CRISPR-Cas9 Delivery via Lipid Nanoparticles: A 2024 Guide to In Vivo Cancer Gene Editing for Therapeutic Development
This article provides a comprehensive, current analysis of lipid nanoparticle (LNP)-mediated delivery of CRISPR-Cas9 for cancer gene editing, tailored for researchers and drug development professionals.
CRISPR-Cas9 Delivery via Lipid Nanoparticles: A 2024 Guide to In Vivo Cancer Gene Editing for Therapeutic Development
Abstract
This article provides a comprehensive, current analysis of lipid nanoparticle (LNP)-mediated delivery of CRISPR-Cas9 for cancer gene editing, tailored for researchers and drug development professionals. We first explore the foundational principles of CRISPR-Cas9 mechanics and LNP design rationales for overcoming delivery barriers. Methodologically, we detail state-of-the-art formulation strategies, cargo loading (mRNA/protein/RNP), and in vivo targeting approaches for solid and hematological tumors. The troubleshooting section addresses critical challenges including immunogenicity, editing efficiency, and off-target effects. Finally, we present a comparative validation of LNP platforms against viral and other non-viral vectors, examining preclinical efficacy data, safety profiles, and translational readiness. This synthesis aims to inform strategic decisions in next-generation oncology therapeutic development.
Foundations of CRISPR-LNP Synergy: Core Principles and Rationale for Cancer Therapy
CRISPR-Cas9 is a programmable genome-editing system derived from bacterial adaptive immunity, repurposed for precise genetic manipulation. In oncology research, it enables the functional validation of oncogenes and tumor suppressors, the creation of engineered cell therapies (e.g., CAR-T cells), and the direct targeting of cancer-driving mutations. The efficacy of this toolbox is contingent upon the efficient delivery of its ribonucleoprotein (RNP) components into target cells. This protocol series is framed within a thesis investigating lipid nanoparticle (LNP)-mediated delivery of CRISPR-Cas9 for in vivo cancer gene editing, emphasizing RNP formulation for enhanced stability and editing precision.
Mechanism of Action: Key Components & Quantitative Benchmarks
The core CRISPR-Cas9 system requires two fundamental components: the Cas9 endonuclease and a single guide RNA (sgRNA). The sgRNA directs Cas9 to a specific genomic locus complementary to its 20-nucleotide spacer sequence, adjacent to a Protospacer Adjacent Motif (PAM; NGG for SpCas9). Cas9 induces a double-strand break (DSB), which is repaired by the cell's endogenous mechanisms, primarily Non-Homologous End Joining (NHEJ) or Homology-Directed Repair (HDR).
Table 1: Key Components of the CRISPR-Cas9 Toolbox for Oncology
| Component | Description | Key Consideration for Oncology Targets |
|---|---|---|
| Cas9 Nuclease | Effector protein (commonly S. pyogenes SpCas9, ~160 kDa) that cleaves DNA. | Size impacts delivery efficiency; engineered variants (e.g., SaCas9) are smaller for viral delivery. |
| Single Guide RNA (sgRNA) | Chimeric RNA combining tractRNA and crRNA for target recognition. | On-target efficiency and off-target potential must be rigorously validated for each target locus. |
| Protospacer Adjacent Motif (PAM) | Short DNA sequence (e.g., 5'-NGG-3') required for Cas9 binding. | Defines targetable genomic sites; base editors or Cas9 variants with altered PAMs expand target range. |
| Repair Template | Donor DNA template for HDR-mediated precise editing. | Essential for introducing specific point mutations or knock-ins; low efficiency in non-dividing cells. |
Table 2: Quantitative Benchmarks for CRISPR-Cas9 Editing in Cancer Cell Lines
| Parameter | Typical Range | Measurement Method |
|---|---|---|
| Transfection Efficiency (RNP) | 70-95% in immortalized lines | Flow cytometry for fluorescently tagged RNPs |
| Indel Formation Rate (NHEJ) | 20-80% | T7 Endonuclease I assay or NGS |
| HDR Efficiency | 1-20% | NGS or phenotypic selection |
| Off-Target Indel Frequency | <0.1% - 5.0% (target-dependent) | GUIDE-seq or CIRCLE-seq |
Detailed Protocols
Protocol 3.1: Formulation of CRISPR-Cas9 RNP for LNP Encapsulation
Objective: Prepare purified, pre-assembled Cas9-sgRNA RNP complexes suitable for LNP formulation. Materials: Recombinant Cas9 protein (purified), sgRNA (chemically synthesized or in vitro transcribed), Nuclease-Free Duplex Buffer, Amicon Ultra centrifugal filters. Procedure:
- Resuspend sgRNA in nuclease-free duplex buffer to 100 µM.
- Assemble RNP by mixing Cas9 protein and sgRNA at a 1:1.2 molar ratio (e.g., 10 µM Cas9 with 12 µM sgRNA) in a total volume of 100 µL.
- Incubate at 25°C for 10 minutes for complex formation.
- Concentrate and exchange buffer into citrate buffer (pH 5.0) using a 100-kDa molecular weight cutoff centrifugal filter to prepare for LNP encapsulation. Determine final RNP concentration via spectrophotometry.
Protocol 3.2:In VitroValidation of On-Target Editing in Cancer Cells
Objective: Assess CRISPR-Cas9 RNP (delivered via LNPs or electroporation) editing efficiency at the target locus. Materials: Target cancer cell line (e.g., A549, HeLa), formulated LNPs containing RNP, Opti-MEM, genomic DNA extraction kit, PCR reagents, T7 Endonuclease I assay kit. Procedure:
- Seed cells in a 24-well plate at 70% confluence.
- Treat cells with LNP-RNP complexes (e.g., 100 nM RNP final concentration) or electroporate with 2 µg of RNP.
- Incubate cells for 72 hours to allow for editing and repair.
- Harvest cells and extract genomic DNA.
- Amplify the target genomic region (~500-800 bp) via PCR.
- Denature and reanneal the PCR amplicons to form heteroduplex DNA.
- Digest with T7 Endonuclease I for 1 hour at 37°C.
- Analyze fragments via agarose gel electrophoresis. Calculate indel percentage using densitometry.
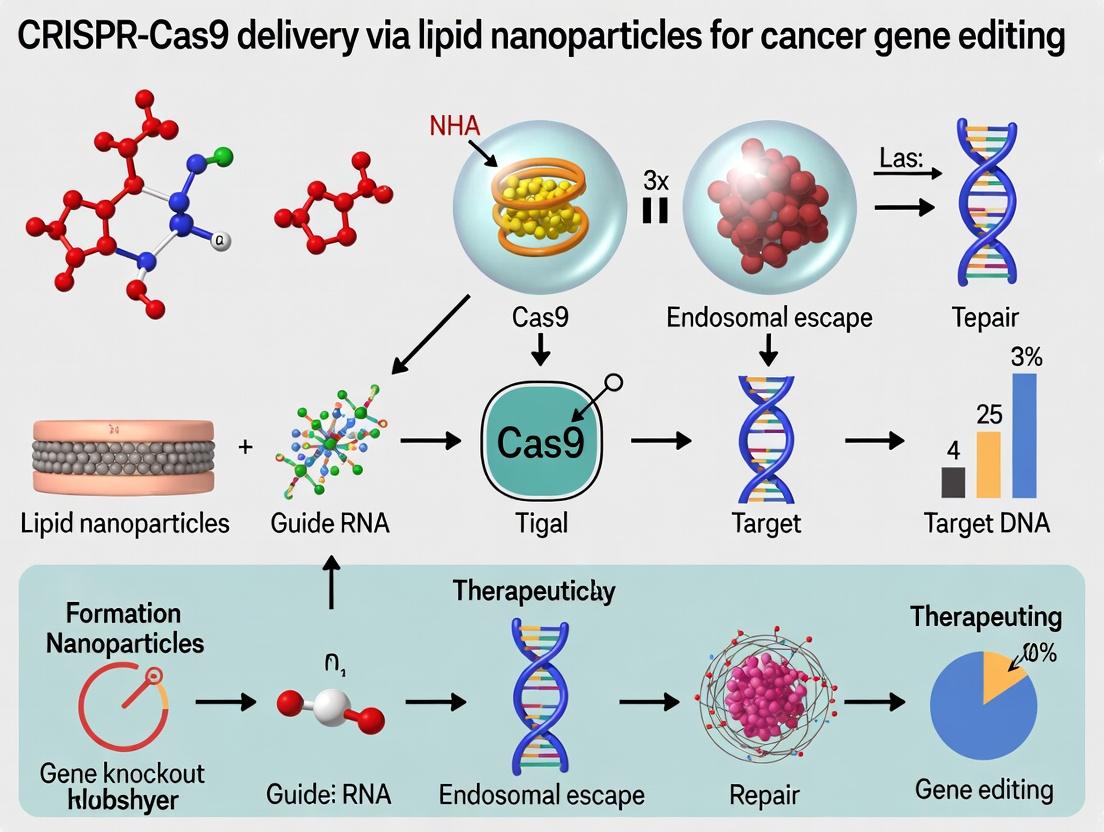
Visualizing the Workflow and Mechanism
Title: LNP-CRISPR RNP Workflow for Cancer Cells
Title: CRISPR-Cas9 DNA Targeting and Repair Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CRISPR-Cas9 Oncology Research
| Reagent/Material | Supplier Examples | Function in Protocol |
|---|---|---|
| SpCas9 Nuclease (NLS-tagged) | Thermo Fisher, Synthego, IDT | Core editing enzyme; nuclear localization ensures genomic access. |
| Chemically Modified sgRNA | Synthego, IDT, Horizon | Enhances stability and reduces immunogenicity; critical for RNP activity. |
| Ionizable Cationic Lipid (e.g., DLin-MC3-DMA) | Avanti, MedChemExpress | Key LNP component for encapsulating RNP and enabling endosomal escape. |
| T7 Endonuclease I | NEB, Integrated DNA Technologies | Detects indels by cleaving mismatched heteroduplex DNA (Protocol 3.2). |
| Nucleofector System & Kits | Lonza | Electroporation-based delivery of RNP to hard-to-transfect cells. |
| NGS-based Off-Target Analysis Kit (e.g., GUIDE-seq) | Integrated DNA Technologies | Comprehensive profiling of potential off-target editing sites. |
| Genomic DNA Cleanup Kit | Qiagen, Zymo Research | Rapid purification of high-quality gDNA for downstream editing analysis. |
Why Lipid Nanoparticles? Overcoming the Systemic Delivery Challenge for In Vivo Gene Editing
For in vivo CRISPR-Cas9 gene editing, particularly in cancer research, systemic delivery remains the paramount challenge. Viral vectors, while efficient, pose immunogenicity and insertional mutagenesis risks. Lipid nanoparticles (LNPs) have emerged as the leading non-viral platform for systemic delivery due to their ability to encapsulate large nucleic acid payloads (mRNA and sgRNA), protect them from degradation, facilitate endosomal escape, and enable targeted delivery to tissues beyond the liver through rational design.
Table 1: Comparative Delivery Modalities for In Vivo CRISPR-Cas9
| Delivery Modality | Packaging Capacity | Immunogenicity | Manufacturing | Tropism (Post-IV) | Key Limitation |
|---|---|---|---|---|---|
| AAV | < 4.7 kb | High (pre-existing/adaptive) | Complex, scalable | Broad (serotype-dependent) | Size limit, persistent expression, genotoxic risk |
| Polymer Nanoparticles | High | Moderate | Moderate | Primarily Liver/Lung | Variable batch-to-batch reproducibility, potential toxicity |
| Cationic Liposomes | High | Moderate to High | Simple | Lung, Spleen | High cytotoxicity, low serum stability |
| Ionizable Lipid LNPs | High | Low to Moderate | Scalable (T-junction) | Primarily Liver (engineered for extrahepatic) | Standard formulations are hepatotropic |
Table 2: Recent Preclinical LNP-CRISPR Studies for Cancer (2023-2024)
| Target (Cancer Model) | LNP Formulation Highlights | Payload | Key Outcome (Efficiency) | Route |
|---|---|---|---|---|
| PLK1 (HCC) | Novel ionizable lipid (LP01) | Cas9 mRNA + sgRNA | >70% gene editing in vivo, 100% tumor regression | Intravenous |
| CD47 (Glioblastoma) | LNP with BBB-targeting peptide | saCas9 mRNA + sgRNA | ~50% gene editing in tumor, significant survival benefit | Intravenous |
| PD-1 (Melanoma) | Standard MC3-based LNP | Cas9 mRNA + sgRNA | ~35% editing in T-cells, enhanced anti-tumor immunity | Intravenous |
Detailed Protocol: Formulation of CRISPR-LNPs for Systemic Delivery
Objective: To prepare ionizable lipid LNPs co-encapsulating Cas9 mRNA and a single guide RNA (sgRNA) using rapid, scalable microfluidic mixing.
I. Materials & Reagent Setup (The Scientist's Toolkit)
Table 3: Essential Research Reagent Solutions
| Reagent/Category | Example Product/Component | Function & Critical Note |
|---|---|---|
| Ionizable Lipid | DLin-MC3-DMA, SM-102, or novel proprietary lipids | Key for endosomal escape; structure determines potency & tropism. |
| Helper Lipid | DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine) | Enhances bilayer stability and in vivo circulation. |
| Cholesterol | Pharmaceutical grade | Modulates membrane fluidity and stability. |
| PEGylated Lipid | DMG-PEG2000 or DSG-PEG2000 | Controls particle size, prevents aggregation, and modulates pharmacokinetics. |
| Aqueous Phase Buffer | Citrate Buffer (pH 4.0), 10 mM | Acidic pH protonates ionizable lipid for efficient RNA encapsulation. |
| CRISPR Payload | Cas9 mRNA (purified, modified) + sgRNA (chemically modified) | Co-encapsulation at a defined mass ratio (e.g., 1:1 to 3:1 mRNA:sgRNA). |
| Microfluidic Device | NanoAssemblr Ignite or Precision NanoSystems Chip | Enables reproducible, rapid mixing for uniform particle formation. |
| Dialysis System | Slide-A-Lyzer cassettes (MWCO 20kDa) | Removes organic solvent and free components, exchanges buffer to PBS. |
II. Step-by-Step Procedure
Lipid Solution Preparation (Organic Phase):
- Combine the following lipids in ethanol at the molar ratio 50:10:38.5:1.5 (Ionizable Lipid:DSPC:Cholesterol:PEG-lipid).
- Typical total lipid concentration: 10-12 mM.
- Vortex and warm gently (37°C) to ensure complete dissolution.
RNA Solution Preparation (Aqueous Phase):
- Dilute Cas9 mRNA and sgRNA in 10 mM citrate buffer (pH 4.0).
- Maintain an N/P ratio (moles of amine groups on ionizable lipid to moles of phosphate in RNA) between 3 and 6 for optimal encapsulation. A typical starting point is N/P=4.
- Mix gently and keep on ice.
Microfluidic Mixing:
- Load the lipid-ethanol solution and RNA-citrate buffer into separate syringes.
- Set up the microfluidic instrument with a standard staggered herringbone mixer chip.
- Set the Total Flow Rate (TFR) to 12 mL/min and a Flow Rate Ratio (FRR, aqueous:organic) of 3:1.
- Initiate mixing, collecting the crude LNP suspension in a vial.
Buffer Exchange & Purification:
- Immediately dilute the crude LNP formulation with at least 1 volume of PBS (pH 7.4).
- Transfer to a dialysis cassette (MWCO 20 kDa) and dialyze against 1L of PBS for 4 hours at 4°C, with one buffer change after 2 hours.
- Alternatively, use tangential flow filtration (TFF) for larger-scale purification.
Characterization & Quality Control:
- Size and PDI: Measure by Dynamic Light Scattering (DLS). Target diameter: 70-100 nm. PDI < 0.2.
- Encapsulation Efficiency (EE%): Use Ribogreen assay. Measure fluorescence of RNA in untreated LNPs (total) and in supernatant after disruption with 1% Triton X-100 (free). Calculate EE% = [(Total - Free)/Total] x 100. Target > 90%.
- Zeta Potential: Measure in PBS. Expect slightly negative surface charge (~ -5 to -15 mV).
Pathway & Workflow Visualization
Diagram Title: LNP-Mediated Systemic CRISPR Delivery Workflow
Diagram Title: Mechanism of Ionizable Lipid-Mediated Endosomal Escape
The advent of CRISPR-Cas9 gene editing presents a transformative opportunity for oncology research, enabling the direct correction of oncogenic mutations, disruption of tumor suppressor genes, or engineering of immune cells. However, its clinical translation is critically dependent on safe and efficient in vivo delivery to tumor sites. Lipid Nanoparticles (LNPs) have emerged as the leading non-viral delivery platform, validated by the success of mRNA vaccines. This document details the anatomy of an oncology-specific LNP, focusing on the four key lipid components and their optimized formulation for CRISPR-Cas9 delivery in cancer gene editing research. The broader thesis posits that rational, tumor-microenvironment-responsive design of each LNP component is essential for achieving targeted, efficient, and safe gene editing in vivo.
Key Lipid Components and Their Functions
Table 1: Core Lipid Components of an Oncology LNP for CRISPR-Cas9 Delivery
| Component Class | Primary Function(s) in Oncology LNP | Common Examples (Current) | Key Rationale for Cancer Gene Editing |
|---|---|---|---|
| Ionizable Lipid | 1. Complexation & Protection: Binds negatively charged nucleic acids (Cas9 mRNA + gRNA or RNP) via electrostatic interaction at low pH. 2. Endosomal Escape: Becomes positively charged in acidic endosomes, destabilizes the endosomal membrane via the "proton sponge" effect or hexagonal phase formation, releasing cargo into cytosol. | DLin-MC3-DMA, SM-102, ALC-0315, C12-200, 5A2-SC8 | The ionizable pKa (~6.2-6.6) is crucial. It must be neutral at physiological pH (minimal toxicity) but cationic in tumor and endosomal microenvironments (often acidic). Enables cytosolic delivery of CRISPR machinery. |
| Phospholipid (Helper Lipid) | 1. Structural Integrity: Forms the core lamellar structure of the LNP bilayer. 2. Fusion & Permeability: Promotes membrane destabilization and fusion with the endosomal membrane, aiding escape. Often adopts non-bilayer phases. | DSPC, DOPE, DPPC | DOPE is frequently preferred over DSPC for gene editing LNPs due to its propensity to form inverted hexagonal (HII) phases that significantly enhance endosomal escape efficiency. |
| Cholesterol | 1. Membrane Stability & Rigidity: Modulates LNP bilayer fluidity and integrity. 2. Fusion Facilitation: Enhances interaction and fusion with cellular membranes. 3. PEG-lipid Anchoring: Helps stabilize the PEG-lipid within the bilayer. | Cholesterol (often phytosterols like β-sitosterol) | Phytosterols (e.g., β-sitosterol) are increasingly used to replace cholesterol, shown to improve in vivo efficacy by further enhancing endosomal escape and intracellular processing. |
| PEG-Lipid | 1. Stealth & Stability: Creates a hydrophilic barrier, reducing opsonization, preventing aggregation, and prolonging circulation time. 2. Particle Size Control: During formulation, its incorporation dictates final LNP size via surface coverage. 3. Controllable Shedding: PEG dissociation in vivo facilitates cellular uptake. | DMG-PEG2000, DSG-PEG2000, ALC-0159 | Shorter acyl chains (C14 vs. C18) enable faster dissociation ("PEG shedding") post-injection, crucial for LNP-cell interaction and uptake by tumor cells. Rate of shedding can be tuned for optimal pharmacokinetics. |
Experimental Protocols for LNP Characterization & Testing
Protocol 3.1: Microfluidic Formulation of CRISPR-LNPs Objective: To prepare uniform LNPs encapsulating CRISPR-Cas9 mRNA and single-guide RNA (sgRNA) via rapid mixing. Materials: Ionizable lipid, Helper lipid (DOPE), Cholesterol, PEG-lipid (DMG-PEG2000), CRISPR-Cas9 mRNA, sgRNA, Ethanol (100%), Sodium Acetate Buffer (pH 4.0), PBS (pH 7.4), Microfluidic mixer chip (e.g., NanoAssemblr), Syringes, Tubing. Procedure:
- Prepare the lipid mix in ethanol: Combine ionizable lipid, DOPE, cholesterol, and PEG-lipid at a molar ratio (e.g., 50:10:38.5:1.5). Adjust total lipid concentration to ~10-20 mM.
- Prepare the aqueous phase in sodium acetate buffer (pH 4.0): Combine CRISPR-Cas9 mRNA and sgRNA at a pre-optimized mass ratio (e.g., 1:1 by weight). Total nucleic acid concentration should match the desired N/P ratio (molar ratio of amine groups in ionizable lipid to phosphate groups in RNA).
- Load the lipid and aqueous phases into separate syringes.
- Connect syringes to a microfluidic mixer. Set the total flow rate (TFR) to 12-15 mL/min and the flow rate ratio (FRR, aqueous:organic) to 3:1.
- Initiate mixing. The resulting suspension is collected in a vial.
- Immediately dialyze the formed LNPs against PBS (pH 7.4) for 2-4 hours at room temperature using a dialysis cassette (MWCO 10-20 kDa) to remove ethanol and adjust the pH.
- Filter the final LNP formulation through a 0.22 µm sterile filter. Store at 4°C.
Protocol 3.2: In Vitro Gene Editing Assessment in Cancer Cell Lines Objective: To quantify CRISPR-Cas9-mediated knockout efficiency in tumor cells treated with CRISPR-LNPs. Materials: Cultured target cancer cells (e.g., A549, HeLa), CRISPR-LNPs targeting a reporter or endogenous gene (e.g., EMSY, PLK1), Lipofectamine (positive control), Genomic DNA extraction kit, T7 Endonuclease I or Surveyor Mutation Detection Kit, NGS library prep kit (optional), Flow cytometer for fluorescent reporters. Procedure:
- Seed cells in a 24-well plate at 70-80% confluence.
- After 24h, treat cells with CRISPR-LNPs at varying doses (e.g., 0.1-1.0 µg RNA/well). Include untreated and Lipofectamine-transfected controls.
- Incubate cells for 48-72 hours.
- Harvest: Extract genomic DNA using a commercial kit.
- Amplify: PCR amplify the genomic target region surrounding the CRISPR cut site.
- Assess Editing: Option A (T7E1/Surveyor): Denature and reanneal PCR products to form heteroduplexes. Digest with mismatch-cleaving enzyme (T7E1) and analyze fragments by agarose gel electrophoresis. Calculate indel % = 100 * (1 - sqrt(1 - (b+c)/(a+b+c))), where a=parental band, b+c=cleavage products. Option B (NGS, Gold Standard): Purify PCR products, prepare sequencing libraries, and perform deep sequencing. Analyze reads for insertions/deletions (indels) at the target site using software (e.g., CRISPResso2).
- Functional Assay: Perform downstream assays (e.g., Western blot for protein knockdown, cell viability assay for essential oncogenes).
Visualizations
Title: LNP Journey for Tumor Gene Editing
Title: LNP Development & Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Oncology CRISPR-LNP Research
| Item | Function/Application | Example Product/Brand |
|---|---|---|
| Ionizable Lipid | The functional core of the LNP; binds nucleic acids and enables endosomal escape. Critical for efficacy. | SM-102, ALC-0315 (commercially available); Proprietary lipids (e.g., C12-200 from academic licensing). |
| Microfluidic Mixer | Enables reproducible, scalable, and rapid mixing for forming uniform, stable LNPs. | NanoAssemblr (Precision NanoSystems), µSNAP (Diagnostic Biochips), or custom chip systems. |
| Dynamic Light Scattering (DLS) Instrument | Measures LNP hydrodynamic diameter, polydispersity index (PDI), and zeta potential. | Zetasizer Nano (Malvern Panalytical), DelsaMax Pro (Beckman Coulter). |
| RiboGreen Assay Kit | Quantifies both total and free RNA to calculate LNP encapsulation efficiency accurately. | Quant-iT RiboGreen RNA Assay (Invitrogen). |
| T7 Endonuclease I / Surveyor Kit | Accessible, gel-based method for initial quantification of CRISPR-induced indel mutations. | Surveyor Mutation Detection Kit (IDT), T7 Endonuclease I (NEB). |
| Next-Generation Sequencing (NGS) Service/Kit | Gold-standard, quantitative analysis of editing efficiency, specificity, and mutation profiles. | Illumina MiSeq platform; CRISPResso2 analysis pipeline. |
| Cancer Cell Line Panel | In vitro models for screening LNP efficacy across genetic backgrounds and tissue types. | NCI-60 panel, patient-derived organoids (PDOs). |
| Syngeneic or Xenograft Mouse Models | In vivo models for evaluating biodistribution, tumor targeting, and therapeutic gene editing efficacy. | CT26 (murine colon), 4T1 (murine breast), or Hepa1-6 (murine liver) for syngeneic; various human cell line xenografts. |
This application note details target identification and validation protocols within a broader thesis framework focusing on CRISPR-Cas9 delivery via lipid nanoparticles (LNPs) for in vivo cancer gene editing. Precise target selection is paramount for developing effective LNP-CRISPR therapies. This document categorizes high-value targets, presents quantitative validation data, and provides actionable protocols for knockout/knock-in screening.
High-Value Target Categories & Validation Data
Targets are prioritized based on functional impact, clinical relevance, and suitability for LNP-CRISPR delivery (e.g., single-gependency factors).
Table 1: High-Value Oncogene Targets for Knockout
| Target Gene | Cancer Type(s) | Therapeutic Rationale | Validated sgRNA Efficiency (KO%)* | Key Functional Readout |
|---|---|---|---|---|
| KRAS (G12C/D/V) | Pancreatic, Lung, Colorectal | Drives proliferation & survival; mutation-specific targeting possible. | 85-95% | Reduced p-ERK/ p-AKT, apoptosis. |
| MYC | Breast, Lymphoma, Prostate | Master regulator of cell growth; non-druggable by conventional means. | 70-85% | Decreased proliferation, tumor regression in vivo. |
| BCL2 | CLL, Lymphoma | Anti-apoptotic protein; knockout induces intrinsic apoptosis. | 80-90% | Increased Caspase-3/7 activity. |
| EGFR (mutant) | Glioblastoma, NSCLC | Promotes uncontrolled growth; resistance to TKIs is common. | 75-88% | Inhibition of spheroid growth in 3D culture. |
Data from pooled CRISPR screens using NGS-based readout (e.g., TIDE, NGS).
Table 2: Tumor Suppressor Genes for Knock-in/Rescue
| Target Gene | Cancer Type(s) | Therapeutic Rationale | Delivery Strategy | Key Functional Readout |
|---|---|---|---|---|
| TP53 | Ovarian, Lung, Sarcoma | Restores apoptosis & cell cycle arrest. | HDR-mediated correction or wild-type cDNA knock-in. | Increased p21 expression, senescence. |
| PTEN | Prostate, Glioma | Restores PI3K/AKT pathway regulation. | HDR or homology-independent targeted integration (HITI). | Reduced p-AKT, decreased proliferation. |
| RB1 | Retinoblastoma, SCLC | Re-establishes cell cycle checkpoint control. | Large cDNA knock-in via advanced HDR methods. | G1/S arrest, reduced E2F target expression. |
Table 3: Immunomodulatory Targets for Knockout in T/CAR-T Cells
| Target Gene | Cell Type | Therapeutic Rationale | Validated KO Efficiency | Key Functional Readout |
|---|---|---|---|---|
| PD-1 (PDCD1) | Primary T-cells | Enhances anti-tumor activity by blocking exhaustion checkpoint. | >90% in primary T-cells | Increased IFN-γ secretion, enhanced tumor killing. |
| TGFBR2 | CAR-T cells | Abrogates immunosuppressive TGF-β signaling in tumor microenvironment. | 80-87% | Improved persistence in solid tumor models. |
| SOCS1 | NK/CAR-T cells | Augments JAK/STAT signaling, boosting cytokine response. | 75-82% | Enhanced IL-2/IL-15 driven expansion. |
Detailed Experimental Protocols
Protocol 3.1: In Vitro Pooled CRISPR Knockout Screen for Oncogene Dependency Objective: Identify essential oncogenes in a specific cancer cell line. Materials: Brunello or similar genome-wide sgRNA library, lentiviral packaging mix, polybrene, puromycin, genomic DNA extraction kit, NGS primers. Procedure:
- Lentivirus Production: Co-transfect HEK293T cells with sgRNA library plasmid, psPAX2, and pMD2.G. Harvest virus at 48/72h.
- Cell Infection & Selection: Infect target cancer cells at MOI~0.3 to ensure single integration. Select with puromycin (1-2 µg/mL) for 5-7 days.
- Population Maintenance: Passage cells for ~14 population doublings, maintaining >500x library representation.
- Genomic DNA & NGS Prep: Extract gDNA from initial (T0) and final (T14) populations. Amplify sgRNA regions via PCR and sequence on an Illumina platform.
- Analysis: Use MAGeCK or BAGEL2 to identify sgRNAs significantly depleted in the final population, indicating essential genes.
Protocol 3.2: LNP Formulation for In Vivo CRISPR-Cas9/sgRNA Delivery Objective: Formulate LNPs encapsulating Cas9 mRNA and sgRNA for in vivo target validation. Materials: Ionizable lipid (e.g., DLin-MC3-DMA), DSPC, cholesterol, PEG-lipid, Cas9 mRNA, sgRNA, microfluidic mixer. Procedure:
- Lipid Solution: Dissolve ionizable lipid, DSPC, cholesterol, and PEG-lipid in ethanol at molar ratio 50:10:38.5:1.5.
- Aqueous Solution: Dilute Cas9 mRNA and sgRNA (mass ratio ~3:1) in citrate buffer (pH 4.0).
- Mixing: Using a microfluidic device, mix the aqueous and ethanol phases at a 3:1 flow rate ratio (aqueous:ethanol) to form particles.
- Dialysis & Characterization: Dialyze against PBS, filter sterilize. Characterize by size (DLS, target ~80 nm), PDI, encapsulation efficiency (RiboGreen assay).
Protocol 3.3: Ex Vivo Knockout in Primary T-Cells for Immunomodulation Objective: Generate PD-1 knockout T-cells for functional assays. Materials: Human PBMCs, anti-CD3/CD28 activator, IL-2, Cas9 RNP (recombinant Cas9 + in vitro transcribed sgRNA), electroporation system. Procedure:
- T-cell Activation: Isolate PBMCs, activate with anti-CD3/CD28 beads and IL-2 (100 IU/mL) for 48h.
- RNP Complex Formation: Incubate 60 pmol Cas9 protein with 120 pmol sgRNA targeting PDCD1 for 10 min at room temp.
- Electroporation: Wash activated T-cells, resuspend in electroporation buffer. Add RNP complex and electroporate using a 4D-Nucleofector (program EO-115).
- Recovery & Validation: Culture cells in IL-2 media. After 72h, assess KO efficiency by flow cytometry (loss of PD-1 surface expression) and T7E1 assay on genomic DNA.
Visualization of Key Pathways & Workflows
Diagram Title: Oncogene Pathway and CRISPR Knockout Intervention
Diagram Title: LNP-CRISPR Workflow from Target ID to Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for CRISPR Target Validation
| Reagent/Material | Function | Example Product/Note |
|---|---|---|
| Validated sgRNA Libraries | Genome-wide or focused sgRNA sets for pooled screens. | Brunello (4 sgRNAs/gene) or Calabrese (kinase/phosphatase) libraries. |
| High-Activity Cas9 | Endonuclease for DNA cleavage. | Recombinant SpCas9 (NLS-tagged) for RNP assembly; Cas9 mRNA for LNP delivery. |
| Ionizable Cationic Lipid | Key LNP component for encapsulating nucleic acids and endosomal escape. | DLin-MC3-DMA or SM-102. Critical for in vivo delivery efficiency. |
| Microfluidic Mixer | Enables reproducible, scalable LNP formation via rapid mixing. | NanoAssemblr Ignite or similar. Ensures uniform particle size. |
| NGS-Based KO Analysis Kit | Quantifies editing efficiency and screen results. | Illumina CRISPR sgRNA library sequencing kits; TIDE or ICE analysis software. |
| Electroporation System | Enables high-efficiency RNP delivery to hard-to-transfect cells (e.g., T-cells). | Lonza 4D-Nucleofector with optimized cell-type specific kits. |
| Activated T-cell Media | Supports expansion and viability of primary T-cells during editing. | TexMACS or similar, supplemented with IL-2/IL-7/IL-15. |
Application Notes
In Vivo Gene Editing for Solid Tumors
Recent preclinical studies have demonstrated successful in vivo editing of oncogenes (e.g., KRAS G12D) and checkpoint genes (e.g., PD-1) within solid tumors using intravenously or intratumorally administered CRISPR-LNPs. These LNPs, often formulated with ionizable lipids like SM-102 or ALC-0315, achieve tumor-selective delivery through both passive (EPR effect) and active targeting mechanisms. Editing efficiencies in murine models range from 10-45% in tumor tissue, leading to significant tumor growth inhibition and, in some cases, complete regression when combined with immune checkpoint blockade.
Ex Vivo Engineering of Cell Therapies
CRISPR-LNPs are being utilized to engineer next-generation CAR-T and TCR-T cells ex vivo. This approach enables highly efficient, non-viral knockout of endogenous genes (e.g., TRAC, PDCD1) and simultaneous targeted knock-in of therapeutic transgenes. Protocols using pre-complexed Cas9 RNP loaded into LNPs show >80% knockout and ~30-40% knock-in efficiency in primary human T cells within 24-48 hours, significantly accelerating manufacturing timelines compared to viral vectors.
Targeting Non-Coding Regulatory Elements
Beyond protein-coding oncogenes, programs are targeting non-coding genomic elements, such as enhancers and promoter regions driving oncogene expression. This requires precise delivery of base editors or prime editors via LNPs. Success is measured by deep sequencing to assess low-frequency editing (1-10%) that results in a measurable downstream transcriptional downregulation of the target oncogene (e.g., MYC).
Protocols
Protocol 1: Formulation of Targeted CRISPR-LNPs for Systemic Administration
Objective: Prepare PEGylated LNPs encapsulating saCas9 mRNA and sgRNA targeting a tumor-associated antigen gene.
Materials:
- Ionizable lipid (e.g., ALC-0315)
- Helper phospholipid (DSPC)
- Cholesterol
- PEG-lipid (DMG-PEG2000)
- saCas9 mRNA (cleanCap, poly(A)-tail)
- sgRNA (chemically modified)
- Ethanol solution
- Sodium acetate buffer (pH 4.0)
- Phosphate-buffered saline (PBS)
- Microfluidic mixer (e.g., NanoAssemblr)
Procedure:
- Lipid Stock Preparation: Dissolve ionizable lipid, DSPC, cholesterol, and DMG-PEG2000 in ethanol at a molar ratio of 50:10:38.5:1.5 to a total lipid concentration of 12.5 mM.
- Aqueous Phase Preparation: Dilute saCas9 mRNA and sgRNA in sodium acetate buffer (pH 4.0) to a final concentration of 0.2 mg/mL total RNA. Maintain an N:P ratio of 6:1.
- Mixing: Using a microfluidic mixer, combine the ethanol lipid phase and the aqueous RNA phase at a 3:1 flow rate ratio (total flow rate: 12 mL/min).
- Formulation & Dialysis: Immediately dilute the formed LNP suspension in 1X PBS (pH 7.4). Dialyze against PBS for 4 hours at 4°C using a 100 kDa MWCO membrane to remove ethanol and exchange the buffer.
- Characterization: Measure particle size and PDI by DLS, encapsulation efficiency by RiboGreen assay, and test sterility.
Protocol 2: In Vivo Efficacy Assessment in an Orthotopic Tumor Model
Objective: Evaluate the antitumor activity of CRISPR-LNPs targeting KRAS G12D in a pancreatic cancer model.
Materials:
- KPC-derived murine cancer cells (harboring KRAS G12D)
- C57BL/6 mice
- Prepared CRISPR-LNPs (targeting KRAS)
- Control LNPs (scramble sgRNA)
- IVIS imaging system
- Tissue homogenizer
- Next-generation sequencing (NGS) platform
Procedure:
- Tumor Implantation: Surgically implant KPC cells into the pancreas of C57BL/6 mice (n=10/group).
- Treatment: At day 7 post-implantation, administer CRISPR-LNPs or control LNPs via tail vein injection (2 mg/kg mRNA dose). Repeat dosing every 5 days for a total of 3 injections.
- Monitoring: Monitor tumor growth weekly via ultrasound or bioluminescence imaging. Record body weight and signs of toxicity.
- Terminal Analysis: At day 28, euthanize animals. Harvest tumors, liver, and spleen.
- Editing Analysis: Homogenize tissues. Isolate genomic DNA. Perform PCR amplification of the KRAS target locus and analyze editing frequency by NGS.
- Histopathology: Fix tissues in formalin, section, and stain with H&E or for markers of apoptosis (TUNEL) and proliferation (Ki67).
Data Tables
Table 1: Summary of Select Clinical-Stage CRISPR-LNP Programs (2023-2024)
| Developer/Sponsor | Program/Target | Indication | Phase | Key Delivery Details | Primary Endpoints (Clinical) |
|---|---|---|---|---|---|
| Intellia Therapeutics | NTLA-2001 (TTR gene) | Hereditary ATTR Amyloidosis | Phase 3 | LNP: Proprietary, liver-tropic | Serum TTR reduction, safety |
| Beam Therapeutics | BEAM-101 (BCL11A enhancer) | Sickle Cell Disease | Phase 1/2 | LNP: For ex vivo HSC editing | HbF levels, transfusion needs |
| Verve Therapeutics | VERVE-101 (PCSK9 gene) | HeFH / ASCVD | Phase 1b | LNP: GalNAc-LNP, liver-targeted | Serum PCSK9 & LDL-C reduction |
| (Preclinical Leaders) | KRAS G12D / PD-1 | Solid Tumors | IND-enabling | Tumor-targeted LNP | Tumor editing %, ORR in planned trials |
Table 2: Preclinical Efficacy Data from Recent CRISPR-LNP Studies in Oncology Models
| Target Gene | Cancer Model | LNP Formulation | Route | Editing Efficiency (% indels) | Outcome (vs. Control) | Citation (Year) |
|---|---|---|---|---|---|---|
| PD-1 | MC38 Colon Carcinoma | ALC-0315-based | i.v. | 35% (TILs) | 60% tumor growth inhibition | Liu et al., 2023 |
| PLK1 | HCC (Orthotopic) | C12-200-based | i.v. | 22% (tumor) | 80% survival increase (Day 60) | Wang et al., 2023 |
| KRAS G12D | Pancreatic (KPC) | Custom ionizable lipid | i.t. | 41% (tumor) | Complete regression in 3/10 mice | Wang et al., 2024 |
| CDK4 | Glioblastoma | DLin-MC3-DMA-based | i.v. (CED) | 18% (tumor) | Doubled median survival | Patel et al., 2024 |
Visualizations
Title: CRISPR-LNP Journey from Injection to Gene Editing
Title: Development Pipeline for CRISPR-LNP Cancer Therapies
The Scientist's Toolkit
Table 3: Essential Research Reagents for CRISPR-LNP Cancer Research
| Reagent/Material | Function/Description | Example Vendor/Cat. No. (Representative) |
|---|---|---|
| Ionizable Cationic Lipids | Critical for RNA encapsulation and endosomal escape. Protonation in acidic endosomes disrupts the membrane. | SM-102 (Avanti), ALC-0315 (MedKoo), DLin-MC3-DMA (Sigma) |
| Modified Nucleoside mRNA | Template for Cas9 protein expression. CleanCap and poly(A) tails enhance stability and translation. | Trilink Biotechnologies (Cas9 mRNA) |
| Chemically Modified sgRNA | 2'-O-methyl and phosphorothioate modifications at 3' ends improve stability and reduce immunogenicity. | Synthego, IDT |
| Microfluidic Mixer | Enables reproducible, scalable production of uniform LNPs via rapid mixing of lipid and aqueous phases. | Precision NanoSystems (NanoAssemblr), Dolomite |
| RiboGreen Assay Kit | Fluorescent assay to quantify both encapsulated and total RNA, calculating encapsulation efficiency. | Invitrogen (R11490) |
| NGS Editing Analysis Kit | Amplification and barcoding kit for deep sequencing to quantify indel frequencies at target loci. | Illumina (Miseq), IDT (xGen Amplicon) |
| GalNAc Conjugates | Ligands attached to LNPs for active targeting of hepatocytes (liver) via the asialoglycoprotein receptor. | Bio-Techne |
| Targeting Ligands (e.g., Peptides) | Conjugated to PEG-lipids to direct LNPs to specific tumor cell surface markers (e.g., integrins). | Creative Biolabs, Peptide Specialty Labs |
From Bench to Tumor: Methodologies for Formulating, Loading, and Targeting CRISPR-LNPs
Within the broader thesis on CRISPR-Cas9 delivery via lipid nanoparticles (LNPs) for cancer gene editing research, the selection of the gene-editing cargo is a critical determinant of experimental success. This guide provides a detailed comparison of three primary cargo strategies: in vitro transcribed (IVT) mRNA encoding Cas9 and sgRNA, preassembled sgRNA/Cas9 Ribonucleoprotein (RNP) complexes, and plasmid DNA (pDNA) encoding the CRISPR machinery. The choice impacts editing efficiency, specificity, duration of effect, immunogenicity, and manufacturing complexity, all pivotal for both in vitro and future in vivo therapeutic applications in oncology.
Quantitative Comparison of Cargo Strategies
The following table summarizes key characteristics based on current literature and experimental data.
Table 1: Comparative Analysis of LNP-CRISPR Cargo Strategies
| Parameter | mRNA + sgRNA | sgRNA/Cas9 RNP | Plasmid DNA (pDNA) |
|---|---|---|---|
| Editing Onset | Fast (4-12 h) | Fastest (1-4 h) | Slow (12-48 h) |
| Editing Duration | Short-lived (24-72 h) | Shortest (< 24 h) | Prolonged (days-weeks) |
| Theoretical Editing Efficiency* | High (≈ 60-80%) | Very High (≈ 70-90%) | Moderate (≈ 30-60%) |
| Off-target Risk | Moderate | Lowest | Highest |
| Immunogenicity Risk | High (IVT RNA) | Low (Protein) | High (CpG motifs) |
| Cargo Size/Complexity | Moderate (~3-4.5 kb) | Large (~160 kDa protein) | Large (~9-10 kb plasmid) |
| Formulation Complexity | Moderate | High (RNP stability) | Low |
| Manufacturing | Scalable (enzymatic) | Complex (protein expression) | Highly Scalable (bacterial) |
| Primary Application in Cancer Research | In vivo transient editing, immune cell engineering | In vitro/ex vivo high-fidelity editing (e.g., T-cells, organoids) | Stable cell line generation, screening |
*Efficiency can vary significantly based on cell type, LNP formulation, and target gene.
Detailed Protocols
Protocol 1: Formulation of LNPs Loaded with sgRNA/Cas9 RNP
Objective: To encapsulate preassembled CRISPR-Cas9 RNP complexes into ionizable lipid LNPs for high-efficiency, transient gene editing.
- RNP Complex Assembly: Mix purified recombinant Cas9 protein with synthetic sgRNA at a 1:1.2 molar ratio in nuclease-free duplex buffer (e.g., 30 mM HEPES, 100 mM KCl). Incubate at room temperature for 10-20 minutes.
- Lipid Solution Preparation: Prepare an ethanol-phase solution containing ionizable lipid (e.g., DLin-MC3-DMA), DSPC, cholesterol, and PEG-lipid at a molar ratio typical for your LNP system (e.g., 50:10:38.5:1.5). Maintain lipid total concentration at ~10 mM.
- Aqueous Phase Preparation: Dilute the assembled RNP complexes in a citrate buffer (pH 4.0) containing a stabilizer like trehalose. Final RNP concentration should be ~50 µg/mL.
- Microfluidic Mixing: Use a microfluidic device (e.g., NanoAssemblr). Set the flow rate ratio (aqueous:ethanol) to 3:1, with a total combined flow rate of 12 mL/min. Mix the two phases rapidly to induce spontaneous nanoparticle formation.
- Buffer Exchange & Dialysis: Immediately dilute the formed LNP suspension in 1x PBS (pH 7.4) to quench particle formation. Dialyze against a large volume of PBS (pH 7.4) for 2-4 hours at 4°C to remove ethanol and exchange the external buffer.
- Concentration & Characterization: Concentrate LNPs using centrifugal filters (100 kDa MWCO). Characterize by dynamic light scattering (DLS) for size and PDI, and measure RNP encapsulation efficiency using a Ribogreen assay.
Protocol 2: Assessing Gene Editing Efficiency via T7 Endonuclease I (T7EI) Assay
Objective: To quantify indel formation at the target genomic locus following LNP-mediated delivery.
- Cell Transfection & Harvest: Seed target cancer cells (e.g., HeLa, A549) in a 24-well plate. Treat with LNP formulations at optimized concentrations. Harvest genomic DNA 72-96 hours post-transfection using a commercial kit.
- PCR Amplification: Design primers flanking the CRISPR target site (~500-800 bp amplicon). Perform PCR using a high-fidelity polymerase. Verify amplicon size and purity by agarose gel electrophoresis.
- Heteroduplex Formation: Purify PCR products. Denature and reanneal using a thermal cycler program: 95°C for 5 min, ramp down to 85°C at -2°C/s, then to 25°C at -0.1°C/s.
- T7EI Digestion: Digest the reannealed DNA with T7 Endonuclease I (NEB) for 30-60 minutes at 37°C. Include an undigested control.
- Analysis: Run digested and control samples on a 2% agarose gel. Image and quantify band intensities. Calculate indel frequency using the formula: % Indel = 100 × [1 - (1 - (b+c)/(a+b+c))^0.5], where a is the integrated intensity of the undigested band, and b & c are the digested fragment bands.
Signaling Pathways and Workflows
Title: Workflow of CRISPR Cargo Strategies from LNP to Gene Editing
Title: Key Pathways in LNP Delivery and Cargo-Specific Responses
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for LNP-CRISPR Cancer Gene Editing Research
| Reagent/Material | Function in Research | Example/Notes |
|---|---|---|
| Ionizable Cationic Lipid | Core LNP component enabling nucleic acid/protein encapsulation and endosomal escape. | DLin-MC3-DMA, SM-102, ALC-0315. Critical for in vivo delivery. |
| Microfluidic Mixer | Enables reproducible, scalable production of uniform, stable LNPs. | NanoAssemblr (Precision NanoSystems), microfluidic chips. Essential for protocol standardization. |
| Recombinant Cas9 Protein | For RNP assembly. High-purity, nuclease-free, with nuclear localization signals (NLS). | Commercial sources (e.g., IDT, Thermo Fisher) or in-house purification from E. coli. |
| Chemically Modified sgRNA | Enhances stability and reduces immunogenicity of both RNP and mRNA strategies. | Incorporation of 2'-O-methyl, phosphorothioate bonds. Synthesized commercially. |
| T7 Endonuclease I (T7EI) | Enzyme for detecting indel mutations via mismatch cleavage in PCR amplicons. | Standard for initial efficiency screening. Consider next-gen sequencing for deeper analysis. |
| Ribogreen/Quant-iT Assay | Fluorescent nucleic acid stain for quantifying encapsulation efficiency of RNA/RNP cargo. | Measures free vs. encapsulated cargo post-formulation. |
| Cell Line with Endogenous Target | Cancer cell line with a readily editable, phenotypically relevant gene for functional assays. | e.g., EML4-ALK in NSCLC lines, KRAS in pancreatic lines. |
| Next-Generation Sequencing (NGS) Library Prep Kit | For unbiased, quantitative assessment of on-target editing and genome-wide off-target analysis. | Critical for preclinical safety profiling. Amplicon-based kits available. |
This application note provides detailed protocols for the formulation of lipid nanoparticles (LNPs) for the delivery of CRISPR-Cas9 ribonucleoprotein (RNP) complexes or mRNA for cancer gene editing research. The reproducible and scalable production of LNPs is critical for in vitro and in vivo studies targeting oncogenes. We compare two primary mixing methodologies: precise microfluidic mixing and conventional T-junction mixing, focusing on their impact on LNP characteristics critical for editing efficiency.
Quantitative Comparison: Microfluidics vs. T-Junction Mixing
Table 1: Comparative Output Parameters of LNP Formulation Methods
| Parameter | Microfluidic Mixing (e.g., NanoAssemblr, iLiNP) | T-Junction or In-Line Mixing | Impact on CRISPR-Cas9 Delivery |
|---|---|---|---|
| Particle Size (nm) | 60 - 100 nm (tight distribution, PDI < 0.1) | 80 - 150 nm (broader distribution, PDI 0.15 - 0.3) | Smaller, uniform size enhances tumor penetration and cellular uptake. |
| Encapsulation Efficiency (%) | > 95% for mRNA; 80-90% for RNP | 70 - 85% for mRNA; 60-75% for RNP | High EE minimizes wasted cargo, reduces cost, and improves dose consistency. |
| Polydispersity Index (PDI) | 0.05 - 0.1 | 0.15 - 0.3 | Low PDI ensures predictable pharmacokinetics and biodistribution. |
| Process Scalability | Linear scale-up via cartridge/chip number or size (mL/min to L/hr). | Challenging; scale-up alters hydrodynamics, affecting particle characteristics. | Enables seamless transition from research (mg) to preclinical (g) scales. |
| Reproducibility (Batch-to-Batch) | Excellent (Cv < 5% for size) | Moderate to Poor (Cv 10-20% for size) | Critical for generating reliable, publishable gene-editing data. |
| Mixing Time (ms) | ~1 - 10 ms | ~100 - 1000 ms | Rapid mixing prevents lipid precipitation, yielding uniform core structure. |
Detailed Experimental Protocols
Protocol 2.1: Microfluidic Formulation of CRISPR-Cas9 mRNA LNPs
Objective: To formulate uniform LNPs encapsulating CRISPR-Cas9 mRNA using a staggered herringbone micromixer (SHM) chip.
Research Reagent Solutions & Materials:
- Lipids: Ionizable cationic lipid (e.g., DLin-MC3-DMA, SM-102), DSPC, Cholesterol, PEG-lipid (DMG-PEG2000).
- Aqueous Phase: CRISPR-Cas9 mRNA in 10 mM citrate buffer, pH 4.0.
- Organic Phase: Ethanol (100%).
- Equipment: Microfluidic mixer (e.g., NanoAssemblr Benchtop), syringe pumps, PDMS or glass SHM chip.
- Buffers: 1x PBS, pH 7.4 (for dialysis), Tris-EDTA buffer.
Procedure:
- Lipid Stock Preparation: Dissolve lipids in ethanol at a molar ratio (e.g., 50:10:38.5:1.5 - ionizable lipid:DSPC:Chol:PEG-lipid). Total lipid concentration: 10-20 mM.
- Aqueous Phase Preparation: Dilute CRISPR-Cas9 mRNA in citrate buffer to a target concentration of 0.1 mg/mL. Maintain an N/P ratio (amine to phosphate) of 3-6.
- Priming: Load lipid-ethanol solution into one syringe and mRNA aqueous solution into another. Connect to microfluidic chip inputs.
- Mixing: Set total flow rate (TFR) to 12 mL/min and flow rate ratio (FRR, aqueous:organic) to 3:1. Initiate simultaneous pumping. Mixing occurs via chaotic advection in the SHM channels.
- Collection: Collect the crude LNP suspension in a vial.
- Buffer Exchange & Dialysis: Dialyze against 1x PBS (pH 7.4) for 4 hours at 4°C to remove ethanol and increase pH, allowing LNP maturation.
- Characterization: Measure size, PDI, and concentration via DLS/NTA. Quantify encapsulation efficiency using Ribogreen assay.
Protocol 2.2: T-Junction Mixing Formulation of CRISPR-Cas9 RNP LNPs
Objective: To formulate LNPs encapsulating pre-complexed Cas9 protein and sgRNA using a turbulent T-junction mixer.
Research Reagent Solutions & Materials:
- Lipids: Same as Protocol 2.1.
- Aqueous Phase: Pre-complexed Cas9 RNP in sodium acetate buffer, pH 5.0.
- Organic Phase: Ethanol (100%).
- Equipment: Two-channel syringe pump, PEEK T-junction mixer, tubing.
- Buffers: 1x PBS, pH 7.4.
Procedure:
- Lipid & Aqueous Prep: Prepare lipid ethanolic solution as in 2.1. Prepare RNP complex in acetate buffer.
- Mixer Setup: Connect lipid and aqueous streams via tubing to a T-junction, with output tubing leading to a collection vial.
- Mixing: Set aqueous and organic flow rates to equal velocities (e.g., 5 mL/min each). Turbulent mixing occurs at the junction.
- Collection & Dialysis: Collect effluent and immediately dilute with 1x PBS. Dialyze against PBS for 4 hours at 4°C.
- Characterization: As in 2.1. Use a fluorescence-based assay (if using labeled RNP) for encapsulation efficiency.
Visualized Workflows and Pathways
Diagram 1: LNP Formulation Workflow Comparison
Diagram 2: LNP Mechanism for Cancer Cell Gene Editing
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Key Research Reagent Solutions for CRISPR-LNP Production
| Item | Function & Role in Formulation | Example/Catalog Consideration |
|---|---|---|
| Ionizable Cationic Lipid | Critical for self-assembly, endosomal escape via proton sponge effect. Key determinant of potency. | SM-102, DLin-MC3-DMA, proprietary lipids. |
| Helper Phospholipid | Stabilizes LNP bilayer structure, influences fusogenicity and rigidity. | DSPC, DOPE. |
| Cholesterol | Modulates membrane fluidity and integrity, enhances stability in vivo. | Pharmaceutical grade. |
| PEGylated Lipid | Provides steric stabilization, controls particle size, reduces clearance. Impacts targeting. | DMG-PEG2000, DSG-PEG2000. |
| CRISPR Payload | Active editing machinery. mRNA (for in situ expression) or pre-complexed RNP (for immediate activity). | CRISPR-Cas9 mRNA, Cas9 protein + sgRNA. |
| Acidic Buffer | Maintains pH during mixing to keep ionizable lipid neutral, enabling proper self-assembly. | Citrate, acetate buffer, pH 4-5. |
| Microfluidic Mixer Chip | Enforces rapid, reproducible mixing via defined geometry (e.g., Staggered Herringbone). | NanoAssemblr cartridge, Dolomite chips. |
| T-Junction Fitting | Creates turbulent flow for nanoparticle precipitation in conventional method. | PEEK or stainless steel 2-in-1 union. |
| Dialysis System | Removes organic solvent, exchanges buffer to physiological pH for LNP "maturation". | Slide-A-Lyzer cassettes, tangential flow filtration. |
| Characterization Tools | Measures critical quality attributes (CQA): size, charge, encapsulation, editing efficiency. | DLS/Zetasizer, NTA, Ribogreen assay, T7E1 assay. |
Application Notes
Within the context of a broader thesis on CRISPR-Cas9 delivery for cancer gene editing, the strategic engineering of Lipid Nanoparticles (LNPs) to exploit or enhance tumor accumulation is paramount. Passive targeting, relying on the Enhanced Permeability and Retention (EPR) effect, is often considered a baseline. Active targeting, through the surface functionalization of LNPs with ligands, aims to improve specificity and cellular uptake within the tumor microenvironment. This document synthesizes current data and protocols for both approaches, focusing on their application for systemic delivery of CRISPR-Cas9 ribonucleoproteins (RNPs) or mRNA.
Quantitative Comparison of Targeting Strategies
Table 1: Key Metrics in Passive vs. Active Targeting for Anti-Tumor LNPs
| Metric | Passive Targeting (EPR) | Active Targeting (Ligand-mediated) | Measurement Method |
|---|---|---|---|
| Typical Tumor Accumulation (%ID/g) | 0.5-3% | 2-8% (varies by ligand/ model) | Quantitative bioimaging (IVIS, PET), Radioisotope tracing |
| Cellular Internalization | Primarily non-specific (e.g., endocytosis) | Receptor-mediated endocytosis | Flow cytometry (FITC-labeled LNPs), confocal microscopy |
| Influence of PEG Density | Critical: Low/medium PEG extends circulation; High PEG inhibits cellular uptake | Moderate: Requires balancing stealth (PEG) with ligand accessibility | Pharmacokinetics (PK) studies, in vitro uptake assays |
| Key Design Parameter | Particle size (70-150 nm optimal), surface charge (neutral/slight negative) | Ligand density, coupling chemistry, ligand type (antibody, peptide, small molecule) | Spectroscopy (NMR, FTIR), ELISA-style binding assays |
| Dependence on Tumor Model | High: EPR is heterogeneous (strong in xenografts, weak in many human tumors) | Moderate: Depends on receptor expression uniformity across tumor models | Immunohistochemistry, RNA-seq of target receptor |
| Primary Advantage | Simpler formulation, no risk of anti-ligand immune response | Potential for increased tumor cell specificity and uptake | - |
| Primary Challenge | Low and variable efficiency, off-target distribution | Potential for accelerated blood clearance, complex manufacturing | - |
Table 2: Common Targeting Ligands and Their Receptors for Cancer LNPs
| Ligand Type | Example Ligand | Target Receptor (Cancer Type) | Typical Conjugation Method | Key Consideration for CRISPR Delivery |
|---|---|---|---|---|
| Small Molecule | Folic Acid | Folate Receptor α (Ovarian, Lung) | PEG-lipid terminal functionalization (e.g., DSPE-PEG-Folate) | High receptor expression on many cancer cells; low cost. |
| Peptide | iRGD (CRGDKGPDC) | αvβ3/β5 Integrins + Neuropilin-1 (Various) | Maleimide-thiol coupling to cysteine on PEG-lipid | Enhances tumor penetration, not just binding. |
| Antibody Fragment | scFv (anti-EGFR) | Epidermal Growth Factor Receptor (EGFR) (Colorectal, Glioblastoma) | Thiol-maleimide or click chemistry (DBCO-Azide) | High specificity; larger size may affect PK and orientation. |
| Aptamer | AS1411 | Nucleolin (Various, esp. on tumor vasculature) | Chemical synthesis with lipid tail insertion | Good stability, lower immunogenicity than antibodies. |
| Protein | Transferrin | Transferrin Receptor (TfR) (Highly proliferative tumors) | Chemical crosslinking (e.g., SMPB) to PEG-lipid | Ubiquitous target; risk of off-target editing in healthy tissues. |
Experimental Protocols
Protocol 1: Formulation of Actively Targeted LNPs for CRISPR-Cas9 mRNA/RNP Delivery
Objective: To prepare LNPs encapsulating CRISPR-Cas9 payloads with surface-conjugated targeting ligands (e.g., folate).
Materials:
- Lipids: Ionizable cationic lipid (e.g., DLin-MC3-DMA), DSPC, Cholesterol, PEG-lipid (e.g., DMG-PEG2000), functionalized PEG-lipid (e.g., DSPE-PEG2000-Maleimide or DSPE-PEG2000-Folate).
- Payload: CRISPR-Cas9 mRNA (or sgRNA) OR pre-complexed Cas9 RNP.
- Aqueous Buffer: 10 mM citrate buffer, pH 4.0.
- Non-aqueous Solvent: Ethanol.
- Dialysis Buffer: 1x PBS, pH 7.4.
- Targeting Ligand: Folate-PEG-DSPE (for pre-insertion) or thiol-functionalized ligand (e.g., cysteine-terminated peptide) for post-insertion.
- Equipment: Microfluidic mixer (e.g., NanoAssemblr), syringe pumps, dialysis cassettes (MWCO 10-20 kDa), dynamic light scattering (DLS) instrument.
Procedure:
- Lipid Solution Preparation: Dissolve ionizable lipid, DSPC, cholesterol, and PEG-lipids in ethanol at a molar ratio (e.g., 50:10:38.5:1.5). For pre-insertion active targeting: Replace 0.5 mol% of the PEG-lipid with the ligand-conjugated PEG-lipid (e.g., Folate-PEG-DSPE).
- Aqueous Solution Preparation: Dissolve CRISPR-Cas9 mRNA or RNP in citrate buffer (pH 4.0) at a concentration of 0.1 mg/mL.
- Nanoparticle Formation: Using a microfluidic mixer, rapidly mix the ethanolic lipid stream with the aqueous payload stream at a fixed flow rate ratio (typically 3:1 aqueous:ethanol) and a total flow rate of 12 mL/min. Collect the resulting LNP suspension.
- Buffer Exchange & Dialysis: Immediately dialyze the LNP suspension against 1x PBS (pH 7.4) for 4-18 hours at 4°C to remove ethanol and raise the pH, allowing stable LNP formation.
- Optional Post-Insertion: For ligands incompatible with acidic pH or ethanol, perform post-insertion. Incubate pre-formed LNPs with ligand-conjugated micelles (e.g., Maleimide-PEG-DSPE + thiol-ligand) at 37°C for 1-2 hours. Remove free ligand by size-exclusion chromatography.
- Characterization: Measure particle size, PDI, and zeta potential via DLS. Determine encapsulation efficiency using a Ribogreen assay (for mRNA) or gel electrophoresis.
Protocol 2: Evaluating Tumor Accumulation via In Vivo Imaging
Objective: To quantitatively compare the tumor accumulation of passively vs. actively targeted LNPs in a murine xenograft model.
Materials:
- LNPs: Formulated per Protocol 1, loaded with a near-infrared dye (e.g., DiR or ICG) instead of therapeutic payload, with and without targeting ligand.
- Animal Model: Immunodeficient mice (e.g., BALB/c nude) with subcutaneous human cancer xenografts (e.g., KB tumors for folate targeting).
- Equipment: IVIS Spectrum or similar in vivo imaging system, anesthesia setup, analysis software.
Procedure:
- Imaging Agent Preparation: Prepare DiR-loaded targeted and non-targeted LNPs using the standard formulation method, adding the lipophilic DiR dye to the ethanolic lipid solution.
- Animal Administration: When tumors reach ~200 mm³, randomize mice into groups (n=5). Inject each mouse intravenously via the tail vein with 100 μL of DiR-LNPs (equivalent lipid dose ~5 mg/kg).
- Longitudinal Imaging: Anesthetize mice at predetermined time points (e.g., 1, 4, 24, 48 hours) post-injection. Acquire fluorescence images (Ex/Em: 745/800 nm) using standardized settings (exposure time, f/stop).
- Ex Vivo Analysis: At the terminal time point (e.g., 48 hours), euthanize mice, harvest tumors and major organs (liver, spleen, kidneys, lungs, heart). Image organs ex vivo to quantify distribution.
- Data Quantification: Use imaging software to draw regions of interest (ROIs) around tumors and organs. Report fluorescence intensity as Radiant Efficiency ([p/s/cm²/sr] / [μW/cm²]). Calculate Tumor-to-Background or Tumor-to-Liver ratios for comparison.
Visualization Diagrams
Diagram 1: Passive vs Active Targeting Pathways for LNPs
Diagram 2: LNP Formulation Workflow for CRISPR
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Engineering Targeted LNPs
| Item / Reagent | Function / Role in Experiment | Example Vendor/Cat. No. (Representative) |
|---|---|---|
| Ionizable Cationic Lipid | Core component for encapsulating nucleic acids (mRNA, sgRNA) via electrostatic interaction; critical for endosomal escape. | DLin-MC3-DMA (MedChemExpress, HY-108027) |
| Functionalized PEG-Lipid | Provides "stealth" and extends circulation; functional group (Maleimide, DBCO, NHS) allows ligand conjugation for active targeting. | DSPE-PEG(2000)-Maleimide (Avanti, 880126P) |
| Microfluidic Mixer | Enables reproducible, scalable production of uniform LNPs via rapid mixing of lipid and aqueous phases. | NanoAssemblr Ignite (Precision NanoSystems) |
| Fluorescent Lipophilic Tracer | Incorporates into LNP lipid bilayer for in vitro and in vivo tracking (cellular uptake, biodistribution). | DiD or DiR Vybrant Dye (Thermo Fisher, V22887) |
| Quant-iT RiboGreen Assay | Quantifies encapsulated vs. free mRNA within LNPs to determine loading efficiency and capacity. | Quant-iT RiboGreen RNA Assay Kit (Thermo Fisher, R11490) |
| Thiolated Targeting Ligand | Contains free -SH group for covalent conjugation to Maleimide-functionalized LNPs via thiol-maleimide "click" chemistry. | cRGDfC peptide (Targeting αvβ3 integrin) (PeptideGen) |
| Size Exclusion Columns | Purifies post-insertion LNPs or removes unencapsulated payloads by separating based on hydrodynamic size. | Sepharose CL-4B (Cytiva, 17015001) or PD SpinTrap G-25 (Cytiva) |
| Dynamic Light Scattering (DLS) Instrument | Measures critical quality attributes (CQAs): hydrodynamic diameter (size), polydispersity index (PDI), and zeta potential. | Zetasizer Ultra (Malvern Panalytical) |
Cell-type specific delivery of CRISPR-Cas9 payloads via Lipid Nanoparticles (LNPs) is a transformative approach in precision cancer gene editing. This application note details strategies and protocols for targeting three critical cell populations in oncology: tumor cells, T cells (for CAR-T engineering), and myeloid cells. The integration of selective targeting ligands with LNP formulations enables precise genomic modifications, offering potential for next-generation therapies.
Ligand-Functionalized LNP Targeting
Current strategies employ surface-conjugated antibodies, antibody fragments, or peptides to direct LNPs to specific cell surface markers.
Table 1: Targeting Ligands and Corresponding Cell Markers
| Target Cell Type | Key Surface Marker | Targeting Ligand/Strategy | Common Payload | Editing Goal |
|---|---|---|---|---|
| Tumor Cells | EGFR, HER2, PSMA | Anti-EGFR nanobody, Transferrin | Cas9/sgRNA to TP53, KRAS | Knockout oncogenes, restore tumor suppressors |
| T Lymphocytes | CD3, CD5, CD8 | Anti-CD3 scFv, CD5-binding peptide | Cas9/sgRNA to TRAC, PDCD1 | Disrupt endogenous TCR, knockout checkpoint (PD-1) for CAR-T engineering |
| Myeloid Cells (e.g., TAMs, MDSCs) | CD11b, CD33, CSF1R | Anti-CD11b antibody, Mannose | Cas9/sgRNA to NF-κB, STAT3 | Reprogram immunosuppressive tumor microenvironment |
LNP Formulation & Delivery Efficiency Data
Table 2: Recent Performance Metrics of Targeted LNPs in vivo
| Formulation (Target) | Model | Encapsulation Efficiency (%) | Cell-Type Specificity Fold-Change (vs. Non-targeted) | In Vivo Editing Efficiency (%) | Key Reference (Year) |
|---|---|---|---|---|---|
| Anti-EGFR LNP (Tumor) | Glioblastoma (Mouse) | 92.5 ± 3.1 | 8.7x in tumor cells | 38.2 ± 5.6 in tumor tissue | (2023) |
| CD5-LNP (T Cells) | Humanized mouse | 88.7 ± 2.8 | 15.3x in circulating T cells | 62.1 ± 4.3 in splenic T cells | (2024) |
| Mannose-LNP (Myeloid) | Melanoma (Mouse) | 85.2 ± 4.5 | 11.2x in tumor-associated macrophages | 41.8 ± 6.1 in TAMs | (2023) |
Detailed Protocols
Protocol: Fabrication of Ligand-Conjugated, CRISPR-Loaded LNPs
Aim: To synthesize targeted LNPs encapsulating Cas9 mRNA and sgRNA. Materials:
- Ionizable lipid (e.g., DLin-MC3-DMA), cholesterol, DSPC, DMG-PEG2000, Maleimide-PEG2000-DMG.
- Cas9 mRNA and sgRNA (target-specific).
- Targeting ligand (e.g., scFv or nanobody) with a free cysteine or maleimide group.
- Microfluidic mixer (e.g., NanoAssemblr).
- Zetasizer Nano ZS for DLS and zeta potential.
- Ribogreen assay kit for encapsulation efficiency.
Procedure:
- Prepare Lipid Mix: Combine ionizable lipid, cholesterol, DSPC, and DMG-PEG2000-maleimide (molar ratio 50:38.5:10:1.5) in ethanol.
- Prepare Aqueous Phase: Dilute Cas9 mRNA and sgRNA in citrate buffer (pH 4.0).
- Form Nanoparticles: Use a microfluidic device to mix the lipid phase and aqueous phase at a 3:1 flow rate ratio (aqueous:organic). Collect in PBS.
- Ligand Conjugation: Incubate freshly made LNPs with thiol-functionalized targeting ligand (10:1 molar ratio of ligand:maleimide-PEG-lipid) for 2 hours at room temperature. Pass through a desalting column to remove unreacted ligand.
- Purification & Characterization: Dialyze LNPs against PBS. Measure particle size (target: 70-100 nm), PDI (<0.2), and zeta potential. Use Ribogreen assay to determine RNA encapsulation efficiency (>85% is optimal).
Protocol:Ex VivoGene Editing of Human T Cells for CAR-T Engineering
Aim: To generate knock-out (e.g., PD-1, TCR) or knock-in (CAR) CAR-T cells using CD5-targeted LNPs. Materials:
- Fresh human PBMCs or isolated CD3+ T cells.
- CD5-LNPs encapsulating Cas9 mRNA and sgRNA targeting TRAC locus and/or AAV6 donor template for CAR insertion.
- RetroNectin-coated plates, IL-2, anti-CD3/CD28 activator.
Procedure:
- T Cell Activation: Isolate CD3+ T cells from PBMCs using magnetic beads. Activate with anti-CD3/CD28 beads in TexMACS medium with 100 IU/mL IL-2 for 24-48h.
- LNP Transfection: Wash activated T cells. Resuspend at 1e6 cells/mL. Add CD5-LNPs at an mRNA dose of 50-100 ng/µL per 1e6 cells. Incubate for 4-6h.
- AAV Transduction (for knock-in): If performing CAR knock-in, add AAV6 donor vector (MOI 10^4-10^5) 24h post-LNP treatment.
- Culture & Expansion: Replace medium with fresh IL-2-containing medium. Expand cells for 7-14 days.
- QC Analysis: On day 7, assess editing efficiency via flow cytometry (loss of TCRαβ, CAR expression) and NGS of the target locus. Measure cell proliferation and phenotype.
Protocol: Assessing Tumor Microenvironment Reprogramming via Myeloid-Targeted Editing
Aim: To evaluate the functional impact of STAT3 knockout in tumor-associated macrophages (TAMs) using mannose-LNPs. Materials:
- Syngeneic tumor model (e.g., MC38 colon carcinoma in C57BL/6 mice).
- Mannose-LNPs with Cas9/sgRNA-Stat3.
- Flow cytometry antibodies: CD45, CD11b, F4/80, MHC II, CD86, CD206.
Procedure:
- LNP Administration: When tumors reach ~100 mm^3, inject mice intravenously with Mannose-LNPs (0.5 mg/kg mRNA dose) or controls. Repeat every 3-4 days for a total of 3 doses.
- Tumor Harvest & Processing: 48h after final dose, harvest tumors, digest to single-cell suspension.
- Immune Profiling: Stain cells for myeloid markers. Use flow cytometry to gate on CD45+CD11b+F4/80+ TAMs. Assess STAT3 knockout efficiency by intracellular staining for pSTAT3 or sequencing. Analyze M1/M2 polarization via MHCII/CD86 vs. CD206.
- Functional Assays: Isolate TAMs by sorting. Co-culture with activated T cells to assess suppression of T cell proliferation. Measure cytokine levels (IL-10, TGF-β, IL-12) in tumor homogenates.
Visualizations
Diagram Title: Mechanism of Targeted LNP Delivery and Gene Editing
Diagram Title: Workflow for CAR-T Cell Engineering via Targeted LNPs
Diagram Title: Myeloid Reprogramming via STAT3 Knockout
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Targeted CRISPR-LNP Research
| Reagent/Material | Function & Role in Application | Example Vendor/Product Note |
|---|---|---|
| Ionizable Cationic Lipid | Core component of LNP; enables RNA encapsulation and endosomal escape. Critical for efficiency. | DLin-MC3-DMA, SM-102, ALC-0315. Commercial kits available (Precision NanoSystems). |
| Functionalizable PEG-Lipid | Provides stealth and a conjugation point (e.g., maleimide) for attaching targeting ligands. | DMG-PEG2000, Maleimide-PEG2000-DMG. Avanti Polar Lipids. |
| Targeting Ligand (scFv, Nanobody) | Confers cell-type specificity by binding to surface markers (CD3, EGFR, etc.). | Recombinant proteins with engineered cysteine or click-chemistry handles. |
| Cas9 mRNA (Modified) | The effector protein for gene editing; nucleoside-modified mRNA reduces immunogenicity and increases translation. | Trilink BioTechnologies (CleanCap), Aldevron. |
| sgRNA (Chemically Modified) | Guides Cas9 to the specific genomic locus; chemical modifications enhance stability. | Synthego, IDT (Alt-R). |
| Microfluidic Mixer | Enables reproducible, scalable production of uniform, small-diameter LNPs. | NanoAssemblr (Precision NanoSystems), microfluidic chips (Dolomite). |
| In Vivo JetRNA | A non-targeting, high-efficiency LNP standard for benchmarking in vivo delivery. | Polyplus-transfection. |
| AAV6 Serotype | Common donor template vector for high-efficiency homology-directed repair (HDR) in T cells. | Vigene, Vector Biolabs. |
| T Cell Activation Beads | Robustly activates T cells for high editing efficiency and expansion. | Gibco Dynabeads CD3/CD28. |
| Ribogreen Assay Kit | Quantifies encapsulated vs. free RNA to determine LNP encapsulation efficiency. | Invitrogen Quant-iT RiboGreen. |
This document details application notes and protocols for in vivo administration of CRISPR-Cas9-loaded lipid nanoparticles (LNPs) in preclinical cancer models. These protocols are designed to support a thesis investigating the efficacy and safety of LNP-mediated gene editing for oncology research, with a focus on optimizing delivery parameters.
Key Research Reagent Solutions
Table 1: Essential Reagents and Materials for LNP-CRISPR Experiments
| Reagent/Material | Function/Description |
|---|---|
| CRISPR-Cas9 Plasmid DNA or mRNA | Gene editing machinery payload. sgRNA defines the genomic target. |
| Ionizable Cationic Lipid (e.g., DLin-MC3-DMA, SM-102, ALC-0315) | Key LNP component for encapsulating nucleic acids and facilitating endosomal escape. |
| Helper Lipids (DSPC, Cholesterol, PEG-lipid) | Stabilize LNP structure, modulate fluidity, and prevent rapid clearance. |
| Microfluidic Mixer (e.g., NanoAssemblr) | Enables reproducible, scalable production of monodisperse LNPs. |
| In Vivo Luciferase Reporter Cell Line | Allows for real-time, non-invasive tracking of tumor growth and response. |
| Animal Model (e.g., Immunocompetent or Xenograft mice) | Provides the biological system for evaluating efficacy and toxicity. |
| In Vivo Imaging System (IVIS) | Quantifies bioluminescent or fluorescent signals from tumors. |
| Tissue Lysis & Genomic DNA Extraction Kit | For downstream analysis of editing efficiency (e.g., NGS, T7E1 assay). |
Administration Routes: Protocols and Considerations
Intravenous (IV) Bolus Injection
Primary Protocol: This is the standard route for systemic delivery to disseminated tumors or primary tumors accessible via circulation.
- Animal Preparation: Mice are placed in a restrainer. The tail is warmed (∼37°C for 1-2 min) using a heat lamp or warm water to dilate veins.
- Injection Procedure: Using a 0.3-1 mL insulin syringe with a 29-gauge needle, the LNP formulation is injected into one of the two lateral tail veins. The needle is inserted parallel to the vein, and 100-200 µL is injected as a steady bolus over ∼10 seconds. Successful injection is indicated by lack of resistance and no immediate blanching or swelling.
- Post-Injection: Apply gentle pressure with gauze to achieve hemostasis.
- Key Notes: Formulations must be sterile, endotoxin-free, and particle size should be optimized (<150 nm preferred) for prolonged circulation.
Local/Intratumoral (IT) Injection
Primary Protocol: Used for accessible solid tumors to achieve high local concentration and minimize systemic exposure.
- Animal Preparation: Mice are anesthetized (e.g., 2-3% isoflurane). The tumor area is shaved and disinfected.
- Injection Procedure: Using a 0.3-1 mL syringe with a 29-gauge needle, the needle is inserted into the tumor mass at a shallow angle. A volume not exceeding 20-30% of the tumor volume (typically 20-100 µL) is injected slowly to prevent leakage. The needle is held in place for 10-15 seconds before withdrawal.
- Post-Injection: Monitor for leakage; if it occurs, apply gentle pressure.
- Key Notes: Ultrasound guidance can be used for deep-seated tumors. This route is ideal for assessing on-target editing with minimal off-target organ effects.
Dosing and Scheduling Parameters
Table 2: Summary of Dosing and Scheduling Parameters for LNP-CRISPR in Mouse Models
| Parameter | Typical Range for IV Administration | Typical Range for IT Administration | Key Considerations & Rationale |
|---|---|---|---|
| LNP Dose (mg/kg nucleic acid) | 0.5 - 5 mg/kg | 0.1 - 1 mg/kg total injected mass | Dose-finding is critical. Higher doses (1-5 mg/kg) often required for systemic efficacy but increase hepatotoxicity risk. |
| Injection Volume (Mouse) | 5 - 10 mL/kg (100-200 µL for 20g mouse) | 20-30% of tumor volume (max 100 µL) | Adhere to species-specific volume limits to avoid distress. |
| Particle Concentration | 0.2 - 1.0 mg/mL (nucleic acid) | 0.5 - 2.0 mg/mL (nucleic acid) | Affects viscosity and injectability. Must be characterized (size, PDI) pre-injection. |
| Dosing Frequency (Schedule) | Single dose, or Q3Dx2, Q7Dx3 | Single dose, or Q7Dx2-4 | Depends on tumor kinetics and LNP pharmacokinetics. Frequent dosing may induce anti-Cas9 immunity or PEG immunity. |
| Treatment Window | Initiate when tumors are palpable (50-100 mm³) | Initiate when tumors are 100-150 mm³ (for injectability) | Consistent baseline is required for efficacy comparisons. |
| Blood Collection for PK | 5-15 min, 30 min, 1, 2, 4, 8, 24h post-injection | Often not performed for IT | Essential for understanding systemic exposure and clearance after IV dosing. |
Detailed Experimental Protocol: Efficacy Study in a Subcutaneous Xenograft Model
Objective: Evaluate the tumor growth inhibition of CRISPR-Cas9 LNPs targeting an oncogene.
Workflow:
- Tumor Inoculation: Subcutaneously inject 1-5x10^6 luciferase-expressing cancer cells (e.g., A549-luc, HCT116-luc) into the flank of immunodeficient mice (e.g., NU/J or NSG).
- Randomization: When tumors reach 50-100 mm³, randomize mice into cohorts (n=5-10): (a) Vehicle Control, (b) Non-targeting sgRNA LNP, (c) Targeting sgRNA LNP.
- Treatment Administration: Administer LNP formulations via IV or IT route according to the parameters in Table 2. Example: 1 mg/kg, IV, Q7Dx3.
- Monitoring:
- Tumor Volume: Measure with calipers 2-3 times weekly. Calculate volume = (Length x Width²)/2.
- Bioluminescence Imaging (BLI): Image weekly after IP injection of D-luciferin (150 mg/kg) using an IVIS spectrum.
- Body Weight: Record 2-3 times weekly as a basic health metric.
- Endpoint Analysis:
- Terminal Harvest: At study endpoint (e.g., when control tumors reach 1500 mm³), collect tumors, liver, spleen, and other relevant organs.
- Editing Analysis: Isolate genomic DNA from tumors. Assess indel frequency via T7 Endonuclease I assay or Next-Generation Sequencing.
- Histopathology: Fix tissues in 10% NBF for H&E staining and immunohistochemistry.
Diagrams
Title: LNP-CRISPR Delivery and Mechanism Workflow
Title: Preclinical Efficacy Study Timeline
Optimizing Efficacy and Safety: Solving Key Challenges in CRISPR-LNP Delivery
The efficacy of CRISPR-Cas9 gene editing delivered via lipid nanoparticles (LNPs) for cancer therapy is significantly hampered by pre-existing and treatment-induced immune responses. Two primary immunogenic challenges are prevalent: (1) Adaptive immunity against the bacterial-derived Cas9 nuclease, and (2) Reactivity against polyethylene glycol (PEG), a common LNP surface polymer used to confer stealth properties. This document provides application notes and detailed protocols for researchers aiming to quantify and mitigate these immune responses to improve in vivo delivery and editing outcomes.
Quantifying Pre-existing Anti-Cas9 and Anti-PEG Immunity
Protocol 2.1: Serum ELISA for Detecting Anti-Cas9 and Anti-PEG IgG
Objective: To quantify pre-existing antibody titers in patient or model animal serum.
Materials:
- Coating Antigen: Recombinant S. pyogenes Cas9 protein (for anti-Cas9 ELISA) or methoxy-PEG-BSA conjugate (for anti-PEG ELISA).
- Coating Buffer: Carbonate-bicarbonate buffer, pH 9.6.
- Wash Buffer: PBS containing 0.05% Tween-20 (PBST).
- Blocking Buffer: PBS containing 5% non-fat dry milk or 3% BSA.
- Test Samples: Human or murine serum/plasma, serially diluted.
- Detection Antibody: HRP-conjugated anti-human IgG (Fc-specific) or anti-mouse IgG.
- Substrate: TMB (3,3',5,5'-Tetramethylbenzidine) substrate solution.
- Stop Solution: 1M H₂SO₄.
Procedure:
- Coating: Dilute coating antigen (2 µg/mL for Cas9, 5 µg/mL for PEG-BSA) in carbonate buffer. Add 100 µL per well to a 96-well high-binding plate. Seal and incubate overnight at 4°C.
- Washing: Aspirate and wash wells 3 times with 300 µL PBST.
- Blocking: Add 200 µL of blocking buffer per well. Incubate for 2 hours at room temperature (RT). Wash 3x.
- Sample Addition: Add 100 µL of serially diluted serum samples (in blocking buffer) to wells. Include blank (buffer only) and negative/positive control sera. Incubate for 2 hours at RT. Wash 5x.
- Detection: Add 100 µL of HRP-conjugated detection antibody (diluted as per manufacturer's guidelines in blocking buffer). Incubate for 1 hour at RT. Wash 7x.
- Development: Add 100 µL of TMB substrate per well. Incubate in the dark for 10-20 minutes.
- Stop & Read: Add 50 µL of stop solution per well. Immediately measure absorbance at 450 nm with a reference at 570 nm.
Data Analysis: Plot absorbance vs. serum dilution. The titer is often reported as the dilution factor that yields an absorbance value 2.1 times greater than the negative control.
Table 1: Prevalence of Pre-existing Immunity in Healthy Human Donors
| Immune Target | Assay Type | % Positive Donors (Recent Studies) | Median Titer (Range) | Key Citation (Year) |
|---|---|---|---|---|
| Anti-SpCas9 IgG | ELISA | 58-78% | ~1:100 (1:50 - 1:400) | Charlesworth et al. (2019) |
| Anti-PEG IgG | ELISA | ~40-45% | ~1:1000 (1:100 - 1:10,000) | Yang & Lai (2020) |
Strategies and Protocols for Mitigating Immunogenicity
Mitigating Anti-Cas9 Immunity
Strategy A: Epitope Mapping and Deimmunization via Mutagenesis
Protocol 3.1.A: In Silico Prediction and Validation of Immunodominant T-Cell Epitopes
- Use netMHCIIpan or similar tools to predict human MHC class II-binding peptides from the SpCas9 sequence.
- Synthesize predicted 15-mer peptides overlapping by 11 amino acids.
- Isolate CD4+ T-cells from human PBMCs.
- Co-culture T-cells with autologous antigen-presenting cells (APCs) loaded with individual peptides.
- Measure T-cell activation via IFN-γ ELISpot or flow cytometry for activation markers (CD69, CD154).
- Mutate key anchor residues in confirmed immunodominant epitopes to alanine using site-directed mutagenesis.
- Express and purify the deimmunized Cas9 variant. Validate editing efficiency and re-test immunogenicity in the T-cell assay.
Strategy B: Induction of Antigen-Specific Immune Tolerance
Protocol 3.1.B: Hepatic-Targeted mRNA-LNP Delivery for Tolerance Induction
- Tolerogen Design: Formulate LNPs with ionizable lipid (e.g., DLin-MC3-DMA), DSPC, cholesterol, and PEG-lipid to preferentially target hepatocytes. Encapsulate mRNA encoding a non-functional, immunologically "native" SpCas9.
- Animal Dosing: Administer a low dose (e.g., 0.1 mg/kg) of the Cas9 mRNA-LNP tolerogen intravenously to mice.
- Challenge: 7-14 days later, administer a therapeutic dose (e.g., 1 mg/kg) of functional Cas9/sgRNA mRNA-LNPs.
- Assessment: Compare anti-Cas9 antibody and Cas9-specific T-cell responses in tolerized vs. naive mice using Protocol 2.1 and 3.1.A.
Table 2: Efficacy of Anti-Cas9 Mitigation Strategies in Murine Models
| Strategy | Cas9 Platform | Key Metric | Result vs. Control | Ref. |
|---|---|---|---|---|
| Deimmunized Cas9 (eCas9) | mRNA-LNP | Anti-Cas9 IgG (Day 28) | ~80% reduction | Moreno et al. (2022) |
| Hepatic Tolerogen | mRNA-LNP | Anti-Cas9 IgG (Post-challenge) | ~90% reduction | Li et al. (2021) |
| Switching to SaCas9 | mRNA-LNP | Pre-existing Seroprevalence (Human) | <10% vs. >60% for SpCas9 | Wang et al. (2022) |
Mitigating Anti-PEG Immunity
Strategy C: Employing Alternative Stealth Lipids or PEG Alternatives
Protocol 3.2.C: Formulating and Testing PEG-free LNPs
- Lipid Screening: Replace standard PEG-lipid (e.g., DMG-PEG2000) with alternative stealth polymers (e.g., poly(2-oxazoline)s, polydopamine) or zwitterionic lipids.
- Formulation: Prepare LNPs via microfluidic mixing using the new stealth lipid, ionizable lipid, DSPC, and cholesterol.
- Characterization: Measure particle size (PDI), zeta potential, and encapsulation efficiency.
- In Vivo Testing: Inject LNPs (with a reporter mRNA) into PEG-immunized mice (pre-injected with PEGylated proteins). Measure anti-PEG IgM/IgG levels (Protocol 2.1) and compare reporter gene expression (e.g., luciferase) in target tissues (e.g., liver, tumor) to standard PEG-LNPs using IVIS imaging.
Strategy D: Using Low-Immunogenicity PEG Variants
Protocol 3.2.D: Synthesis and Evaluation of Branched, Low-Immunogenicity PEG-Lipids
- Synthesize or source a PEG-lipid conjugate where the PEG chain is a branched, low-molecular-weight (e.g., 1kDa) polymer.
- Formulate LNPs incorporating this variant at a reduced molar ratio (e.g., 0.5 mol% vs. standard 1.5 mol%).
- Test the immunogenicity and "accelerated blood clearance" (ABC) phenomenon in vivo compared to linear DMG-PEG2000 LNPs.
Table 3: Impact of PEG Modification on LNP Immunogenicity and Pharmacokinetics
| PEG-Lipid Type | Molar Ratio (%) | ABC Phenomenon Observed? | Anti-PEG IgM Induction | Relative Expression in Liver (vs. Naive) |
|---|---|---|---|---|
| Linear DMG-PEG2000 (Standard) | 1.5 | Yes (Strong) | High | ~20% |
| Branched PEG2000-Lipid | 1.5 | Reduced | Moderate | ~60% |
| PEG-free (Zwitterionic Lipid) | N/A | No | Negligible | >95% |
Research Reagent Solutions Toolkit
| Reagent / Material | Function/Application in Immunogenicity Research | Example Vendor/Catalog |
|---|---|---|
| Recombinant S. pyogenes Cas9 Protein | Antigen for anti-Cas9 ELISA; for in vitro immunogenicity assays. | Sino Biological, #CT117 |
| Methoxy-PEG-BSA Conjugate (5kDa PEG) | Critical antigen for detecting anti-PEG antibodies via ELISA. | Creative PEGWorks, #PG2-BNCH-5k) |
| Human IFN-γ ELISpot Kit | Quantify Cas9 peptide-specific T-cell responses at single-cell level. | Mabtech, #3420-2H) |
| Ionizable Lipid (DLin-MC3-DMA) | Core component of liver-targeting LNPs for tolerance studies. | MedChemExpress, #HY-108787) |
| DMG-PEG2000 (Linear) | Standard PEG-lipid for LNP stabilization; induces anti-PEG immunity. | Avanti Polar Lipids, #880151) |
| Branched PEG2000-DMG | Alternative PEG-lipid designed to reduce immunogenicity. | BroadPharm, #BP-22975) |
| Deimmunized Cas9 (eCas9) mRNA | Template for producing Cas9 with reduced MHC-II epitopes. | Trilink BioTechnologies, Custom) |
| Zwitterionic Lipid (e.g., DOPE-C3-PCA) | PEG-alternative for formulating stealth, PEG-free LNPs. | Sigma-Aldrich, Custom Synthesis) |
Experimental and Strategic Decision Workflows
Diagram 1: Immunogenicity Mitigation Strategy Decision Tree
Diagram 2: Anti-Cas9 Immune Response and Intervention Points
Application Notes
Optimizing Biodistribution for Tumor Targeting
Effective delivery of CRISPR-Cas9 payloads to tumor sites is the first critical hurdle. The composition and physicochemical properties of LNPs directly influence their pharmacokinetics and tissue distribution. Current research indicates that tuning the polyethylene glycol (PEG)-lipid component and incorporating targeting ligands can significantly shift biodistribution profiles from the liver (the default site for most conventional LNPs) towards tumors.
Key Quantitative Findings (Biodistribution):
| LNP Modification | PEG-Lipid Mol % | Size (nm) | Surface Charge (mV) | Primary Organ Accumulation (% Injected Dose/g, 24h) | Tumor Accumulation (% Injected Dose/g, 24h) |
|---|---|---|---|---|---|
| Conventional (MC3-based) | 1.5 | 80 | -2 to +2 | Liver: >60 | <3 |
| Short PEG Chain (C14) | 2.5 | 70 | -1 | Liver: 45 | 8 |
| PEGylated with cRGD Peptide | 1.0 | 85 | -5 | Tumor: 15 | 15 |
| Low PEG Density & Anionic | 0.5 | 100 | -15 | Spleen: 40 | 5 |
Enhancing Endosomal Escape
Once internalized, LNPs must escape the endosomal compartment to avoid lysosomal degradation and release their cargo into the cytoplasm. This is largely mediated by the ionizable lipid, which becomes positively charged in the acidic endosome and interacts with anionic endosomal membranes, leading to membrane destabilization.
Key Quantitative Findings (Endosomal Escape):
| Ionizable Lipid | pKa | Membrane Fusion Assay (% Escape) | Functional Gene Knockout In Vitro (%) | Cytotoxicity (IC50, μM) |
|---|---|---|---|---|
| DLin-MC3-DMA | 6.4 | 35% | 40% | >50 |
| SM-102 | 6.8 | 65% | 75% | 45 |
| ALC-0315 | 6.2 | 50% | 60% | >50 |
| Novel Lipid X (proprietary) | 7.1 | 70% | 80% | 30 |
Enabling Nuclear Delivery of CRISPR-Cas9 Ribonucleoprotein (RNP)
For non-dividing cancer cells, the final barrier is nuclear entry of the Cas9 RNP. While plasmid DNA can leverage the cell's nuclear import machinery during mitosis, RNP delivery requires optimization for active nuclear transport. Strategies include the incorporation of nuclear localization signals (NLS) on the Cas9 protein and using LNPs that promote rapid RNP release near the nucleus.
Key Quantitative Findings (Nuclear Delivery):
| Delivery Strategy | NLS on Cas9 | LNP Core Composition | Nuclear Localized RNP (% of Total Cellular RNP, 12h) | Editing Efficiency in Non-Dividing Cells (%) |
|---|---|---|---|---|
| Standard RNP LNP | No | Standard | 8% | 5% |
| NLS-RNP LNP | SV40 + c-Myc | Standard | 22% | 25% |
| NLS-RNP + Core-Optimized LNP | SV40 + c-Myc | Buffering Polymer | 35% | 48% |
Experimental Protocols
Protocol 1: Formulation and Characterization of Tumor-Targeted LNPs
Objective: To prepare cRGD-functionalized LNPs encapsulating Cas9 mRNA and sgRNA, and characterize their physical properties.
Materials:
- Ionizable lipid (e.g., SM-102), DSPC, Cholesterol, PEG-lipid (e.g., DMG-PEG2000), Mal-PEG2000-DSPE.
- cRGD peptide (cyclic Arg-Gly-Asp) with a terminal cysteine.
- Cas9 mRNA, sgRNA targeting gene of interest.
- Ethanol, sodium acetate buffer (pH 4.0), PBS (pH 7.4).
- Microfluidic mixer (e.g., NanoAssemblr Ignite).
Procedure:
- Lipid Mixture: Dissolve ionizable lipid, DSPC, cholesterol, and Mal-PEG2000-DSPE (molar ratio 50:10:38.5:1.5) in ethanol.
- Aqueous Phase: Dilute Cas9 mRNA and sgRNA in sodium acetate buffer (pH 4.0).
- Formulation: Using the microfluidic mixer, combine the ethanol phase and aqueous phase at a 3:1 flow rate ratio (total flow rate 12 mL/min). Collect the LNP suspension.
- Functionalization: Incubate the formed LNPs with cRGD peptide (1:5 molar ratio to Mal-PEG-lipid) at room temperature for 1 hour under gentle agitation.
- Buffer Exchange: Dialyze or use tangential flow filtration against PBS (pH 7.4) to remove ethanol and unencapsulated materials.
- Characterization: Measure size and PDI via DLS, zeta potential via electrophoretic light scattering, and RNA encapsulation efficiency using a Ribogreen assay.
Protocol 2: Quantifying Endosomal Escape Efficiency
Objective: To assess the ability of formulated LNPs to escape endosomes using a split-GFP reporter assay.
Materials:
- HeLa cells stably expressing GFP11-tagged late endosome marker (Rab7).
- LNPs encapsulating GFP1-10 mRNA.
- Confocal microscopy system with quantitative image analysis software.
- Cell culture reagents.
Procedure:
- Seed HeLa-Rab7-GFP11 cells in glass-bottom dishes.
- Treat cells with LNPs containing GFP1-10 mRNA at a predetermined optimal concentration.
- Incubate for 6 hours.
- Fix cells, stain nuclei with DAPI, and mount.
- Acquire z-stack confocal images.
- Analysis: Quantify the percentage of GFP1-10 signal (green) that is NOT co-localized with the Rab7-GFP11 signal (red) using co-localization analysis tools (e.g., Pearson's coefficient). A lower coefficient indicates higher endosomal escape.
Protocol 3: Assessing Nuclear Delivery and Editing in Non-Dividing Cancer Cells
Objective: To measure nuclear import of Cas9 RNP and subsequent gene editing efficiency in serum-arrested cells.
Materials:
- Cas9 protein conjugated with dual NLS (SV40 + c-Myc) and labeled with a fluorescent dye (e.g., Alexa Fluor 647).
- sgRNA complexed with the labeled Cas9 to form RNP.
- LNPs formulated for RNP encapsulation (e.g., using charge-mediated complexation).
- Cancer cell line (e.g., U2OS).
- Serum-free medium for cell cycle arrest.
- Flow cytometer, genomic DNA extraction kit, T7 Endonuclease I assay reagents.
Procedure:
- Induce cell cycle arrest by culturing U2OS cells in serum-free medium for 48 hours. Confirm arrest via flow cytometry for DNA content.
- Treat arrested cells with NLS-Cas9 RNP LNPs targeting a reporter or genomic locus.
- Nuclear Delivery Measurement (4h): Harvest a subset of cells, isolate nuclei using a commercial nuclear isolation kit, and measure the fluorescence intensity of the labeled Cas9 in the nuclear fraction via flow cytometry. Compare to total cellular fluorescence.
- Editing Efficiency Measurement (72h): Harvest genomic DNA from remaining cells. Amplify the target region by PCR. Perform T7 Endonuclease I assay on the PCR product and analyze fragments by gel electrophoresis to quantify indel percentage.
Diagrams
LNP Biodistribution Optimization Workflow
Ionizable Lipid-Mediated Endosomal Escape
Strategies for RNP Nuclear Delivery
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Material | Function in CRISPR-LNP Research | Example Vendor/Catalog |
|---|---|---|
| Ionizable Lipids (SM-102, ALC-0315) | Critical component for self-assembly and endosomal escape; protonation in acidic endosomes disrupts membrane. | MedChemExpress, Avanti Polar Lipids |
| PEG-Lipids (DMG-PEG2000) | Provides steric stabilization, controls particle size, and influences pharmacokinetics/biodistribution. | Avanti Polar Lipids (880151) |
| Microfluidic Mixer (NanoAssemblr) | Enables reproducible, scalable production of LNPs with precise size control via rapid mixing. | Precision NanoSystems |
| Fluorescently Labeled Cas9 Protein | Allows direct visualization and quantification of cellular uptake, endosomal escape, and nuclear delivery. | Thermo Fisher Scientific (TrueCut Cas9) |
| cRGD Peptide | Targeting ligand for functionalizing LNPs; binds to αvβ3 integrins overexpressed on tumor vasculature/cells. | Peptide International |
| T7 Endonuclease I Assay Kit | Standard method for detecting and quantifying CRISPR-induced indel mutations at the target genomic locus. | NEB (E3321) |
| Ribogreen Assay Kit | Quantifies both encapsulated and total RNA in LNP formulations to determine encapsulation efficiency. | Thermo Fisher Scientific (R11490) |
| Nuclear Isolation Kit | For clean separation of nuclei from cytoplasm to quantify nuclear-localized RNP cargo. | MilliporeSigma (NUC101) |
Application Notes
Within a research thesis focusing on CRISPR-Cas9 delivery via lipid nanoparticles (LNPs) for in vivo cancer gene editing, managing off-target effects is paramount for therapeutic safety and accurate interpretation of phenotypic outcomes. The combination of high-fidelity Cas9 variants and sophisticated sgRNA design tools is essential for establishing a robust and specific editing platform.
1. High-Fidelity Cas9 Variants: Quantitative Comparison These engineered variants reduce off-target editing by destabilizing non-specific interactions between Cas9 and the DNA backbone, while maintaining robust on-target activity. For LNP delivery, variants with high on-target potency are critical due to the transient and often limited expression window.
Table 1: Comparison of High-Fidelity *S. pyogenes Cas9 Variants*
| Variant | Key Mutations | Reported On-Target Efficiency (vs. WT) | Reported Off-Target Reduction (vs. WT) | Primary Mechanism |
|---|---|---|---|---|
| SpCas9-HF1 | N497A/R661A/Q695A/Q926A | ~70-100% (context-dependent) | Undetectable for most sgRNAs | Reduces non-specific DNA backbone contacts. |
| eSpCas9(1.1) | K848A/K1003A/R1060A | ~70-100% (context-dependent) | Significant reduction | Reduces non-specific DNA backbone contacts. |
| HypaCas9 | N692A/M694A/Q695A/H698A | Often >90% | >10,000-fold for some sites | Stabilizes fidelity-checking conformational state. |
| evoCas9 | M495V/Y515N/K526E/R661Q | Highly variable; can exceed WT | Up to 93-fold average reduction | Directed evolution for fidelity in human cells. |
| Sniper-Cas9 | F539S/M763I/K890N | Frequently >90%, can outperform WT | Strong reduction across multiple sites | Combination of fidelity and enhanced activity. |
Selection Note for LNP Delivery: evoCas9 and Sniper-Cas9 often show superior on-target activity in human cells, a critical attribute for the single-dose, transient expression typical of LNP delivery. SpCas9-HF1 and eSpCas9 remain excellent choices for well-characterized, high-efficiency target sites.
2. sgRNA Design Tools: Features and Applications Optimal sgRNA design is the first and most critical step for specificity. Modern tools integrate multiple predictive models.
Table 2: Selected sgRNA Design and Analysis Tools
| Tool Name | Primary Function | Key Feature for Off-Target Analysis | Input/Output |
|---|---|---|---|
| CRISPOR | Design & off-target prediction | Integrates multiple scoring algorithms (Doench ’16, Moreno-Mateos, etc.) and lists top off-target sites. | Input: Genomic sequence. Output: Ranked sgRNAs with predicted efficacy & off-target sites. |
| CHOPCHOP | Design & off-target prediction | Visualizes on- and off-target sites directly on the genome browser. | Input: Gene ID or genomic sequence. Output: Ranked sgRNAs with off-target loci. |
| Cas-OFFinder | Genome-wide off-target search | Searches for potential off-targets with bulges (mismatches/indels). | Input: sgRNA sequence, mismatch number, PAM. Output: List of all genomic loci meeting criteria. |
| GuideScan2 | Design for coding regions | Considers exon/intron structure and designs paired sgRNAs for deletions. | Input: Gene or region. Output: Optimal sgRNAs for gene knockouts. |
| CCTop | CRISPR/Cas9 target online tool | Predicts and ranks off-target sites with detailed mismatch positioning. | Input: Target sequence. Output: sgRNA candidates and off-target profiles. |
Protocols
Protocol 1: In Silico sgRNA Design and Off-Target Ranking for a Cancer Target Gene Objective: To design high-specificity sgRNAs targeting the coding exon of an oncogene (e.g., KRAS G12C allele) for LNP-CRISPR knockout studies. Materials: Computer with internet access, target gene sequence (FASTA format). Procedure:
- Identify Target Region: Obtain the genomic DNA sequence of the exon containing the KRAS G12C mutation (e.g., from NCBI Nucleotide). Isolate a 500bp window centered on the mutation.
- CRISPOR Analysis: a. Navigate to the CRISPOR website. b. Paste the target sequence or the genomic coordinates (e.g., chr12:25,398,284-25,398,784) into the input field. Select the correct genome assembly (e.g., hg38) and Cas9 variant (e.g., SpCas9-HF1). c. Execute the design. The tool will output a list of all possible sgRNAs with associated PAMs.
- Prioritize sgRNAs: Rank candidates based on: a. Specificity Scores: Favor sgRNAs with high "CFD specificity score" (≥70) and low "Off-target score". b. On-Target Efficiency: Use the "Doench ’16" or "Moreno-Mateos" efficiency score (≥60). c. Genomic Context: Select sgRNAs where the cut site is as close as possible to the mutation site and within the first half of the coding exon.
- Manual Off-Target Verification: a. For the top 3 candidate sgRNAs, copy the predicted top 10-20 potential off-target sites from CRISPOR. b. Cross-reference these loci with databases of functional genomic elements (e.g., UCSC Genome Browser) to rule out editing in known oncogenes, tumor suppressors, or essential genes.
- Final Selection: Choose 2-3 sgRNAs for empirical validation. Cloning-ready oligonucleotide sequences are provided by CRISPOR.
Protocol 2: Empirical Validation of sgRNA Specificity Using Targeted Deep Sequencing (in vitro) Objective: To quantify on-target and predicted off-target editing rates for candidate sgRNAs prior to LNP formulation. Materials: HEK293T or relevant cancer cell line, Lipofectamine 3000, plasmids encoding high-fidelity Cas9 (e.g., evoCas9) and sgRNA expression cassettes, PCR reagents, NGS library prep kit, Illumina-compatible sequencing platform. Procedure:
- Transfection: Co-transfect cells with the Cas9 plasmid and individual sgRNA plasmids (for each top candidate) in triplicate. Include a non-targeting sgRNA control.
- Genomic DNA Harvest: 72 hours post-transfection, harvest genomic DNA using a standard extraction kit.
- Amplicon Library Preparation: a. Primer Design: Design PCR primers (with overhangs for NGS indexes) to generate ~250-300bp amplicons spanning the on-target site and the top 3-5 predicted off-target sites for each sgRNA. b. Primary PCR: Perform first-round PCR to amplify each target locus from the genomic DNA samples. c. Indexing PCR: Add unique dual indices and full Illumina adapter sequences via a second, limited-cycle PCR. d. Pool & Purify: Quantify libraries, pool equimolarly, and purify.
- Sequencing & Analysis: Sequence the pooled library on a MiSeq (2x300bp). Process data using a CRISPR specificity analysis pipeline (e.g., CRISPResso2). a. Align reads to reference sequences. b. Quantify the percentage of indel mutations at each target locus. c. Calculate the ratio of on-target to off-target activity for each sgRNA.
- Decision Point: Select the sgRNA with the highest on-target efficiency and the greatest margin (>100-fold) over the highest off-target site for progression to in vivo LNP formulation.
Protocol 3: Formulation and Testing of LNP-Encapsulated High-Fidelity CRISPR RNP Objective: To prepare LNPs containing purified high-fidelity Cas9 protein:sgRNA ribonucleoprotein (RNP) complexes for in vivo delivery. Materials: Purified recombinant high-fidelity Cas9 protein (e.g., HypaCas9), chemically synthesized sgRNA (with 2'-O-methyl modifications), microfluidic mixer, lipid stocks (ionizable lipid, DSPC, cholesterol, PEG-lipid), PBS (pH 7.4), dialysis cassettes, dynamic light scattering (DLS) instrument. Procedure:
- RNP Complex Formation: Incubate purified Cas9 protein with synthetic sgRNA at a 1:1.2 molar ratio in duplex buffer for 10 minutes at room temperature to form active RNP complexes.
- Lipid Solution Preparation: Dissolve the ionizable lipid, DSPC, cholesterol, and PEG-lipid in ethanol at the desired molar ratio (e.g., 50:10:38.5:1.5).
- Aqueous Phase Preparation: Dilute the RNP complexes in sodium acetate buffer (pH 5.0) to a final concentration suitable for encapsulation.
- Microfluidic Mixing: Using a staggered herringbone or T-junction mixer, rapidly combine the ethanolic lipid stream with the aqueous RNP stream at a fixed flow rate ratio (typically 3:1 aqueous:ethanol). This induces spontaneous nanoparticle formation.
- Buffer Exchange & Purification: Immediately dilute the formed LNP suspension in PBS (pH 7.4). Dialyze against PBS for 4 hours to remove ethanol and stabilize the LNPs.
- Characterization: Measure particle size and polydispersity index (PDI) via DLS (target: 70-100 nm, PDI <0.2). Measure RNP encapsulation efficiency using a fluorescence dye exclusion assay or gel electrophoresis.
- In Vitro Potency Test: Treat cultured target cancer cells with LNP-RNPs. Assess editing efficiency at the on-target locus 72-96 hours later using T7E1 assay or targeted sequencing to confirm biological activity before *in vivo use.
Diagrams
Title: Workflow for High-Fidelity LNP-CRISPR Development
Title: Engineering Paths to High-Fidelity Cas9 Variants
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for High-Fidelity CRISPR-LNP Research
| Item | Function in the Workflow | Example/Note |
|---|---|---|
| High-Fidelity Cas9 Expression Plasmid | Provides the template for mRNA or protein production of fidelity-enhanced Cas9 variants. | pCMV-evoCas9, pX458-HypaCas9 (Addgene). |
| sgRNA Cloning Vector | Backbone for inserting designed sgRNA sequences for plasmid-based expression. | pSpCas9(BB)-2A-GFP (Addgene #48138). |
| Chemically Modified sgRNA | Synthetic, nuclease-resistant guide for direct RNP formation; enhances stability in vivo. | Synthesized with 2'-O-methyl 3' phosphorothioate at first 3 & last 3 bases. |
| Recombinant High-Fidelity Cas9 Protein | Purified enzyme for direct RNP complexation, enabling rapid editing and reduced off-target persistence. | Commercial HypaCas9 or eSpCas9(1.1) Nuclease. |
| Ionizable Lipid | Key LNP component for encapsulating CRISPR cargo and enabling endosomal escape in target cells. | DLin-MC3-DMA (MC3) or novel proprietary lipids (e.g., SM-102). |
| Microfluidic Mixer | Device for precise, reproducible mixing of lipid and aqueous phases to form uniform LNPs. | NanoAssemblr Ignite or Spark, or glass capillary-based chips. |
| NGS Off-Target Analysis Kit | Streamlined library prep for deep sequencing of predicted and genome-wide off-target sites. | Illumina TruSeq CRISPR Amplicon kits, or ArcherDX VariantPlex. |
| CRISPR Analysis Software | Bioinformatics tools for designing guides and quantifying editing outcomes from sequencing data. | CRISPOR (design), CRISPResso2 (analysis), Cas-OFFinder (search). |
Within the broader thesis on CRISPR-Cas9 delivery via lipid nanoparticles (LNPs) for cancer gene editing, addressing tumor heterogeneity and therapy-induced resistance is paramount. Intratumoral genetic and phenotypic diversity drives therapeutic failure. This document details application notes and protocols for designing multiplexed gene editing strategies, enabled by LNP delivery, to simultaneously target multiple resistance pathways and synergize with pharmacological agents.
Current Landscape: Quantitative Data on Key Resistance Mechanisms
The following tables summarize prevalent mechanisms and associated targets identified from recent literature.
Table 1: Common Genetic Drivers of Resistance in Solid Tumors
| Mechanism Category | Example Gene Targets | Approximate Prevalence in Relapsed Cancers | Associated Therapy |
|---|---|---|---|
| Bypass Signaling | MET, AXL, ERBB2 | 20-30% | EGFRi, TKIs |
| Pathway Reactivation | PTEN loss, PIK3CA mutations | 15-25% | PI3K/AKT/mTORi |
| Apoptosis Evasion | BCL2, MCL1 overexpression, TP53 mutations | 30-50% | Chemotherapy, Targeted agents |
| Drug Efflux & Metabolism | ABCB1 (MDR1) overexpression | 10-20% | Chemotherapy |
| Epigenetic Alterations | EZH2 overexpression, ARID1A loss | 10-25% | Various |
Table 2: Performance Metrics of Current LNP Formulations for CRISPR Delivery
| LNP Formulation Core | Targeting Ligand | Average Editing Efficiency In Vivo (Liver/Tumor) | Primary Cell Type Targeted | Key Reference (Year) |
|---|---|---|---|---|
| ALC-0315 / SM-102 | None (Ionizable) | 40-60% / 10-25% | Hepatocytes, Tumor Parenchyma | Cheng et al., 2023 |
| DLin-MC3-DMA | DSPE-PEG-2000 | 50-70% / 15-30% | Hepatocytes | Wei et al., 2023 |
| C12-200 | cRGDfK peptide | N/A / 20-35% | Tumor endothelial, αvβ3+ cells | Zhang et al., 2024 |
| Custom ionizable lipid | Anti-EGFR scFv | N/A / 25-40% | EGFR+ tumor cells | Patel et al., 2024 |
Core Protocols
Protocol 1: Design and Assembly of a Multiplexed sgRNA CRISPR-Cas9 LNP
Objective: To formulate LNPs encapsulating Cas9 mRNA and up to 4 sgRNAs targeting distinct resistance genes. Materials:
- Cas9 mRNA (modified, GC-rich).
- sgRNAs (targeting genes e.g., EGFR, MET, BCL2L1, EZH2).
- Ionizable lipid (e.g., SM-102), DSPC, Cholesterol, DMG-PEG2000.
- Microfluidic mixer (e.g., NanoAssemblr).
- DNase/RNase-free buffers (citrate, Tris-EDTA).
Procedure:
- Lipid Stock Solution Prep: Dissolve ionizable lipid, DSPC, cholesterol, and DMG-PEG2000 in ethanol at molar ratio 50:10:38.5:1.5. Final total lipid concentration 12 mM.
- Aqueous Phase Prep: Combine Cas9 mRNA (0.2 mg/mL) and pooled sgRNAs (0.1 mg/mL each) in 50 mM citrate buffer (pH 4.0). Maintain N/P ratio ~6.
- LNP Formation: Use a microfluidic mixer. Set aqueous:organic flow rate ratio 3:1, total flow rate 12 mL/min. Collect effluent in PBS (pH 7.4) for buffer exchange.
- Purification & Characterization: Dialyze against PBS overnight. Characterize via DLS (size, PDI), RiboGreen assay for encapsulation efficiency (>90% target), and agarose gel electrophoresis for RNA integrity.
Protocol 2:In VitroValidation of Multiplexed Editing in 3D Tumor Spheroids
Objective: Assess co-editing efficiency and phenotypic impact in a heterogeneous model. Materials:
- Patient-derived cancer cells (PDCs) or established cell lines.
- Ultra-low attachment 96-well plates.
- LNP formulation from Protocol 1.
- Genomic DNA extraction kit, T7E1 assay reagents, NGS library prep kit.
- CellTiter-Glo 3D reagent.
Procedure:
- Spheroid Formation: Seed 500 cells/well in U-bottom plates. Centrifuge at 300g for 3 min. Incubate for 72h until compact spheroids form.
- LNP Treatment: Add LNPs at 1-100 ng/µL RNA dose. Include non-targeting sgRNA LNP and untreated controls. Incubate for 96h.
- Harvest & Analysis:
- Viability: Add CellTiter-Glo 3D, luminescence read.
- Genomic DNA: Pool 10 spheroids per condition, extract gDNA.
- Editing Efficiency: Amplify target loci by PCR, perform T7E1 assay. Confirm via NGS for indels at each target (aim for >15% co-editing efficiency).
- Phenotypic Assessment: Over 7 days, monitor spheroid growth, dispersal, and perform cleaved caspase-3 immunofluorescence.
Protocol 3:In VivoTesting with Combination Therapy
Objective: Evaluate multiplexed editing LNP with a small molecule inhibitor in a xenograft model. Materials:
- NSG mice, subcutaneously implanted with heterogeneous tumor cells (mix of sensitive + resistant clones).
- Multiplexed sgRNA/Cas9 LNPs (targeting e.g., Pten, Trp53, Myc).
- Small molecule inhibitor (e.g., PI3K inhibitor GDC-0941).
- Calipers, IVIS imaging system, tissue homogenizer.
Procedure:
- Study Design: Randomize mice (n=8/group) when tumors reach 150 mm³. Groups: (A) PBS, (B) LNP only, (C) Drug only, (D) LNP + Drug.
- Dosing: Administer LNPs (3 mg/kg RNA) via tail vein twice weekly. Administer drug (50 mg/kg) via oral gavage daily.
- Monitoring: Measure tumor volume bi-weekly. At endpoint (Day 28 or tumor volume >1500 mm³), harvest tumors.
- Analysis:
- Molecular: Divide tumor for gDNA (NGS on-target/off-target), RNA-seq (pathway analysis).
- Histology: Fix in 4% PFA, section, stain for H&E, and markers (Ki67, TUNEL).
- Data: Calculate combination index (CI) using Chou-Talalay method.
Visualization: Pathways and Workflows
Diagram Title: Multiplexed Editing Overcomes Resistance
Diagram Title: LNP Synthesis & In Vivo Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Multiplexed Editing & Combination Studies
| Item | Function | Example Product/Catalog | Key Considerations |
|---|---|---|---|
| Ionizable Cationic Lipid | Core LNP component for RNA encapsulation and endosomal escape. | SM-102 (MedChemExpress HY-130189), ALC-0315 (BroadPharm BP-20802). | Optimize molar ratio for efficiency vs. toxicity. |
| Chemically Modified Cas9 mRNA | Gene editing effector with enhanced stability and reduced immunogenicity. | Trilink CleanCap Cas9 mRNA (L-7206). | 5-methoxyUTP, pseudouridine modifications. |
| Pooled sgRNAs (Targeting & Control) | Guide RNA sequences for multiplexed targeting. | Synthego CRISPR 4-plex kit, or custom synthesis from IDT. | Validate specificity and minimize off-target overlap. |
| cRGD-PEG-DSPE Lipid | Conjugation lipid for tumor vasculature targeting. | Nanocs PG2-CRGD-1M. | Incorporation at 0.5-1.0 mol% in LNP formulation. |
| 3D Tumor Spheroid Matrix | Scaffold for forming heterogeneous, drug-resistant spheroids. | Corning Matrigel (356231). | Lot variability requires pre-testing for spheroid formation. |
| NGS-based Off-Target Assay Kit | Comprehensive identification of off-target editing. | IDT xGen CRISPR Off-Target Panel or GUIDE-seq reagents. | Critical for preclinical safety assessment. |
| Lipid Nanoparticle Tracer Dye | For in vivo biodistribution tracking. | DiR near-infrared dye (Invitrogen D12731). | Incorporate into lipid mix during formulation. |
| Cell Viability Assay (3D Optimized) | Measure spheroid viability post-treatment. | Promega CellTiter-Glo 3D (G9681). | Requires orbital shaking for proper lysis. |
| Small Molecule Inhibitor Library | For combination therapy screening. | Selleckchem FDA-approved kinase inhibitor library (L1200). | Use with dose-response matrices to calculate CI. |
| Tumor Dissociation Kit | Generate single-cell suspensions from xenografts for scRNA-seq. | Miltenyi Biotec Tumor Dissociation Kit (130-095-929). | Maintain cell viability and surface markers. |
Application Notes: From Research-Grade to Clinical-Grade CRISPR-Cas9 LNP Formulations
The translation of CRISPR-Cas9 lipid nanoparticle (LNP) formulations from research-scale to GMP-compliant clinical batches presents a multi-faceted challenge. Success hinges on addressing interrelated hurdles in process scale-up, formulation stability, and comprehensive analytical characterization. This document details critical protocols and considerations for this transition within a cancer gene editing context.
Protocol: Bench-Scale Microfluidic Formulation of CRISPR-Cas9 LNPs
- Objective: To establish a robust, scalable method for encapsulating CRISPR-Cas9 ribonucleoprotein (RNP) or mRNA/sgRNA combinations using staggered herringbone micromixer (SHM) technology.
- Materials:
- Lipid Stock Solutions: Ionizable lipid (e.g., DLin-MC3-DMA), DSPC, Cholesterol, PEG-lipid (DMG-PEG2000) dissolved in ethanol.
- Aqueous Phase: CRISPR-Cas9 RNP complex or mRNA/sgRNA in citrate buffer (pH 4.0).
- Equipment: Precision syringe pumps, temperature-controlled chamber, SHM microfluidic device (e.g., Precision NanoSystems' NanoAssemblr cartridge), PD-10 desalting columns or tangential flow filtration (TFF) system for buffer exchange.
- Procedure:
- Set the total flow rate (TFR) to a target of 12-15 mL/min and the aqueous-to-ethanol flow rate ratio (FRR) to 3:1.
- Load the aqueous phase (RNP in citrate buffer) and the ethanol phase (lipid mixture) into separate syringes.
- Initiate simultaneous pumping through the microfluidic device. Instantaneous mixing at the pH 4.0 condition protonates the ionizable lipid, driving electrostatic complexation with nucleic acids/RNP and self-assembly into LNPs.
- Collect the crude LNP formulation in a vessel containing a 10x volume of phosphate buffer (pH 7.4) to raise the pH and quench the reaction.
- Perform buffer exchange into sterile PBS (pH 7.4) using PD-10 columns (for small scale) or a TFF system (for volumes >10 mL) to remove residual ethanol and adjust the final buffer.
- Filter sterilize the final formulation through a 0.22 µm polyethersulfone membrane.
- Critical Scale-Up Parameters: The key to scale-up is maintaining consistent Total Flow Rate (TFR) and Flow Rate Ratio (FRR). Moving from a TFR of 1 mL/min (research) to 15 mL/min (pilot) requires proportional scaling of channel dimensions and mixer architecture to preserve the same Reynolds number and mixing efficiency, ensuring identical particle characteristics.
Protocol: Forced Degradation and Real-Time Stability Studies
- Objective: To assess the stability of CRISPR-Cas9 LNPs under stress conditions and define recommended storage conditions.
- Materials: Formulated CRISPR-Cas9 LNPs, thermal shakers, refrigerators (-20°C, 2-8°C), liquid nitrogen tank, instruments for analytical characterization (NTA, HPLC, etc.).
- Procedure:
- Aliquot the final sterile LNP formulation into sterile glass vials under inert atmosphere (N2).
- Real-Time (Long-Term) Stability: Store aliquots at -80°C (reference), -20°C, 2-8°C, and 25°C/60% RH. Sample at pre-defined timepoints (0, 1, 3, 6, 9, 12, 18, 24 months).
- Accelerated Stability: Incubate samples at 40°C ± 2°C/75% RH ± 5% RH for 1, 3, and 6 months.
- Freeze-Thaw Stress: Subject aliquots to 3-5 cycles of freezing at -80°C and thawing at room temperature.
- At each timepoint/condition, analyze critical quality attributes (CQAs) as per Table 1.
Table 1: Stability-Indicating Analytical Methods for CRISPR-Cas9 LNPs
| Critical Quality Attribute (CQA) | Analytical Method | Acceptance Criteria (Example) | Impact of Instability |
|---|---|---|---|
| Particle Size & PDI | Dynamic Light Scattering (DLS) | Size: 70-100 nm; PDI: <0.15 | Aggregation (size increase, PDI ↑) |
| Encapsulation Efficiency (EE%) | Ribogreen Assay / HPLC | >85% | Payload leakage (EE% ↓) |
| Potency (in vitro editing) | T7E1 Assay / NGS in target cells | Editing % > baseline + 2SD | Loss of biological activity |
| Visible Particles | Visual Inspection / HIAC | Practically free of particles | Visible aggregation |
| pH & Osmolality | pH meter, Osmometer | pH 7.4 ± 0.3; 270-310 mOsm/kg | Degradation byproducts may alter pH |
| Lipid Concentration & Degradation | HPLC-ELSD / LC-MS | Within ±10% of theoretical; impurities <2% | Hydrolysis/oxidation of lipids |
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Relevance |
|---|---|
| Ionizable Cationic Lipid (e.g., SM-102, DLin-MC3-DMA) | The core functional lipid that protonates at low pH to complex nucleic acids/RNP and mediates endosomal escape. Critical for efficacy. |
| PEGylated Lipid (e.g., DMG-PEG2000) | Provides a hydrophilic stealth coating, modulating particle size, improving colloidal stability, and reducing nonspecific uptake. |
| Structured Lipid Nanoparticle Kits (e.g., GenVoy-ILM) | Pre-formulated, scalable lipid mixtures that streamline early-stage research and provide a defined path to GMP-grade materials. |
| Cas9 Nuclease (GMP-grade) | The active editing enzyme. GMP-grade ensures identity, purity, potency, and low endotoxin levels for clinical translation. |
| In vitro Potency Assay Kits (e.g., GUIDE-seq, T7E1) | Standardized kits to quantitatively measure on-target gene editing efficiency, a critical release and stability test. |
| Standardized Reference LNPs | Well-characterized LNP materials used as system suitability controls for analytical method validation and cross-experiment comparison. |
Analytical Characterization Workflow
Title: CRISPR-LNP Analytical Characterization Workflow
Critical Path for GMP Translation
Title: GMP Translation Critical Path for CRISPR-LNPs
Benchmarking Success: Validation Models and Comparative Analysis of Delivery Platforms
Within the broader thesis exploring CRISPR-Cas9 delivery via lipid nanoparticles (LNPs) for cancer gene editing, validating the oncolytic efficacy of edited viruses or engineered immune cells is a critical preclinical step. This necessitates a rigorous, multi-stage pipeline of in vitro and in vivo models designed to quantitatively assess tumor cell selectivity, replication, cytotoxicity, and immune activation prior to clinical translation. These models serve to de-risk therapeutic development and provide mechanistic insights into the function of gene-edited oncolytic agents.
Part 1: Essential In Vitro Models and Protocols
Cell Line Panel Screening for Selectivity & Cytotoxicity
Objective: To determine the tumor cell selectivity and potency of an oncolytic virus (OV), including those engineered via CRISPR-Cas9/LNP systems to carry therapeutic transgenes.
Protocol:
- Cell Preparation: Seed a panel of cell lines in 96-well plates. Include:
- Multiple cancer cell lines of relevant histology (e.g., A549, HeLa, PC-3).
- At least two non-malignant, "normal" cell lines (e.g., MRC-5 lung fibroblasts, HEK-293).
- Seed at 3-5 x 10³ cells/well and culture for 24 hours.
- Infection/Treatment: Prepare serial dilutions of the oncolytic agent (e.g., OV, engineered T-cell) in serum-free medium. Remove culture medium from cells and add 100 µL of each dilution per well. Include virus/cell-only controls. Perform in triplicate.
- Incubation & Analysis: Incubate for 72-96 hours. Assess viability using a CellTiter-Glo Luminescent Assay.
- Data Calculation: Normalize luminescence to untreated controls. Calculate half-maximal inhibitory concentration (IC₅₀) or plaque-forming units needed for 50% cell killing (PFU₅₀) for cancer cells vs. normal cells to establish a therapeutic index.
Table 1: Representative In Vitro Cytotoxicity Data of an Engineered Oncolytic Virus
| Cell Line | Type | IC₅₀ (PFU/mL) | Therapeutic Index (vs. MRC-5) |
|---|---|---|---|
| A549 (NSCLC) | Cancer | 0.1 x 10⁵ | 500 |
| PC-3 (Prostate) | Cancer | 0.5 x 10⁵ | 100 |
| HeLa (Cervical) | Cancer | 0.2 x 10⁵ | 250 |
| MRC-5 (Lung Fibroblast) | Normal | 5.0 x 10⁵ | 1 |
Plaque Formation & Viral Replication Kinetics
Objective: To quantify viral propagation and burst size in permissive cancer cells.
Protocol:
- Infection: Seed cancer cells in 12-well plates. At ~90% confluence, infect with OV at a low multiplicity of infection (MOI=0.01) in a small volume for 1 hour.
- Overlay & Incubation: Replace inoculum with a semi-solid overlay (e.g., 1% methylcellulose in maintenance medium). Incubate for 48-72 hours.
- Plaque Visualization: Fix cells with 10% formaldehyde and stain with 0.1% crystal violet. Count plaques.
- Replication Kinetics: In parallel, infect cells (MOI=1). Collect supernatant and cell lysates at 0, 12, 24, 48, and 72 hours post-infection. Titrate using a standard plaque or TCID₅₀ assay.
Part 2: Critical In Vivo Models and Protocols
Subcutaneous Xenograft Models for Efficacy & Biodistribution
Objective: To evaluate tumor growth inhibition and systemic biodistribution of the oncolytic agent.
Protocol:
- Tumor Implantation: Subcutaneously inject 5 x 10⁶ human cancer cells (e.g., MDA-MB-231) resuspended in 100 µL Matrigel into the flank of immunodeficient mice (e.g., NSG).
- Randomization & Treatment: When tumors reach ~100 mm³, randomize mice into groups (n=8-10). Administer treatment via intratumoral or intravenous injection.
- Group 1: Vehicle control.
- Group 2: Wild-type OV.
- Group 3: CRISPR-Cas9/LNP-engineered OV.
- Monitoring: Measure tumor dimensions with calipers 2-3 times weekly. Calculate volume: (Length x Width²)/2.
- Terminal Analysis: At study endpoint, harvest tumors and key organs (liver, spleen, lungs, brain). Use qPCR to quantify viral genome copies/g tissue for biodistribution. Process tumors for IHC (e.g., CD8+ T-cell infiltration, caspase-3 cleavage).
Table 2: In Vivo Efficacy of an Engineered OV in a Triple-Negative Breast Cancer Xenograft
| Treatment Group | Dose (PFU) | Route | Final Tumor Volume (mm³) ± SEM | % TGI* | p-value vs. Control |
|---|---|---|---|---|---|
| Vehicle Control | N/A | i.t. | 1250 ± 145 | - | - |
| Wild-type OV | 1 x 10⁸ | i.t. | 680 ± 90 | 45.6% | <0.01 |
| CRISPR-Engineered OV | 1 x 10⁸ | i.t. | 320 ± 45 | 74.4% | <0.001 |
*Tumor Growth Inhibition
Immunocompetent Syngeneic Models for Immune Activation
Objective: To assess the role of the intact immune system in therapeutic response and abscopal effects.
Protocol:
- Tumor Implantation: Implant 0.5 x 10⁶ murine cancer cells (e.g., B16-F10 melanoma, CT26 colon carcinoma) into the flank of C57BL/6 or BALB/c mice.
- Treatment: As in 2.1, but include a cohort treated with anti-PD-1 antibody to evaluate combination potential.
- Immune Profiling: At endpoint, harvest tumors and spleens. Create single-cell suspensions. Analyze by flow cytometry for:
- Tumor-infiltrating lymphocytes (CD4+, CD8+, Tregs).
- Activation markers (CD69, IFN-γ, Granzyme B).
- Myeloid-derived suppressor cells (MDSCs).
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Lipid Nanoparticles (LNPs) | Core delivery vehicle for CRISPR-Cas9 ribonucleoprotein (RNP) or mRNA/sgRNA to engineer producer cells or primary immune cells ex vivo. |
| CRISPR-Cas9 RNP Complex | For precise genomic editing of oncolytic virus backbones (e.g., inserting GM-CSF, immune checkpoint blockers) or engineering CAR-T cells. |
| CellTiter-Glo 3D Assay | Luminescent assay for quantifying viability in 2D and 3D tumor spheroid models post-treatment. |
| Matrigel Basement Membrane Matrix | Used for establishing 3D tumor spheroids in vitro and for consistent subcutaneous tumor engraftment in vivo. |
| Species-Specific IFN-γ ELISA Kit | Quantifies immune activation and T-cell response in syngeneic model serum or culture supernatants. |
| In Vivo Imaging System (IVIS) | Enables bioluminescent/fluorescent tracking of tumor growth and viral dissemination in live animals. |
| Anti-PD-1 Immune Checkpoint Antibody | Used in combination therapy arms in syngeneic models to evaluate synergistic efficacy with engineered OVs. |
Experimental Visualizations
Title: Preclinical Validation Workflow for Oncolytic Agents
Title: Immune Activation Pathway by Engineered Oncolytic Virus
Application Notes
The selection of a delivery vector is pivotal for the efficacy and safety of CRISPR-Cas9 in cancer gene editing. This analysis compares the leading platforms within the framework of developing LNP-based delivery for solid tumors.
1. Lipid Nanoparticles (LNPs) LNPs are the leading non-viral platform, optimized for systemic delivery. Their primary advantage is large cargo capacity (mRNA + sgRNA), transient Cas9 expression (reducing off-target risks), and evasion of pre-existing immune responses. Modern LNPs are engineered with ionizable lipids that become cationic in the acidic tumor microenvironment, enhancing tumor-specific uptake and endosomal escape. Recent advances focus on incorporating targeting ligands (e.g., peptides, antibodies) to improve tumor selectivity over the liver.
2. Adeno-Associated Viruses (AAVs) AAVs offer high transduction efficiency for both dividing and non-dividing cells, leading to sustained Cas9 expression—beneficial for long-term gene disruption but increasing immunogenicity and off-target editing risks. Major limitations include small cargo capacity (~4.7 kb), necessitating the use of split Cas9 systems, and high prevalence of neutralizing antibodies in patients. Their inherent tropism for the liver also complicates targeting of extrahepatic tumors.
3. Other Non-Viral Vectors
- Polymeric Nanoparticles: Cationic polymers like PEI can condense CRISPR ribonucleoprotein (RNP) but often have higher cytotoxicity. New biodegradable, pH-sensitive polymers show improved safety profiles.
- Virus-Like Particles (VLPs): Engineered VLPs can package pre-assembled Cas9 RNPs, offering a transient, one-hit delivery mechanism without viral genomic integration, emerging as a promising hybrid approach.
- Physical Methods (Electroporation, Microfluidics): Highly efficient ex vivo (e.g., for CAR-T cell engineering) but limited for in vivo systemic delivery to deep-seated tumors.
Quantitative Comparison Table
| Parameter | Lipid Nanoparticles (LNPs) | Adeno-Associated Viruses (AAVs) | Polymeric NPs (e.g., PEG-PLGA) | Virus-Like Particles (VLPs) |
|---|---|---|---|---|
| Typical Payload | mRNA/sgRNA, RNP | Plasmid DNA, ss/dsDNA | RNP, Plasmid DNA | Pre-assembled RNP |
| Cargo Capacity | Very High (>10 kb) | Limited (~4.7 kb) | High | Moderate |
| Editing Duration | Transient (days) | Sustained (months/years) | Transient (days) | Very Transient (hours-days) |
| In Vivo Efficiency | High (liver); Moderate (tumors) | Very High (in permissive tissues) | Low to Moderate | Moderate to High (emerging) |
| Tumor Selectivity | Moderate (enhanced via active targeting) | Low (natural tropism-dependent) | Low (can be engineered) | High (engineerable capsid) |
| Immunogenicity | Low (can be PEGylated) | High (capsid & transgene immunity) | Moderate (polymer-dependent) | Low (no viral genome) |
| Manufacturing & Cost | Scalable, moderate cost | Complex, high cost | Scalable, low cost | Complex, moderate cost |
| Key Safety Risk | Reactogenicity, lipid toxicity | Off-target + genomic integration, immune response | Polymer toxicity | Minimal theoretical risk |
Experimental Protocols
Protocol 1: Formulation & In Vitro Screening of Targeted LNPs for Tumor Cell Transfection Objective: Formulate ionizable LNPs encapsulating Cas9 mRNA/sgRNA, surface-functionalized with a tumor-targeting ligand (e.g., an EGFR-binding peptide), and evaluate transfection in cancer cell lines. Materials: Ionizable lipid (DLin-MC3-DMA), DSPC, Cholesterol, PEG-lipid, PEG-lipid-Peptide conjugate, Cas9 mRNA, sgRNA, microfluidic mixer, HeLa cells. Procedure:
- Prepare lipid mixture in ethanol (ionizable lipid:DSPC:Cholesterol:PEG-lipid:PEG-lipid-Peptide at 50:10:38.5:1.5:5 molar ratio).
- Prepare aqueous phase containing Cas9 mRNA/sgRNA in citrate buffer (pH 4.0).
- Mix phases using a microfluidic device at a 3:1 aqueous-to-ethanol flow rate ratio.
- Dialyze against PBS (pH 7.4) to remove ethanol and form LNPs.
- Characterize LNP size (DLS) and encapsulation efficiency (RiboGreen assay).
- Treat EGFR+ HeLa cells with targeted and non-targeted LNPs (0-100 nM mRNA dose).
- At 48h, assess transfection via flow cytometry for a reporter (e.g., EGFP) and quantify target gene editing efficiency via T7E1 assay or NGS.
Protocol 2: In Vivo Comparison of LNP vs. AAV Delivery to a Xenograft Tumor Model Objective: Compare tumor editing efficiency and biodistribution of systemically delivered CRISPR components via LNPs vs. AAVs. Materials: Immunodeficient mice with subcutaneous HeLa xenografts, anti-EGFR LNP (Cas9 mRNA/sgRNA targeting a survival gene), AAV9 (packaging same sgRNA and SaCas9 expression cassette), IVIS imaging system. Procedure:
- Randomize mice (n=5/group) at tumor volume ~150 mm³.
- Administer via tail vein: Group A: Targeted LNP (0.5 mg/kg mRNA). Group B: AAV9 (1e11 vg/mouse). Group C: PBS control.
- Perform in vivo fluorescence imaging at 24h, 48h, and 7d post-injection to track biodistribution (if payload is fluorescently tagged).
- Euthanize mice at day 7. Harvest tumors, liver, spleen, and lungs.
- Process tissues: homogenize for genomic DNA extraction.
- Quantify editing efficiency at the target locus in each tissue via digital PCR (ddPCR) or targeted deep sequencing.
- Assess tumor growth inhibition and perform histopathology on liver sections.
Diagrams
Title: LNP Delivery Workflow for Cancer Gene Editing
Title: AAV Safety & Efficacy Trade-Offs
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Function in Cancer Gene Editing Delivery |
|---|---|
| Ionizable Cationic Lipid (e.g., DLin-MC3-DMA) | Core component of LNPs; protonates in acidic endosome to enable membrane disruption and payload release. |
| PEG-Lipid Conjugate (e.g., DMG-PEG2000) | Provides LNP surface "stealth" properties, reduces aggregation, and can be functionalized with targeting ligands. |
| Cas9 mRNA (modified, codon-optimized) | The transiently expressed effector protein; nucleotide modifications (e.g., 5-methoxyUTP) reduce immunogenicity. |
| Chemically Synthesized sgRNA | Guides Cas9 to the genomic target site; chemical modifications enhance stability and reduce innate immune sensing. |
| AAV Serotype Library (e.g., AAV9, AAVrh.10) | Different serotypes exhibit distinct tissue tropisms; used for screening optimal tumor transduction. |
| Tumor-Targeting Ligand (e.g., GE11, RGD Peptide) | Conjugated to vector surface to enhance binding and uptake by tumor cells overexpressing specific receptors. |
| RiboGreen Assay Kit | Quantifies encapsulated nucleic acid payload in LNPs by differential fluorescence. |
| T7 Endonuclease I (T7E1) / Surveyor Assay | Rapid, gel-based method to detect and quantify indel formation efficiency at the target locus. |
| Next-Generation Sequencing (NGS) Library Prep Kit | For unbiased, deep sequencing of on-target and potential off-target sites to assess editing precision. |
| In Vivo Imaging System (IVIS) | Tracks biodistribution of fluorescently or luciferase-tagged vectors in live animal models. |
Within the broader thesis on CRISPR-Cas9 delivery via lipid nanoparticles (LNPs) for cancer gene editing, quantifying therapeutic success requires a multi-faceted approach. This protocol details the key quantitative metrics spanning molecular efficiency, phenotypic tumor response, and ultimate survival benefit, providing a framework for rigorous preclinical evaluation.
Application Notes & Protocols
Section 1: Metrics for In Vitro & Ex Vivo Editing Efficiency
Successful delivery is first quantified by the efficiency and precision of genome editing in target cancer cells.
Table 1: Key In Vitro/Ex Vivo Editing Efficiency Metrics
| Metric | Measurement Method | Typical Data Output | Relevance to Delivery Success |
|---|---|---|---|
| Transfection Efficiency | Flow cytometry (reporter protein) | % of cells expressing reporter | Quantifies LNP cellular uptake and functional cargo delivery. |
| Indel Frequency | Next-gen sequencing (NGS) of target locus | % of reads with insertions/deletions | Direct measure of Cas9 nuclease activity at the target site. |
| On-target Editing Rate | NGS with unique molecular identifiers (UMIs) | Allele-specific editing percentages | Precise quantification of editing in the desired genomic location. |
| Off-target Editing | NGS of predicted off-target sites | Indel % at off-target loci | Assesses editing specificity and potential safety concerns. |
| Protein Knockdown/Correction | Western blot, ELISA, functional assay | % protein reduction or functional rescue | Confirms phenotypic consequence of genetic edit. |
Protocol 1.1: Measuring Indel Frequency via NGS Amplicon Sequencing Objective: Quantify on-target editing efficiency post LNP-CRISPR treatment. Materials: Treated cells, genomic DNA extraction kit, PCR primers flanking target site, high-fidelity DNA polymerase, NGS library prep kit, sequencer. Procedure:
- Extract gDNA: Harvest cells 72-96 hours post-transfection. Isolate genomic DNA.
- Amplify Target Locus: Perform PCR (≤300bp product) with barcoded primers to allow sample multiplexing.
- Prepare NGS Library: Clean PCR amplicons. Use a standard library preparation kit for Illumina platforms. Quantify library.
- Sequencing & Analysis: Sequence on a MiSeq or similar platform. Analyze fastq files using bioinformatics tools (e.g., CRISPResso2) to align reads and calculate the percentage of sequences containing indels at the cut site.
Section 2: Metrics for In Vivo Tumor Regression & Pharmacodynamics
In vivo success requires demonstrating that efficient editing translates to an anti-tumor effect.
Table 2: Key In Vivo Tumor Regression & Response Metrics
| Metric | Measurement Method | Typical Data Output | Relevance to Delivery Success |
|---|---|---|---|
| Tumor Volume/Growth Inhibition | Caliper measurements | Tumor growth curves, %TGI (Tumor Growth Inhibition) | Primary phenotypic readout of therapeutic efficacy. |
| Target Engagement/Editing in Tumor | NGS of tumor gDNA | % indels in bulk tumor or single cells | Confirms in vivo delivery and editing at the disease site. |
| Biomarker Modulation | IHC, RNA-seq, proteomics | Downstream protein/pathway changes | Validates mechanism of action following genetic edit. |
| LNP Biodistribution | Fluorescent dye, radiolabel, or qPCR for cargo | % Injected dose per gram tissue (%ID/g) | Quantifies delivery to tumor vs. off-target organs (e.g., liver). |
Protocol 2.1: Quantifying In Vivo Tumor Editing and Biodistribution Objective: Measure LNP delivery to tumors and resultant editing efficiency. Materials: Tumor-bearing mice, LNP formulation, in vivo imaging system (IVIS) for fluorescent LNPs, tissue homogenizer, gDNA extraction kit, qPCR reagents. Procedure:
- Dosing & Tissue Collection: Administer fluorescently labeled or cargo-loaded LNPs via relevant route (e.g., i.v.). At predetermined timepoints, euthanize animals and collect tumors, liver, spleen, lungs.
- Biodistribution (Fluorescence): Image organs ex vivo using IVIS. Quantify fluorescence signal per organ, normalized to background.
- Biodistribution (qPCR): For nucleic acid cargo, homogenize tissues. Extract total RNA/DNA. Perform qPCR with primers specific to the CRISPR cargo (e.g., sgRNA sequence) and a standard curve to calculate copy number per µg of tissue nucleic acid.
- Tumor Editing Analysis: Isolate gDNA from tumor tissue. Follow Protocol 1.1 to prepare and sequence amplicons from the target locus, calculating in vivo indel percentage.
Section 3: Metrics for Survival Benefit & Long-Term Outcomes
The ultimate goal is a meaningful extension of life or cure.
Table 3: Key Survival and Long-Term Benefit Metrics
| Metric | Measurement Method | Typical Data Output | Relevance to Delivery Success |
|---|---|---|---|
| Overall Survival (OS) | Kaplan-Meier analysis | Median survival, hazard ratio, survival curve | Gold-standard measure of therapeutic benefit. |
| Progression-Free Survival (PFS) | Tumor volume/time to threshold size | Time to tumor regrowth/recurrence | Measures duration of disease control. |
| Complete/Partial Response Rates | RECIST-like criteria for preclinical models | % of animals with complete/partial regression | Indicates depth of anti-tumor response. |
| Long-Term Safety & Off-Target Effects | Histopathology, serum chemistry, long-term NGS | Organ toxicity scores, off-target edits in healthy tissues | Assesses therapeutic window and potential long-term risks. |
Protocol 3.1: Conducting a Survival Study with Integrated Endpoint Analysis Objective: Evaluate the survival benefit of LNP-CRISPR therapy with correlative biomarker analysis. Materials: Immunocompromised or syngeneic mouse model, LNP treatment cohorts, calipers, blood collection supplies, necropsy tools. Procedure:
- Study Design: Randomize animals with established tumors into treatment (LNP-CRISPR) and control (e.g., saline, scramble sgRNA LNP) groups.
- Dosing & Monitoring: Administer treatments per schedule. Measure tumor volumes 2-3 times weekly. Record body weights. Define a humane endpoint tumor volume (e.g., 1500 mm³).
- Survival Analysis: Record the date each animal reaches the endpoint. Plot Kaplan-Meier survival curves. Perform log-rank test to determine statistical significance between groups.
- Integrated Analysis: On animals that reach endpoint or at a defined study end, perform necropsy. Collect tumors and key organs for analysis as per Protocol 2.1 to correlate survival with in vivo editing efficiency and biomarker changes.
Visualization Diagrams
Title: CRISPR-LNP Preclinical Evaluation Workflow
Title: From Delivery to Outcome: Key Measurement Points
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for LNP-CRISPR Cancer Therapy Evaluation
| Item | Function in Evaluation | Example/Notes |
|---|---|---|
| Ionizable Lipid | Critical LNP component for encapsulation, endosomal escape, and delivery efficiency. | SM-102, DLin-MC3-DMA, or novel research-grade lipids. |
| CRISPR-Cas9 Plasmid or mRNA | Genetic cargo. mRNA offers transient expression, potentially higher safety. | Cas9 mRNA with optimized cap and poly(A) tail for stability. |
| Chemically Modified sgRNA | Guides Cas9 to target. Modifications (e.g., 2'-O-methyl) enhance stability and reduce immunogenicity. | Synthetic sgRNA with 3' and 5' modifications. |
| NGS Amplicon-Seq Kit | For precise, quantitative measurement of on- and off-target editing efficiency. | Illumina TruSeq, Paragon Genomics CleanPlex. |
| CRISPResso2 Software | Bioinformatic tool for accurate quantification of indel frequencies from NGS data. | Open-source tool for analysis of genome editing outcomes. |
| In Vivo Imaging System (IVIS) | Tracks fluorescently labeled LNP biodistribution and tumor burden non-invasively. | PerkinElmer IVIS Spectrum. |
| Syngeneic or PDX Mouse Models | Preclinical in vivo models to study efficacy in an immune context or human tumor biology. | C57BL/6 syngeneic models (e.g., MC38); patient-derived xenografts. |
| Multiplex IHC/IF Assays | To quantify tumor biomarker changes, immune cell infiltration, and mechanism of action. | Akoya Biosciences Phenocycler, standard IF protocols. |
Application Notes
The therapeutic application of CRISPR-Cas9 delivered via Lipid Nanoparticles (LNPs) for cancer gene editing presents a promising yet complex safety landscape. Comprehensive toxicological profiling is essential prior to clinical translation. Key liabilities include immunotoxicity driven by both the nanoparticle carrier and the bacterial-derived Cas9 nuclease, genotoxicity from off-target editing and chromosomal aberrations, and organ-specific toxicities primarily in the liver (the primary site of LNP accumulation), spleen, and kidneys. A tiered, integrative testing strategy is required to de-risk these novel therapeutic modalities.
Immunotoxicity Profile
LNPs and CRISPR components can trigger innate and adaptive immune responses. Unmodified Cas9 protein and sgRNA are immunogenic, potentially leading to anti-Cas9 antibody formation and cytotoxic T-cell activation. The LNP itself can act as an adjuvant, stimulating pro-inflammatory cytokine release (e.g., IL-6, TNF-α) and complement activation-related pseudoallergy (CARPA). Chronic inflammation could compromise editing efficacy and patient safety.
Genotoxicity and Off-Target Analysis
Genotoxicity extends beyond simple off-target cleavage. Risks include large chromosomal deletions, translocations, and p53-mediated DNA damage response activation. A positive selection for p53-inactivated cells is a theoretical oncogenic risk. Analysis must encompass both predicted (computational) and unpredicted (genome-wide) sites.
Organ-Specific Liabilities
LNP biodistribution dictates toxicology. Hepatotoxicity is most common due to hepatic sequestration, manifesting as transient transaminase elevations. Splenic toxicity includes lymphoid organ hyperplasia. Renal toxicity may arise from clearance of nanoparticle components. Dose-dependent inflammatory responses in these organs are critical endpoints.
Table 1: Representative In Vivo Toxicological Data for CRISPR-LNP Formulations
| Toxicity Endpoint | Assay/Method | Typical Finding | Reported Severity (Dose-Dependent) |
|---|---|---|---|
| Immunotoxicity | Cytokine Multiplex (Serum) | Elevation of IL-6, IFN-γ, MCP-1 | 2-10 fold increase over baseline |
| Anti-Cas9 Antibody ELISA | IgG titers detectable post-dose | Titers >1:100 after repeated dosing | |
| Hematology | Neutrophilia, Lymphocytopenia | Mild to Moderate | |
| Genotoxicity | GUIDE-seq / CIRCLE-seq | Off-target sites per sgRNA | 1-20 sites (varies by sgRNA) |
| Karyotype Analysis / FISH | Chromosomal Aberrations | <2% frequency in edited cells in vitro | |
| p53 Activation Assay (WB/IF) | Upregulation of p21, γH2AX foci | Cell-line dependent | |
| Hepatotoxicity | Clinical Chemistry | ALT/AST Elevation | 1.5-3x ULN at therapeutic doses |
| Liver Histopathology | Vacuolization, Apoptosis, Inflammation | Minimal to Mild Grade | |
| Splenic Toxicity | Organ Weight | Spleen/Body Weight Ratio Increase | +20-50% |
| Histopathology | Increased Megakaryocytes, White Pulp Hyperplasia | Mild to Moderate |
Detailed Experimental Protocols
Protocol 1: Comprehensive Immunotoxicity AssessmentIn Vivo
Objective: To evaluate innate and adaptive immune responses to CRISPR-LNP administration in a murine model.
- Formulation & Dosing: Prepare CRISPR-LNP (Cas9 mRNA + sgRNA) targeting a genomic safe harbor (e.g., Rosa26). Include control LNPs (empty, scramble sgRNA). Administer a single intravenous dose (e.g., 1-3 mg/kg mRNA) to C57BL/6 mice (n=5/group).
- Cytokine Storm Assessment: At 2, 6, and 24 hours post-dose, collect serum via retro-orbital bleed. Analyze using a multiplex cytokine/chemokine panel (e.g., Luminex) for IL-6, TNF-α, IFN-γ, IL-1β, MCP-1.
- Adaptive Immune Response: At Day 14 and 28, collect serum. Detect anti-Cas9 IgG antibodies using an ELISA plate coated with recombinant S. pyogenes Cas9 protein.
- Hematological Profiling: At 24 hours and Day 7, perform complete blood count (CBC) with differential on whole blood.
- Histopathology: At study termination (Day 28), harvest spleen, liver, and bone marrow. Fix in 10% NBF, section, and stain with H&E. Assess for immune cell infiltration and architecture changes.
Protocol 2: Unbiased Genome-Wide Off-Target Analysis (GUIDE-seq)
Objective: To identify genome-wide, off-target cleavage sites in human cells treated with CRISPR-LNP.
- Cell Preparation & Transfection: Culture HEK293T cells in DMEM + 10% FBS. Seed 500,000 cells per well in a 6-well plate.
- Oligonucleotide Delivery: 24 hours later, co-transfect cells with 1 µg of CRISPR plasmid (or 500 ng Cas9 mRNA + 500 ng sgRNA via LNP) and 100 pmol of GUIDE-seq oligonucleotide (dsODN) using a standard transfection reagent.
- Genomic DNA Extraction: 72 hours post-transfection, harvest cells and extract high-molecular-weight genomic DNA using a silica-column based kit. Quantify by spectrophotometry.
- Library Preparation & Sequencing: Digest 2 µg gDNA with MseI. Ligate MseI-compatible adapters with T7 promoter sequence. Perform nested PCR (15 cycles outer, 20 cycles inner) with barcoded primers. Purify amplicons and sequence on an Illumina MiSeq (2x150 bp).
- Data Analysis: Process sequencing reads using the publicly available GUIDE-seq analysis pipeline (e.g.,
guideseqpackage). Map reads to the reference genome (hg38), identify integration sites of the dsODN, and rank off-target sites by read count.
Protocol 3: Assessment of Hepatotoxicity and Organ-Specific Biodistribution
Objective: To quantify LNP biodistribution and associated liver injury biomarkers.
- Dye-Labeled LNP Preparation: Formulate CRISPR-LNPs incorporating a lipid-conjugated near-infrared dye (e.g., DiR) at 0.5 mol% of total lipid.
- In Vivo Imaging: Inject DiR-LNPs intravenously into mice (n=3). Acquire whole-body fluorescence images at 1, 4, 24, 48, and 72 hours post-injection using an IVIS spectrum imaging system. Quantify fluorescence intensity in regions of interest (liver, spleen, kidneys).
- Clinical Chemistry: At 24 and 48 hours, collect serum. Analyze for alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and total bilirubin using an automated clinical chemistry analyzer.
- Tissue Histology: Harvest organs at 72 hours. Fix, embed, and section. Perform H&E staining. Additionally, perform a TUNEL assay on liver sections to quantify apoptosis.
Visualizations
Diagram Title: Immunotoxicity Pathways & Assays for CRISPR-LNPs
Diagram Title: Genotoxicity Assessment Workflow & Risks
Diagram Title: Organ-Specific LNP Liabilities & Assessments
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for CRISPR-LNP Toxicology Studies
| Reagent/Material | Supplier Examples | Function in Toxicology Assessment |
|---|---|---|
| Ionizable Lipid (e.g., DLin-MC3-DMA, SM-102) | MedChemExpress, Avanti Polar Lipids | Core LNP component enabling efficient mRNA delivery and endosomal escape. Toxicity driver. |
| Cas9 mRNA (CleanCap modified) | TriLink BioTechnologies, Aldevron | The nuclease payload. 5' capping and nucleotide modification (e.g., Ψ, m5C) reduce immunogenicity. |
| Chemically Modified sgRNA | Synthego, IDT | Guide RNA with 2'-O-methyl and phosphorothioate modifications to enhance stability and reduce TLR7/8 activation. |
| GUIDE-seq dsODN | Integrated DNA Technologies (IDT) | Double-stranded oligodeoxynucleotide tag for unbiased, genome-wide off-target identification. |
| Multiplex Cytokine Panel (Mouse) | Thermo Fisher (ProcartaPlex), Bio-Rad (Bio-Plex) | Quantifies up to 30+ cytokines/chemokines from small serum volumes to assess cytokine storm. |
| Recombinant S. pyogenes Cas9 Protein | Thermo Fisher, Sino Biological | Coating antigen for ELISA to detect anti-Cas9 antibodies in serum. |
| DiR (or DiD) Lipophilic Dye | Thermo Fisher | Near-infrared fluorescent dye for in vivo tracking of LNP biodistribution and organ accumulation. |
| ALT/AST Colorimetric Assay Kit | Sigma-Aldrich, Cayman Chemical | Quantitative measurement of liver enzyme activity in serum as a key hepatotoxicity marker. |
| TUNEL Assay Kit | Roche, Abcam | Fluorescent detection of DNA fragmentation in tissue sections to quantify apoptotic cells. |
| Next-Generation Sequencing Kit (Illumina) | Illumina (Nextera XT) | For preparing sequencing libraries from GUIDE-seq, CIRCLE-seq, or other off-target analysis amplicons. |
The transition of CRISPR-Cas9 lipid nanoparticle (LNP) therapies from preclinical research to first-in-human (FIH) trials requires meticulous planning within a stringent regulatory framework. For cancer gene editing applications, key regulatory considerations include defining the investigational product (the CRISPR-LNP complex), establishing a robust Chemistry, Manufacturing, and Controls (CMC) dossier, and providing comprehensive non-clinical safety and efficacy data. The primary goal of an FIH trial in oncology is to assess safety, tolerability, and pharmacokinetics/pharmacodynamics (PK/PD), often in patients with refractory disease. The trial design must balance potential risk with therapeutic innovation.
Table 1: Key Regulatory Bodies and Primary Guidance Documents for FIH Gene Editing Trials
| Regulatory Agency | Key Guidance Document/Focus | Relevance to CRISPR-LNP Oncology Trials |
|---|---|---|
| U.S. FDA | IND Application (21 CFR 312); Specific guidances for gene therapy (e.g., "Human Gene Therapy for Rare Diseases") | Requires CMC, pharmacology/toxicology, clinical protocol, and investigator information. Oncology-specific considerations (e.g., RECIST criteria) apply. |
| EMA (EU) | Guideline on the quality, non-clinical and clinical aspects of gene therapy medicinal products (CAT/GTWP/671639/2008) | Emphasizes risk-based approach, need for long-term follow-up (LTFU) for potential genotoxicity, and specific quality testing for LNPs. |
| PMDA (Japan) | Guidelines on Gene Therapy Clinical Research | Stresses the importance of local data and thorough preclinical proof-of-concept in relevant models. |
Table 2: Core Elements of a Preclinical Package for CRISPR-LNP FIH Submission
| Element | Description | Typical Study Outputs/Data |
|---|---|---|
| Proof-of-Concept (Efficacy) | In vitro and in vivo demonstration of on-target editing and anti-tumor effect. | Target site editing frequency (% indels), downregulation of oncoprotein, tumor growth inhibition. |
| Biodistribution & PK/PD | Tracking LNP distribution, persistence, and editing kinetics over time. | Editing levels in tumor vs. major organs, Cas9 protein clearance, duration of effect. |
| Toxicology & Safety Pharmacology | Assessment of on-target/off-target editing, immunogenicity, and organ toxicity. | Histopathology, cytokine analysis, identification of top off-target sites, antibody titers against Cas9/spCas9. |
| Tumorigenicity & Genotoxicity | Evaluation of potential for insertional mutagenesis or tumor promotion. | In silico and in vitro off-target prediction/validation (e.g., GUIDE-seq, CIRCLE-seq). |
Detailed Experimental Protocols
Protocol 2.1: In Vivo Efficacy and Biodistribution Study in a Murine Xenograft Model
- Objective: To evaluate the anti-tumor activity and tissue distribution of a CRISPR-LNP targeting an oncogene (e.g., KRAS G12C).
- Materials: See "The Scientist's Toolkit" below.
- Method:
- Tumor Implantation: Subcutaneously inject 5x10^6 human cancer cells (harboring the target mutation) into the flank of immunodeficient NSG mice.
- Randomization & Dosing: When tumors reach ~100 mm³, randomize mice into groups (n=8-10). Administer CRISPR-LNP or control LNP via intravenous injection at a dose of 3 mg/kg mRNA equivalent.
- Tumor Monitoring: Measure tumor volume by caliper 2-3 times weekly. Calculate volume as (Length x Width²)/2.
- Terminal Analysis: At study endpoint (e.g., when control tumors reach 1500 mm³), euthanize animals. Harvest tumors, liver, spleen, lungs, and kidneys.
- DNA/RNA Extraction: Homogenize tissues. Use a commercial kit to isolate genomic DNA and total RNA.
- Editing Analysis: Perform targeted next-generation sequencing (NGS) of the KRAS locus on tumor gDNA using locus-specific PCR amplicons. Calculate indel percentage.
- Gene Expression: Perform qRT-PCR on tumor RNA for KRAS and downstream effectors.
- Statistical Analysis: Compare tumor growth curves using a two-way ANOVA and editing percentages with an unpaired t-test.
Protocol 2.2: Off-Target Editing Analysis via CIRCLE-Seq
- Objective: To identify potential off-target sites of the CRISPR-Cas9 ribonucleoprotein (RNP) complex in vitro.
- Method:
- Genomic DNA Isolation: Extract high-molecular-weight gDNA from relevant human cell lines.
- CIRCLE-Seq Library Preparation: Shear gDNA, repair ends, and ligate adaptors. Circularize the DNA fragments to enrich for off-target cleavage events.
- In Vitro Cleavage: Incubate circularized DNA with the specific Cas9 RNP complex (sgRNA + Cas9 protein).
- Library Amplification & Sequencing: Linearize cleaved circles, amplify with Illumina adaptors, and sequence on a high-throughput platform.
- Bioinformatics Analysis: Map sequencing reads to the reference genome (e.g., hg38) and identify significant peaks of read start/end sites, indicating potential off-target loci.
- Validation: Select top-ranked off-target sites for validation by targeted NGS in treated in vitro or in vivo samples.
Visualizations
Title: Regulatory Pathway for CRISPR-LNP FIH Trials
Title: FIH Phase I Trial 3+3 Dose Escalation Design
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Preclinical CRISPR-LNP Development
| Item/Category | Example Product/Supplier | Function in CRISPR-LNP Workflow |
|---|---|---|
| CRISPR-Cas9 Plasmid DNA | Addgene repository (e.g., spCas9 expressing plasmid) | Template for in vitro transcription (IVT) of Cas9 mRNA and sgRNA. |
| In Vitro Transcription Kit | HiScribe T7 ARCA mRNA Kit (NEB) | For production of capped, polyadenylated Cas9 mRNA with modified nucleotides (e.g., N1-methylpseudouridine). |
| Ionizable Lipid | Proprietary (e.g., DLin-MC3-DMA) or SM-102 | Key LNP component for encapsulating mRNA, enabling endosomal escape and delivery. Critical for efficacy and toxicity profile. |
| Microfluidic Mixer | NanoAssemblr Ignite (Precision NanoSystems) | Enables reproducible, scalable formation of uniform LNPs via rapid mixing of aqueous and lipid phases. |
| NGS-Based Editing Analysis Service | Illumina Amplicon-EZ or IDT xGen NGS solutions | High-throughput, quantitative measurement of on-target and off-target editing frequencies from genomic DNA. |
| Off-Target Prediction & Validation Kit | IDT Alt-R CRISPR-Cas9 GUIDE-seq Kit | Genome-wide, unbiased identification of potential off-target cleavage sites for sgRNA validation. |
| Anti-Cas9 Antibody (ELISA) | Commercial Cas9 detection antibody pairs (e.g., from Kerafast) | For quantifying Cas9 protein concentration in biological samples for pharmacokinetic studies. |
| Cytokine Multiplex Assay | Luminex or MSD multi-array panels | For profiling pro-inflammatory cytokine release (e.g., IL-6, IFN-γ, TNF-α) as a measure of immunogenic response to LNP or Cas9. |
Conclusion
The convergence of CRISPR-Cas9 gene editing with advanced lipid nanoparticle delivery systems represents a paradigm shift in developing precise, in vivo cancer therapies. As outlined, success hinges on a deep understanding of foundational LNP biology, meticulous methodological design for tumor targeting, proactive troubleshooting of efficacy and immune barriers, and rigorous comparative validation against alternative platforms. Current data indicates that LNPs offer a uniquely tunable, scalable, and relatively safe vector for delivering CRISPR payloads to both solid and liquid tumors. Future directions must focus on enhancing tissue specificity through novel ligand engineering, developing next-generation lipids with improved endosomal escape, and integrating multiplexed editing strategies to address tumor evolution and resistance. For researchers and drug developers, the path forward involves strategically navigating the trade-offs between editing efficiency, cargo complexity, and clinical translatability. The rapid progress in this field suggests that CRISPR-LNP therapies are poised to move from compelling preclinical proofs-of-concept to transformative clinical realities in oncology within the coming decade.