].
Furthermore, the integration of nanotechnology and microfluidics in these miniaturized biosensors allows for better control over reagents and a reduction in background noise [88]. Since the LOD is determined by the signal-to-noise ratio (SNR), a higher signal (from enhanced sensitivity) coupled with lower noise leads to a significantly improved SNR [87]. This directly translates to a lower (better) LOD, enabling the detection of pathogens, viruses, or disease biomarkers at ultra-low concentrations that are undetectable by traditional diagnostics [88]. This is paramount for early-stage disease diagnosis, where biomarker levels are minimal.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key solutions and materials essential for experiments aimed at characterizing sensitivity and LOD in biosensing.
Table 3: Essential Research Reagent Solutions for Sensitivity and LOD Studies
| Reagent/Material | Function | Example in Nanobiosensor Context |
|---|---|---|
| Analyte Standards | To create the calibration curve for determining sensitivity and range. | Purified target biomarker (e.g., PSA, cytokine) in a matrix matching the sample. |
| Blank Matrix | To estimate the background signal and calculate the LoB and LOD. | Analyte-free serum, buffer, or other sample simulant. |
| Functionalized Nanomaterials | To serve as the transduction element, enhancing signal response. | Gold nanoparticles, graphene oxide, or quantum dots coated with specific antibodies or aptamers [88]. |
| Immobilization Reagents | To attach biorecognition elements (e.g., antibodies) to the transducer surface. | Cross-linkers like EDC/NHS, or self-assembled monolayers (SAMs). |
| Signal Generation Substrates | To produce a measurable signal (optical, electrochemical) upon analyte binding. | Enzymatic substrates (e.g., TMB for HRP), electroactive tags, or fluorescent dyes. |
| Blocking Buffers | To minimize non-specific binding, thereby reducing background noise. | Solutions of BSA, casein, or other proteins that passivate unused surface areas [88]. |
The head-to-head comparison unequivocally demonstrates that sensitivity and LOD, while related, are non-interchangeable performance metrics. Sensitivity quantifies the magnitude of a method's response to concentration changes, whereas the LOD is a statistical measure of its detection capability governed by the signal-to-noise ratio. For researchers and drug development professionals, this distinction is critical. Evaluating a new nanobiosensor requires assessing both parameters: high sensitivity for precise quantification across the dynamic range, and a low LOD for early detection capabilities. The integration of nanomaterials and microfluidics provides a powerful pathway to optimize both, pushing the boundaries of diagnostic accuracy beyond the capabilities of traditional methods and paving the way for more sensitive, reliable, and early-stage diagnostic solutions.
In the evolving landscape of medical diagnostics, cross-reactivity remains a formidable obstacle to accurate disease detection, particularly for pathogens and biomarkers with high structural similarity. This challenge is especially pronounced in serological testing for flaviviruses like Zika and Dengue, where antibody cross-reactivity can lead to false positives and diagnostic ambiguity, ultimately compromising patient care and public health responses [89] [90]. The proteome composition and individual protein structures of these viruses are so similar that conventional serological tests often cannot reliably distinguish between them, creating an urgent need for more specific diagnostic approaches [90].
The emergence of nanobiosensor technology represents a paradigm shift in addressing these limitations. By leveraging the unique properties of nanomaterials and innovative detection mechanisms, nanosensors offer promising pathways to enhance specificity while maintaining high sensitivity in complex biological samples [2] [91]. This comparison guide objectively evaluates the performance of advanced nanobiosensors against traditional diagnostic platforms, with a specific focus on their capabilities to minimize cross-reactivity in clinically challenging scenarios. For researchers, scientists, and drug development professionals, understanding these technological distinctions is crucial for selecting appropriate diagnostic platforms and advancing the development of next-generation detection systems.
Performance Comparison: Nanobiosensors vs. Traditional Diagnostics
The following tables provide a comprehensive comparison of performance metrics and methodological approaches between nanobiosensors and traditional diagnostics for managing cross-reactivity.
Table 1: Performance Metrics Comparison for Cross-Reactivity Management
| Performance Parameter | Traditional Serological Assays | Nanobiosensor Platforms |
|---|---|---|
| Specificity for ZIKV vs. DENV | Variable; often compromised by cross-reactivity [90] | High (97.8% demonstrated in BERA biosensor) [92] |
| Sensitivity | IgM-ELISA shows high specificity but poor sensitivity [89] | 92.7% sensitivity (BERA); detects antibodies at 20 nM [89] [92] |
| Sample Volume Requirement | High (depleted by multiple tests) [90] | Low (enables testing with limited samples) [46] |
| Time to Result | Up to 4 weeks with PRNT confirmation [90] | Minutes to hours [89] [92] |
| Multiplexing Capability | Limited (requires separate tests) [46] | High (simultaneous detection of multiple targets) [89] [46] |
| Cost Considerations | Lower initial cost but higher overall with confirmatory testing | Potentially lower per data point in multiplexed format [46] |
Table 2: Methodological Approaches to Cross-Reactivity Challenges
| Methodological Aspect | Traditional Diagnostics | Nanobiosensor Solutions |
|---|---|---|
| Primary Strategy | Multiple assays and sample testing [90] | Component-resolved diagnosis with specific epitopes [93] |
| Key Target Proteins | Whole viral proteins prone to cross-reactivity | Zika NS1, Domain III (highly specific) [89] |
| Experimental Design | Serial testing with different platforms | Single-step differential detection [89] |
| Detection Principle | Colorimetric/colorimetric ELISA [46] | Magnetic relaxation, electrochemical, optical [89] [91] |
| Signal Transduction | Enzymatic color development [46] | T2 MR changes, electrical properties, photoluminescence [89] [92] |
Experimental Approaches and Detailed Protocols
Magnetic Relaxation Nanosensor (MRnS) for Zika/Dengue Differentiation
The customizable magnetic relaxation nanosensor platform represents a significant advancement in flavivirus discrimination. This methodology utilizes functionalized iron oxide nanoparticles (IONPs) conjugated to various viral proteins to specifically detect and differentiate cross-reactive antibodies through changes in spin-spin magnetic relaxation time (T2 MR) of water protons [89].
Detailed Experimental Protocol:
IONP Synthesis and Functionalization:
- Synthesize IONPs via co-precipitation of FeCl₃ and FeCl₂ in alkaline medium with polyacrylic acid (PAA) coating [89].
- Conjugate specific Zika proteins (ZENV, Z-D-III, Z-NS1) and DENV proteins to IONPs using EDC-NHS chemistry.
- Purify functionalized MRnS through dialysis against PBS (pH 7.4) and adjust to [Fe] = 4.0 mM.
Sample Preparation and Assay Execution:
- Dilute patient serum samples in appropriate buffer (1:100 ratio).
- Mix 100 μL of functionalized MRnS with 50 μL of prepared sample.
- Incubate at room temperature for 15 minutes with gentle agitation.
Measurement and Data Analysis:
- Measure T2 MR values using a benchtop NMR relaxometer.
- Calculate ΔT2 MR values relative to negative controls.
- Establish calibration curves with known antibody concentrations for quantification.
- Implement pattern recognition algorithms for one-step differentiation using mixed MRnS panels.
This approach enables detection of Zika antibodies at concentrations as low as 20 nM with high specificity, effectively discriminating between Zika and Dengue infections even in co-infection scenarios [89].
Bioelectric Recognition Assay (BERA) Biosensor Platform
The cell-based BERA biosensor utilizes mammalian cells as biological recognition elements with immobilized antibodies to detect target viruses through measurable changes in electrical properties [92].
Detailed Experimental Protocol:
Cell Preparation and Sensor Fabrication:
- Culture Vero cells in Dulbecco's Modified Eagle Medium with 10% FBS and antibiotics.
- Harvest cells at density of 2.5 × 10⁶ mL⁻¹ using trypsin/EDTA treatment.
- Electro-insert monoclonal antibodies against SARS-CoV-2 Spike protein S1 subunit into cell membranes using square electrical pulses at 1800 V/cm.
Assay Configuration and Measurement:
- Transfer antibody-electroinserted cells to carbon-screen printed electrodes.
- Apply 50 μL of clinical sample (nasopharyngeal/oropharyngeal swabs) to biosensor chamber.
- Measure open circuit potential (OCP) changes in real-time using high-precision A/D converters.
- Record electrical signal variations upon target-antibody binding.
Data Interpretation and Validation:
Quantum Dot-Linked Immunosorbent Assay (QLISA)
The QLISA platform replaces enzymatic reporters in traditional ELISA with quantum dots for enhanced sensitivity and multiplexing capability, significantly improving cross-reactivity management [46].
Detailed Experimental Protocol:
Surface Modification and Plate Preparation:
- Immobilize capture antibodies on high protein-binding plates overnight at 4°C.
- Block remaining surfaces with serum albumin (1% in PBS) for 2 hours at room temperature.
- Wash plates with PBS-Tween (0.05%) between steps.
Quantum Dot Conjugation and Detection:
- Conjugate detection antibodies to QDs with different emission spectra using EDC chemistry.
- Add samples and standard dilutions to wells, incubate for 90 minutes.
- Apply QD-antibody conjugates and incubate for 60 minutes with gentle shaking.
Signal Measurement and Analysis:
- Measure photoluminescence using plate reader with appropriate excitation/emission filters.
- Generate standard curves for target quantification.
- Utilize multiple QD colors for simultaneous detection of different analytes.
QLISA demonstrates significantly improved detection limits compared to traditional ELISA, enabling measurement of interleukin-6 at approximately 50 pg/mL, undetectable by standard ELISA methods [46].
Technological Mechanisms and Signaling Pathways
The enhanced specificity of nanobiosensors in managing cross-reactivity stems from their fundamental operational mechanisms, which differ significantly from traditional diagnostic approaches.
The fundamental advantage of nanobiosensors lies in their capacity for component-resolved diagnostics, which utilizes specific protein subunits or epitopes rather than whole antigens to minimize cross-reactivity [93]. For Zika and Dengue discrimination, targeting the Zika NS1 region and domain III (Z-D-III) demonstrates higher specificity, with NS1 showing particularly superior discriminatory power [89]. This approach contrasts with traditional assays that employ broad-spectrum antibodies against entire viral proteins, which frequently recognize conserved regions across flaviviruses.
The multiplexing capability of nanobiosensors further enhances specificity through pattern recognition. By simultaneously detecting multiple targets in a single sample, these platforms can identify unique response signatures that distinguish between highly similar pathogens [89] [46]. Magnetic relaxation nanosensors achieve this through mixtures of functional MRnS conjugated to different viral proteins, enabling one-step differentiation despite antibody cross-reactivity [89].
The Researcher's Toolkit: Essential Reagents and Materials
Successful implementation of cross-reactivity-resistant diagnostics requires specific reagents and materials optimized for maximum specificity.
Table 3: Essential Research Reagents for Cross-Reactivity Management
| Reagent/Material | Function and Importance | Specific Application Examples |
|---|---|---|
| Recombinant ZIKV NS1 Protein | Highly specific antigen for Zika detection; minimal cross-reactivity with DENV [89] [90] | Coating antigen for capture in immunosensors; specificity validation |
| Zika Domain III (Z-D-III) Protein | Specific envelope protein domain with reduced cross-reactivity compared to full envelope [89] | MRnS conjugation for differential detection; QLISA development |
| Monoclonal Antibodies Against S1 Subunit | Target-specific antibodies for precise viral detection [92] | Electro-insertion in BERA biosensors; immunosenor development |
| Functionalized Iron Oxide Nanoparticles | Magnetic core for relaxation-based sensing; customizable surface conjugation [89] | MRnS platform for one-step Zika/Dengue differentiation |
| Quantum Dots with Various Emission Spectra | Photoluminescent nanoparticles for multiplexed detection; signal amplification [46] | QLISA development; simultaneous multi-analyte detection |
| Screen-Printed Carbon Electrodes | Transduction platform for electrochemical sensing; portable form factor [92] | BERA biosensor implementation; point-of-care device development |
| EDC-NHS Crosslinking Chemistry | Reliable conjugation of biomolecules to nanoparticle surfaces [89] | Antibody immobilization; sensor functionalization |
The evolving landscape of diagnostic technologies demonstrates a clear trajectory toward nanobiosensor platforms with enhanced specificity for challenging diagnostic scenarios involving cross-reactive targets. The experimental data and performance comparisons presented in this guide consistently show that nanobiosensors outperform traditional diagnostic methods in key metrics specifically relevant to cross-reactivity management, including specificity, multiplexing capability, and time-to-result.
For researchers and drug development professionals, the implications are substantial. The component-resolved diagnosis approach enabled by these technologies represents a fundamental shift from broadly targeted immunoassays to precisely engineered detection systems that leverage specific protein subunits and epitopes with minimal cross-reactivity [93]. The development of biosensors targeting Zika NS1 and domain III proteins exemplifies this strategic approach, demonstrating that intelligent target selection is as crucial as detection technology itself [89].
Future advancements will likely focus on further integration of multiplexing capabilities and artificial intelligence for pattern recognition in complex samples, potentially enabling comprehensive pathogen identification from minimal sample volumes [91] [46]. Additionally, the ongoing development of point-of-care compatible platforms promises to translate these specificity enhancements from laboratory settings to clinical environments where they can most impact patient care and disease management [92]. As these technologies mature, they will undoubtedly become indispensable tools in the global effort to combat infectious diseases and improve diagnostic accuracy across healthcare systems.
The field of medical diagnostics is undergoing a revolutionary transformation, driven by the integration of nanotechnology. The critical metric of turnaround time (TAT)—the period from test initiation to result availability—is being radically shortened, shifting diagnostic processes from hours to minutes. This transition is largely fueled by the development and implementation of nanobiosensors, analytical devices that leverage the unique properties of nanomaterials to achieve unprecedented speed, sensitivity, and specificity [3] [91].
Traditional diagnostic techniques, while reliable, often involve complex, multi-step processes that require centralized laboratories, sophisticated equipment, and skilled personnel. These methods, including enzyme-linked immunosorbent assays (ELISA), polymerase chain reaction (PCR), and mass spectrometry, are frequently burdened with lengthy TATs, which can delay critical treatment decisions [94] [28]. In clinical practice, for instance, laboratory TATs for common tests have historically averaged around 55 minutes, with some processes extending for hours [94]. In contrast, nanobiosensors are engineered to function as rapid, point-of-care (POC) or even self-testing devices, offering real-time, in-situ analysis that is redefining the boundaries of diagnostic efficiency [95] [91]. This guide provides an objective comparison of the performance of advanced nanobiosensors against traditional diagnostic methods, with a focused analysis of the experimental data underscoring this seismic shift in speed and accuracy.
Quantitative Comparison: Traditional Diagnostics vs. Nanobiosensors
The performance differential between traditional diagnostics and nanobiosensors can be quantified across several key metrics. The following tables consolidate experimental data from recent studies to facilitate a direct comparison.
Table 1: Comparison of Turnaround Time (TAT) and Key Performance Metrics
| Diagnostic Method | Typical TAT Range | Limit of Detection (LOD) | Key Applications | Data Source/Experimental Context |
|---|---|---|---|---|
| Traditional Laboratory Tests | 55 minutes to >24 hours [94] | Varies with technique (e.g., ELISA, PCR) | Common chemistry panels, critical care tests [94] | CAP Q-Probes survey; benchmarking studies on intra-laboratory TAT [94] |
| STAT/Emergent Radiology Reads | 60 - 120 minutes [96] | Not Applicable (Imaging) | Critical CT/MRI cases (e.g., stroke, trauma) [96] | Industry standards for radiology reporting from exam completion to final report [96] |
| Electrochemical Nanobiosensors | Minutes (Real-time, continuous) [3] | Ultra-high (e.g., fM to aM levels) [28] | Glucose monitoring, anticancer drug detection (e.g., Doxorubicin) [3] [97] | Intravascular biosensors for real-time biomarker tracking; sensors for drug monitoring [3] [97] |
| Optical Nanobiosensors | Minutes (Real-time) [3] [91] | Ultra-high (Single-molecule detection) [28] | Oxygen saturation, biomarker detection, cancer diagnosis [3] [28] | Single-molecule diagnostics using plasmonic-scattering microscopy and SERS [28] |
| Microfluidic-Integrated Nanobiosensors | Minutes (Rapid test systems) [95] | ~84 aM (attomolar) [28] | Infectious disease detection, cancer biomarker profiling (e.g., microRNA in EVs) [95] [28] | Lab-on-a-chip devices for breast cancer diagnostics via extracellular vesicle (EV) analysis [28] |
Table 2: Analysis of Advantages and Disadvantages
| Method Type | Key Advantages | Major Disadvantages |
|---|---|---|
| Traditional Methods [94] [28] | Well-established, standardized, high analytical quality for centralized processing. | Lengthy TAT (hours to days), requires sophisticated instruments and trained personnel, high cost, poor suitability for point-of-care use. |
| Nanobiosensors [3] [68] [97] | Extremely rapid TAT (minutes), ultra-high sensitivity and specificity, portability for point-of-care testing, cost-effective for mass production, enable continuous monitoring. | Challenges in long-term stability and reproducibility, lack of standardized regulatory protocols, potential biocompatibility concerns for implantable models. |
Experimental Protocols: Unpacking the Methodologies
The remarkable performance of nanobiosensors is validated through rigorous and innovative experimental protocols. Below is a detailed breakdown of the core methodologies cited in the comparison data.
Protocol for Electrochemical Nanobiosensors in Drug Monitoring
This protocol is typical for sensors detecting anticancer drugs like Doxorubicin [97].
- Sensor Fabrication: A working electrode (e.g., glassy carbon) is modified with nanomaterials such as multi-walled carbon nanotubes (MWCNTs), graphene oxide, or gold nanoparticles to enhance surface area and electrical conductivity.
- Bioreceptor Immobilization: Recognition elements (e.g., antibodies, molecularly imprinted polymers, or DNA aptamers specific to the target drug) are immobilized onto the nanomaterial-functionalized electrode surface.
- Electrochemical Measurement: The fabricated sensor is immersed in a solution containing the sample (e.g., blood serum). Techniques like Cyclic Voltammetry (CV) or Differential Pulse Voltammetry (DPV) are applied.
- Signal Transduction & Readout: The binding of the target drug molecule to the bioreceptor alters the electrochemical properties at the electrode interface (e.g., change in current or potential). This change is measured and is directly proportional to the drug concentration, providing a quantifiable result in minutes [97].
Protocol for Optical Nanobiosensors in Single-Molecule Diagnostics
This protocol leverages super-resolution microscopy (SRM) techniques for extreme sensitivity [28].
- Sample Preparation: The biological sample (e.g., serum, plasma) is prepared and introduced onto a specially designed sensing surface, often functionalized with plasmonic nanoparticles (e.g., gold nanorods) or quantum dots.
- Biomarker Capture: Target biomarkers (e.g., specific proteins or nucleic acids) bind to their complementary bioreceptors (e.g., antibodies) on the nanostructured surface.
- Optical Signal Generation: The binding event is probed using techniques like:
- Surface-Enhanced Raman Spectroscopy (SERS): The plasmonic nanostructure dramatically enhances the Raman scattering signal from the target molecule, providing a unique fingerprint that can be detected at the single-molecule level [28].
- Plasmonic Scattering Microscopy: The binding of a molecule to a metallic nanoparticle changes its localized surface plasmon resonance (LSPR), causing a measurable shift in the scattered light's properties [28].
- Super-Resolution Imaging: SRM methods like STORM or DNA-PAINT are employed to bypass the diffraction limit of light, allowing for the precise localization and quantification of individual binding events with nanometer-scale resolution [28].
Workflow Visualization: Traditional vs. Nanobiosensor Diagnostics
The following diagram illustrates the stark contrast in the number of steps and time required for traditional laboratory diagnostics versus a microfluidic-integrated nanobiosensor, which consolidates most steps into a single, automated device.
The Scientist's Toolkit: Essential Research Reagents & Materials
The development and operation of high-performance nanobiosensors rely on a specific set of nanomaterials and reagents. The following table details key components and their functions in a typical experimental setup.
Table 3: Key Research Reagent Solutions for Nanobiosensor Development
| Item | Function in Experiment | Specific Examples & Applications |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Signal amplification; transduce binding events into optical (color/ LSPR shift) or electrochemical signals. [68] [91] [28] | Used as labels in immunoassays; functionalized with antibodies for cancer biomarker detection. [28] |
| Graphene & Carbon Nanotubes (CNTs) | Enhance electrochemical sensitivity due to excellent electrical conductivity and large surface area. [97] [91] [28] | Modify electrodes in sensors for detecting anticancer drugs like Doxorubicin. [97] |
| Quantum Dots (QDs) | Act as fluorescent labels with high photostability; enable multiplexed detection via different emission wavelengths. [3] [91] [28] | Used in optical biosensors for simultaneous detection of multiple pathogens or biomarkers. [91] |
| Molecularly Imprinted Polymers (MIPs) | Serve as synthetic, stable artificial receptors for specific molecular recognition. [97] | Used as an alternative to antibodies in sensors for monitoring drugs like Vismodegib. [97] |
| Microfluidic Chip | Provides a miniaturized platform for automating fluid handling, mixing, and separation; reduces reagent use and analysis time. [88] [28] | Integrated with nanobiosensors to create lab-on-a-chip devices for analyzing extracellular vesicles. [28] |
| DNA Aptamers | Act as synthetic, single-stranded DNA/RNA recognition elements with high affinity and specificity for targets. [28] | Used as bioreceptors for small molecules, proteins, or whole cells, offering stability and design flexibility. [28] |
Technological Foundations: How Nanobiosensors Achieve Their Performance
The dramatic improvement in TAT and accuracy is rooted in the fundamental properties of nanomaterials and their integration into sensor design.
Core Signaling Principles
The operation of a nanobiosensor can be broken down into a universal signaling pathway, where a biological recognition event is converted into a measurable signal. The core principles are illustrated below.
The Role of Nanomaterials
Nanomaterials are the cornerstone of this technology. Their high surface-to-volume ratio maximizes the area available for bioreceptor immobilization, increasing the probability of target capture and thus the sensor's sensitivity [68] [88] [91]. Furthermore, their unique quantum confinement effects and plasmonic properties enable the highly efficient signal transduction required for detecting low-abundance biomarkers and operating the miniaturized systems that lead to faster TATs [91] [28]. The convergence of these materials with microfluidics and sophisticated bioreceptors creates a synergistic effect, pushing the boundaries of diagnostic science far beyond the capabilities of traditional methods.
The empirical data and experimental protocols presented in this guide objectively demonstrate that nanobiosensors represent a superior alternative to traditional diagnostic methods in terms of speed, sensitivity, and point-of-care applicability. The ability to reduce turnaround time from hours to minutes, while maintaining or even improving diagnostic accuracy, positions nanobiosensors as a transformative force in medical research and clinical practice. For researchers and drug development professionals, mastering these technologies and their underlying methodologies is no longer a frontier pursuit but an essential competency for driving the future of precision medicine and personalized healthcare.
The accurate detection of proteins and nucleic acids is a cornerstone of modern diagnostics, biomedical research, and drug development. For decades, the gold standards in laboratories worldwide have been the enzyme-linked immunosorbent assay (ELISA) for protein detection and the polymerase chain reaction (PCR) for nucleic acid analysis [98] [99]. However, the evolving demands of precision medicine and rapid diagnostics have highlighted limitations in these conventional methods, particularly regarding sensitivity, speed, and adaptability for point-of-care use.
The emergence of nanobiosensors represents a paradigm shift in detection technologies. These devices integrate nanotechnology with biological recognition elements to create analytical tools that operate at the nanoscale [59] [91]. By leveraging the unique properties of nanomaterials such as gold nanoparticles, quantum dots, and carbon nanotubes, nanobiosensors offer the potential to overcome the inherent constraints of traditional methods [59]. This case study provides a objective comparison of these technologies, framing the analysis within a broader research thesis on diagnostic accuracy and highlighting the transformative potential of nanosensing platforms for scientific and clinical applications.
Established Gold Standards: ELISA and PCR
ELISA operates on the principle of immobilizing a target antigen or antibody onto a solid surface (typically a 96-well plate), followed by a series of binding and washing steps that ultimately produce a colorimetric signal proportional to the target's concentration. Its four main variants—direct, indirect, sandwich, and competitive—offer flexibility for different experimental needs [98]. The technique is valued for its ability to screen many samples simultaneously and its relatively simple protocol, but it provides limited information about the target protein beyond its presence and concentration [98].
PCR and its quantitative variant (qPCR) enable the exponential amplification of specific DNA sequences through thermal cycling. The process involves repeated cycles of denaturation, primer annealing, and enzyme-driven extension, allowing even minute quantities of target nucleic acids to be detected [100] [99]. Reverse Transcription PCR (RT-PCR) extends this capability to RNA targets by first converting RNA to complementary DNA (cDNA). The key advantage of PCR is its incredible sensitivity and specificity, but it requires sophisticated equipment, trained personnel, and is susceptible to inhibitors in complex biological matrices [99].
The Emerging Paradigm: Nanobiosensors
Nanobiosensors are analytical devices that combine a biological recognition element (such as an antibody, aptamer, or nucleic acid probe) with a nanomaterial-based transducer [59] [91]. The fundamental working principle involves the specific interaction between the biological element and the target analyte (protein or nucleic acid), which generates a physicochemical signal amplified and converted by the nanomaterial into a measurable output [59].
These sensors are broadly categorized by their transduction mechanism:
- Electrochemical nanobiosensors detect changes in electrical properties (current, potential, impedance) upon target binding [59] [101].
- Optical nanobiosensors rely on changes in optical properties, such as surface plasmon resonance (SPR), fluorescence, or colorimetric shifts [59] [102].
- Magnetic nanobiosensors use magnetic nanoparticles to isolate and detect targets, often simplifying sample processing [59].
The integration of nanomaterials is crucial—it provides a high surface-to-volume ratio for increased probe density and enhances signal generation, leading to significant improvements in sensitivity and lower detection limits compared to conventional platforms [59] [91].
Table 1: Core Methodological Principles of Each Detection Platform
| Technology | Core Principle | Primary Target | Key Steps |
|---|---|---|---|
| ELISA | Antigen-antibody binding with enzyme-mediated colorimetric signal generation | Proteins, antibodies [98] | Coating, blocking, detection, signal readout [98] |
| PCR/qPCR | Enzymatic amplification of specific DNA sequences with fluorescent detection | DNA (RNA via RT-PCR) [99] | Denaturation, annealing, extension, signal detection [100] |
| Nanobiosensors | Biorecognition event transduced via nanomaterial-enhanced signal | Proteins, nucleic acids, small molecules [59] [101] | Probe immobilization, sample introduction, binding, signal transduction [59] |
Experimental Protocols & Workflows
Standard ELISA Protocol for Protein Detection
The sandwich ELISA protocol, one of the most common formats, involves these critical stages [98]:
- Coating: A capture antibody is adsorbed onto a polystyrene microplate well surface through incubation.
- Blocking: The well is treated with a blocking agent (e.g., Bovine Serum Albumin or BSA) to cover any remaining protein-binding sites on the plastic surface, thereby minimizing non-specific binding in subsequent steps.
- Sample Incubation: The sample containing the target antigen is added. If present, the antigen binds specifically to the immobilized capture antibody.
- Detection Antibody Incubation: A second, enzyme-conjugated antibody that recognizes a different epitope on the target antigen is added, forming a "sandwich" complex.
- Substrate Addition: A colorimetric substrate for the enzyme is introduced. The enzyme catalyzes a reaction that converts the substrate into a colored product.
- Signal Measurement & Analysis: The reaction is stopped, and the intensity of the color, measured as absorbance using a plate reader, is proportional to the amount of target antigen in the sample.
Standard PCR/qPCR Protocol for Nucleic Acid Detection
A typical RT-qPCR workflow for detecting RNA targets, such as viral RNA, consists of [99]:
- RNA Extraction & Purification: RNA is isolated from the sample (e.g., swab, blood) using chemical or magnetic bead-based methods. This step is critical for removing inhibitors.
- Reverse Transcription (RT): The purified RNA is mixed with reverse transcriptase enzyme and specific primers to generate complementary DNA (cDNA).
- qPCR Amplification: The cDNA is combined with sequence-specific primers, a DNA polymerase (e.g., Taq polymerase), and nucleotides in a thermal cycler. The process involves:
- Denaturation: High temperature (~95°C) separates the DNA strands.
- Annealing: Lower temperature allows primers to bind to their complementary sequences on the target cDNA.
- Extension: The polymerase synthesizes new DNA strands.
- The cycle repeats 30-40 times, exponentially amplifying the target. A fluorescent probe or DNA-binding dye in the reaction mixture allows real-time monitoring of the amplification. The cycle threshold (Ct), at which fluorescence exceeds a background level, is used for quantification.
Representative Nanobiosensor Protocol: LSPR-based Serologic Detection
A cutting-edge protocol for detecting antibodies (proteins) using a Localized Surface Plasmon Resonance (LSPR) nanosensor, which outperformed ELISA in sensitivity, involves [102]:
- Nanosensor Fabrication: Gold nanorods (GNRs) are synthesized and functionalized with a linker molecule, DHLA. The target antigen (e.g., SARS-CoV-2 nucleocapsid protein) is then covalently conjugated to the GNR-DHLA complex via carbodiimide-activated amidation, forming the GNR-DHLA-N nanosensor.
- Characterization: The constructed nanosensor is characterized using UV-Vis spectroscopy, Dynamic Light Scattering (DLS), and zeta potential measurements to confirm successful bioconjugation and colloidal stability.
- Sample Incubation: The functionalized nanosensors are incubated with the test sample (e.g., patient serum). If present, specific antibodies bind to the immobilized antigens on the nanorod surface.
- Signal Transduction & Readout: The antibody binding event alters the local refractive index around the gold nanorods, causing a measurable redshift in their LSPR extinction spectrum. This shift is quantified using a spectrometer.
- Data Analysis: The magnitude of the spectral shift is correlated with the concentration of target antibodies in the sample.
Performance Comparison: Experimental Data
Direct comparative studies and meta-analyses of published data reveal significant differences in the operational and performance characteristics of ELISA, PCR, and nanobiosensors.
Sensitivity and Detection Limits
Sensitivity is a critical parameter, especially for early disease diagnosis or detecting low-abundance biomarkers. Nanobiosensors consistently demonstrate a superior ability to detect targets at ultralow concentrations.
Table 2: Comparative Sensitivity and Detection Limits
| Technology | Target Class | Specific Target | Reported Limit of Detection (LOD) |
|---|---|---|---|
| ELISA | Protein | Aspergillus galactomannan fungal marker | 0.4 ng/mL [103] |
| PCR | Nucleic Acid | SARS-CoV-2 RNA | ~100 copies/μL (via RT-qPCR) [99] |
| Electrochemical Nanobiosensor | Nucleic Acid | HPV E6/E7 mRNA | 0.1 fM (~100 copies) [101] |
| Electrochemical Nanobiosensor | Nucleic Acid | miRNA (via CHA/TDT amplification) | 26 fM [101] |
| LSPR Optical Nanosensor | Protein (Antibody) | Anti-SARS-CoV-2 IgG | Outperformed ELISA, detecting antibodies earlier in infection (before 10 days post-onset) [102] |
Analysis Time, Throughput, and Cost
The time-to-result and operational complexity are decisive factors in many clinical and research scenarios.
Table 3: Comparison of Operational and Economic Parameters
| Parameter | ELISA | PCR/qPCR | Nanobiosensors |
|---|---|---|---|
| Total Assay Time | ~2-4 hours [98] [102] | 6-8 hours (including sample prep) [99] | Minutes to <2 hours [101] [102] |
| Sample Preparation | Moderate (dilutions required) | High/Complex (RNA extraction critical) | Simple (often minimal processing) [103] [101] |
| Throughput | High (96-well format) | Moderate (limited by thermal cycler capacity) | Variable (improving with microfluidics) [59] |
| Equipment Needs | Plate reader (common) | Thermal cycler, RT enzyme (specialized) | Portable readers possible [101] [91] |
| Cost per Test | Low (for reagents) | Moderate to High | Potentially low (aiming for mass production) [59] |
| Technical Expertise | Moderate | High (required) | Low (goal for POC devices) [59] [91] |
The Scientist's Toolkit: Key Research Reagents & Materials
The development and implementation of these diagnostic platforms rely on a specific set of reagents and materials.
Table 4: Essential Research Reagents and Their Functions
| Category | Specific Item | Primary Function in Assay |
|---|---|---|
| Core Biological Reagents | Specific Antibodies (monoclonal/polyclonal) | Recognition element for antigens in ELISA and some nanobiosensors [98] [102] |
| Primers (forward and reverse) | Sequence-specific binding to target DNA for PCR amplification [100] | |
| Aptamers (ssDNA/RNA oligonucleotides) | Synthetic "chemical antibodies" with high affinity for targets; used in advanced biosensors [100] | |
| Key Enzymes & Proteins | DNA Polymerase (e.g., Taq) | Enzymatically synthesizes new DNA strands during PCR [100] |
| Reverse Transcriptase | Converts RNA into cDNA for RT-PCR [99] | |
| Horseradish Peroxidase (HRP) | Enzyme conjugate that catalyzes colorimetric reaction in ELISA [98] | |
| Critical Nanomaterials | Gold Nanoparticles (AuNPs) / Gold Nanorods (GNRs) | Transduction element in optical/electrochemical sensors; enhances signal via LSPR or conductivity [59] [102] |
| Quantum Dots (QDs) | Fluorescent nanoparticles used as highly bright labels in optical detection [59] | |
| Carbon Nanotubes (CNTs) | Improve electron transfer in electrochemical sensors, boosting sensitivity [59] [101] | |
| Specialized Buffers & Substrates | Blocking Buffer (e.g., BSA) | Prevents non-specific binding of proteins to solid surfaces in ELISA and nanosensors [98] |
| Chromogenic/Electrochemiluminescent Substrate | Generates measurable signal (color/light) upon enzyme action in ELISA/ECL sensors [98] [101] |
Discussion & Future Research Directions
The experimental data substantiates the thesis that nanobiosensors represent a significant advancement over conventional methods in key areas of diagnostic performance. Their primary advantages include:
- Superior Sensitivity: The use of nanomaterials like AuNPs and QDs provides a high surface-to-volume ratio and unique optoelectronic properties, enabling detection down to the attomolar range for some targets, far exceeding typical ELISA and rivaling or surpassing PCR without the need for amplification [59] [101].
- Rapid Analysis: The simplified workflows and direct transduction mechanisms of nanobiosensors drastically reduce time-to-result, which is critical for point-of-care decision-making [101] [91].
- Potential for Point-of-Care (POC) Use: The ongoing miniaturization of these platforms through lab-on-a-chip and microfluidics integration, coupled with portable readers, positions them as ideal candidates for decentralized testing outside central laboratories [59] [91].
However, the transition of nanobiosensors from research prototypes to mainstream tools faces several challenges that align with the broader context of diagnostic technology evolution:
- Standardization and Mass Production: Reproducible, large-scale fabrication of nanobiosensors with consistent performance remains a hurdle [59].
- Biological Matrix Interference: Complex samples like blood or serum can sometimes cause non-specific signals, affecting accuracy [59].
- Regulatory Hurdles and Long-Term Stability: Comprehensive clinical validation and meeting regulatory standards (FDA, CE) are necessary. The long-term stability of functionalized nanomaterials in biosensors also requires further investigation [91].
Future research is focused on overcoming these barriers. Key directions include the development of multiplexed nanobiosensors using polymer nanofibers for simultaneous detection of multiple pathogens, the creation of fully integrated lab-on-a-chip platforms, and the exploration of novel nanomaterial hybrids to further push the boundaries of sensitivity and specificity [59] [91]. The ultimate goal is to create robust, user-friendly, and cost-effective diagnostic systems that can be deployed at the bedside, in a doctor's office, or in resource-limited settings, thereby democratizing high-precision diagnostics.
This objective comparison between established gold standards and emerging nanotechnologies clearly delineates a transformative period in bioanalytical science. While ELISA and PCR remain robust, well-understood, and irreplaceable for many high-throughput laboratory applications, their limitations in speed, complexity, and sensitivity are evident. Nanobiosensors, backed by compelling experimental data, demonstrate a clear capacity to address these limitations, offering dramatic improvements in detection limits, assay rapidity, and potential for miniaturization.
The choice of technology must be guided by the specific application context. For routine, high-volume protein quantification in a centralized lab, ELISA retains its utility. For absolute nucleic acid identification with unparalleled specificity, PCR is still the benchmark. However, for applications demanding ultra-early disease detection, rapid field-based testing, or continuous monitoring, nanobiosensors represent the vanguard of diagnostic innovation. As research efforts resolve current challenges related to standardization and regulatory approval, nanobiosensors are poised to redefine the paradigms of protein and nucleic acid detection, thereby accelerating progress in biomedical research, drug development, and clinical diagnostics.
Market Adoption and Real-World Efficacy Data
The field of medical diagnostics is undergoing a profound transformation, driven by the convergence of nanotechnology and advanced sensing technologies. Nanobiosensors represent a groundbreaking class of analytical devices that integrate biological recognition elements with nanomaterials to achieve unprecedented detection capabilities [75] [21]. These devices leverage the unique physicochemical properties of nanomaterials—including their high surface-to-volume ratio, quantum confinement effects, and enhanced reactivity—to detect biological molecules with exceptional sensitivity and specificity [21]. As the healthcare landscape increasingly emphasizes early disease detection and personalized medicine, understanding the comparative performance of nanobiosensors against traditional diagnostic methods becomes crucial for researchers, scientists, and drug development professionals. This analysis provides a structured comparison of their real-world efficacy, supported by experimental data and methodological insights, to inform technology adoption decisions in both clinical and research settings.
Performance Comparison: Nanobiosensors vs. Traditional Diagnostics
The quantitative evaluation of diagnostic technologies encompasses multiple performance metrics, including sensitivity, detection limits, and accuracy. The tables below synthesize comparative experimental data across these dimensions.
Table 1: Comparison of Detection Limits and Sensitivity Across Diagnostic Platforms
| Technology Type | Detection Mechanism | Limit of Detection (LOD) | Key Applications | Experimental Evidence |
|---|---|---|---|---|
| Nanobiosensors | Plasmonic, electrochemical, optical | Single-molecule level [21] | Early cancer detection, infectious diseases, neurodegenerative disorders [21] | Microfluidic-integrated biosensor for breast cancer miRNA: LOD 84 aM [21] |
| Electrochemical Biosensors | Electron transfer variation | Varies with design and functionalization [3] | Glucose monitoring, blood pressure assessment [3] | Implantable glucose sensors with oxygen electrodes [3] |
| Optical Biosensors | Light interaction measurement | Limited by label-free detection constraints [3] | Oxygen saturation, biomarker detection [3] | Fluorescence quenching for intravascular glucose monitoring [3] |
| Enzyme-linked Immunosorbent Assay (ELISA) | Colorimetric/chemiluminescence | Nanomolar to picomolar range [21] | Protein quantification, antibody detection | Conventional standard; limited for low-abundance biomarkers [21] |
| Polymerase Chain Reaction (PCR) | Nucleic acid amplification | Varies with target and sample prep [21] | Pathogen detection, genetic testing | Multiplex PCR for antifungal resistance: weeks faster than culture [4] |
Table 2: Accuracy and Real-World Performance Metrics
| Technology | Reported Accuracy | Analysis Time | Key Advantages | Identified Limitations |
|---|---|---|---|---|
| Advanced AI-Enhanced Nanobiosensors | Up to 94% in early disease detection [104] | Near real-time (minutes) [104] | Ultrasensitive, potential for continuous monitoring | "Black box" problem, requires explanation for diagnoses [104] |
| Generative AI Models (e.g., GPT-4, Gemini) | 52.1% overall diagnostic accuracy (meta-analysis) [71] | Seconds to minutes | Rapid data processing, multi-modal integration | Significantly inferior to expert physicians (15.8% accuracy difference) [71] |
| Expert Physicians | 67.9% accuracy (exceeds AI overall) [71] | Hours to days (with testing) | Contextual understanding, clinical reasoning | Subject to workload, fatigue, cognitive biases |
| Conventional Biosensors | Varies by specific technology and application [3] | Minutes to hours | Established protocols, broader regulatory acceptance | Sensitivity to chemical interferences, limited long-term durability [3] |
Experimental Protocols and Methodologies
Validation Frameworks for Diagnostic Technologies
Rigorous experimental validation is fundamental to establishing diagnostic efficacy. For nanobiosensors, protocols typically involve multiple phases:
1. Analytical Validation: This phase assesses fundamental performance parameters. Studies utilize standardized reference materials and spike-recovery experiments in controlled matrices to determine limits of detection (LOD), dynamic range, sensitivity, and specificity. For instance, a microfluidic-integrated nanobiosensor for breast cancer diagnostics was validated by spiking specific concentrations of EV-associated microRNA into buffer solutions, achieving an LOD of 84 aM [21]. Cross-reactivity is evaluated against structurally similar molecules to establish specificity.
2. Clinical Validation: This critical phase tests performance with real biological samples. Protocols typically involve case-control or cohort studies comparing the new technology against gold-standard methods. A representative study design is illustrated below, showing the pathway from sample collection to result interpretation:
For AI-based diagnostics, validation follows different paradigms. The meta-analysis of generative AI models evaluated performance across 83 studies, employing strict inclusion criteria: direct comparison between AI and human clinicians, use of primary data, and availability of specific comparative performance data [71]. Studies were assessed for risk of bias using the Prediction Model Study Risk of Bias Assessment Tool (PROBAST), with 76% of studies rated as high risk, often due to small test sets or unknown training data for AI models [71].
Advanced Integrated Systems
The most sophisticated validation approaches involve convergent technologies. For example, the integration of nanobiosensors with super-resolution microscopy (SRM) creates platforms for spatially resolved biomolecular interrogation beyond the diffraction limit of conventional optics [21]. Proof-of-concept implementations include:
- Plasmonic-SRM Hybrids: Combining localized surface plasmon resonance with techniques like STORM or PALM for single-molecule detection at metal interfaces.
- Electrochemical-Optical Correlatives: Simultaneously measuring electrical signals and optical signatures from the same nanobiosensor platform.
- SRM-Enabled Immunoassays: Utilizing nanoscale resolution to quantify biomarker distribution and density.
These integrated systems face unique validation challenges, including reproducibility, multiplexing capability, and standardization of imaging protocols, which are active areas of methodological development [21].
Technological Foundations and Signaling Mechanisms
Operational Principles of Nanobiosensors
Nanobiosensors function through specific interactions between target analytes and bioreceptors, generating detectable physicochemical changes transduced into measurable signals [21]. The fundamental signaling pathway can be visualized as follows:
This framework highlights how nanomaterials serve as high-performance interfaces that enhance signal generation through their large surface-to-volume ratio, tunable optical/electronic characteristics, and quantum confinement effects [21]. The transducer then converts these nanoscale interactions into quantifiable signals such as electrical fluctuations, optical shifts, or resonance frequency changes.
Comparative Signaling Pathways
Traditional diagnostics typically employ different signaling mechanisms. ELISA relies on antibody-antigen interactions with enzyme-mediated color change, while PCR depends on nucleic acid amplification with fluorescent detection. These methods often require multiple processing steps, larger sample volumes, and lack the single-molecule sensitivity achievable with advanced nanobiosensors [21].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of nanobiosensors require specialized materials and reagents that enable their superior performance characteristics.
Table 3: Essential Research Reagents and Materials for Nanobiosensor Development
| Material/Reagent | Function | Specific Examples | Role in Experimental Protocols |
|---|---|---|---|
| Gold Nanoparticles (AuNPs) | Signal amplification, biocompatible substrate | Spherical AuNPs, nanorods | Plasmonic enhancement in optical sensors; functionalization platform [21] |
| Quantum Dots (QDs) | Fluorescent tagging, signal generation | CdSe/ZnS core/shell QDs | High-intensity fluorescence for multiplexed detection [3] [21] |
| Graphene & 2D Materials | Electron transfer enhancement, sensing platform | Graphene oxide, MoS₂ | High conductivity for electrochemical sensors; large surface area [21] |
| Functional Bioreceptors | Molecular recognition | Antibodies, aptamers, enzymes | Target-specific binding (e.g., glucose oxidase for glucose sensors) [3] [21] |
| Microfluidic Components | Sample processing, fluid control | PDMS chips, microchannels | Automated sample handling, miniaturization (lab-on-a-chip) [21] |
| CRISPR Components | Nucleic acid detection | Cas enzymes, gRNA | Specific sequence identification for molecular diagnostics [75] |
| Surface Modification Agents | Bioconjugation, stability | PEG, thiol compounds | Improve biocompatibility, reduce fouling, enhance functionalization [21] |
The comprehensive analysis of market adoption and real-world efficacy data reveals a dynamic diagnostic landscape where nanobiosensors demonstrate distinct advantages in sensitivity and detection limits over traditional methods, particularly for applications requiring single-molecule detection or continuous monitoring. However, traditional diagnostics maintain important strengths in established protocols and broader regulatory acceptance. The integration of artificial intelligence with both nanobiosensors and traditional diagnostic methods shows promising but uneven results, with current AI systems performing comparably to non-expert physicians but still lagging behind expert clinicians [71]. Future diagnostic platforms will likely leverage hybrid approaches that combine the ultrasensitive detection capabilities of nanobiosensors with the clinical validation and reasoning strengths of medical experts, ultimately accelerating the transition toward personalized medicine and precision diagnostics.
Conclusion
The comparative analysis conclusively demonstrates that nanobiosensors represent a significant leap forward in diagnostic accuracy, offering dramatically enhanced sensitivity, specificity, and speed over traditional methods like ELISA and microscopy. Their ability to detect biomarkers at ultra-low concentrations, even at the single-molecule level, opens new frontiers for early disease detection and personalized medicine. Future progress hinges on overcoming challenges related to mass production, standardization, and regulatory pathways. The continued convergence of nanobiosensors with microfluidics, AI, and point-of-care technologies is poised to redefine clinical diagnostics, enabling real-time health monitoring and fundamentally improving patient outcomes in oncology, neurology, and global health.
References
- 1. Nanotechnology-Enabled Biosensors: A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856107/]
- 2. A Methodical Review on the Applications and Potentialities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8799955/]
- 3. Recent Advances in Micro- and Nano-Enhanced Intravascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12349352/]
- 4. What are the 2025 Trends in Diagnostics? [https://www.hartmannyoung.com/resources/blog/what-are-the-2025-trends-in-diagnostics-/]
- 5. Editorial: Advanced nanobiosensors for non-invasive ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1208679/full]
- 6. Nano Biosensors: Properties, applications and ... [https://www.sciencedirect.com/science/article/pii/S2238785421002751]
- 7. Single-Walled Carbon Nanotube Biosensor for Real-Time ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325009698]
- 8. Nanotube sensors enhance accuracy in continuous health ... [https://healthcare-in-europe.com/en/news/nanotube-sensors-accuracy-continuous-health-monitoring.html]
- 9. Gold-Based Nanohybrid Materials in Biosensing [https://www.sciencedirect.com/science/article/abs/pii/S0039914025013050]
- 10. New insights into biosensing, bioimaging, genomics ... [https://pubmed.ncbi.nlm.nih.gov/40306530/]
- 11. Frontiers | Carbon Quantum Dots for Biomedical Applications: Review and Analysis [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2021.700403/full]
- 12. Frontiers | Recent Advances on Synthesis and Potential Applications of Carbon Quantum Dots [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2022.906838/full]
- 13. Graphene and Carbon Quantum Dots: Competing Carbons in Harmonized Photoelectrochemical Platforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508723/]
- 14. Carbon Nanotube-Based Field-Effect Transistor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109531/]
- 15. Graphene-Based Biosensors: Enabling the Next Generation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467994/]
- 16. A Review on Biosensors and Recent Development of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7915135/]
- 17. Types of Biosensors : Optical, Electrochemical, ... [https://www.rfwireless-world.com/articles/biosensor-types-and-working-principles]
- 18. The Rising Role of Biosensors in Modern Technology [https://www.delveinsight.com/blog/rising-role-of-biosensors]
- 19. Piezoelectric Biosensors - an overview [https://www.sciencedirect.com/topics/engineering/piezoelectric-biosensors]
- 20. Piezoelectric biosensors: shedding light on principles and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10920441/]
- 21. Nanobiosensors for Single-Molecule Diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564644/]
- 22. Nanobiosensors in neurodegenerative disease diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078979/]
- 23. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 24. Nanomaterials-based biosensing strategies for biomarkers ... [https://www.sciencedirect.com/science/article/pii/S2590137022001388]
- 25. Improving biosensor accuracy and speed using dynamic ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566323007716]
- 26. Reduction of Biosensor False Responses and Time Delay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10683760/]
- 27. A Review on Biosensors and Recent Development of ... [https://www.mdpi.com/1424-8220/21/4/1109]
- 28. Nanobiosensors for Single-Molecule Diagnostics: Toward ... [https://www.mdpi.com/2079-6374/15/10/705]
- 29. Optical nanomaterial-based detection of biomarkers in liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10938695/]
- 30. Circulating tumor cells: Blood-based detection, molecular ... [https://www.sciencedirect.com/science/article/pii/S1535610825003149]
- 31. Cell-free DNA testing for the detection and prognosis ... [https://www.nature.com/articles/s41467-025-61890-z]
- 32. A Review of Nanotechnology in microRNA Detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11311607/]
- 33. Diagnostic Potential of Cross-Specimen microRNA Panels as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578759/]
- 34. Advancements in nanosensors for cancer detection [https://www.aimspress.com/article/doi/10.3934/biophy.2024028?viewType=HTML]
- 35. Cell-free DNA as a potential alternative to genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408905/]
- 36. Current Status of α-Synuclein Biomarkers and the Need for α ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384595/]
- 37. PET Tracers, Co-pathology and PPMI Findings Featured at ... [https://www.michaeljfox.org/news/pet-tracers-co-pathology-and-ppmi-findings-featured-2025-adpd-conference]
- 38. Optical biosensors for diagnosing neurodegenerative ... [https://www.nature.com/articles/s44328-025-00040-3]
- 39. ASAP Research Round-Up | Q2 2025 [https://parkinsonsroadmap.org/news/asap-research-round-up-q2-2025/]
- 40. Pain-Free Alpha-Synuclein Detection by Low-Cost ... [https://www.mdpi.com/2079-4991/14/2/170]
- 41. Electrochemical biosensors in early detection of Parkinson ... [https://www.sciencedirect.com/science/article/abs/pii/S000989812402254X]
- 42. Predicting Parkinson's disease and its progression based ... [https://www.nature.com/articles/s41531-025-01097-7]
- 43. Nanobiosensors for revolutionizing parasitic infections diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12168311/]
- 44. Are Nanobiosensors an Improved Solution for Diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8066167/]
- 45. Laboratory diagnostics for human Leishmania infections [https://pmc.ncbi.nlm.nih.gov/articles/PMC9636697/]
- 46. Multiplexed Nanobiosensors: Current Trends in Early ... [https://www.mdpi.com/1424-8220/20/23/6890]
- 47. Impact of nanotechnology on conventional and artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10066940/]
- 48. Lab on Chips Market Size to Worth USD 15.58 Billion by [https://www.globenewswire.com/news-release/2025/05/16/3082835/0/en/Lab-on-Chips-Market-Size-to-Worth-USD-15-58-Billion-by-2032-at-9-71-CAGR-Research-by-SNS-Insider.html]
- 49. Lab on Chip Market Size to Hit USD 17.00 Billion by 2034 [https://www.precedenceresearch.com/lab-on-chip-market]
- 50. Towards practical point-of-care quick, ubiquitous ... [https://www.nature.com/articles/s41378-025-01057-4]
- 51. Advances in Point-of-Care Infectious Disease Diagnostics [https://www.mdpi.com/2075-4418/15/22/2845]
- 52. POC Sensor Systems and Artificial Intelligence—Where We ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467669/]
- 53. Lab-on-a-Chip and Microfluidics World Congress 2025 [https://www.selectbioconferences.com/loacwc2025]
- 54. Advances in multiplexed photoelectrochemical sensors for ... [https://www.sciencedirect.com/science/article/pii/S1385894725001184]
- 55. Multiplexed Point-of-Care Testing – xPOCT - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5538621/]
- 56. Multiplexed Optical Nanobiosensing Technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562344/]
- 57. Research Progress on Multiplexed Pathogen Detection ... [https://www.mdpi.com/2079-6374/15/6/378]
- 58. Advancements in nanobiosensor technologies for in-vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11609235/]
- 59. Nanobiosensors for revolutionizing parasitic infections diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02685-2]
- 60. Machine learning in point-of-care testing: innovations, ... [https://www.nature.com/articles/s41467-025-58527-6]
- 61. Towards Sustainable Scaling-Up of Nanomaterials ... [https://www.mdpi.com/2673-4117/6/7/149]
- 62. Nano-OPS Printer for High Rate Nano-Manufacturing and ... [https://gtr.ukri.org/projects?ref=EP%2FR025304%2F1]
- 63. Nanosensors Market Size to Surge USD 1838.11 Mn by 2034 [https://www.precedenceresearch.com/nanosensors-market]
- 64. Nanofabrication Market Size, Key Highlights, Sustainability ... [https://www.linkedin.com/pulse/nanofabrication-market-size-key-highlights-6g7je/]
- 65. Strategizing Growth: Nano Biosensors Industry Market's ... [https://www.marketreportanalytics.com/reports/nano-biosensors-industry-87351]
- 66. Two Distinct Sample Prep Approaches to Overcome Matrix ... [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/analytical-chemistry/solid-phase-extraction/sample-prep-overcome-matrix-effect?srsltid=AfmBOoqg0hvqPzQYq7oALTYgX45MVfh10W6NBj5QlhpsGjxEPksYFUkQ]
- 67. Overcoming the Effects of Matrix Interference in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3290108/]
- 68. Nanobiosensors in diagnostics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5998262/]
- 69. Chemistry-informed recommender system to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318058/]
- 70. Experts See 17 Laboratory Trends Dominating 2025 [https://clpmag.com/diagnostic-technologies/experts-see-17-laboratory-trends-dominating-2025/]
- 71. A systematic review and meta-analysis of diagnostic ... [https://www.nature.com/articles/s41746-025-01543-z]
- 72. Editorial: Advanced nanobiosensors for non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10242179/]
- 73. Aptamers Offer The Highest Batch Consistency For ... [https://aptamergroup.com/aptamers-offer-the-highest-batch-consistency-for-reliable-reproducibility/]
- 74. Nanoplasmonic Biosensors: A Comprehensive Overview and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12067471/]
- 75. Nanobiosensors: A Technology Transforming Our Present ... [https://www.icn2.cat/en/news/5521-nanobiosensors-a-technology-transforming-our-present-and-future]
- 76. Batch-to-Batch Quality Consistency Evaluation of Botanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3665986/]
- 77. Nanobiosensor‐based diagnostic tools in viral infections [https://pmc.ncbi.nlm.nih.gov/articles/PMC8420101/]
- 78. Diagnostic Challenges and Patient Safety: The Critical Role of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12134007/]
- 79. Recent advances in biomarker detection of oral squamous ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1597086/full]
- 80. Next-generation microfluidics based on artificial intelligence [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25007507]
- 81. AI-Enabled Microfluidics for Respiratory Pathogen Detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473228/]
- 82. Artificial Intelligence-Assisted Nanosensors for Clinical ... [https://www.mdpi.com/2079-6374/15/10/656]
- 83. Sensitivity and Limit of Detection [https://www.sciencedirect.com/science/article/abs/pii/S092234870870220X]
- 84. The difference between sensitivity and detection range in ... [https://www.bosterbio.com/blog/post/the-difference-between-sensitivity-and-the-minimum-level-of-assay-range-in-elisa-testing?srsltid=AfmBOopxIFGGL3roeSwaK_ZR106e604z_clTpiWiW7NVZuUch-Y4Y--M]
- 85. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 86. Detection limit [https://en.wikipedia.org/wiki/Detection_limit]
- 87. Detection limit matters. Sensitivity not really [https://www.biolinscientific.com/blog/qcm-sensitivity-vs-limit-of-detection-lod?update_2025=1]
- 88. Recent Advancements in Nanobiosensors: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9599941/]
- 89. Rapid Detection and One-Step Differentiation of Cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369906/]
- 90. Five Methods You Can Use to Overcome Zika-Dengue ... [https://thenativeantigencompany.com/five-methods-you-can-use-to-overcome-zika-dengue-cross-reactivity/]
- 91. Nanosensors in healthcare: transforming real-time monitoring ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00125k]
- 92. Development and performance characteristics evaluation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8051012/]
- 93. A systematic review of allergen cross-reactivity: Translating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10959674/]
- 94. Laboratory Turnaround Time - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2282400/]
- 95. Advancements in nanobiosensor technologies for in-vitro ... [https://www.sciencedirect.com/science/article/pii/S2405844024163372]
- 96. Radiology Turnaround Time (TAT) Benchmarks [https://www.aag.health/post/radiology-turnaround-time-benchmarks]
- 97. Review Frontiers in nano-biosensors for drug monitoring [https://www.sciencedirect.com/science/article/abs/pii/S1385894725068779]
- 98. Western Blot: When to Use Each Immunoassay Technique ELISA vs [https://www.thermofisher.com/blog/life-in-the-lab/western-blot-or-elisa/]
- 99. A comparison of conventional and advanced electroanalytical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9270057/]
- 100. Recent Progress in DNA Biosensors: Target-Specific and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384124/]
- 101. PCR Independent Strategy-Based Biosensors for RNA ... [https://www.mdpi.com/2079-6374/14/4/200]
- 102. Serologic LSPR-nanosensor against SARS-COV-2 ... [https://www.nature.com/articles/s44328-025-00029-y]
- 103. Nano-biosensor based on the combined use of ... [https://www.sciencedirect.com/science/article/pii/S2214180422000046]
- 104. How AI Achieves 94% Accuracy In Early Disease Detection [https://globalrph.com/2025/04/how-ai-achieves-94-accuracy-in-early-disease-detection-new-research-findings/]